Abstract
Evidence‐based clinical examination and assessment of the athlete with hip joint related pain is complex. It requires a systematic approach to properly differentially diagnose competing potential causes of athletic pain generation. An approach with an initial broad focus (and hence use of highly sensitive tests/measures) that then is followed by utilizing more specific tests/measures to pare down this imprecise differential diagnosis list is suggested. Physical assessment measures are then suggested to discern impairments, activity and participation restrictions for athletes with hip‐join related pain, hence guiding the proper treatment approach.
Level of Evidence:
5
Keywords: Athlete, diagnostic accuracy, examination, hip joint
INTRODUCTION
The prevalence of hip pain in the general population is 10%, and increases with age.1 Pain in the hip and groin region in athletes is usually characterised by longstanding symptoms that often do not resolve within 6‐12 months.2,3 Hip and groin pain has been reported to commonly occur in athletes who participate in soccer and ice hockey, and approximately 10‐20% of all injuries in these sports are hip and/or groin injuries.4-6 Pelvis, groin, hip and thigh injuries in sport include multiple, complex and longstanding conditions, causing great frustration among athletes and sports practitioners. Pain in these regions may originate from many anatomical structures such as muscle, tendon, ligament, cartilage or bone. Musculotendinous groin and hamstring injuries are the most frequent injuries, and are especially prevalent problems among different forms of football.7-9 Moreover, the recurrence rates of these injuries are very high, and a major problem during the rehabilitation and return‐to‐sport phase.8
Intra‐articular hip injuries are frequent sources of hip and groin pain in athletes that are not related to the musculotendinous structures around the hip and groin. In elite soccer athletes, intra‐articular hip injuries account for up to 10% of all hip and groin injuries.9 Intra‐articular hip injuries include femoroacetabular impingement (FAI), acetabular labral tear (ALT), chondral injuries and synovitis. Intra‐articular injuries of the hip joint have in recent years been recognised as an important differential diagnose in athletes with hip and groin pain. This is reflected in the 2012 injury‐report from the Australian Football League (AFL), where the incidence of hip related injuries seem to have increased during the last ten years, whereas groin injuries seem to have decreased, which may reflect a better understanding or focus on the contribution of intra‐articular hip injury to groin pain in athletes.8 In clinical situations with signs of synovitis with no sign of any intra‐articular injury this may reflect hip joint overuse and will often tend to resolve fairly quickly. In situations where specific intra‐articular injuries with damage to the labrum/cartilage are present, operative procedures may be necessary, as conservative treatment may not resolve the athlete's pain and/or disability. Furthermore, more serious and severe injury such as high and low energy fractures or pain generated from other anatomical areas such as the pelvis and spine also needs to be considered when examining the athlete with hip problems. Examining athletes with hip and groin pain is therefore complex. Consequently, the purpose of this clinical commentary is to introduce an evidence‐based examination and physical assessment approach for athletes with hip joint‐related pathology.
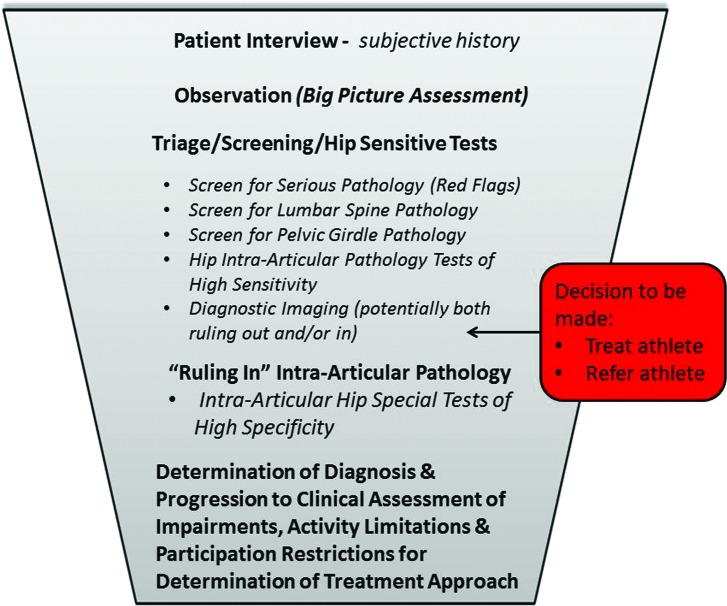
A succinct, systematic approach to clinical examination is always warranted. This is particularly the case for intra‐articular pathology of the hip, which, unfortunately continues to suffer from the lack of high quality evidence support of various examination and testing measures. The approach suggested within this commentary is one of ruling out more medically serious pathology initially, by utilization of highly sensitive tests early in the examination, and narrowing down the differential diagnoses to improve the likelihood of a particular diagnosis (Figure 1). The athlete's history, observations of their movements, clinical examination and diagnostic imaging (components of a systematic examination) each have the ability to affect the identification of the existence of a particular diagnosis. Diagnostic accuracy values for special tests, diagnostic imaging, and occasionally subjective reports include sensitivity (SN), specificity (SP), positive likelihood ratio (+LR), and negative likelihood ratio (−LR). Tests with high SN will be positive for most people who actually have the problem and, therefore, have a low rate of false negatives (the test finding was negative, but the pathology is actually present). When it is important to “not miss” a positive case (such as in a fracture), utilization of tests with high SN is necessary. This is crucial for screening tests in which positive findings simply indicate the need for more investigation. Therefore, the most meaningful finding with a highly sensitive test is a negative finding, since it assists the clinician to rule out a disorder with confidence. A suggested useful acronym is SnNout, meaning a test with high Sn when Negative is used to help rule out the condition.10,11 The potential for false positives (the test is positive, but the pathology is not actually present) exists with highly SN tests. Therefore, these tests, by their nature, are designed to capture several potential competing diagnoses, many of which may be not present (false positive). Again, the purpose of these tests is to not miss a positive case. These tests are therefore utilized early in the examination process to screen for the potential of more serious pathology and/or rule out other potential pain generators. Tests with high SP will be appropriately negative in clients who do not have the disorder and therefore have a low rate of false positives. Tests with high SP are best to rule in a disorder, and should be performed later in the examination to “rule in” the most likely diagnosis/diagnoses from the differential diagnosis list generated by the sensitive tests. The acronym SpPin is often used for these tests. A highly Sp test when Positive is used to help rule in the condition.10,11
Figure 1.
Examination Sequence (Funnel Approach) for Hip‐Joint Related Examination with Progression to Determination of Treatment Approach
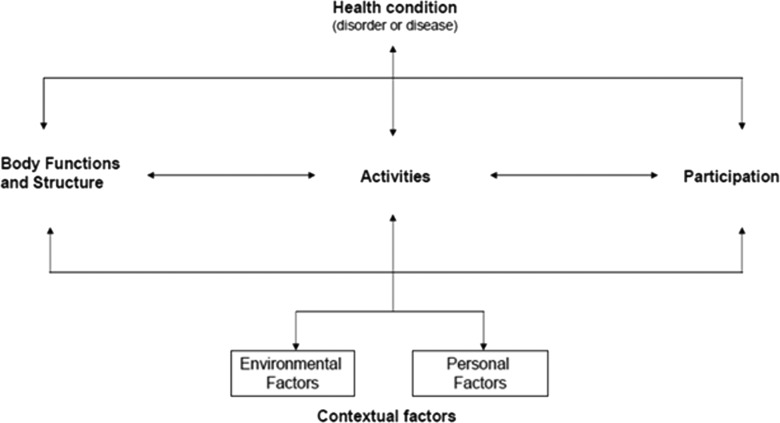
As the clinician systematically reasons through the broad to narrow focused clinical examination sequence (funnel approach) they should be able to reasonably determine a primary diagnosis and/or important differential diagnostic considerations including additional investigations that may be pertinent to proceed to, most notably assessment of specific impairments, activity limitations, and participation restrictions in order to optimize a structured and individualized rehabilitation for the individual athlete. Assessment of outcome and functional ability can be related to body functions and structure (impairments), activities (activity limitations) and participation (participation restrictions) according to the ICF model.12 Environmental factors that interact with all these components are also included. Body functions are physiological functions of body systems (including psychological functions) and body structures are anatomical parts of the body (e.g. organs, limbs and their components). Activities are the execution of a particular task or action by an individual, such as running or kicking, while participation is the involvement in a “real life” situation, such as participating in a game of football. Therefore activity limitations are difficulties an individual may have in executing particular activities, while participation restrictions are problems an individual may experience in involvement in “real life” situations. Environmental factors make up the physical and social environment in which people live and conduct their lives. Personal factors are also included in the model but are not classified (Figure 2).12
Figure 2.
