Abstract
Percutaneous Transseptal Mitral Commissurotomy (PTMC) has replaced surgical commissurotomy as a treatment of choice in selected patients of rheumatic mitral stenosis. Various randomized trials have shown PTMC to be equal or superior to surgical commissurotomy in terms of hemodynamic improvement as well as long term survival. Systemic embolism is one of the dreaded complications of PTMC, which is reported in 0.5–5% of cases and involves cerebral circulation in 1% of cases. Most of the time, periprocedural embolism during PTMC is caused by the mobilization of preexisting thrombus in the left atrial appendage. We report an unusual case of acute stroke due embolization of mitral valve tissue during PTMC.
Keywords: Mitral stenosis, Valve tissue, Embolization, Stroke
1. Introduction
Percutaneous Transseptal Mitral Commissurotomy (PTMC) has replaced surgical commissurotomy as a treatment of choice in selected patients of rheumatic mitral stenosis. Various randomized trials have shown PTMC to be equal or superior to surgical commissurotomy in terms of hemodynamic improvement as well as long term survival.1,2 Systemic embolism is one of the dreaded complications of PTMC, which is reported in 0.5–5% of cases3 and involves cerebral circulation in 1% of cases.4 Most of the time, periprocedural embolism during PTMC is caused by the mobilization of pre-existing thrombus in the left atrial appendage (LAA).5 We report an unusual case of acute stroke due to embolization of mitral valve tissue during PTMC.
2. Case presentation
A 27-year-old male presented to us with New York Heart Association (NYHA) class II dyspnea for the past five years with recent worsening of symptoms to NTHA class III. He also complained of hemoptysis and frequent episodes of paroxysmal nocturnal dyspnea. Physical examination revealed a regular heart rate of 84/min, blood pressure of 108/80 mm Hg and respiratory rate of 18/min. On auscultation, first heart sound was loud with an opening snap. He had a low pitched, rumbling mid diastolic murmur extending throughout the diastole with presystolic accentuation. The second heart sound was normally split with loud pulmonary component. No other auscultatory events were appreciable. Electrocardiogram showed sinus rhythm, left atrial (LA) and right ventricular enlargement and right axis deviation. Chest roentgenogram showed findings suggestive of LA enlargement and pulmonary artery hypertension. There was grade III pulmonary venous hypertension with Kerley B lines. A transthoracic echocardiogram (Fig. 1, Video 1) confirmed the diagnosis of severe rheumatic mitral stenosis with a mitral valve area of 0.93 cm2 by pressure half time (PHT) and 0.86 cm2 by planimetry. LA and the left atrial appendage (LAA) were free of clot (Fig. 1D). Wilkins echocardiographic mitral valve score was 6. The valve appeared highly fibrotic however there was no calcification, which was later confirmed on cinefluoroscopy.
Fig. 1.
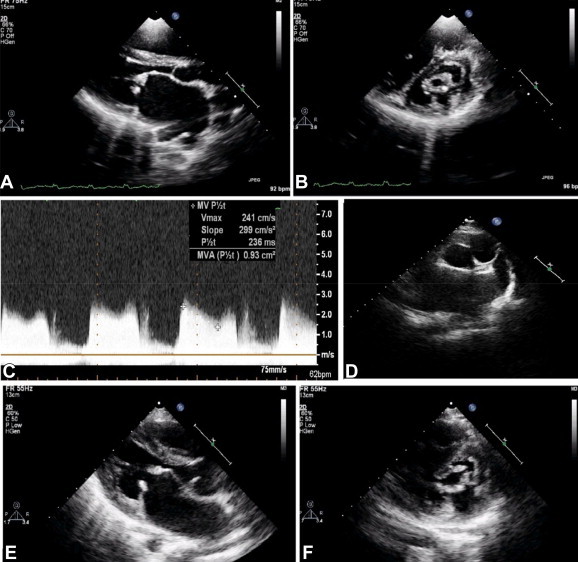
Pre-dilation transthoracic echocardiogram in A. Parasternal long axis view (PLAx) and B. Parasternal short axis (PSAx) view showing thick stenotic mitral valve C. Continuous wave Doppler interrogation across mitral valve showing significant transmitral gradient and severe mitral stenosis (mitral valve area by pressure half time = 0.93 cm2) D. PSAx view showing clear left atrial appendage. Post-dilation transthoracic echocardiogram in E. PLAx and F. PSAx view showing successful dilation with split opened both mitral commissures.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2014.05.022.
The following is the supplementary video related to this article:
Baseline transthoracic echocardiogram in parasternal long and short axis view showing thick fibrotic stenosed mitral valve.
PTMC was performed using Inoue technique, details of which are described elsewhere.4 The patient received 3000 units of unfractionated heparin after successful septal puncture and LA entry. A single dilatation (Video 2) by 26-mm Inoue balloon (Toray, New York) inflated to 25 mm successfully reduced the LA pressures from 32 mm Hg to 13 mm Hg and mean transmitral gradient fell from 23 mm Hg to 8 mm Hg. An immediate post dilatation echocardiogram (Fig. 1E and F) showed successful opening of both the mitral commissures. Mitral valve area increased to 1.50 cm2 without development of any significant mitral regurgitation.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2014.05.022.
