Abstract
Aims
Coronary artery disease is the leading cause of mortality and morbidity in our country, of which ST elevation myocardial infarction (STEMI) accounts for the major part of health spending. We sought to study the effect of induction of government health insurance scheme on the trends of reperfusion in patients of acute STEMI.
Methods and results
1133 patients presenting with acute STEMI enrolled. 1079 (95.1%) received some form of reperfusion therapy. Primary PCI was used in 60.6% of patients as the primary reperfusion modality, a six fold increase as compared to previous years. Government health insurance accounted for the one third of all. 34.5% patients underwent pharmacological reperfusion, most commonly with streptokinase. 4.9% patients of STEMI did not receive any form of reperfusion therapy in contrast to 14% during previous years.
Conclusion
Introduction of government health insurance along with increased awareness has resulted in dramatic changes in the management of STEMI patients.
Keywords: Government health insurance, STEMI, Reperfusion
1. Introduction
Coronary artery disease is the leading cause of mortality globally.1 60% of the world's heart disease is expected to occur in India.2 Early restoration of patency of the infarct related artery is standard of care in management of acute ST elevation myocardial infarction (STEMI).3 Patients presenting with STEMI are usually from the local population and many from poor socio economic status. Affordability of interventional procedures is always a problem. In rural population, awareness among people about coronary artery disease and the recent advances in treatment is lacking. Government schemes have been introduced which cover medical treatment, including emergencies, for below poverty line citizens. These schemes along with subsidies provided by the treating hospital have resulted in an increasing number of primary angioplasties (PCI), which is a life saving procedure.
2. Materials and methods
This was a retrospective observational study done at Cardiology Department of Christian Medical College (CMC), Vellore, a tertiary care centre. The Department of Cardiology, CMC Vellore is equipped with all the required facilities for tackling cardiac emergencies and primary PCI. The cardiac catheterization laboratory and interventional cardiologists are available round the clock. The department receives around 700–800 patients of acute ST elevation myocardial infarction per year. All patients irrespective of age who presented with acute STEMI were included in the study. Acute ST elevation myocardial infarction (STEMI) was defined as per the recent universal definition of MI.4
2.1. Data collection and analysis
In this study, we aim to study the current trends in revascularization in STEMI in a tertiary care centre in South India. The number of patients thrombolysed with streptokinase, tenecteplase or undergoing primary PCI were determined since February 1st 2012,when Tamil Nadu Chief Minister's Comprehensive Health Scheme (TNCMCHS) was started in our institute. The percentages, mean and standard deviations were calculated. The data was scrutinized for the trends in revascularization. Data was collected from the in-patient and out-patient records as well as the records in the Coronary Care Unit (CCU) and Chest Pain Unit (CPU). Other variables that were taken into account included age, gender and risk factors for coronary artery disease. The number of patients who benefited with TNCMCHS was also taken into account. This was compared with the published data from our institute before the scheme was introduced.
3. Results
Between 1st February 2012 and 31st October 2013, a total of 1133 patients with ST-segment elevation myocardial infarction (STEMI) were enrolled into this study. The collected data is given in tabular column Table 1.
-
•
Inferior wall MI includes Inferior and all other combinations (Right ventricular, Posterior and Lateral)
-
•
Anterior wall MI includes Anterior, Antero-sepal, Anterolateral and Extensive anterior wall STEMI
-
•
Smoker includes only current smoker
Table 1.
Comparison of baseline characteristics and management strategy of patients enrolled in earlier study by Brajesh et al5 from the same centre vs present study.
| Characteristics | Earlier study n = 1905 (%) | Present study n = 1133 (%) |
|---|---|---|
| Age | 56.3 ± 11.8 | 54.2 ± 10.4 |
| Males | 1577 (83) | 938 (82.8) |
| Females | 328 (17) | 195 (17.2) |
| Smoking | 589 (31) | 373 (32.9) |
| Diabetes Mellitus | 944 (49.7) | 474 (41.8) |
| Hypertension | 657 (34) | 428 (37.7) |
| Dyslipidemia | 1345 (70) | 530 (46.8) |
| Location of MI | ||
| Anterior wall MI | 1150 (60) | 581 (51.2) |
| Inferior wall MI | 727 (38) | 552 (48.8) |
| Reperfusion therapy | ||
| Pharmacological | 1431 (75.1) | 392 (34.5) |
| PCI | 205 (10.7) | 687 (60.6) |
Data are numbers (%) or mean + SD.
4. Discussion
Mean age of STEMI patients in present study is 54.2 ± 10.4 years, similar (56.3 ± 11.8 years) to the previous data 2008–2011, Brajesh et al 2012 from the same centre. In our country, cardiovascular diseases occur a decade earlier as compared to west. Early age of STEMI could lead to tremendous loss of productive years and can have an adverse outcome on the economy as well as national growth. Affordability is the main hindrance in our country for availing the best medical care for STEMI patients.