ICF model of disability. Adapted from WHO, 2002.12
CLINICAL EXAMINATION OF THE HIP
It is important to begin the hip examination process as comprehensively as possible (including all potential diagnoses) and (as a result of each systematic step in the examination process) narrow the differential diagnosis list down as far as possible. Additionally, this broad to narrow approach of the hip examination is an approach of general to more isolated examination procedures. For example, in the client interview the clinician asks broad, open‐ended questions that are likely to include multiple potential diagnoses. As the examination continues, the examination process becomes more focused. This is particularly the case after the triage/screening/sensitive tests section that is intended to rule out not only the potential for red flag/non‐musculoskeletal disease processes, but to also rule out potential pain generators in other joints, as well as other potential diagnoses common to the pain generating joint(s). Determination of necessity of referral to a physician is also required at this stage of the examination.
If screening is conclusively negative the clinician then determines that it is appropriate to continue with the rest of the examination process. If screening is not conclusively negative, the clinician is required to make a clinically sound judgment on the appropriateness of referral out to the appropriate medical personnel immediately or whether an attempt at appropriate intervention will assist in determining the athlete's medical status.
Patient Interview ‐ Subjective History
The subjective history has been suggested to be instrumental in determining 56‐90% of diagnoses in various types of patients.13-16 Physical examination components, on the other hand, only contributed to less than 30% of the diagnoses in the same studies.13-16 In fact, it has been suggested that subjective history, physical examination, and radiographic examination each have their own limitations at each stage and an integrative approach is needed in making a medical diagnosis with more emphasis on subjective history.17
Age of the athlete will assist in differential diagnosis of hip pain. Pediatric and adolescent pathologies, such as Legg‐Calve‐Perthes (typical age of onset is 3 to 12 years old) and Slipped Capital Femoral Epiphysis (average age of 12.1 years for girls and 14.4 years for boys) will significantly differ in athlete age compared to acetabular labral tear (ALT) (adolescents to older adults) and hip osteoarthritis/osteoporotic femoral neck fractures (older athletes).
Differential diagnosis with regard to the lumbar spine, pelvis and hip is often difficult due to the inter‐dependent relationship between these three regions.18 A few variables have been shown to demonstrate a strong predilection to hip injury. The presence of a limp, groin pain, or limited internal rotation (IR) of the hip significantly predicted diagnosis of a disorder originating primarily from hip opposed to from the spine.19 Athletes with limp were seven times more likely to have a hip disorder than spine disorder, while those with groin pain were seven times more likely to have hip disorder only or hip and spine disorder versus spine disorder only.19 Limited IR in an athlete was 14 times more likely to suggest a hip disorder only or hip and spine disorder versus spine disorder only.19
Groin pain is a common location for multiple hip pathologies (as well as lumbar spine and pelvic girdle pathologies). Groin and thigh pain was found in 55% and 57% of athletes with hip joint pain, respectively.20 Pain referral was also seen in the buttock and lower extremity distal to the knee in 71% and 22% respectively,20 indicating the possibility of combined lumbar spine and hip pathology. The most common locations of pain for athletes with ALT were the central groin and lateral peritrochanteric area.21 The lack of groin pain presentation helps rule out the potential for ALT/FAI with a SN ranging from 96‐100%.22,23
Complaints of clicking, catching, snapping, etc. should cue the clinician to include ALT, intra‐articular pathology, and snapping hip in the differential diagnosis.24-27 Sharp pain with mechanical symptoms has a reported SN of 100%, and SP of 85% for ALT/intra‐articular pathology.25,28 Carefully delineating the source (and relevance) of such symptoms is imperative in determining a proper diagnosis in the athlete. For example, 91% of ballet dancers reported snapping hip, 60% of them could volitionally produce this snapping, yet only 7% were not able to continue dancing due to the snapping.29
Observation
Observation of the athlete presenting with hip pain should include general postural assessment (both statically and dynamically), gait, transfers, and potential limitations in strength and mobility with daily tasks from both the anterior‐posterior view as well as laterally. Asymmetrical landmarks can alert the clinician to some potential structural dysfunctions that may be contributing to the athlete's hip pain. It is important to recognize that the presence of postural abnormality does not necessarily correlate with dysfunction.
The athlete with joint changes may have complaints with some combination of hip joint positions involving flexion, adduction, and/or internal rotation.25 Pain with these motions is often described as deep in the groin region and indicative of potential intra‐articular involvement.30 Pain posturing on part of the athlete may be seen when sitting in chairs (especially lower level chairs), stepping up with the involved leg, squatting, and so forth as these motions will replicate the combinations of these movements in the hip.
Range‐of‐motion (ROM) of the hip can also be observed without formal assessment. In the supine position, the clinician can generally assess for anterior capsular laxity. If an athlete lying supine with relaxed legs demonstrates enough external rotation to have the lateral border of the foot touch the table, he/she likely has laxity of the anterior capsule31 or hip retroversion. Alternatively, the athlete presenting with very little to no external rotation in this position should heighten the clinician's concern for limited anterior capsular mobility or anteversion.
Limitations in hip ROM can also be assessed with daily activities. Gait on level surfaces requires only 30 to 44° of hip flexion, while ascending and descending stairs requires 45 to 66° of hip flexion.32,33 Sitting in a chair of an average seat height requires 112° of hip flexion. Putting on socks requires 120° flexion, 20° abduction and 20° of external rotation.34 Athletes with FAI were not able to squat as deeply as those without FAI when measured using motion analysis.35 Difficulty performing such daily tasks can alert the clinician as to which particular motions to more closely examine during the motion assessment.
Several hip muscles are active during gait, especially the gluteal muscles. Dysfunction of these muscles (primarily the gluteus medius and minimus) is depicted in an excessive drop of the contralateral (or non‐weight‐bearing “swinging”) side of the pelvis, or Trendelenburg gait pattern.36 Athletes with hip osteoarthritis37 and slipped capital femoral epiphysis,38 have demonstrated this type of gait dysfunction. Athetes with hip dysfunction involving the strength deficits of the gluteus maximus are likely to present with functional deficits during stair climbing, step‐ups, and sit to stand maneuvers since these muscles generate torque in order to propel the upper body of a person upward and forward from a position of hip flexion.36,39
Triage/Screening
Ruling out Serious Pathology ‐ Red Flags
Determining appropriateness for continuation of the examination with or without potential referral to a physician is a question that should be answered early in the examination. Presence of potential serious pathology requires referral to the most appropriate medical professional. The clinician must be aware of disorders affecting the abdominal and pelvic organs that can also refer pain to the hip region, mimicking a musculoskeletal dysfunction. Previous history of cancer, such as prostate cancer in men or any reproductive cancer or breast cancer in a woman is a red flag since these cancers may be associated with metastases to the hip joint.40 Multiple sources of pain and pathology were discovered in a study examining females with groin pain, further suggesting the need for a detailed screen as part of the clinical examination.41 Other red flags of concern with respect to the patient presenting with hip and/or groin pain include a history of trauma, fever, unexplained weight loss, burning with urination, night pain, and prolonged corticosteroid use.42-44
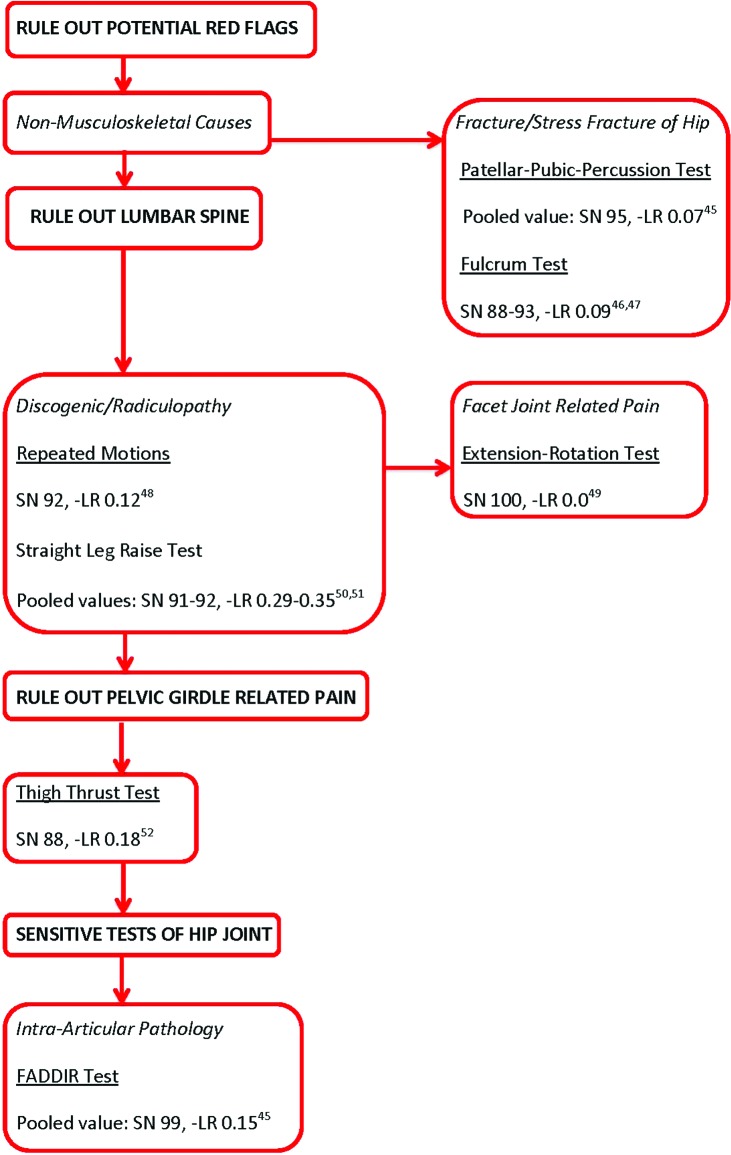
Special testing for potential red flags from non‐musculoskeletal and musculoskeletal related causes (fracture/stress fracture) of the hip should utilize detailed subjective and objective findings. Testing to rule out (highly SN tests) non‐musculoskeletal, serious hip pathology are suggested at this stage in the examination. Figure 3 is the suggested sequence of examination in the triage/screening section of the examination. Table 1 describes the suggested testing for femoral fracture/stress fractures. The patellar‐pubic percussion test alters post‐test probability of a femoral neck fracture not existing to an almost conclusive degree in pooled analysis,45 while the fulcrum test alters post‐test probability of a femoral stress fracture not existing from a very small46 to almost conclusive47 degree10 in two studies of lower quality.
