Abstract
Objective
To compare the long term effects of yoga based cardiac rehabilitation program with only physiotherapy based program as an add-on to conventional rehabilitation after coronary artery bypass grafting (CABG) on risk factors.
Methods
In this single blind prospective randomized parallel two armed active control study, 1026 patients posted for CABG at Narayana Hrudayalaya Institute of Cardiac Sciences, Bengaluru (India) were screened. Of these, 250 male participants (35–65 years) who satisfied the selection criteria and consented were randomized into two groups.
Within and between group comparisons were done at three points of follow up (i.e. 6th week, 6th month, and 12th month) by using Wilcoxon's signed ranks test and Mann Whitney U test respectively.
Results
Yoga group had significantly (p = 0.001, Mann Whitney) better improvement in LVEF than control group in those with abnormal baseline EF (<53%) after 1 year. There was a better reduction in BMI in the yoga group (p = 0.038, between groups) in those with high baseline BMI (≥23) after 12 months. Yoga group showed significant (p = 0.008, Wilcoxon's) reduction in blood glucose at one year in those with high baseline FBS ≥110 mg/dl. There was significantly better improvement in yoga than the control group in HDL (p = 0.003), LDL (p = 0.01) and VLDL (p = 0.03) in those with abnormal baseline values. There was significantly better improvement (p = 0.02, between groups) in positive affect in yoga group. Within Yoga group, there was significant decrease in perceived stress (p = 0.001), anxiety (p = 0.001), depression (p = 0.001), and negative affect (p = 0.03) while in the control group there was reduction (p = 0.003) only in scores on anxiety.
Conclusion
Addition of yoga based relaxation to conventional post-CABG cardiac rehabilitation helps in better management of risk factors in those with abnormal baseline values and may help in preventing recurrence.
Keywords: Yoga, Physiotherapy, Cardiac rehabilitation, LVEF, Risk factors
1. Introduction
World Health Organization (WHO) has been sounding an alarm on the rapidly rising burden of cardio-vascular disorders for the past 15 years.1 The reported prevalence of coronary artery disease (CAD) in adult surveys has risen 4-fold over the last 40 years (to a present level of around 10%) accounting for 29% of all deaths in 2005.2 It strikes Indians early and kills many in their productive mid-life years.3
Coronary artery bypass grafting (CABG) is by far the most common among the surgical methods of management in CAD4 even in India. The cardiac functional status and the level of psychosocial stress before surgery can influence the quality of life and prognosis after CABG.5,6 LVEF as seen in 2D-echocardiogram has favorable correspondence to invasive data7 and has been found to be of predictive value for both, the immediate post-operatives prognosis (the duration of hospital stay) and late mortality after CABG.8,9 Depression has been found to be another independent prognostic factor for mortality, readmission, cardiac events and lack of functional benefits 6 months10 to 5 years11 after CABG. These observations point to the need for integrating psychosocial interventions during critical care to provide holistic and effective management after CABG.12
Several studies have documented the benefits of relaxation techniques in pre and post-operative period. In a two armed randomized controlled study, Engblom et al13 showed increased hobby activities and reduction in scores on Beck's Depression Index during the first post-operative year after CABG in the group who had a comprehensive post-op rehabilitation (physical exercise, relaxation training, group discussion sessions and dietary advice) as compared to the group who had hospital based rehabilitation. Another study observed significant reductions in both state and trait anxiety after 6 weeks of progressive muscular relaxation in anxious patients after CABG.14 Patients who listened to audiotape information containing information to improve post-operative outcomes had significantly increased physical activity with fewer symptoms of shoulder pain or back pain or anorexia, than the control group.15
It is noteworthy that a few similar interventional studies,13–15 observed no changes in the quality of life after 6 weeks to one year of interventions which points to the need for carefully designed type, frequency and duration of interventions. Yoga including meditation has been incorporated in life style interventions in CAD since nineteen seventies. Yoga is emerging as a useful rehabilitation tool for various chronic lifestyle related ailments.16 Transcendental Meditation (TM) program has been found to decrease CAD risk factors, cardiovascular morbidity,17,18 carotid atherosclerosis,19 and mortality.20,21 Intensive yoga based life style modification program have been shown to retard coronary atherosclerosis.22–24 There are no published studies reporting the effect of add-on yogic relaxation techniques in post-CABG rehabilitation. Hence the present study was planned to assess the complimentary effects of yogic relaxation with the hypothesis that this would offer additional benefits to conventional post-CABG rehabilitation.
2. Methods
2.1. Participants
One thousand twenty six patients with CAD (established by coronary angiogram) who were posted for elective CABG surgery at Narayana Hrudayalaya Institute of Cardiac Sciences (NHICSc), Bengaluru (India) were screened. Two hundred and fifty male participants in the age range of 35–65 years, who fulfilled the selection criteria were randomized into two groups.
Inclusion criteria were: (a) those with established double or triple vessel disease posted for elective CABG, (b) males between 35 and 65 years of age, and (c) those with their residential address within 200 km from NHICSc hospital to ensure compliance for follow up. Female patients posted for CABG were excluded as the post-CABG prognosis is different in females25 and the number of females available for final subgroup analysis would be insufficient. Other exclusion criteria were: emergency CABG, CABG with valve surgeries, acute and chronic renal failure with or without dialysis, physical disabilities that would prevent them from doing yoga practices, neuro-psychiatric illness, and patients already exposed to yoga. Those with left ventricular ejection fraction (LVEF) <30% were also excluded as the ethical committee was not convinced about the safety of the procedure and this was the first study with no published evidence for the safety of the yoga techniques used.
The study was funded by the Department of AYUSH, Ministry of Health and Family Welfare, New Delhi, India under the ‘Extra Mural Research’ scheme. The research protocol including the informed consent forms in English and Kannada languages, were approved by the institutional ethics committee of both SVYASA University and NHICSc. Signed informed consent was obtained from all participants before recruitment.
2.2. Design
This was a single blind longitudinal prospective randomized parallel two armed control study, conducted by the division of yoga and life sciences of the SVYASA University, Bengaluru, India between 2003 and 2007 at NHICSc., Bengaluru.
2.3. Procedure
Participants were allocated to two groups using a computer-generated random number table (www.randomizer.org). The table was generated by the statistician at the university center, that allocated them to the yoga based life style modification program (YLSP) or physiotherapy based life style modification program (PTLSP) groups. After recruitment all baseline data were documented by the research team. The Yoga therapist personally visited the ward and taught yogic relaxation twice a day for 1–3 days after admission during the pre-operative preparation. After ensuring the correctness of practice with right understanding, the patient was asked to continue the practice using a pre-recorded audio tape. After the surgery, the nurses in the ICU ensured the practice through the audio player. Two to three days before discharge, when the patient was out of the ICU, the yoga therapist sat with the patient and revised the practice under supervision. After discharge they were asked to continue the practices twice daily. They were taught more yoga techniques (Table 1) during their 6th week and 6th month follow up visits. Home practice (one hour/day) was monitored by providing a life style diary and regular weekly phone calls by the therapist. All relevant data were taken on the day before surgery and during their follow up visits after 6 weeks, 6 months and 1 year after surgery.
Table 1.
List of practices for the experimental group (yoga based life style modification program).
| Module | Duration | Yoga based life style modification program |
|---|---|---|
| 1 | Pre-op day to 6 weeks | Deep Relaxation Technique (DRT) |
| Mind sound resonance technique (MSRT) | ||
| Nadisuddhi Pranayama | ||
| 2 | 6 weeks to 6 months | Sukshma vyayamas for |
| Wrist – Manibandha shakti vikasaka | ||
| Back of hand – Karaprasta shakti vikasaka | ||
| Elbows – Kaphoni shakti vikasaka | ||
| Neck – Griva shakti vikasaka I & II | ||
| Back – Kati shakti vikasaka I & II | ||
| Eyes – Netra shakti vikasaka | ||
| Legs – Padasanchala | ||
| Quick relaxation technique (QRT), DRT and MSRT | ||
| 3 | 6 months to 12 months | Yogic Breathing practices |
| Prasarita hasta swasah (Hands in & out breathing) | ||
| Utkashita hasta swasah (Hands stretch breathing) | ||
| Vyaghra swasah (Tiger breathing) | ||
| Ekapadauttana swasah (Straight leg raise breathing) | ||
| Asanas – 20 min | ||
| Standing position | ||
| Ardha kati chakrasana (Lateral half wheel posture) | ||
| Trikonasana (Triangle posture) | ||
| Vrikshasana (Tree posture) | ||
| Garudasana (Eagle posture) | ||
| Prone posture | ||
| Bhujangasana (Serpent posture) | ||
| Sitting posture | ||
| Vakrasana (Spinal twist with leg straight) | ||
| Ardhamatsyendrasana (Half spinal twist) | ||
| Vajrasana (Diamond posture) | ||
| Supine posture, QRT, DRT and MSRT |
2.4. Blinding
As this was an interventional study, the participants and trainers could not be blinded; the team who did the laboratory assessments and the statistician were blind to the source of the data.