4.1. Trends in STEMI
This study also analyzed the main risk factors for CAD prevalence in the Indian population which included diabetes mellitus (41.8%), systemic hypertension (37.7%), current smokers (32.9%) and dyslipidemia (51%). As in the previous data from Brajesh et al diabetes mellitus is a significant contributor to cardiovascular diseases.5–7
The present study highlights the current scenario of STEMI and its management in a tier 3 South Indian city. With 24 h available cardiac catheterization laboratories and experienced cardiologists, the rates of primary PCI has been steadily increasing. Primary PCI was used in 60.6% of patients as the primary reperfusion modality, a six fold increase as compared to previous years (Figs. 1 and 2).
Fig. 1.
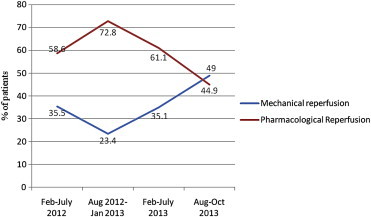
Trends of reperfusion in STEMI.
Fig. 2.
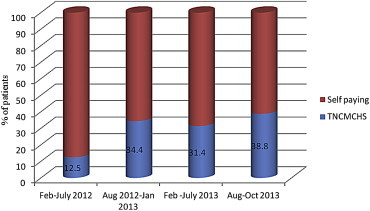
Contribution of TNCMCHS for mechanical reperfusion over study period.
There are many reasons for this, such as early diagnosis and referral from rural hospitals and general practitioners, good transport facilities due to 108 Ambulance services started under government health initiative, easy availability of government health insurance (TNCMCHS) and growing awareness. In the general population, there is an increased acceptance of mechanical reperfusion as a treatment modality, possibly as a result of the increased awareness due to better results seen in patients undergoing the procedure under the scheme. TNCMCHS covered patients made up to one third of the total number of patients undergoing mechanical reperfusion (Figs. 2 and 3). Still, a large proportion of patients (70.8%) are able to pay for primary revascularization therapy and get benefited as our hospital has subsidized the costs.
Fig. 3.
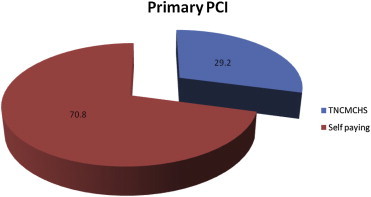
Source of finances for primary PCI over study period (% of patients).
34.5% patients still underwent pharmacological reperfusion due to various reasons including unwillingness to undergo invasive procedures in spite of clearly explaining the risk benefits. Streptokinase was primarily used for pharmacological reperfusion, in almost all the patients. Tenecteplase (TNK) was rarely used as the thrombolytic agent, mainly due to the cost factor and those patients may have opted for primary angioplasty, as primary PCI is offered at only double the cost of the drug.
An encouraging result was seen in the analysis of patients who did not receive any reperfusion therapy because of various reasons. 4.9% patients of STEMI did not receive reperfusion therapy and this is in contrast to earlier data where 14% did not receive any form of reperfusion.
Mechanical reperfusion, the ideal choice when done according to standard care, is slowly replacing pharmacological reperfusion as primary modality for STEMI management. But it has a long way to go especially in a rural setting in a developing country like India. Greater awareness in general population, government health initiatives which are easily accessible to the general population, early referral from the general practitioner, quicker transport and a well equipped referral hospital, all have an important roles to play.
In foreseeable future, mechanical reperfusion in form of primary PCI or as adjunct to thrombolysis will be more widely used as the first-line approach in contemporary management of STEMI in areas catered by our institute.
5. Conclusion
Universal health insurance, quicker transportation, early referral and lower procedural cost will help to provide the mechanical reperfusion therapy available to all STEMI patients in foreseeable future.
Conflicts of interest
All authors have none to declare.
Acknowledgment
Researchers would like to acknowledge Christian Medical College (CMC) Vellore in for providing the equipment and facilities for this research.
References
- 1.Lopaze A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Gaffar A., Reddy K.S., Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–810. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Antman E.M., Anbe D.T., Armstrong P.W. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction–executive summary. Circulation. 2004;110:588–636. doi: 10.1161/01.CIR.0000134791.68010.FA. [DOI] [PubMed] [Google Scholar]
- 4.Thygesen K., Alpert J.S., Jaffe A.S. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 5.Kunwar Brajesh Kumar, Hooda Amit, Joseph George. Recent trends in reperfusion in ST elevation myocardial infarction in a South Indian tier-3 city. Indian Heart J. 2012;64:368–373. doi: 10.1016/j.ihj.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;361:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 7.Jose V.J., Gupta S.N. Mortality and morbidity of acute ST segment elevation myocardial infarction in the current era. Indian Heart J. 2004;56:210–214. [PubMed] [Google Scholar]