Figure 3.
Algorithm for Hip Pathology Screening in the Athletic Hip. SN=sensitivity, ‐LR=negative likelihood ratio, FADDIR=flexion‐adduction‐internal rotation test
Table 1.
Screening of Serious Pathology Related to the Hip Joint.
| Special Test | Performance | Positive Result |
|---|---|---|
| Fracture/Stress Fracture of the Hip | ||
| Patellar pubic percussion test | The athlete is supine with bilateral legs relaxed. Clinician places stethoscope over pubic tubercle on ipsilateral side of lower extremity being tested. Clinician listens through stethoscope as they tap the ipsilateral patella. Tapping and placing a tuning fork over the patella can also be used in place of tapping the patella directly. | A diminished percussion noted on the side of pain. |
| Stress fracture/fulcrum test | The athlete is sitting on edge of table with bilateral feet off edge. Clinician places one forearm under athlete's thigh to be tested and other hand applies downward pressure to the proximal knee. | Reproduction of athlete's concordant pain. |
Screen for Lumbar Spine and Pelvic Girdle Pathology
Once red flags are ruled out, an efficient way to begin to differentiate the many potential pain referral sources is through the lower quarter screening examination. The traditional lower quarter screen consists of testing of dermatomes, myotomes, deep tendon reflexes, and possible upper motor involvement.
The clinician should also differentially diagnose the potential contribution of the pelvic girdle and lumbar spine as the primary pain generator for the athlete's hip pain. Screening (highly SN) tests for these areas are employed to limit the extent of the differential diagnosis for pathology contributing to the athlete's hip pain (Table 2). Repeated motions almost conclusively alters post‐test probability,10 while straight leg raise only to a small degree assists with ruling out the existence of discogenic/radiculopathy pathology10 in two pooled analyses.50,51 Facet joint pathology is almost conclusively ruled out10 with the seated extension‐rotation test according to two studies49,53 of low bias.54
Table 2.
Special Tests for Ruling out Lumbar Spine and Pelvic Girdle Contributions to Hip pain.
| Special Test | Performance | Positive Result |
|---|---|---|
| Lumbar Spine Radiculopathy | ||
| Repeated Motion | The athlete is standing (loaded spine) or prone/supine (unloaded spine). Athlete is asked to perform repeated flexion and extension motions of the lumbar spine. May also require repeated side‐bending. | Repeated motion in one direction causes pain to centralize (move to the center of the spine) and repeated motion in another direction causes pain to peripheralize (move further down the involved leg). |
| Straight Leg Raise Test | The athlete is supine with legs relaxed. Clinician passively flexes, slightly adducts and internally rotates leg to be assessed while maintaining knee in extension. | Reproduction of athlete's concordant pain that is relieved by decreasing hip flexion, but then increased by passive head/neck flexion |
| Lumbar Spine Facet Joint Dysfunction | ||
| Seated Extension‐Rotation | The athlete is seated as clinician stabilizes their sacrum as athlete moves into end‐range lumbar spine extension and rotation. If no pain, clinician can provide overpressure into further extension and rotation motion. | Reproduction of athlete's concordant pain either with active motion or passive overpressure. |
| SI Joint Dysfunction | ||
| Thigh Thrust Test | The clinician places their caudal hand under the sacrum of the supine athlete and flexes the side to be assessed to 90° hip flexion. The clinician provides longitudinal load force through the femur for up to 30 seconds; if no pain 3‐5 thrusts can be implemented. | Reproduction of athlete's concordant pain either with longitudinal overpressure load or thrust(s). |
Intra‐Articular Hip Pathology Special Tests of High Sensitivity
Once serious pathology and the lumbar spine/pelvic girdle have been ruled out, the clinician should utilize highly SN hip tests to rule out competing diagnoses, as well as pare down the differential diagnosis of hip pathology (Table 3). The suggested tests/screening examination should focus on the potential presence of intra‐articular pathology. The flexion‐adduction‐internal rotation (FADDIR) test is suggested for the potential determination of intra‐articular pathology not existing (screening ability) as it has strong SN and ‐LR with poor SP and +LR, thereby serving appropriately as a screening test and not a diagnostic test with the ability to alter post‐test probability of ruling out intra‐articular pathology to a moderate degree. The diagnostic ability of this test though only alters post‐test probability of the potential presence of an intra‐articular pathology diagnosis to a very small degree or worse.10
Table 3.
Sensitive Tests for Intra‐Articular Hip Involvement
| Special Test | Performance | Positive Result |
|---|---|---|
| FADDIR Test | Clinician passively moves the supine athlete's leg to approximately 90° of hip and knee flexion. The leg is then passively adducted and internally rotated with overpressure to both motions. | Reproduction of athlete's concordant groin pain. |
Diagnostic Imaging (potentially for both ruling out and/or in)
Diagnostic imaging can also be a worthwhile tool to assist the clinician with both potentially ruling in and ruling out possible intra‐articular pathology. Radiographic examination of the hip joint, like other regions of the body, is dependent on the type of pathology. Not unlike other portions of the examination of the hip joint, the value of diagnostic imaging should be cautioned for some diagnosis, such as developmental hip dysplasia and FAI.55 Several studies have found hip pathological changes in asymptomatic individuals.56-59 Therefore, diagnosis made solely on diagnostic imaging interpretation is not advisable in clinical practice.
Radiographs
Anterior‐posterior (AP) and lateral (axial “frog leg”) views are the standard views utilized in plain film radiographs. As with all extremity joints comparison between sides is necessary. Assessment of particular aspects on the AP view includes:
Hip dislocations and most fractures are often seen on AP and lateral views.
An AP view with the hip internally rotated provides a necessary view of the femoral neck in those athletes in whom femoral neck fractures are suspected but standard radiographic findings are negative.
Neck‐shaft angle: An abnormal head neck offset (or pistol grip deformity) can be seen on these views.
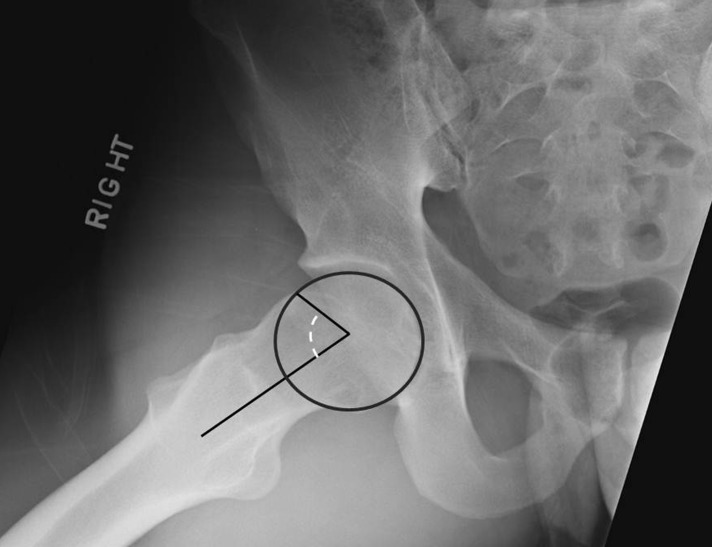
Alpha angle: a parameter typically measured with an AP or Dunn view (Figure 4) used to quantify the degree of femoral deformity and reflects the insufficient anterolateral head‐neck offset and femoral head asphericity.60 Alpha angles greater than 55‐60° have been suggested to be associated with symptomatic impingement,60,61 although recent findings have suggested much higher values to discriminate between subjects with pathology and controls.62 A larger than normal alpha angle is associated with CAM morphology (not necessarily symptomatic CAM pathology).
Cross‐Over Sign: a cross‐over sign on the AP view is where a portion of the anterior wall of the acetabulum (dashed white line on Figure 5) projects further laterally, or “crosses over” the posterior wall (solid black line on Figure 5). This sign is associated with pincer morphology of the hip.