2.5. Intervention
Pharmacotherapy as advised by the clinician and the conventional post-operative rehabilitation practices, were common to both groups. The medication dosages during the baseline and intervention periods were kept stable by participant and physician consent. There was no significant difference in the percentage of subjects taking medications in the two groups (Table 3). Under conventional post-CABG rehabilitation, common daily practices (30 min) were administered by a team of trained physiotherapists to both groups which included: (a) gradually increasing distance and speed of walking with intermittent relaxation covering a total of about 2 km/day, (b) breathing exercises and (c) breathing through lung exerciser. Different sets of reading material were provided for the two groups.
Table 3.
Demographic data.
| Particulars | YLSP | PTLSP | |
|---|---|---|---|
| Sex (only male) | n = 129 | n = 121 | |
| Age range (years) | 35–65 | 35–65 | |
| Age (years) Mean (SD) | 53.34 (6.42) | 52.6 (6.85) | |
| Education | School | 25 | 26 |
| Undergraduates | 37 | 39 | |
| Graduates | 26 | 40* | |
| Post-Graduates | 32 | 25 | |
| Socio-economic Status | Upper class | 10 | 08 |
| Middle class | 65 | 79 | |
| Lower class | 35 | 42 | |
| Duration of CAD | <1 year | 71 | 80 |
| 1–5 | 42 | 42 | |
| 5–10 | 7 | 08 | |
| Nature of CAD | SVD | 20 | 15 |
| DVD | 31 | 39 | |
| TVD | 69 | 76 | |
| Associated conditions | HTN | 38 | 31 |
| DM | 20 | 15 | |
| HTN + DM | 53 | 63 | |
| Ejection fraction | ≤35 | 3 | 4 |
| 36–40 | 8 | 6 | |
| 41–45 | 11 | 18 | |
| 46–50 | 19 | 27 | |
| 51–55 | 33 | 36 | |
| 56–60 | 46 | 38 | |
| Medications | Antiplatelet agents | 117 | 111 |
| Statins | 89 | 86 | |
| Beta-blockers | 67 | 69 | |
| ACEI/ARB's | 76 | 65 | |
| CCB/Nitrates | 29 | 24 | |
| Hypoglycemic agents | 73 | 78 | |
| Family history of CAD | 28 | 22 | |
| Cigarette smoking | 23 | 22 | |
| Tobacco chewing | 18 | 16 | |
| Alcohol consumption | 25 | 15* | |
*p < 0.05, Independent Samples t test.
Abbreviations: YLSP: yoga life style program; PTLSP: physiotherapy life style program; SVD: single vessel disease; DVD: double vessel disease; TVD: triple vessel disease; HTN: hypertension; DM: diabetes mellitus; CAD: coronary artery disease; SD: standard deviation; ACEI: Angiotensin Converting Enzyme Inhibitors; ARB: Angiotensin Receptor Blocker; CCB: Calcium Channel Blocker.
2.6. Yoga intervention (Table 1)
The integrated yoga intervention included simple and safe practices at physical, mental, emotional, intellectual levels to reach a state of mastery over the modifications of the mind (Chitta Vritti Nirodhah – definition of yoga by sage Patanjali) through effortless blissful inner awareness during all practices. Three yoga modules (of 30 min each) were prepared to suit the three periods of rehabilitation. The first module (upto 6th week) included MSRT (Mind Sound Resonance Technique), breath awareness and DRT (deep relaxation technique), all done in supine posture. MSRT is a systematic training consisting of 8 steps of sound meditation (based on Māndukya Upanishad26 and Gheranda Samhitā.27 It involves gentle chanting of the syllables A, U, M, and OM to feel the resonance inside the body cavities i.e. abdomen, chest, skull and entire trunk respectively. This is done repeatedly while alternating between audible chanting (Ahata Nādanusandhāna) and mental chanting (Anāhata Nādanusandhāna). This phase is followed by a resolve and closing prayer. Physical postures and pranayama practices were added in the second (6th week to 6th month) and third (6th month to 12th month) yoga modules (Table 1). These three modules of integrated approach of yoga therapy for life style disorders were developed by experts on the basis of ancient yogic scriptures. These modules have been found to be safe and beneficial in our clinical practice at 250 bedded holistic health home, Arogyadhama, Bangalore, since last 20 years.28
Counseling for the YLSP group on yogic life style modification included the concepts of right living from Indian yoga psychology while the PTLSP group were counseled using scientific information on life style modification recommended in conventional cardiac rehabilitation programs.29 This concept of right living according to yogic tradition was introduced gradually in these modules as the person would return to work and normal life style. These included concepts of do's (niyamas) and don'ts (yamas) from Ashtānga yoga of Patanjali,30 Karma yoga from Bhagavadgita that helps in working without stress31; Bhakti yoga, the path of pure love that opens up avenues for healthy relationships32; and Jňana yoga that transforms the basic notions about life through introspective correction of the meaning and purpose of life.33 All these concepts were meant to help the individual to move towards blissfully contented joyful living with the right understanding in tune with the laws of nature that govern one's existence.
2.7. Control group intervention
The non-yogic intervention for the control group was designed to match the duration (30 min), and the level of physical activity suitable to different stages in the post-operative period (Table 2). This module of physical activity was an add-on and different from the conventional physiotherapy based rehabilitation which was common to both groups.
Table 2.
List of practices for the control group (physiotherapy based life style modification program).
| Module | Duration | Physiotherapy based life style modification program |
|---|---|---|
| 1 | Pre-op day to 6 weeks | Breathing practices |
| Physiotherapy exercises for wrist, back of hand, elbows, neck, back and legs | ||
| 2 | 6 weeks to 6 months | Breathing exercises – Inhale through the nose and exhale forcibly through the mouth |
| Breathing through lung exerciser | ||
| Additional Physiotherapy exercises for wrist, back of hand, elbows, neck, Back, legs, Shoulder rotation, slow side bending, knee cap tightening | ||
| Supine rest | ||
| 3 | 6 months to 12 months | Additional Physiotherapy exercises |
| Standing position practices | ||
| Sit-ups, Hip rotation, Knee rotation, Forward drill, | ||
| Backward drill, Sideward drill, Full arm rotation, | ||
| Free walking, | ||
| Sitting in a chair – | ||
| Chakki chalana, Ankle bending, Toe Bending, | ||
| Leg spread exercises with support - sideways, front and back | ||
| Supine rest |
The practices included mild stretches followed by breathing exercises and supine rest. Care was taken by the therapists to avoid the yoga concepts while counseling or teaching the control group intervention.
2.8. Measurements
All demographic details and base line data were documented on pre-op day. The routine pre-operative assessments included coronary angiogram performed one to four weeks before posting for surgery, Echocardiogram, ECG, lipid profiles, renal function tests, clinical assessments etc as per the conventional hospital protocol.
2.8.1. Left ventricular ejection fraction (LVEF)
2D Doppler Echo-cardiogram was recorded using Vivid-4 model, GE Company's ultrasound sound equipment, USA (Pmax – 1.2 KVA, Frequency – 50 Hz) by a certified technician using a 3 MV (lesser resolution) transducer. This was documented in the pre-operative week, and also during each follow up visit in 6th week, 6th month and 12th month after the surgery.
BMI and other clinical variables were also documented at each of the follow up visits.