The following is the supplementary video related to this article:
Successful dilation of mitral valve with Inoue balloon 26 mm prepared to 25 mm .
Immediately after the procedure, patient complained of slurring of speech with weakness of left half of the body. The weakness rapidly progressed to complete left side hemiplegia with left facial palsy and his sensorium began to worsen. He was immediately shifted for a computed tomography (CT) scan which excluded an intracranial hemorrhage. A diagnosis of cardio-embolic stroke was entertained and the patient was shifted back to catheterization lab for urgent catheter directed revascularization. Selective intra-arterial digital subtraction angiography (IADSA) of cerebral circulation using 6F ENVOY (Cordis Neurovascular, Miami Lakes, Fl) guiding catheter revealed complete occlusion of right internal carotid artery before its bifurcation into middle and anterior cerebral artery (Fig. 2A). Using a 0.021″ PROWLER SELECT Plus (Cordis Neurovascular, Miami Lakes, Fl) microcatheter, the lesion was crossed successfully with 0.014″ transcend guidewire (Boston Scientific, Natick, Mass, USA) (Fig. 2B and C). Solitaire FR clot retrieval device (ev3, Irvine, California) was used to retrieve extremely hard fibrotic material (Fig. 2E) from the lesion. Despite multiple attempts, the hard fibrotic embolic material couldn't be completely retrieved and flow not restored. Temporal association with balloon dilatation and absence of any preprocedure clot in the LA/LAA made us to suspect the embolised material to be a mitral valve fragment. We retrospectively analysed the post PTMC echocardiogram, and found multiple tissue tags attached to the chordae and mitral valve (Video 3), suggesting valve disruption secondary to balloon dilation, which could possibly be the cause of cerebral embolism. These tissue fragments were not present prior to balloon dilatation. Histopathology of the retrieved material (Fig. 3) confirmed it to be a detached valve tissue.
Fig. 2.
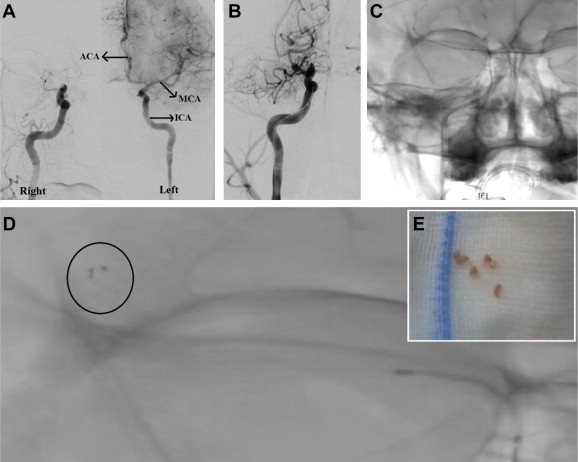
A. Intra-arterial digital subtraction angiography (IADSA) showing normal left ICA, MCA and ACA, while the right ICA is completely blocked before its bifurcation into right MCA and ACA. B. Attempting to cross the lesion using 0.021 PROWLER SELECT Plus microcatheter. C. Lesion successfully crossed by 0.014 transcends guidewire. D. Solitaire FR clot retrieval device in situ (circled). E. Retrieved hard and fibrotic embolised material. ICA: internal carotid artery, MCA: middle cerebral artery, ACA: anterior cerebral artery.
Fig. 3.
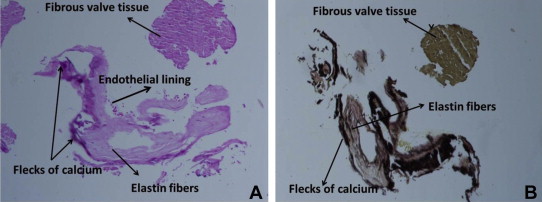
Histopathology of retrieved embolised tissue stained with A. Hematoxylin and eosin (HE) stain and B. Elastic Van Gieson (EVG) stain under 100X magnification, showing endothelial lining, fibrous tissue and elastin fibers with flecks of calcium, confirming the tissue to be embolised valve.
Supplementary video related to this article can be found at http://dx.doi.org/10.1016/j.ihj.2014.05.022.
The following is the supplementary video related to this article:
Post-PTMC transthoracic echocardiogram in parasternal long axis, parasternal short axis and apical 4 chamber view showing successful balloon dilation with opening of both mitral commissures. There are multiple highly mobile tissue tags attached to the chordae and mitral valve. These tags developed post dilation and were not present before dilation (to compare with video 1).
The patient continued to have dense left hemiparesis and altered sensorium. A repeat CT scan after 24 h showed large right hemispheric infarct with midline shift. An urgent decompression craniotomy to relieve intracranial tension was performed, following which his sensorium gradually improved. He was eventually discharged after 20 days of the procedure, in fully conscious oriented state with grade II/V power in left upper and lower limbs.