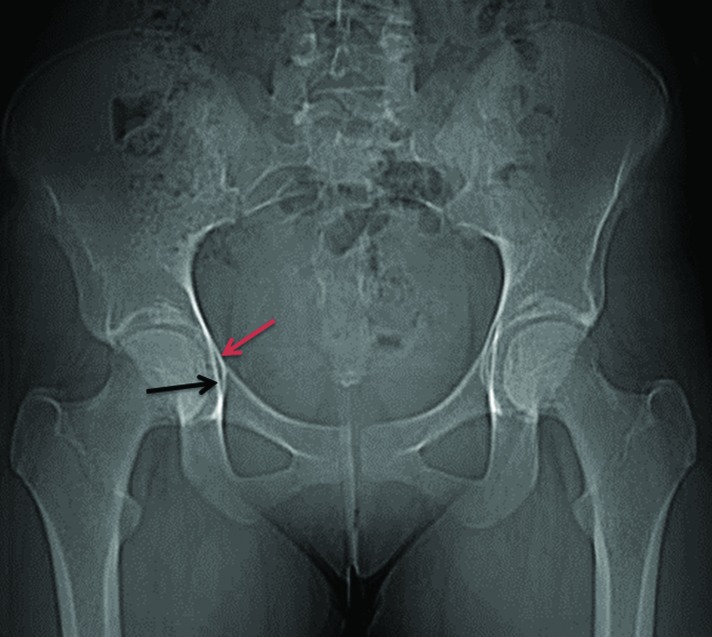
Femoral head and acetabulum orientation: assessment for acetabular dysplasia, acetabular protrusio (acetabular overcoverage). Coxa profunda is the medialization of the medial wall of the acetabulum (red arrow in Figure 6) past the ilioischial line (black arrow in Figure 6) while acetabular protrusio is when the medial most femoral head overlaps the ilioischial line.63
Neck‐shaft angle: assessment for coxa vara or coxa valga.
Joint space width and osteophytes for assessment of osteoarthritis.
Bone disease such as bony cysts (suggestive of OA), tumors, Legg‐Calve‐Perthes disease.
Figure 4.
Dunn lateral radiograph demonstrating α angle.
Figure 5.
Crossover sign
Figure 6.
Anteroposterior pelvic radiograph demonstrating coxa profunda.
Lateral view radiograph: this view is performed with the athlete's hip flexed, abducted, and externally rotated while they are lying supine. This view allows for the capability to view for any possible pelvic obliquity or slipped capital femoral epiphysis. Children with suggestive groin symptoms should have hip AP and frog‐leg lateral radiographs to rule out slipped capital femoral epiphysis.64
Measures of joint space, the maximum thickness of subchondral sclerosis, and the size of the largest osteophyte have been utilized to diagnose hip OA with radiographs. Minimal joint space (i.e., the shortest distance between the femoral head margin and the acetabulum) was the index most strongly associated with other radiologic features of OA.64
The diagnostic accuracy of radiography is much better for fractures, especially of the proximal femur (SN 90‐95%/SP 68‐100%)65 than for other pathologies of the hip, particularly FAI. Furthermore, radiography of the hip has shown limited reliability,55,66,67 meaning that disagreement between even experienced raters is not unusual.
Magnetic Resonance Imaging (MRI)
Both soft tissue (e.g. tendon, labral, and bursal lesions) and osseous tissue (e.g. stress fractures and osteonecrosis) can reliably be assessed with MRI. Since MRI is more SN to bone marrow edema, it is often used to assess subtle occult fractures and diagnosis such as sports related groin pain, pubic bone marrow edema and/or bone stress injuries of the pubis bone.68 Combining arthrography [magnetic resonance arthrography (MRA)] has recently been shown to be both more SN and SP for the diagnosis of hip pathological lesions such as ALTs than MRI,69 although less SN and SP for diagnosis such as gluteal tendinopathy.70
For imaging of intra‐articular hip pathology, MRI/MRA represents the best technique because it enables clinicians to directly visualize cartilage, it provides superior soft tissue contrast, and it offers the prospect of multidimensional imaging. However, opinions differ on the diagnostic efficacy of MRI/MRA and on the question of which MRI/MRA technique is most appropriate.71
Diagnostic accuracy pooled analysis for FAI assessment with MRI revealed SN of 66% and SP of 79% while MRA pooled analysis was 91% SN and 80% SP.69 Pooled analysis for detection of articular cartilage lesions in the hip was SN 59% and SP 94%.72 The most recent diagnostic accuracy values for MRI for gluteal tendon tear range from 33‐100% SN and 92‐100% SP.70 Also, similar to radiographs, MRI/MRA, have shown some limitations in inter‐rater reliability.73
Computed Tomography (CT)
These scans are traditionally utilized for acetabular wall and femoral head fractures, as well as the more subtle hip dislocations. The assessment of osseous abnormalities, such as shape and size of the femoral head (as in a bony exostosis for cam impingement) and acetabulum, anteversion and retroversion measurements are important uses of CT scan.
Computed tomography generally shows stronger diagnostic accuracy for FAI and ALT (SN 92‐97%, SP 87‐100%)74,75 than detection of articular cartilage lesions (SN 88%, SP 82%).74 As with radiographs and MRI/MRA,56,76 findings of abnormalities in asymptomatic individuals57 require caution in diagnostic interpretation of CT findings in the hip joint. Additional radiation exposure is also a concern of CT.
Diagnostic Ultrasonography (US)
An advantage of US is that it does not involve radiation. It is typically used for the assessment of muscle and tendon pathology in the hip,70 although it has also been suggested for its diagnostic utility of various other soft‐tissue hip and lower extremity pathologies.77 Ultrasonography has even been suggested for the use of screening for developmental hip dysplasia,78 although a recent systematic review cautions its use in this manner due to weak evidence support for this clinical utility of US.79 Generally, the clinical value of US has not been widely investigated scientifically in relation to hip and groin injuries in athletes, although many clinicians use this modality in their examination.80,81
The diagnostic accuracy of US for ALT (SN 82%, SP 60%)82 is not equal to that of other utilized modalities such as MRI/MRA and CT. Additionally, although suggested for tendon assessment, limitations in diagnostic accuracy (SN 61%, SP 100%) seem to exist.83
Bone Scan (Scintigraphy)
Bone scans are typically utilized to help diagnosis tumors, necrosis and stress fractures of the hip. This is particularly the case with proximal femoral (femoral neck and inter‐trochanteric) fractures (SN 91%, SP 100%).84
Intra‐articular Joint Injection
Several authors have documented the diagnostic usefulness of an intra‐articular hip injection in order to identify intra‐articular hip abnormalities85,86 although having stronger SN (85%) than SP (26%).87 These injections are supported much more strongly as a better determinant of those athletes less likely to do well with surgical correction of FAI.87
“Ruling In” Intra‐Articular Pathology
The use of SP clinical special tests, along with diagnostic imaging as outlined previously, is suggested at this point in the examination to rule in the particular hip joint pathology. The clinician is cautioned regarding study findings suggesting limitations in the clinical applicability of many hip special tests.45,88-91 Clinical special tests are a very small component of the overall orthopedic/sports examination. Reliance of findings on special testing alone is unsatisfactory clinical practice. The recommended tests, description of their performance and diagnostic accuracy are outlined in Table 4 & 5.
TABLE 4.
Description of Suggested Special Tests for Hip Joint Ligamentous Laxity.
| Special Test | Performance | Positive Result | Interpretation |
|---|---|---|---|
| Dial Test | Athlete supine with the hip in a neutral flexion/extension and abduction/adduction position, the clinician grasps the client's leg at the femur and tibia and passively rolls it into full IR. The LE is released and allowed to ER. | A negative Dial test constitutes ER of the lower limb less than 45°, as measured vertically, with a firm endpoint. | No reliability or diagnostic validity has been reported for this test |
| Log Roll Test | Athlete supine with hip in a neutral flexion/extension and abduction/adduction position, the leg is passively rolled into full IR and ER. | A click reproduced during the test is suggestive of labral tear, while increased ER ROM may indicate iliofemoral ligament laxity. | Inter‐rater reliability: ICC = 0.63;92 ĸ = 0.6193 Good reliability; No diagnostic validity has been reported for this test |
ER=external rotation, IR=internal rotation, ĸ=kappa statistic for reliability
TABLE 5.