2.9. Biochemical measures
Fasting blood glucose (intra-assay CV = 0.9%, inter-assay CV = 1.8%), Total cholesterol (intra-assay CV = 0.8%, inter-assay CV = 1.7%) and triglycerides (intra-assay CV = 1.5%, inter-assay CV = 1.8%) were measured using the enzymatic calorimetric method. HDL cholesterol (intra-assay CV = 2.9%, inter-assay CV = 3.6%) was measured using a homogenous calorimetric assay, whereas LDL cholesterol (intra-assay CV = 0.9%, inter-assay CV = 2.0%) was measured using a homogenous turbidimetric assay.
2.10. Psychological measures
Perceived stress scale (PSS): This is a popularly used self-rated measure of ‘stress in daily life’ that is perceived by the subject as uncontrollable and overwhelming. It is a validated tool34 that has 14 items scored on a 5-point scale and with a reliability score of 0.85.35
Hospital anxiety and depression (HADS) is a widely used validated36,37 self-reported instrument designed to assess anxiety and depression in non-psychiatric population. This 14-item questionnaire consists of two sub-scales of seven items for self-reported anxiety and depression. Patients are asked to answer what they experienced during the last two weeks, on a scale of 4 ranging from 0 (“not at all”) to 3 (“very much”). The reliability of HADS, and the two sub-scales (HADS-anxiety and HADS-depression) are 0.85, 0.79 and 0.87 respectively.38
Positive and Negative Affect Scale (PANAS): PANAS has two sub-scales i.e. positive affect (PA) and negative affect (NA) consisting of 10 items each. PA reflects the extent to which a person feels enthusiastic, active, and alert. A high PA score reflects a state of high energy, full concentration and pleasurable engagement. NA is a general dimension of subjective distress subsuming a variety of aversive mood states. A high NA score indicates more distress. This descriptive scale has proven validity39 and its reliability ranges from 0.86 to 0.90 for PA and 0.84 to 0.87 for NA.39
2.11. Data extraction and analysis
Data were analyzed using SPSS version 10.0. The baseline comparisons between the two groups were done by using independent samples t test. The baseline mean values of the drop out group were also compared with that of the study group by independent samples t test. As the data were not normally distributed, Wilcoxon's signed rank test and Mann–Whitney U test were used to compare the means within and between groups respectively.
3. Results
Fig. 1 shows the trial profile. Of the 1026 screened, 250 fulfilled the selection criteria and were recruited after obtaining the informed consent. Forty in yoga group and forty five in control group dropped out. The main reason for drop out was the constraint on time to come for follow up to NHICSc, as most of the patients were from different towns in Karnataka and they opted to get their routine follows up done from local medical practitioners.
Fig. 1.
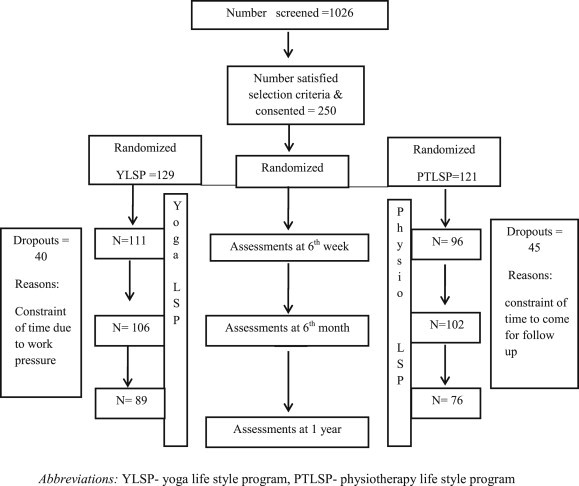
Trial profile.
The baseline characteristics are shown in Table 3. The groups were matched with no significant (p > 0.01, independent samples t test) difference between the groups at baseline except that the number of subjects consuming alcohol were higher in the yoga group. Comparison of baseline mean values of the drop out group with those who continued with the study also showed no significant difference. Three patients in yoga group and four in control group had very low (25–35%) baseline LVEF. Table 4 shows the results after the intervention.
Table 4.
Changes in ejection fraction in yoga and control groups after post-CABG rehabilitation.
| Group | Baseline |
6th week |
6th month |
1 year |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | Wilcoxon p value | n | Mean ± SD | Wilcoxon p value | n | Mean ± SD | Wilcoxon p value | ||
| EF Total | Y | 129 | 52.22 ± 6.69 | 111 | 54.58 ± 5.80 | 0.001 | 106 | 54.96 ± 5.38 | 0.001 | 89 | 55.91 ± 5.21 | 0.001 |
| C | 121 | 53.39 ± 7.14 | 96 | 53.85 ± 6.33 | 0.001 | 102 | 53.94 ± 6.68 | 0.001 | 76 | 54.12 ± 6.84 | 0.001 | |
| Mann Whitney | p value | 0.16 | 0.38 | 0.9 | 0.5 | |||||||
| EF ≤53 Median |
Y | 69 | 47.36 ± 5.23 | 61 | 51.61 ± 6.15 | 0.001 | 55 | 52.42 ± 5.89 | 0.001 | 49 | 53.28 ± 5.69 | 0.001 |
| C | 60 | 47.07 ± 5.68 | 50 | 49.0 ± 5.55 | 0.001 | 48 | 48.72 ± 6.29 | 0.001 | 33 | 48.89 ± 6.76 | 0.001 | |
| Mann Whitney | p Value | 0.63 | 0.24 | 0.43 | 0.02* | |||||||
| EF ≥53 Median |
Y | 60 | 57.87 ± 2.31 | 50 | 58.03 ± 2.66 | 0.001 | 51 | 58.34 ± 2.55 | 0.001 | 40 | 58.53 ± 2.27 | 0.001 |
| C | 61 | 58.72 ± 2.05 | 46 | 57.94 ± 3.37 | 0.001 | 54 | 57.96 ± 5.38 | 0.001 | 43 | 55.91 ± 5.21 | 0.001 | |
| Mann Whitney | p Value | 0.04* | 0.55 | 0.98 | 0.38 | |||||||
*p < 0.05, **p < 0.001.
Legend: Yoga group showed significantly better increase in EF than control group in those with abnormal baseline EF (EF ≤ 53, median). There was significant improvement in both groups with no significant difference between groups at each point of follow up. In subgroup with abnormal baseline EF (≤53, median) there was progressive increase in EF in both yoga and control groups. Yoga group improved better than control group all along and the Mann Whitney showed significant p values (p = 0.02) at one year. In the subgroup with normal baseline EF (≥53, median), the yoga group showed continuing increase in EF, while there was a decrease in EF at all points in the control group. The Mann Whitney did not show significant difference between groups at any of these points of follow up.
Abbreviations: Y: yoga group (yoga life style program); C: control (physiotherapy life style program); SD: standard deviation; EF: Ejection Fraction.
3.1. LVEF
The recent guidelines from the American Society of Echocardiography have defined an abnormal ejection fraction (EF) of the left ventricle on echocardiographic measurement as one that is less than 55%.40 Similarly, a few other studies defined LVEF less than 0.55 as systolic dysfunction in heart failure patients.41,42 Based on data from a number of more recent studies, a value less than 54% has been suggested as the cut-off value that is associated with moderate adverse outcomes.43 Another study on a large cohort (2300 subjects) of European white and Indian Asian subjects that looked at ethnicity-specific reference values of LVEF reported a cut off value of 52%.44 Based on these studies, as our target population belonged to Indian Asian community, we set our cut off LVEF value as 53%, which was our median value between the reported cut off values. Thus, we considered values ≥53% as normal and <53% as abnormal for the analysis of our data.
There was significant improvement in LVEF in both groups with no significant difference between groups at each point of follow up. In the subgroup with abnormal baseline EF (<53, median) there was progressive increase in both yoga and control groups. Yoga group improved better than control group all along and the Mann Whitney showed significant p values (p = 0.02) at one year.
In the subgroup with normal baseline EF (≥53, median), the yoga group showed continuing increase in EF, while there was a decrease in EF at all points in the control group. The Mann Whitney did not show significant difference between groups at any of these points of follow up.