3. Discussion
PTMC is complicated by systemic embolism in 0.5–5% of cases,3 and is reported to be 0.6% with Inoue technique.6 Mobilization of pre-existing thrombus, mostly in the left atrial appendage (LAA)5 is the predominant cause of cardio-embolic stroke during PTMC, but it can be due to air leaking from balloon, embolization of fibrinothrombotic material and calcium emboli.7 Performing routine transesophageal echocardiography (TEE) in all patients prior to the procedure, intraprocedure heparinization and careful catheter manipulation in the left atrium are proposed precautions to prevent systemic embolization.8
Management involves urgent cerebral imaging to exclude intracranial hemorrhage and prompt revascularisation. Revascularisation can be achieved by systemic thrombolytic therapy with tissue plasminogen activator or various endovascular approaches, including intraarterial thrombolysis, mechanical thrombectomy, intracranial angioplasty and stent retriever thrombectomy.9
There are isolated case reports of systemic calcium embolization after PTMC.10,11 However all these reported cases had significant mitral valve calcification, which was not evident in our case on echocardiography as well as on cinefluoroscopy. To the best of our knowledge this is first case report of documented valve tissue embolization after balloon dilation of mitral valve. Development of multiple tissue tags suggests valve disruption secondary to shearing effect of balloon dilation as the possible cause of cerebral embolism. Recognizing this entity as a possible cause of acute stroke is important as lytic therapy either systemic or intraarterial is bound to fail, and mechanical revascularisation remains the only viable therapeutic option.
Conflicts of interest
All authors have none to declare.
References
- 1.Ben Farhat M., Ayari M., Maatouk F. Percutaneous balloon versus surgical closed and open mitral commissurotomy: seven-year follow-up results of a randomized trial. Circulation. 1998;97:245–250. doi: 10.1161/01.cir.97.3.245. [DOI] [PubMed] [Google Scholar]
- 2.Ommen S.R., Nishimura R.A., Grill D.E., Holmes D.R., Jr., Rihal C.S. Comparison of long-term results of percutaneous mitral balloon valvotomy with closed transventricular mitral commissurotomy at a single North American Institution. Am J Cardiol. 1999;84:575–577. doi: 10.1016/s0002-9149(99)00381-1. [DOI] [PubMed] [Google Scholar]
- 3.Vahanian Alec, Palacios Igor F. Percutaneous approaches to valvular disease. Circulation. 2004;109:1572–1579. doi: 10.1161/01.CIR.0000124794.16806.E3. [DOI] [PubMed] [Google Scholar]
- 4.Otto C.M., Bonow R.O. “Valvular heart disease”. In: Bonow R.O., editor. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 9th ed. Saunders; Philadelphia: 2012. pp. 1468–1539. [Google Scholar]
- 5.Kronzon I., Tunick P.A., Glassman E., Slater J., Schwinger M., Freedberg R.S. Transoesophageal echocardiography to detect atrial clots in candidates for percutaneous transseptal mitral balloon valvuloplasty. J Am Coll Cardiol. 1990;16:1320–1322. doi: 10.1016/0735-1097(90)90572-7. [DOI] [PubMed] [Google Scholar]
- 6.Drobinski G., Montalescot G., Evans J. Systemic embolism as a complication of percutaneous mitral valvuloplasty. Cathet Cardiovasc Diagn. 1992;25:327–330. doi: 10.1002/ccd.1810250416. [DOI] [PubMed] [Google Scholar]
- 7.Vahanian A., Lung B., Cormier B. In: “Mitral Valvuloplasty.” Textbook of Interventional Cardiology. 5th ed. Topol Eric J., editor. Saunders; Philadelphia: 2008. pp. 879–893. [Google Scholar]
- 8.Nobuyoshi M., Arita T., Shirai S. Percutaneous balloon mitral valvuloplasty: a review. Circulation. 2009 Mar 3;119:e211–e219. doi: 10.1161/CIRCULATIONAHA.108.792952. [DOI] [PubMed] [Google Scholar]
- 9.Meyers P.M., Schumacher H.C., Connolly E.S., Jr., Heyer E.J., Gray W.A., Higashida R.T. Current status of endovascular stroke treatment. Circulation. 2011 Jun 7;123:2591–2601. doi: 10.1161/CIRCULATIONAHA.110.971564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Powell B.D., Holmes D.R., Jr., Nishimura R.A., Rihal C.S. Calcium embolism of the coronary arteries after percutaneous mitral balloon valvuloplasty. Mayo Clin Proc. 2001 Jul;76:753–757. doi: 10.4065/76.7.753. [DOI] [PubMed] [Google Scholar]
- 11.Montalescot G., Drobinski G., Thomas D. Peripheral calcific embolism after percutaneous mitral valvuloplasty. Arch Mal Coeur Vaiss. 1992 Jun;85:905–907. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Baseline transthoracic echocardiogram in parasternal long and short axis view showing thick fibrotic stenosed mitral valve.
Successful dilation of mitral valve with Inoue balloon 26 mm prepared to 25 mm .
Post-PTMC transthoracic echocardiogram in parasternal long axis, parasternal short axis and apical 4 chamber view showing successful balloon dilation with opening of both mitral commissures. There are multiple highly mobile tissue tags attached to the chordae and mitral valve. These tags developed post dilation and were not present before dilation (to compare with video 1).