Description of Suggested Special Tests for Intra‐Articular Pathology.
| Special Test | Performance | Positive Result | Interpretation |
|---|---|---|---|
| Ligamentum Teres Tear Test | Clinician passively flexes hip fully, then extends 30°, leaving the hip at about 70° flexion (knee is flexed 90°). The hip is then abducted fully and then adducted 30°, typically leaving it at about 30° abduction. The leg is then passively internally and externally rotated to available end‐range. | Reproduction of concordant pain with either internal or external rotation. | SN 90%, ‐LR 0.11; SP 85%, +LR 6.594 Both a (‐) and (+) test alters post‐test probability of a ligamentum teres tear not existing/existing to a moderate degree in one high quality study. |
| Thomas Test | The athlete sits at the edge of the plinth. The athlete is then instructed to lie back, pulling both knees to his or her chest. One knee (the asymptomatic side) is held to the chest and the other is slowly lowered into extension of the hip by the clinician. The knee is allowed to extend. Internal and external rotation of the leg has also been suggested. | Reproduction of athlete's concordant pain with/without a click. | SN 89%, −LR 0.12, SP 92%, +LR 11.123 A (‐) test alters post‐test probability of ALT not existing to a moderate degree, while a (+) test alters post‐test probability of ALT existing to an almost conclusive degree with one high quality study. |
PHYSICAL ASSESSMENT OF THE HIP (IMPAIRMENTS, ACTIVITY LIMITATIONS & PARTICIPATION RESTRICTIONS)
As mentioned previously, the tests included in the physical examination are not specifically aimed for establishing the athlete's diagnosis of intra‐articular hip pain, but are extremely valuable in guiding the establishment of the treatment plan. While there are some correlative findings of these impairments in particular intra‐articular pathologies, their diagnostic value is often limited.95-97
Motion tests (AROM, PROM, Accessory Motions, & Flexibility)
Motion and strength testing of the hip joint currently suffers from inconclusive findings in those with impairments in many instances. As such, it has been recommended these findings should be interpreted with caution.96 These findings again underlie the importance of a comprehensive examination when assessing the athlete for hip pain. The hip joint motion assessment characteristics are listed in Table 6.
Table 6.
Hip Joint Motion Assessment Properties.
| Joint | Closed Packed Position | Resting Position | Capsular Pattern | ROM Norms | End Feel |
|---|---|---|---|---|---|
| Femoral‐acetabular | Full extension, abuction, internal rotation | 30° flexion, 30° abduction, slight external rotation | Flexion, abduction, internal rotation | Flexion: 140° with knee flexed Extension: 20° Internal rotation: 45° External rotation: 45° Abduction: 40° Adduction: 25° |
Firm for all motions |
Patterns of lower extremity ROM deficits are often noticed in athletes with FAI and ALT. Most notably, athletes tend to exhibit reduced hip motions of flexion, internal/external rotation, and/or abduction,28,98-101 although abduction was the only significant restriction in a recent higher quality study.97
Additionally, since the greatest strain on the labrum occurs in the position of hip flexion and adduction,102 assessment of hip joint mobility is suggested. Hip anterior‐posterior glide (motions of hip flexion and internal rotation) and lateral glide (hip adduction) should be assessed.103,104
Functional limitations can be correlated with hip ROM limitations. Hip flexion ROM was shown to explain up to 95% of variance in the star excursion balance test (SEBT) performance.105
Muscle testing
Hip strength assessment plays an important role in clinical examination of the hip and groin region, and clinical outcome measures quantifying hip muscle strength are needed.106 Decreased muscle strength seems to be a consistent finding in athletes with hip and groin pathology.107,108 Manual muscle testing (MMT) is often used. The advantage of MMT is that no equipment is necessary. However, MMT has certain limitations when testing patients stronger than a grade 3 (able to raise body segment against gravity). In a classic study performed in 1956, Beasley showed that muscle‐strength deficits up to 50%, assessed by quantitative measurement methods (dynamometer), could not be identified by MMT.109
In athletes with longstanding groin pain, a subjective manual assessment method during hip muscle testing by Hölmich et al has also been proposed.106 This method divides muscle strength into one of three levels; weak, intermediate and strong. Kappa values of the intra‐observer reliability of this procedure ranged from 0.58‐0.72, and the kappa values of the inter‐observer reliability ranges from 0‐0.22, indicating that the procedure is observer‐dependable.106 As with the 0‐5 assessment method, this kind of scale may be able to distinguish between weak and strong patients, but cannot quantify degrees of strength or weakness.
The squeeze test has recently been introduced which quantifies adduction strength by using the cuff of a sphygmomanometer placed between the athlete's knees with the instruction to squeeze the cuff as hard as they can using both legs. The highest pressure displayed on the sphygmomanometer dial (to the nearest 5 mmHg) during the test is then recorded. Malliaris et al, showed that athletes with groin pain had reduced hip adduction pressure (force) in the squeeze test of approximately 20%, compared to healthy controls.107 However, when applying the squeeze test the measured pressure is produced by hip adduction of both legs. By introducing a hand‐held dynamometer, a testing method that can be used for each leg individually, it would be possible to achieve a greater depiction of the actual muscle strength in hip adduction in both the injured and uninjured limb; therefore, a unilateral and reliable quantitative strength assessment method seems warranted for athletes with hip and groin pain.108 The hand‐held dynamometer (HHD) is a quantitative strength measurement method that has been used since the 1940's. It is a portable measurement device that has been shown to be reliable in assessing hip muscle strength.110
HHD using eccentric strength testing (break testing) has generally shown greater strength values than isometric testing (make testing),111,112 about the hip,108 but a high correlation exists between the two types of tests (contraction types).111,113 This means that the make and break test presumably measure the same construct (maximal voluntary strength), just under different conditions. Both tests have clinical advantages and disadvantages that should be considered before use. An advantage of the make test is that isometric loading induces less stress to the musculoskeletal system than eccentric loading, thus minimising the risk of injury and delayed‐onset muscle soreness.114,115 In situations in clinical practice where eccentric testing is not feasible due to the pathological state of the athlete, isometric testing should be preferred.
Strength data obtained by HHD can be used clinically in different ways. One possibility is to use normative values. However, normative values do not often exist for different age groups and levels of physical activity, and is therefore not always an option.116 Another possibility is to use the unaffected limb as a control. A lower limb symmetry index (LSI) can then be calculated by dividing the strength of the affected limb by the unaffected limb. Generally, it has been suggested that leg strength deficits of less than 10% on the injured side compared to the uninjured side should be considered the clinical milestone before returning an athlete to sport following an injury.117,118 However, Thorborg et al showed that eccentric hip adduction symmetry cannot be assumed in injury‐free soccer players.7,119 In fact, the dominant side was 14% stronger than the non‐dominant side with regards to eccentric hip adduction strength, although hip abduction strength was similar.119 This finding of asymmetric eccentric hip adduction strength in injury‐free soccer players, between the dominant and non‐dominant leg, indicates that using contralateral eccentric hip adduction strength as a reference‐point for hip adductor muscle recovery may be questionable.119
Hip muscle performance deficits have been demonstrated in athletes with symptomatic FAI,120 as well as osteoarthritis.121 Athletes with symptomatic FAI have demonstrated hip muscle weakness and an impaired ability to produce maximal hip strength when compared to healthy controls.120 Additionally, gluteus medius and maximus muscle weakness37,121,122 and atrophy121,123,124 have been correlated with hip joint osteoarthritis.
Physical performance measures
Physical performance measures (PPMs) of the hip joint are applicable to the lumbar spine/pelvis and lower extremities. A recent systematic review125 supports the use of the single‐leg stance, single‐leg squat, and the Star Excursion Balance Test (SEBT) for athletes with hip pathology. Athletes with FAI had decreased mean peak squat depth compared to controls, suggesting that maximal squat depth is a potentially valid measure of assessment for FAI.35 The SEBT, a purported measure of balance, range‐of‐motion, and muscle performance,105,126,127 recruited the gluteus medius at 49% of maximal volitional isometric contraction with a medial reach.128 The single‐leg squat also demonstrated a relationship to hip abductor function.129 Dysfunction in any of these PPMs should alert the clinician to perform measures previously discussed (motion tests, muscle performance tests, and so on).
Normative and discriminatory values for involved to non‐involved lower extremities on various hop, speed and agility tests have been reported.130 Most of these tests are reported for either normative values or on knee and ankle pathologies. The reliability of these measures specifically for hip dysfunction has not been established.
The “Sport Test” has been advocated by Wahoff et al to objectively assess an athlete's readiness to return to sport following hip arthroscopy.131 Rather than measuring isolated movements, it analyzes an individual's coordinated movement patterns and power of an involved extremity. The Sport Test includes single knee bends, side‐to‐side lateral movement, diagonal side‐to‐side movement, and forward box lunges. Athletes must score 17/20 or higher to pass each of the four components of the test.131 Although the application of this test on those with ALT has not been investigated, it seems plausible that this test could function as an advanced assessment of sport‐related ability for those athletes with ALT since it replicates most components of sporting activity. However, it is worth noting, that there is a lack of diagnostic accuracy/prediction of the use of the Sport Test in relation to return to sport.