3.2. Secondary outcome measures
3.2.1. BMI
We used a value of 23 as the value to define overweight,45,46 as it has been found that Indians have higher risk at lower values of BMI and the recommended cut off value is 23 (25 in Caucasians). Thus, in the subgroup with high baseline BMI (≥23), there was a significant difference between groups (p = 0.038) with better reduction in yoga group after one year. Also, this subgroup (BMI ≥ 23) showed that the weight and BMI decreased significantly within both groups at 6 weeks and 6 months, whereas only the yoga group showed significant reduction at the end of the year (p < 0.001). In those with BMI <23, there was no significant change in both the groups at any of the three time points (Table 4).
3.3. Biochemical variables
There were total 93 patients with baseline FBS ≥110 mg/dl (55 in yoga the group and 38 in the control). There was better glycemic control in yoga group, as seen by significant decrease within the group in those with FBS ≥110 mg/dl (p = 0.008) at the end of 1 year, whereas in the control group the reduction was not statistically significant (p = 0.8). There was no between group difference (p = 0.41) (Table 5). There were 11 patients who had baseline FBS ≥200 mg/dl (5 in yoga group and 6 in the control); analysis showed that there was a significant reduction in FBS in those with FBS ≥200 mg/dl in the yoga group at 6 months (p = 0.003) and at one year (p = 0.03), whereas in the control group there was a significant reduction after 6 months (p = 0.008) with non-significant change at the end of the year (p = 0.06) (Table 5) with no significant difference between the groups at the end of 6 months (p = 0.213) as well as one year (p = 0.32) (Table 5).
Table 5.
Changes in BMI and psychological measures after one year of intervention.
| Variable | Group | Base line Mean (SD) |
95% CI | 1 Year Mean (SD) |
95% CI | p – value (within group) | % Change | p – value (between the groups) | |
|---|---|---|---|---|---|---|---|---|---|
| STRESS | PSS | Y | 18.76 (4.73) | 9.48–28.03 | 15.54 (4.5) | 6.72–24.36 | 0.001** | 14.94 | 0.12 |
| C | 16.28 (4.46) | 7.53–25.021 | 16.75 (4.30) | 8.32–25.178 | 0.49 | 6.71 | |||
| PANAS | Positive | Y | 39.18 (8.16) | 23.18–55.17 | 40.54 (7.97) | 24.91–56.16 | 0.08 | 3.47 | 0.02* |
| C | 34.67 (8.72) | 17.57–51.76 | 35.83 (8.72) | 18.73–52.92 | 0.36 | 3.34 | |||
| Negative | Y | 28.57 (8.71) | 11.49–45.64 | 26.82 (8.08) | 10.98–42.65 | 0.03* | 6.12 | 0.97 | |
| C | 27.0 (9.46) | 8.45–45.54 | 26.3 (7.62) | 11.36–41.23 | 0.76 | 2.59 | |||
| HADS | Anxiety | Y | 7.42 (3.40) | 0.75–14.08 | 5.75 (3.46) | −1.03 to 12.53 | 0.001** | 27.03 | 0.42 |
| C | 7.84 (3.05) | 1.86–13.81 | 6.15 (2.98) | 0.30–11.99 | 0.003* | 13.02 | |||
| Depression | Y | 6.59 (3.44) | −0.15 to 13.33 | 4.65 (3.51) | −2.22 to 11.52 | 0.001** | 30.77 | 0.07 | |
| C | 6.85 (3.56) | −0.12 to 13.82 | 5.61 (3.30) | −0.85 to 12.07 | 0.05* | 14.66 | |||
| BMI (kg/m2) | ≥23 | Y | 26.60 (2.30) | 26.16–27.03 | 24.47 (1.85) | 20.84–28.09 | 0.001** | 8.00 | 0.038* |
| C | 26.15 (2.10) | 25.76–26.53 | 25.82 (2.25) | 21.41–30.23 | 0.161 | 1.26 | |||
| <23 | Y | 21.47 (1.32) | 18.88–24.05 | 21.70 (1.35) | 20.72–22.67 | 0.55 | 1.07 | 0.39 | |
| C | 21.07 (1.50) | 19.13–24.01 | 20.94 (2.49) | 18.32–23.56 | 0.50 | 0.61 | |||
| Total | Y | 26.76 (3.24) | 20.40–33.11 | 23.93 (2.56) | 18.91–28.94 | 0.001** | 6.72 | 0.001** | |
| C | 25.22 (3.15) | 19.04–31.39 | 24.93 (3.46) | 18.14–31.71 | 0.09 | 1.15 | |||
| Body weight (kgs) | ≥65 | Y | 73.71 (7.88) | 58.26–89.15 | 67.13 (7.59) | 52.25–82.00 | 0.001 | 8.93 | 0.001** |
| C | 75.73 (7.97) | 60.10–91.35 | 73.88 (8.08) | 58.04–89.71 | 0.0015 | 2.45 | |||
| <65 | Y | 63.13 (4.98) | 53.36–72.89 | 60.42 (4.47) | 51.65–69.18 | 0.001** | 4.29 | 0.64 | |
| C | 61.33 (6.57) | 48.45–74.20 | 61.10 (7.85) | 45.71–76.48 | 0.67 | 0.37 | |||
| Total | Y | 69.01 (8.85) | 51.66–86.35 | 64.12 (7.42) | 49.57–78.66 | 0.001** | 7.32 | 0.01* | |
| C | 68.17 (10.34) | 47.90–88.43 | 67.34 (10.41) | 46.93–87.74 | 0.035 | 1.22 | |||
| FBS (mg%) | ≥110 | Y | 147.22 (35.46) | 77.71–216.72 | 135.52 (52.03) | 33.54–237.49 | 0.008* | 7.65 | 0.41 |
| C | 153.77 (41.07) | 73.27–234.26 | 142.48 (50.66) | 43.18–241.77 | 0.08 | 7.34 | |||
| ≥125 | Y | 156.17 (21.34) | 115.15–197.99 | 149.3 (61.9) | 27.98–270.62 | 0.59 | 4.20 | 0.47 | |
| C | 154.41 (18.07) | 119.00–189.82 | 139.00 (46.50) | 47.86–230.14 | 0.17 | 9.97 | |||
| ≥200 | Y | 233.00 (29.46) | 159.81–306.19 | 164.00 (14.17) | 136.23–191.77 | 0.03* | 29.60 | 0.32 | |
| C | 228.40 (27.42) | 190.85–270.15 | 159.80 (44.63) | 72.33–247.27 | 0.06 | 30.03 | |||
| <125 | Y | 117.20 (36.71) | 45.25–181.15 | 121.28 (47.06) | 29.05–213.15 | 0.46 | 3.48 | 0.95 | |
| C | 111.35 (38.34) | 36.21–186.49 | 120.76 (45.65) | 31.29–210.13 | 0.21 | 8.45 | |||
| Total | Y | 122.3 (44.13) | 35.80–208.79 | 119.50 (45.64) | 30.04–208.95 | 0.04* | 2.79 | 0.75 | |
| C | 121 (49.61) | 23.76–218.23 | 124.02 (46.49) | 32.89–215.14 | 0.27 | 2.41 |
*p < 0.05, **p < 0.001.
Legend: Table 5 shows significant differences between the groups where yoga-based lifestyle modification (Y) group showed better improvement in positive affect, BMI and bodyweight as compared to physiotherapy-based lifestyle modification (C).
Abbreviations: PSS: Perceived Stress Scale; PANAS: Positive and Negative Affect Scale; HADS: Hospitals Anxiety and Depression Scale; BMI: Body Mass Index; FBS: Fasting Blood Sugar; Y: yoga group (yoga life style program); C: control (physiotherapy life style program); SD: standard deviation.
3.3.1. Lipid profile
There was significant decrease in triglycerides within both groups (p = 0.001) in those who had high baseline values (≥150 mg/dl) with no significant difference between the groups (p = 0.37). There was significantly better increase in HDL in yoga than control group (p = 0.003 between groups). Also the increase in those with low HDL values (<35 mg/dl) was better in yoga (p = 0.001) group than the control (p = 0.03) group. LDL levels also reduced significantly in both the groups, with non-significant difference between groups.