Patient‐reported outcome measures (PROs)
Investigation of the most traditional hip PROs for hip arthroscopy athletes suggest that the Non‐arthritic Hip Score (NAHS), the Hip Outcome Score (HOS), and the modified Harris Hip Score (mHHS) are commonly used for patients who have undergone hip arthroscopy.132,133 The NAHS was the only PRO with content validity, while the HOS scored best on agreement, internal consistency, and responsiveness, of these three PROs.132,133
However, recently newer and more promising PROs have been developed for patients with hip and groin problems. The 33‐item International Hip Outcome Tool (iHOT‐33) has been developed for hip related problems in younger patients. This questionnaire uses a visual analog scale response format designed for computer self‐administration by young, active athletes with hip pathology. The iHOT‐33 has been shown to be reliable, has demonstrated face, content, and construct validity, and is highly responsive to clinical change.134 Furthermore, a short version of the International Hip Outcome Tool (iHOT‐12) has been developed. It has very similar characteristics to the original rigorously validated 33‐item questionnaire, losing very little information despite being only one‐third the length. It is valid, reliable, and responsive to change. It has been suggested to be used for initial assessment and postoperative follow‐up in routine clinical practice.135
The Copenhagen Hip and Groin Outcome Score (HAGOS) was also recently developed for the assessment of symptoms, activity limitations, participation restrictions and quality of life in physically active, young to middle‐aged athletes with long‐standing hip and/or groin pain.136 The HAGOS consists of six separate subscales assessing pain, symptoms, physical function in daily living, physical function in sport and recreation, participation in physical activities and hip and/or groin‐related quality of life. It is also a valid, reliable, and responsive to change measure.136 HAGOS includes a measure of the athletes’ ability to perform at their usual and optimal pre‐injury level, which is extremely relevant when dealing with athletes with longstanding problems, as their ability to perform is often impaired, even though they have returned to sporting activity.136
Both iHOT and HAGOS have shown to be reliable, valid and responsive measures for patients with hip and/or groin pain. Both of these measures have recently been translated and validated in different languages and by different research groups,135-138 and reference values has been provided in different subgroups for these measures.139,140 So far data from HAGOS indicate that this measures is sensitive to changes in hip and groin pain and functional status, with the ability to discriminate between athletes with and without previous injury.140 Furthermore, substantial disability is more often reported when using iHOT and HAGOS due to the sports specific and patients‐relevant questions asked in these questionnaires compared to the more traditional hip PROs (mHHS and NAHS) where content validity for athletes has never been addressed sufficiently.136 Taken together, this means that athletes often report very few problems in these older PROs due to lack of sports‐specific and more functionally demanding questions.
The tools recommended for use in athletes who have sustained a fracture is limited. The Short Musculoskeletal Function Assessment (SMFA) had good overall responsiveness in athletes with hip fractures and has been recommended for use as one of the measures to evaluate the outcome after a hip fracture.141
SUMMARY
This clinical commentary focuses on an evidence‐based examination and physical assessment of hip joint‐related pathology in athletes. Clinical examination of the athlete with hip pain is a diagnostic challenge requiring a clearly defined approach with sound clinical reasoning. Each component of this approach contributes to the identification of the potential existence/non‐existence of a particular pathology. Furthermore, the athlete's functional ability in relation to important aspects of body functions and structure (impairments), activities (activity limitations) and participation (participation restrictions) is important to identify, in order to optimize and structure and individualized rehabilitation program. The strengths and limitations of each component of the proposed approach vary from athlete to athlete. This systematic, cogent, hip examination and assessment approach must therefore always be individualized to each particular athlete and situation.
REFERENCES
- 1.Picavet HS Schouten JS Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)‐study. Pain. 2003;102(1‐2):167‐178. [DOI] [PubMed] [Google Scholar]
- 2.Fricker PA Taunton JE Ammann W Osteitis pubis in athletes. Infection, inflammation or injury? Sports Med. 1991;12(4):266‐279. [DOI] [PubMed] [Google Scholar]
- 3.van der Waal JM Bot SD Terwee CB van der Windt DA Bouter LM Dekker J The course and prognosis of hip complaints in general practice. Ann. Behav. Med. 2006;31(3):297‐308. [DOI] [PubMed] [Google Scholar]
- 4.Nielsen AB Yde J Epidemiology and traumatology of injuries in soccer. Am. J. Sports Med. 1989;17(6):803‐807. [DOI] [PubMed] [Google Scholar]
- 5.Ekstrand J Hilding J The incidence and differential diagnosis of acute groin injuries in male soccer players. Scand. J. Med. Sci. Sports. 1999;9(2):98‐103. [DOI] [PubMed] [Google Scholar]
- 6.Pettersson M Lorentzon R Ice hockey injuries: a 4‐year prospective study of a Swedish elite ice hockey team. Br. J. Sports Med. 1993;27(4):251‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thorborg K Serner A Petersen J Madsen TM Magnusson P Holmich P Hip adduction and abduction strength profiles in elite soccer players: implications for clinical evaluation of hip adductor muscle recovery after injury. Am. J. Sports Med. 2011;39(1):121‐126. [DOI] [PubMed] [Google Scholar]
- 8.Orchard J, Seward H, Orchard J AFL Injury Report 2012 http://www.afl.com.au/staticfile/AFL%20Tenant/AFL/Files/AFLInjuryReportFor2012.pdf Accessed 5‐29‐14.
- 9.Werner J Hagglund M Walden M Ekstrand J UEFA injury study: a prospective study of hip and groin injuries in professional football over seven consecutive seasons. Br. J. Sports Med. 2009;43(13):1036‐1040. [DOI] [PubMed] [Google Scholar]
- 10.Jaeschke R Guyatt GH Sackett DL Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patientsϿ. The Evidence‐Based Medicine Working Group. JAMA. 1994;271(9):703‐707. [DOI] [PubMed] [Google Scholar]
- 11.Sackett DL Straws SE Richardson WS Rosenberg W Haynes RB Evidence‐Based Medicine: How to Practice and Teach EBM. 2nd ed. London: Harcourt Publishers Limited; 2000. [Google Scholar]
- 12.World Health Organization: Towards a Common Language for Functioning, Disability and Health, ICF. 2002 http://www.who.int/classifications/icf/training/icfbeginnersguide.pdf. Accessed 5‐28‐14.
- 13.Hampton JR Harrison MJ Mitchell JR Prichard JS Seymour C Relative contributions of history‐taking, physical examination, and laboratory investigation to diagnosis and management of medical outpatients. Br Med J. 1975;2(5969):486‐489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peterson MC Holbrook JH Von Hales D Smith NL Staker LV Contributions of the history, physical examination, and laboratory investigation in making medical diagnoses. West J Med. 1992;156(2):163‐165. [PMC free article] [PubMed] [Google Scholar]
- 15.Schmitt BP Kushner MS Wiener SL The diagnostic usefulness of the history of the patient with dyspnea. J Gen Intern Med. 1986;1(6):386‐393. [DOI] [PubMed] [Google Scholar]
- 16.Sandler G Costs of unnecessary tests. Br Med J. 1979;2(6181):21‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roshan M Rao AP A study on relative contributions of the history, physical examination and investigations in making medical diagnosis. J. Assoc. Physicians India. 2000;48(8):771‐775. [PubMed] [Google Scholar]
- 18.Reiman MP Weisbach PC Glynn PE The hips influence on low back pain: a distal link to a proximal problem. J Sport Rehabil. Feb 2009;18(1):24‐32. [DOI] [PubMed] [Google Scholar]
- 19.Brown MD Gomez‐Marin O Brookfield KF Li PS Differential diagnosis of hip disease versus spine disease. Clin Orthop Relat Res. 2004(419):280‐284. [DOI] [PubMed] [Google Scholar]
- 20.Lesher JM Dreyfuss P Hager N Kaplan M Furman M Hip joint pain referral patterns: a descriptive study. Pain Med. 2008;9(1):22‐25. [DOI] [PubMed] [Google Scholar]
- 21.Arnold DR Keene JS Blankenbaker DG Desmet AA Hip pain referral patterns in patients with labral tears: analysis based on intra‐articular anesthetic injections, hip arthroscopy, and a new pain “circle” diagram. Phys Sportsmed. 2011;39(1):29‐35. [DOI] [PubMed] [Google Scholar]
- 22.Keeney JA Peelle MW Jackson J Rubin D Maloney WJ Clohisy JC Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res. 2004(429):163‐169. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy JC Busconi B The role of hip arthroscopy in the diagnosis and treatment of hip disease. Orthopedics. 1995;18(8):753‐756. [DOI] [PubMed] [Google Scholar]
- 24.Byrd JW Snapping hip. Oper Tech Sports Med. 2005;13:303‐308. [Google Scholar]
- 25.Narvani AA Tsiridis E Kendall S Chaudhuri R Thomas P A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg. Sports Traumatol. Arthrosc. 2003;11(6):403‐408. [DOI] [PubMed] [Google Scholar]
- 26.Fitzgerald RH Jr. Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res. 1995(311):60‐68. [PubMed] [Google Scholar]
- 27.Allen WC Cope R Coxa Saltans: The Snapping Hip Revisited. J. Am. Acad. Orthop. Surg. 1995;3(5):303‐308. [DOI] [PubMed] [Google Scholar]
- 28.Burnett RS Della Rocca GJ Prather H Curry M Maloney WJ Clohisy JC Clinical presentation of patients with tears of the acetabular labrum. J. Bone Joint Surg. Am. 2006;88(7):1448‐1457. [DOI] [PubMed] [Google Scholar]
- 29.Winston P Awan R Cassidy JD Bleakney RK Clinical examination and ultrasound of self‐reported snapping hip syndrome in elite ballet dancers. Am. J. Sports Med. 2007;35(1):118‐126. [DOI] [PubMed] [Google Scholar]
- 30.Byrd JW Physical Examination. In: Byrd JW, ed. Operative Hip Arthroscopy. 2nd ed. New York: Springer; 2005. [Google Scholar]
- 31.Philippon MJ Schenker ML Athletic hip injuries and capsular laxity. Operative Tech Orthop. 2005;15:261‐266. [Google Scholar]
- 32.Livingston LA Stevenson JM Olney SJ Stairclimbing kinematics on stairs of differing dimensions. Arch. Phys. Med. Rehabil. 1991;72(6):398‐402. [PubMed] [Google Scholar]
- 33.McFadyen BJ Winter DA An integrated biomechanical analysis of normal stair ascent and descent. J. Biomech. 1988;21(9):733‐744. [DOI] [PubMed] [Google Scholar]
- 34.Magee DJ, ed Orthopedic Physical Assessment, 4th ed. Philadelphia: WB Saunders; 2002. DJ M, ed. Hip. [Google Scholar]
- 35.Lamontagne M Kennedy MJ Beaule PE The effect of cam FAI on hip and pelvic motion during maximum squat. Clin. Orthop. 2009;467(3):645‐650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hurwitz DE Foucher KC Andriacchi TP A new parametric approach for modeling hip forces during gait. J. Biomech. 2003;36(1):113‐119. [DOI] [PubMed] [Google Scholar]
- 37.Youdas JW Madson TJ Hollman JH Usefulness of the Trendelenburg test for identification of patients with hip joint osteoarthritis. Physiother. 2010;26(3):184‐194. [DOI] [PubMed] [Google Scholar]
- 38.Song KM Halliday S Reilly C Keezel W Gait abnormalities following slipped capital femoral epiphysis. J. Pediatr. Orthop. 2004;24(2):148‐155. [DOI] [PubMed] [Google Scholar]
- 39.Arnold AS Salinas S Asakawa DJ Delp SL Accuracy of muscle moment arms estimated from MRI‐based musculoskeletal models of the lower extremity. Comput. Aided Surg. 2000;5(2):108‐119. [DOI] [PubMed] [Google Scholar]
- 40.Henschke N Maher CG Refshauge KM Screening for malignancy in low back pain patients: a systematic review. Eur. Spine J. 2007;16(10):1673‐1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meyers WC Foley DP Garrett WE Lohnes JH Mandlebaum BR Management of severe lower abdominal or inguinal pain in high‐performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am. J. Sports Med. Jan‐Feb 2000;28(1):2‐8. [DOI] [PubMed] [Google Scholar]
- 42.Gabbe BJ Bailey M Cook JL et al. The association between hip and groin injuries in the elite junior football years and injuries sustained during elite senior competition. Br. J. Sports Med. 2010;44(11):799‐802. [DOI] [PubMed] [Google Scholar]
- 43.Leerar PJ Boissonnault W Domholdt E Roddey T Documentation of red flags by physical therapists for patients with low back pain. J Man Manip Ther. 2007;15(1):42‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van den Bruel A Haj‐Hassan T Thompson M Buntinx F Mant D Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: a systematic review. Lancet. 2010;375(9717):834‐845. [DOI] [PubMed] [Google Scholar]
- 45.Reiman MP Goode AP Hegedus EJ Cook CE Wright AA Diagnostic accuracy of clinical tests of the hip: a systematic review with meta‐analysis. Br. J. Sports Med. 2013;47(14):893‐902. [DOI] [PubMed] [Google Scholar]
- 46.Kang L Belcher D Hulstyn MJ Stress fractures of the femoral shaft in women's college lacrosse: a report of seven cases and a review of the literature. Br. J. Sports Med. 2005;39(12):902‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnson AW Weiss CB Jr. Wheeler DL Stress fractures of the femoral shaft in athletes‐‐more common than expected. A new clinical test. Am. J. Sports Med. 1994;22(2):248‐256. [DOI] [PubMed] [Google Scholar]
- 48.Donelson R Aprill C Medcalf R Grant W A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine (Phila Pa 1976). 1997;22(10):1115‐1122. [DOI] [PubMed] [Google Scholar]
- 49.Laslett M Aprill CN McDonald B Oberg B Clinical predictors of lumbar provocation discography: a study of clinical predictors of lumbar provocation discography. Eur. Spine J. 2006;15(10):1473‐1484. [DOI] [PubMed] [Google Scholar]
- 50.van der Windt DA Simons E Riphagen II et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low‐back pain. Cochrane Database Syst Rev. 2010(2):CD007431. [DOI] [PubMed] [Google Scholar]
- 51.Deville WL van der Windt DA Dzaferagic A Bezemer PD Bouter LM The test of Lasegue: systematic review of the accuracy in diagnosing herniated discs. Spine (Phila Pa 1976). 2000;25(9):1140‐1147. [DOI] [PubMed] [Google Scholar]
- 52.Laslett M Aprill CN McDonald B Young SB Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests. Man Ther. 2005;10(3):207‐218. [DOI] [PubMed] [Google Scholar]
- 53.Schwarzer AC Derby R Aprill CN Fortin J Kine G Bogduk N Pain from the lumbar zygapophysial joints: a test of two models. J. Spinal Disord. 1994;7(4):331‐336. [PubMed] [Google Scholar]
- 54.Whiting P Rutjes AW Reitsma JB Bossuyt PM Kleijnen J The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol. 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Clohisy JC Carlisle JC Trousdale R et al. Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res. 2009;467(3):666‐675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Silvis ML Mosher TJ Smetana BS et al. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am. J. Sports Med. 2011;39(4):715‐721. [DOI] [PubMed] [Google Scholar]
- 57.Jung KA Restrepo C Hellman M AbdelSalam H Morrison W Parvizi J The prevalence of cam‐type femoroacetabular deformity in asymptomatic adults. J. Bone Joint Surg. Br. 2011;93(10):1303‐1307. [DOI] [PubMed] [Google Scholar]
- 58.Gerhardt MB Romero AA Silvers HJ Harris DJ Watanabe D Mandelbaum BR The prevalence of radiographic hip abnormalities in elite soccer players. Am. J. Sports Med. 2012;40(3):584‐588. [DOI] [PubMed] [Google Scholar]
- 59.Hartofilakidis G Bardakos NV Babis GC Georgiades G An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J. Bone Joint Surg. Br. 2011;93(5):580‐586. [DOI] [PubMed] [Google Scholar]
- 60.Kassarjian A Hip MR arthrography and femoroacetabular impingement. Semin Musculoskelet Radiol. 2006;10(3):208‐219. [DOI] [PubMed] [Google Scholar]
- 61.Ganz R Parvizi J Beck M Leunig M Notzli H Siebenrock KA Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003(417):112‐120. [DOI] [PubMed] [Google Scholar]
- 62.Kumar R Aggarwal A Femoroacetabular impingement and risk factors: a study of 50 cases. Orthop Surg. 2011;3(4):236‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nepple JJ Lehmann CL Ross JR Schoenecker PL Clohisy JC Coxa profunda is not a useful radiographic parameter for diagnosing pincer‐type femoroacetabular impingement. J. Bone Joint Surg. Am. 2013;95(5):417‐423. [DOI] [PubMed] [Google Scholar]
- 64.Croft P Cooper C Wickham C Coggon D Defining osteoarthritis of the hip for epidemiologic studies. Am. J. Epidemiol. 1990;132(3):514‐522. [DOI] [PubMed] [Google Scholar]
- 65.Rosenberg ZS La Rocca Vieira R Chan SS et al. Bisphosphonate‐related complete atypical subtrochanteric femoral fractures: diagnostic utility of radiography. AJR. Am. J. Roentgenol. 2011;197(4):954‐960. [DOI] [PubMed] [Google Scholar]
- 66.Carlisle JC Zebala LP Shia DS et al. Reliability of various observers in determining common radiographic parameters of adult hip structural anatomy. Iowa Orthop. J. 2011;31:52‐58. [PMC free article] [PubMed] [Google Scholar]
- 67.Konan S Rayan F Haddad FS Is the frog lateral plain radiograph a reliable predictor of the alpha angle in femoroacetabular impingement? J. Bone Joint Surg. Br. 2010;92(1):47‐50. [DOI] [PubMed] [Google Scholar]