Looking at sub-group analysis, the yoga group showed significant reduction in LDL (p = 0.01) levels with significant difference between the groups (p = 0.01) in those who had values >100 mg/dl. VLDL reduced in both the groups significantly with a better reduction (p = 0.03) in Yoga than the control. Thus, yoga group had better changes in lipid profile than control group in those with abnormal baseline values.
3.4. Psychological variables
3.4.1. PSS, HADS and PANAS (Table 5)
Within Yoga group, there was significant decrease in PSS (p = 0.001), HADS-Anxiety (p = 0.001), HADS-Depression (p = 0.001), and PANAS-Negative (p = 0.03). In Control group, there was significant decrease only in HADS-Anxiety, (p = 0.003). Also, there was significant difference between Yoga and Control groups in positive component of PANAS (p = 0.02).
This improvement in positive affect points to better wellness and quality of life. Although no specific validated questionnaire has been included here, the clinicians who checked all patients during follow up reported that those who had practiced yoga returned to normalcy much faster and earlier than the control group.
4. Discussion
This single blind prospective randomized two armed active control study has shown that YLSP was significantly better than PTLSP in increasing LVEF (p = 0.02, Mann Whitney test) one year after CABG surgery in those with abnormal (<median) baseline LVEF values. YLSP was also more beneficial in normalizing many risk factors including BMI, blood glucose, triglycerides, VLDL, LDL and HDL in those with abnormal baseline values. Although anxiety and depression reduced in both cases, positive affect increased only in the yoga group pointing to the role of yoga in promoting psychological wellness in addition to the physical benefits.
To our knowledge, this is the first randomized controlled yoga based life style study with a yearlong follow up in patients after CABG. A systematic review47 of cardiac rehabilitation studies on 7683 patients with coronary heart disease from earlier meta-analyses concluded that both comprehensive cardiac rehabilitation and rehabilitation program based on exercise only are effective in reducing cardiac mortality. Cardiac mortality reduced by 31%, with exercise based cardiac rehabilitation and 26% with comprehensive cardiac rehabilitation program. Although such life style modification studies had established the role of intensive life style modification programs in risk-factor modification and prolonging survival among post-myocardial infarction (MI) patients before 2000, the efficacy of these programs in reducing risk factors in patients after CABG were not well-established48 until more recent randomized prospective studies. A well designed randomized control study on behavioral and educational cardiac rehabilitation program as early as 1995 by Oldenburg et al48 had shown few differences in risk factors between the study groups one year after CABG. Detry et al49 studied the effects of early and short-term (2–3 months) intensive multidisciplinary ambulatory cardiac rehabilitation program after coronary artery bypass surgery (CABG) or acute myocardial infarction which showed better compliance to aspirin intake, a low rate of smoking (14% of the patients), a 15% increase in physical capacity and decrease in resting heart rate. They also observed a 4 mg/dl increase in the HDL-cholesterol while our study has shown an increase in HDL by 8 mg/dl after yoga (6.45 mg% in control group) in those who had low HDL values (Table 6).
Table 6.
Changes in lipid profile after one year of intervention.
| Lipids | Group | Base line Mean (SD) |
95% CI | 1 Year Mean (SD) |
95% CI | p – value (within group) | % Change | p – value (between the groups) | |
|---|---|---|---|---|---|---|---|---|---|
| Total Chol. | >200 | Y | 221.33 (23.86) | 162.06–280.61 | 183.33 (65.73) | 20.03–346.63 | 0.19 | 17.16 | 0.22 |
| C | 219.33 (12.20) | 206.52–232.15 | 217.67 (29.31) | 186.90–248.43 | 0.76 | 14.78 | |||
| <200 | Y | 146.09 (25.13) | 140.05–152.13 | 159.59 (36.53) | 150.82–168.37 | 0.002* | 8.45 | 0.95 | |
| C | 146.12 (21.73) | 140.35–151.89 | 160.51 (33.97) | 151.49–169.52 | 0.001** | 9.85 | |||
| Total | Y | 151.24 (30.35) | 91.75–210.72 | 163.04 (38.01) | 88.54–237.53 | 0.007* | 7.80 | 0.61 | |
| C | 154.21 (29.92) | 95.56–212.85 | 167.43 (38.90) | 91.18–243.67 | 0.003* | 8.57 | |||
| TGLYD | ≥150 | Y | 228.00 (80.99) | 202.10–253.90 | 158.45 (60.17) | 139.20–177.70 | 0.001** | 30.50 | 0.37 |
| C | 237.46 (70.17) | 214.06–260.86 | 175.30 (60.00) | 155.29–195.30 | 0.001** | 26.30 | |||
| <150 | Y | 115.03 (20.73) | 107.56–122.51 | 114.88 (47.15) | 97.88–131.87 | 0.99 | 0.13 | 0.41 | |
| C | 116.93 (20.31) | 108.89–124.96 | 125.48 (45.85) | 107.34–143.62 | 0.23 | 8.20 | |||
| Total | Y | 180.19 (83.54) | 16.45–343.92 | 142.57 (62.9) | 19.28–265.85 | 0.001** | 20.87 | 0.03* | |
| C | 187.13 (78.74) | 32.79–341.46 | 155.28 (57.98) | 41.63–268.92 | 0.001** | 17.02 | |||
| HDL | <35 | Y | 30.17 (3.15) | 28.16–32.17 | 37.92 (6.99) | 33.47–42.36 | 0.001** | 25.68 | 0.57 |
| C | 29.75 (3.91) | 27.92–31.58 | 36.20 (11.80) | 30.68–41.72 | 0.03* | 21.68 | |||
| ≥35 | Y | 40.45 (4.81) | 39.33–41.58 | 40.21 (9.55) | 37.98–42.43 | 0.82 | 0.59 | 0.19 | |
| C | 40.77 (5.85) | 39.05–42.49 | 37.98 (8.66) | 35.43–40.52 | 0.01* | 6.84 | |||
| Total | Y | 38.67 (6.29) | 26.34–50.99 | 40.23 (9.30) | 22.00–58.45 | 0.19 | 4.034 | 0.003* | |
| C | 37.23 (7.39) | 22.74–51.71 | 37.17 (9.68) | 18.19–56.14 | 0.34 | 6.0 | |||
| LDL | ≥100 | Y | 122.52 (22.60) | 112.23–132.81 | 91.38 (43.04) | 71.79–110.98 | 0.01* | 25.41 | 0.01* |
| C | 114.67 (13.76) | 107.05–122.29 | 125.20 (33.87) | 106.44–143.96 | 0.27 | 9.18 | |||
| <100 | Y | 66.54 (19.75) | 61.72–71.36 | 92.19 (28.58) | 85.22–99.17 | 0.001** | 27.82 | 0.84 | |
| C | 69.27 (17.21) | 64.62–73.93 | 91.15 (29.57) | 83.15–99.14 | 0.001** | 31.58 | |||
| Total | Y | 75.97 (27.65) | 21.77–130.16 | 96.61 (29.51) | 38.77–154.44 | 0.001** | 27.16 | 0.75 | |
| C | 78.17 (24.15) | 30.83–125.50 | 98.77 (33.53) | 33.05–164.48 | 0.001** | 26.35 | |||
| VLDL | ≥40 | 55.42 (15.81) | 49.62–61.22 | 55.16 (36.89) | 41.63–68.70 | 0.91 | 0.46 | 0.37 | |
| 55.75 (13.67) | 51.12–60.38 | 48.50 (24.04) | 40.37–56.63 | 0.065 | 13.00 | ||||
| <40 | 26.52 (6.49) | 24.94–28.11 | 27.52 (14.27) | 24.04–31.00 | 0.57 | 3.77 | 0.70 | ||
| 26.99 (7.72) | 24.64–29.33 | 28.55 (12.60) | 24.71–32.38 | 0.46 | 5.46 | ||||
| Total | Y | 34.92 (16.28) | 3.01–66.82 | 28.51 (12.59) | 3.83–53.18 | 0.001** | 18.35 | 0.03* | |
| C | 36.21 (15.28) | 6.26–66.15 | 31.58 (13.22) | 5.66–57.49 | 0.03* | 11.95 |
*p < 0.05, **p < 0.001.
Legend: Table 6 shows significant differences between the groups where yoga-based lifestyle modification (Y) group showed better improvement in total triglycerides, total HDL, LDL in those with baseline more than or equal to 100 mg% and total VLDL as compared to physiotherapy-based lifestyle modification (C).
Abbreviations: Chol: Cholesterol; TLGYD: Triglycerides; LDL: Low Density Lipoproteins; HDL: High Density Lipoproteins; VLDL: Very Low Density Lipoproteins; Y: yoga group (yoga life style program); C: control (physiotherapy life style program); SD: standard deviation.
4.1. LVEF
In patients with CAD, reduced left ventricular function is a good predictor of unfavorable long term prognosis8 and is an important indicator for in-hospital and late mortality after CABG for CAD.50,7,8 An intensive information, education and counseling program in CAD patients with more than 70% stenosis and left ventricular ejection fraction of more than 30%, showed significant improvement in LVEF in those with adherence to the new life style regimen by 80% or more.51 Goodman et al52 studied the effects of 12 weeks of endurance exercise training on exercise performance and left ventricular ejection fraction (EF) in a group of uncomplicated CABG (n = 31) cases. A significant improvement in VO2max was observed after training, accompanied by an increase in the EF during submaximal exercise (60 ± 3% versus 63 ± 2% at 40% VO2max; 61 ± 3% versus 64 ± 3% at 70% VO2max). Although our patients had lower baseline EF values (53%) than Goodman's study group (60%) who were given endurance exercise training, the degree of change after the intervention was similar (around 3%) in both studies. Thus, the effects of both endurance exercise training and yoga appear to offer comparable effects on EF in post-CABG patients. In our study, we observed that LVEF reduced significantly in the control group in those with normal LVEF values (≥53, median) over a span of one year. Though, there was no significant difference between the groups for above mentioned results, this reduction within the control sub-group is surprising, as both the groups underwent successful CABG surgery. Here, one possible explanation could be the absence of relaxation sessions in the control group which were a primary focus in the yoga intervention. In a randomized controlled prospective study,53 90 post MI patients were randomly assigned to either exercise training plus individual relaxation group or exercise training only. Results showed that the occurrence of cardiac events, consisting of cardiac death and of readmission to hospital for unstable angina pectoris, coronary artery bypass grafting (CABG) or recurrent infarction, were significantly higher in the exercise training only group than the group with add-on relaxation in the 2–3 years follow up period after infarction.53 Also, another study showed that for post-CABG patients with normal LVEF (≥55%), the same inpatient exercise protocol triggered a more attenuated cardiac autonomic response compared with patients with reduced LVEF (<55%).54 This finding suggested that post-CABG patients with normal and abnormal LVEF may respond differently to the same exercise protocol in terms of their cardiac autonomic responses and those with abnormal LVEF responding more favorably than those with normal LVEF, and the volume of the inpatient exercises should be prescribed according to the left ventricular function following recovery from CABG.54 This may possibly explain the reduction in LVEF in those with normal values (≥53, median) in the control group in our study.
4.2. Mechanism
We propose that yoga may have operated by reducing stress arousal.55,56 It is known that, chronic stress has an important role in the pathogenesis of atherosclerosis57,58; psychological distress, depression and state anxiety are extremely frequent, often clustered, in patients after CABG60; and these are important determinants of health care utilization within 6 months post discharge in CABG patients.61
Several studies have shown that intensive cardiac rehab techniques do reduce many psychological abnormalities. A year-long prospective study on post-CABG cardiac rehabilitation program showed significant decrease in state anxiety and depression.62 In another study,63 there was significant reduction in anxiety and depression in the anxious and depressed groups at 12 weeks and 6 months but there was no significant reduction at 12 months after an exercise and education-based rehabilitation program after CABG in our study, the yoga group has shown sustained reduction in anxiety, depression, perceived stress and negative affect even after one year. Reduction in sympathetic activity after yoga55,59 has been documented which explains the improvement in these variables observed in the present study. It is interesting to note that positive affect was significantly better in those who practiced yoga instead of PT exercises after CABG pointing to yoga's ability to promote positive wellbeing; this could be an important factor that contributed to the complimentary benefits.
Stress reducing effects of yoga that offer correction in the mind set by regular introspective practices at physical, mental, emotional, and intellectual levels, have been investigated in both healthy volunteers and patients with many non-communicable diseases. This may be mediated through better autonomic regulation as shown by many studies.64–66 Yoga may produce favorable effects through modulation of neuro-endocrino-immunologic pathways. Cortisol levels are positively associated with stress and anxiety67 and Yoga has been shown to reduce cortisol levels both in health68 and disease69 pointing to its effect on Hypothalamo-pituitary-adrenal (HPA) axis.
In addition, the roles of yoga on stress mediators that influence metabolic abnormalities related to lipids (adipose tissue that influences atherosclerosis) have been documented. Kiecolt-Glaser et al70 compared adiponectin and leptin levels in well-matched novice (n = 25) and expert yoga practitioners (n = 25) on three different visits. They found that leptin, which plays a pro-inflammatory role, was 36% higher among novices compared to experts and experts' average adiponectin (anti-inflammatory in effect) levels were 28% higher than novices across all three visits. In addition, experts' average adiponectin to leptin ratio was nearly twice that of novices.70 In our study, we observed better reduction in BMI, lipids and diabetic state in the yoga group than those who practiced physical exercise regularly. Thus, we hypothesize that yoga's effects may be mediated through both central and peripheral adaptation mechanisms i.e. stress-reduction and adipokine mechanisms.
4.3. Limitations of the study
(i) Recruitment took longer than expected. (ii) There were about 40% drop outs at the end of one year and hence we could not carry out intention to treat analysis. (iii) As the surgeons were not confident to allow any new intervention for their high risk cases we could not plan to include patients with very low LVEF undergoing CABG. (iv) Only male patients were included in the study as the numbers of female patients were very few. (v) 2D Doppler Echo-cardiogram findings are subjective and may vary from technician to technician. (vi) It would have been valuable to include waist circumference as an index of central obesity along with the weight and BMI which may be considered in future studies.
4.4. Strengths of this study
(i) This is the first randomized control study that incorporated integrated yoga program starting from the day before CABG surgery and had regular follow up of a comprehensive battery of measurements for one year; (ii) The sample size was good and the hospital follows an internationally accepted protocol for surgery and cardiac rehabilitation; (iii) Well matched active intervention with equal attention to both groups during the entire period of follow up; (iv) Results pointing to better efficacy of YLSP than PTLSP; (v) 12.5% increase in LVEF after one year in those with high risk (low EF) and other risk factors.
5. Conclusion
Integrated yoga based cardiac rehabilitation for one year after uncomplicated CABG normalizes risk factors including LVEF, BMI, Blood glucose and Lipids which may be attributed to improvement in positive affect, decrease in stress, anxiety, depression and negative affect. Continued follow up of these cases is planned.
5.1. Recommendations
We recommend that these yoga modules be incorporated in all post-CABG cardiac rehabilitation programs for better in-hospital outcome and long term prognosis.
5.2. Suggestions for future work
(i) We recommend similar studies to be designed in other parts of India and the World to establish the generalizability of this intervention of this three tier module of YLSP. (ii) Continuous follow up of these patients for longer period. (iii) More studies using subtle instruments to measure myocardial perfusion are necessary to understand the mechanisms.
Conflicts of interest
All authors have none to declare.
Acknowledgments
We are grateful to AYUSH, Ministry of Department of Health and Family Welfare, New Delhi, India, for funding this project. We acknowledge all the cardiologists, cardiac surgeons and echo technicians of NHICSc, Bengaluru for their co-operation. We thank all the therapists, biostatistician and staff of SVYASA for their contribution in conducting the project and writing this manuscript.
References
- 1.Reddy K.S. Cardiovascular diseases in India. World Health Statistics Quarterly. Rapport trimestriel de statistiques sanitaires mondiales. 1992;46:101–107. [PubMed] [Google Scholar]
- 2.Reddy K.S., Shah B., Varghese C., Ramadoss A. Responding to the challenge of chronic diseases in India. Lancet. 2005;366:1744–1749. doi: 10.1016/S0140-6736(05)67343-6. [DOI] [PubMed] [Google Scholar]
- 3.Goel P.K., Bharti B.B., Pandey C.M. A tertiary care hospital-based study of conventional risk factors including lipid profile in proven coronary artery disease. Indian Heart J. 2003;55:234–240. [PubMed] [Google Scholar]
- 4.Haslett C., Chilvers E.R., Boon N.A., Colledge N.R., Hunter J.A. 19th ed. Churchill Livingstone; London: 2004. Davidson's Principles & Practice of Medicine. [Google Scholar]
- 5.Baker R.A., Andrew M.J., Schrader G., Knight J.L. Pre-operative depression and mortality in coronary artery bypass surgery: preliminary findings. ANZ J Surg. 2001;71:130–142. doi: 10.1046/j.1440-1622.2001.02055.x. [DOI] [PubMed] [Google Scholar]
- 6.Blumenthal J.A., Lett H.S., Babyak M.A. Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003 Aug 23;362:604–609. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 7.Kneissl G.D., Reifart N., Fritz U., Baier W., Kaltenbach M. Echocardiographic functional parameters of the left ventricle as a prognostic indicator in coronary heart disease. Versicherungsmedizin. 1990 Jun 1;42:70–77. [PubMed] [Google Scholar]
- 8.Kennedy J.W., Kaiser G.C., Fisher L.D. Clinical and angiographic predictors of operative mortality from the collaborative study in coronary artery surgery (CASS) Circulation. 1981;63:793–802. doi: 10.1161/01.cir.63.4.793. [DOI] [PubMed] [Google Scholar]
- 9.Alderman E.L., Litwin P., Fisher L.D. Results of coronary artery surgery in patients with poor left ventricular function (CASS) Circulation. 1983;68:785–795. doi: 10.1161/01.cir.68.4.785. [DOI] [PubMed] [Google Scholar]
- 10.Mallik S., Krumholz H.M., Lin Z.Q. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005;111:271–277. doi: 10.1161/01.CIR.0000152102.29293.D7. [DOI] [PubMed] [Google Scholar]
- 11.Borowicz L., Royall R., Grega M., Selnes O., Lyketsos C., McKhann G. Depression and cardiac morbidity 5 years after coronary artery bypass surgery. Psychosomatics. 2002;43:464–471. doi: 10.1176/appi.psy.43.6.464. [DOI] [PubMed] [Google Scholar]
- 12.Reid T., Denieffe S., Denny M., McKenna J. Psychosocial interventions for panic disorder after coronary artery bypass graft: a case study. Dimens Crit Care Nurs. 2005;24:165–170. doi: 10.1097/00003465-200507000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Engblom E., Hämäläinen H., Lind J. Quality of life during rehabilitation after coronary artery bypass surgery. Qual Life Res. 1992;1:167–175. doi: 10.1007/BF00635616. [DOI] [PubMed] [Google Scholar]
- 14.Dehdari T., Heidarnia A., Ramezankhani A., Sadeghian S., Ghofranipour F. Effects of progressive muscular relaxation training on quality of life in anxious patients after coronary artery bypass graft surgery. Indian J Med Res. 2009;129:603–608. [PubMed] [Google Scholar]
- 15.Utriyaprasit K., Moore S.M., Chaiseri P. Recovery after coronary artery bypass surgery: effect of an audiotape information programme. J Adv Nurs. 2010;66:1747–1759. doi: 10.1111/j.1365-2648.2010.05334.x. [DOI] [PubMed] [Google Scholar]
- 16.Telles S., Naveen K.V. Yoga for rehabilitation; an overview. Indian J Med Sci. 1997;51:123–127. [PubMed] [Google Scholar]
- 17.Schneider R.H., Staggers F., Alexander C.N. A randomized controlled trial of stress reduction for hypertension in older African Americans. Hypertension. 1995;26:820–827. doi: 10.1161/01.hyp.26.5.820. [DOI] [PubMed] [Google Scholar]
- 18.Alexander C.N., Schneider R.H., Staggers F. A trial of stress reduction for hypertension in older African Americans, II: sex and risk factor subgroup analysis. Hypertension. 1996;28:228–237. doi: 10.1161/01.hyp.28.2.228. [DOI] [PubMed] [Google Scholar]
- 19.Castillo-Richmond A., Schneider R.H., Alexander C.N. Effects of stress reduction on carotid atherosclerosis in hypertensive African Americans. Stroke. 2000;313:568–573. doi: 10.1161/01.str.31.3.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alexander C.N., Barnes V.A., Schneider R.H. A randomized controlled trial of stress reduction on cardiovascular and all-cause mortality in the elderly: results of 8 and 15 year follow-ups. Circulation. 1996;93:629. [Google Scholar]
- 21.Alexander C.N., Robinson P., Orme-Johnson D.W., Schneider R.H., Walton K.G. Effects of transcendental meditation compared to other methods of relaxation and meditation in reducing risk factors, morbidity and mortality. Homeost Health Dis. 1994;35:243–264. [Google Scholar]
- 22.Mahajan A.S., Reddy K.S., Sachdeva U. Lipid profile of coronary risk subjects following yogic lifestyle intervention. Indian Heart J. 1991;51:37–40. [PubMed] [Google Scholar]
- 23.Manchanda S.C., Narang R., Reddy K.S. Retardation of coronary atherosclerosis with yoga lifestyle intervention. J Assoc Physicians India. 2000;48:687–694. [PubMed] [Google Scholar]
- 24.Silberman A., Banthia R., Estay I.S. The effectiveness and efficacy of an intensive cardiac rehabilitation program in 24 sites. Am J Health Promot. 2010;24:260–266. doi: 10.4278/ajhp.24.4.arb. [DOI] [PubMed] [Google Scholar]
- 25.Schulz P., Zimmerman L., Barnason S., Nieveen J. Gender differences in recovery after coronary artery bypass graft surgery. Prog Cardiovasc Nurs. 2005;20:58–64. doi: 10.1111/j.0889-7204.2005.03868.x. [DOI] [PubMed] [Google Scholar]
- 26.Gambhirananda S. Advaita Ashram; Calcutta: 2000. Mandukya Upanishad, with Commentary of Sankaracharya. [Google Scholar]
- 27.Basu R.S. Chaukhamba Sanskrit Pratishthan; Delhi: 2003. Gheranda Samhita. [translation] [Google Scholar]
- 28.Nagarathna R., Nagendra H.R. Swami Vivekananda Yoga Prakashana; Bengaluru: 2002. Yoga for Hypertension & Heart Diseases. [Google Scholar]
- 29.Simpson D.R., Dixon B.G., Bolli P. Effectiveness of multidisciplinary patient counseling in reducing cardiovascular disease risk factors through non-pharmacological intervention: results from the Healthy Heart Program. Can J Cardiol. 2004;20:177–186. [PubMed] [Google Scholar]
- 30.Taimni I.K. The Theosophical Publishing House, Adyar; Chennai: 2001. The Science of Yoga. [10th reprint] [Google Scholar]
- 31.Tapasyananda S. Sri Ramakrishna Math Prakashan, Mylapore; Chennai: 2006. Srimad Bagavad Gita. [Google Scholar]
- 32.Nagendra H.R. Swami Vivekananda Yoga Prakashana; Bengaluru: 2000. Science of Emotion Culture – Bhakti Yoga. [Google Scholar]
- 33.Nagendra H.R. Swami Vivekananda Yoga Prakashana; Bengaluru: 2002. The Path of Intellect – Jnana Yoga. [Google Scholar]
- 34.Leung D.Y., Lam T.H., Chan S.S. Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. 2010;10:513. doi: 10.1186/1471-2458-10-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen S., Kamarck T., Mermelstein R.A. Global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 36.Bjelland I., Dahl A.A., Haug T.T., Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 37.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale – a review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 38.Rodgers J., Martin C.R., Morse R.C., Kendell K., Verrill M. An investigation into the psychometric properties of the hospital anxiety and depression scale in patients with breast cancer. Health Qual Life Outcomes. 2005;14:3–41. doi: 10.1186/1477-7525-3-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative effect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 40.American Society of Echocardiography . 2009. Guidelines and Standards; Recommendations for Use of Echocardiography.http://www.asecho.org/clinical-information/guidelines-standards/#doppler Last accessed 16.01.14. [Google Scholar]
- 41.Varadarajan P., Pai R.G. Prognosis of congestive heart failure in patients with normal versus reduced ejection fractions: results from a cohort of 2258 hospitalized patients. J Card Fail. 2003;9:107–112. doi: 10.1054/jcaf.2003.13. [DOI] [PubMed] [Google Scholar]
- 42.Devereux R.B., Roman M.J., Liu J.E. Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the Strong Heart Study. Am J Cardiol. 2000;86:1090–1096. doi: 10.1016/s0002-9149(00)01165-6. [DOI] [PubMed] [Google Scholar]
- 43.Mahadevan G., Davis R.C., Frenneaux M.P. Left ventricular ejection fraction: are the revised cut-off points for defining systolic dysfunction sufficiently evidence based? Heart. 2008;94:426–428. doi: 10.1136/hrt.2007.123877. [DOI] [PubMed] [Google Scholar]
- 44.Chahal N.S., Lim T.K., Jain P., Chambers J.C., Kooner J.S., Senior R. Population-based reference values for 3D echocardiographic LV volumes and ejection fraction. JACC Cardiovasc Imaging. 2012;5:1191–1197. doi: 10.1016/j.jcmg.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 45.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 46.Kathrotia R.G., Paralikar S.J., Rao P.V., Oommen E.R. Impact of different grades of body mass index on left ventricular structure and function. Indian J Physiol Pharmacol. 2010;54:149–156. [PubMed] [Google Scholar]
- 47.Jolliff J.A., Rees K., Taylor R.S., Thompson D., Oldridge N., Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2000;4:CD001800. doi: 10.1002/14651858.CD001800. [DOI] [PubMed] [Google Scholar]
- 48.Oldenburg B., Martin A., Greenwood J., Bernstein L., Allan R. A controlled trial of a behavioral and educational intervention following coronary artery bypass surgery. J Cardiopulm Rehabil. 1995;15:39–46. doi: 10.1097/00008483-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 49.Detry J.R., Vierendeel I.A., Vanbutsele R.J., Robert A.R. Early short-term intensive cardiac rehabilitation induces positive results as long as one year after the acute coronary event: a prospective one-year controlled study. J Cardiovasc Risk. 2001;8:355–361. doi: 10.1177/174182670100800604. [DOI] [PubMed] [Google Scholar]
- 50.Canver C.C., Heisey D.M., Nichols R.D., Cooler S.D., Kroncke G.M. Long-term survival benefit of internal thoracic artery grafting is negligible in a patient with bad ventricle. J Cardiovasc Surg. 1998;39:57–63. [PubMed] [Google Scholar]
- 51.Swahney R.C., Ramachandra N. Defence Institute of Physiology & Allied Sciences; India: 2000. Coronary Artery Disease (CAD) Regression through Life Style Changes: Vegetarianism, Moderate Exercise, Stress Management through Rajayoga Meditation. [Google Scholar]
- 52.Goodman J.M., Pallandi D.V., Reading J.R., Plyley M.J., Liu P.P., Kavanagh T. Central and peripheral adaptations after 12 weeks of exercise training in post-coronary artery bypass surgery patients. J Cardiopulm Rehabil. 1999;19:144–150. doi: 10.1097/00008483-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 53.Dixhoorn V.J., Duivenvoorden H.J., Staal J.A., Pool J., Verhage F. Cardiac events after myocardial infarction: possible effect of relaxation therapy. Eur Heart J. 1987;8:1210–1214. doi: 10.1093/oxfordjournals.eurheartj.a062194. [DOI] [PubMed] [Google Scholar]
- 54.Mendes R.G., Simões R.P., Costa Fde S. Is applying the same exercise-based inpatient program to normal and reduced left ventricular function patients the best strategy after coronary surgery? A focus on autonomic cardiac response. Disabil Rehabil. 2014;36:155–162. doi: 10.3109/09638288.2013.782362. [DOI] [PubMed] [Google Scholar]
- 55.Vempati R.P., Telles S. Yoga-based guided relaxation reduces sympathetic activity judged from baseline levels. Psychol Rep. 2002;90:487–494. doi: 10.2466/pr0.2002.90.2.487. [DOI] [PubMed] [Google Scholar]
- 56.Michalsen A., Grossman P., Acil A. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Med Sci Monit. 2002;11:555–561. [PubMed] [Google Scholar]
- 57.Brunner E.J., Hemingway H., Walker B.R. Adrenocortical, autonomic, and inflammatory causes of the metabolic syndrome: nested case-control study. Circulation. 2002;106:2659–2665. doi: 10.1161/01.cir.0000038364.26310.bd. [DOI] [PubMed] [Google Scholar]
- 58.Hjemdahl P. Stress and the metabolic syndrome: an interesting but enigmatic association. Circulation. 2002;106:2634–2636. doi: 10.1161/01.cir.0000041502.43564.79. [DOI] [PubMed] [Google Scholar]
- 59.Innes K.E., Bourguignon C., Taylor A.G. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 60.Valentini M., Spezzaferri R., Brambilla G. Complexity of observable psychological distress after surgical myocardial revascularization in male subjects. Ital Heart J Suppl. 2005;6:375–381. [PubMed] [Google Scholar]
- 61.Oxlad M., Stubberfield J., Stuklis R., Edwards J., Wade T.D. Psychological risk factors for cardiac-related hospital readmission within 6 months of coronary artery bypass graft surgery. J Psychosom Res. 2006;61:775–781. doi: 10.1016/j.jpsychores.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 62.Spezzaferri R., Modica M., Racca V. Psychological disorders after coronary artery by-pass surgery: a one-year prospective study. Monaldi Arch Chest Dis. 2009;72:200–205. doi: 10.4081/monaldi.2009.318. [DOI] [PubMed] [Google Scholar]
- 63.O'Rourke A., Lewin B., Whitecross S., Pacey W. The effects of physical exercise training and cardiac education on levels of anxiety and depression in the rehabilitation of coronary artery bypass graft patients. Int Disabil Stud. 1990;12:104–106. doi: 10.3109/03790799009166262. [DOI] [PubMed] [Google Scholar]
- 64.Srivastava R.D., Jain N., Singhal A. Influence of alternate nostril breathing on cardiorespiratory and autonomic functions in healthy young adults. Indian J Physiol Pharmacol. 2005;49:475–483. [PubMed] [Google Scholar]
- 65.Upadhyay D.K., Malhotra V., Sarkar D., Prajapati R. Effect of alternate nostril breathing exercise on cardiorespiratory functions. Nepal Med Coll J. 2008;10:25–27. [PubMed] [Google Scholar]
- 66.Mourya M., Mahajan A.S., Singh N.P., Jain A.K. Effect of slow-and fast-breathing exercises on autonomic functions in patients with essential hypertension. J Altern Complement Med. 2009;15:711–717. doi: 10.1089/acm.2008.0609. [DOI] [PubMed] [Google Scholar]
- 67.Van Eck M., Berkhof H., Nicolson N., Sulon J. The effects of perceived stress, traits, mood states, and stressful daily events on salivary cortisol. Psychosom Med. 1996;58:447–458. doi: 10.1097/00006842-199609000-00007. [DOI] [PubMed] [Google Scholar]
- 68.Kamei T., Toriumi Y., Kimura H., Ohno S., Kumano H., Kimura K. Decrease in serum cortisol during yoga exercise is correlated with alpha wave activation. Percept Mot Skills. 2000;90:1027–1032. doi: 10.2466/pms.2000.90.3.1027. [DOI] [PubMed] [Google Scholar]
- 69.Vadiraja H.S., Raghavendra R.M., Nagarathna R. Effects of a yoga program on cortisol rhythm and mood states in early breast cancer patients undergoing adjuvant radiotherapy: a randomized controlled trial. Integr Cancer Ther. 2009;8:37–46. doi: 10.1177/1534735409331456. [DOI] [PubMed] [Google Scholar]
- 70.Kiecolt-Glaser J.K., Christian L.M., Andridge R. Adiponectin, leptin, and yoga practice. Physiol Behav. 2012;107:809–813. doi: 10.1016/j.physbeh.2012.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]