- 68.Verrall GM Slavotinek JP Fon GT Incidence of pubic bone marrow oedema in Australian rules football players: relation to groin pain. Br. J. Sports Med. 2001;35(1):28‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith TO Hilton G Toms AP Donell ST Hing CB The diagnostic accuracy of acetabular labral tears using magnetic resonance imaging and magnetic resonance arthrography: a meta‐analysis. Eur. Radiol. 2011;21(4):863‐874. [DOI] [PubMed] [Google Scholar]
- 70.Westacott DJ Minns JI Foguet P The diagnostic accuracy of magnetic resonance imaging and ultrasonography in gluteal tendon tears‐‐a systematic review. Hip int. 2011;21(6):637‐645. [DOI] [PubMed] [Google Scholar]
- 71.Mamisch TC Zilkens C Siebenrock KA Bittersohl B Kim YJ Werlen S Hip MRI and its implications for surgery in osteoarthritis patients. Rheum. Dis. Clin. North Am. 2009;35(3):591‐604. [DOI] [PubMed] [Google Scholar]
- 72.Smith TO Simpson M Ejindu V Hing CB The diagnostic test accuracy of magnetic resonance imaging, magnetic resonance arthrography and computer tomography in the detection of chondral lesions of the hip. Eur J Orthop Surg Traumatol. 2013;23(3):335‐344. [DOI] [PubMed] [Google Scholar]
- 73.Reurink G Jansen SP Bisselink JM Vincken PW Weir A Moen MH Reliability and Validity of Diagnosing Acetabular Labral Lesions with Magnetic Resonance Arthrography. J. Bone Joint Surg. Am. 2012. [DOI] [PubMed] [Google Scholar]
- 74.Nishii T Tanaka H Sugano N Miki H Takao M Yoshikawa H Disorders of acetabular labrum and articular cartilage in hip dysplasia: evaluation using isotropic high‐resolutional CT arthrography with sequential radial reformation. Osteoarthritis Cartilage. 2007;15(3):251‐257. [DOI] [PubMed] [Google Scholar]
- 75.Yamamoto Y Tonotsuka H Ueda T Hamada Y Usefulness of radial contrast‐enhanced computed tomography for the diagnosis of acetabular labrum injury. Arthroscopy. 2007;23(12):1290‐1294. [DOI] [PubMed] [Google Scholar]
- 76.Paajanen H Hermunen H Karonen J Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitis pubis compared to asymptomatic athletes during heavy training. Am. J. Sports Med. 2008;36(1):117‐121. [DOI] [PubMed] [Google Scholar]
- 77.Malanga GA Dentico R Halperin JS Ultrasonography of the hip and lower extremity. Phys. Med. Rehabil. Clin. N. Am. 2010;21(3):533‐547. [DOI] [PubMed] [Google Scholar]
- 78.Shipman SA Helfand M Moyer VA Yawn BP Screening for developmental dysplasia of the hip: a systematic literature review for the US Preventive Services Task Force. Pediatrics. 2006;117(3):e557‐576. [DOI] [PubMed] [Google Scholar]
- 79.Shorter D Hong T Osborn DA Screening programmes for developmental dysplasia of the hip in newborn infants. Cochrane Database Syst Rev. 2011(9):CD004595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Branci S Thorborg K Nielsen MB Holmich P Radiological findings in symphyseal and adductor‐related groin pain in athletes: a critical review of the literature. Br. J. Sports Med. 2013;47(10):611‐619. [DOI] [PubMed] [Google Scholar]
- 81.Jansen JA Mens JM Backx FJ Stam HJ Diagnostics in athletes with long‐standing groin pain. Scand. J. Med. Sci. Sports. 2008;18(6):679‐690. [DOI] [PubMed] [Google Scholar]
- 82.Jin W Kim KI Rhyu KH et al. Sonographic evaluation of anterosuperior hip labral tears with magnetic resonance arthrographic and surgical correlation. J. Ultrasound Med. Mar 2012;31(3):439‐447. [DOI] [PubMed] [Google Scholar]
- 83.Fearon AM Scarvell JM Cook JL Smith PN Does ultrasound correlate with surgical or histologic findings in greater trochanteric pain syndromeϿ. A pilot study. Clin Orthop Relat Res. 2010;468(7):1838‐1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rubin SJ Marquardt JD Gottlieb RH Meyers SP Totterman SM O'Mara RE Magnetic resonance imaging: a cost‐effective alternative to bone scintigraphy in the evaluation of patients with suspected hip fractures. Skeletal Radiol. 1998;27(4):199‐204. [DOI] [PubMed] [Google Scholar]
- 85.Byrd JWT Jones KS Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra‐articular injection in hip arthroscopy patients. Am. J. Sports Med. 2004;32(7):1668‐1674. [DOI] [PubMed] [Google Scholar]
- 86.Kivlan BR Martin RL Sekiya JK Response to diagnostic injection in patients with femoroacetabular impingement, labral tears, chondral lesions, and extra‐articular pathology. Arthroscopy. 2011;27(5):619‐627. [DOI] [PubMed] [Google Scholar]
- 87.Ayeni OR Farrokhyar F Crouch S Chan K Sprague S Bhandari M Pre‐operative intra‐articular hip injection as a predictor of short‐term outcome following arthroscopic management of femoroacetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2014. [DOI] [PubMed] [Google Scholar]
- 88.Leibold MR Huijbregts PA Jensen R Concurrent criterion‐related validity of physical examination tests for hip labral lesions: a systematic review. J Man Manip Ther. 2008;16(2):E24‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Burgess RM Rushton A Wright C Daborn C The validity and accuracy of clinical diagnostic tests used to detect labral pathology of the hip: a systematic review. Man Ther. 2011;16(4):318‐326. [DOI] [PubMed] [Google Scholar]
- 90.Tijssen M van Cingel R Willemsen L de Visser E Diagnostics of femoroacetabular impingement and labral pathology of the hip: a systematic review of the accuracy and validity of physical tests. Arthroscopy. 2012;28(6):860‐871. [DOI] [PubMed] [Google Scholar]
- 91.Reiman MP Mather RC 3rd Hash TW 2nd Cook CE Examination of acetabular labral tear: a continued diagnostic challenge. Br. J. Sports Med. 2013. [DOI] [PubMed] [Google Scholar]
- 92.Martin RL Enseki KR Draovitch P Trapuzzano T Philippon MJ Acetabular labral tears of the hip: examination and diagnostic challenges. J. Orthop. Sports Phys. Ther. 2006;36(7):503‐515. [DOI] [PubMed] [Google Scholar]
- 93.Martin RL Sekiya JK The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J. Orthop. Sports Phys. Ther. 2008;38(2):71‐77. [DOI] [PubMed] [Google Scholar]
- 94.O'Donnell J Economopoulos K Singh P Bates D Pritchard M The Ligamentum Teres Test: A Novel and Effective Test in Diagnosing Tears of the Ligamentum Teres. Am. J. Sports Med. 2013. [DOI] [PubMed] [Google Scholar]
- 95.Reichenbach S Leunig M Werlen S et al. Association between cam‐type deformities and magnetic resonance imaging‐detected structural hip damage: a cross‐sectional study in young men. Arthritis Rheum. 2011;63(12):4023‐4030. [DOI] [PubMed] [Google Scholar]
- 96.Dobson F Choi YM Hall M Hinman RS Clinimetric properties of observer‐assessed impairment tests used to evaluate hip and groin impairments: A systematic review. Arthritis Care Res (Hoboken). 2012;64(10):1565‐1575. [DOI] [PubMed] [Google Scholar]
- 97.Nussbaumer S Leunig M Glatthorn JF Stauffacher S Gerber H Maffiuletti NA Validity and test‐retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord. 2010;11:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Clohisy JC Knaus ER Hunt DM Lesher JM Harris‐Hayes M Prather H Clinical presentation of patients with symptomatic anterior hip impingement. Clin. Orthop. 2009;467(3):638‐644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Prather H Hunt D Fournie A Clohisy JC Early intra‐articular hip disease presenting with posterior pelvic and groin pain. Pm R. 2009;1(9):809‐815. [DOI] [PubMed] [Google Scholar]
- 100.Philippon MJ Maxwell RB Johnston TL Schenker M Briggs KK Clinical presentation of femoroacetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2007;15(8):1041‐1047. [DOI] [PubMed] [Google Scholar]
- 101.Song Y Ito H Kourtis L Safran MR Carter DR Giori NJ Articular cartilage friction increases in hip joints after the removal of acetabular labrum. J. Biomech. 2012;45(3):524‐530. [DOI] [PubMed] [Google Scholar]
- 102.Safran MR Giordano G Lindsey DP et al. Strains across the acetabular labrum during hip motion: a cadaveric model. Am. J. Sports Med. 2011;39 Suppl:92S‐102S. [DOI] [PubMed] [Google Scholar]
- 103.Neumann DA Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation. 2nd ed. St Louis: Mosby Elsevier; 2010. [Google Scholar]
- 104.Cook CE Orthopedic Manual Therapy: An Evidence Based Approach. 2nd ed. Upper Saddle River, New Jersey: Pearson Education, Inc; 2012. [Google Scholar]
- 105.Robinson R Gribble P Kinematic predictors of performance on the Star Excursion Balance Test. J Sport Rehabil. 2008;17(4):347‐357. [DOI] [PubMed] [Google Scholar]
- 106.Holmich P Holmich LR Bjerg AM Clinical examination of athletes with groin pain: an intraobserver and interobserver reliability study. Br. J. Sports Med. 2004;38(4):446‐451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Malliaras P Hogan A Nawrocki A Crossley K Schache A Hip flexibility and strength measures: reliability and association with athletic groin pain. Br. J. Sports Med. 2009;43(10):739‐744. [DOI] [PubMed] [Google Scholar]
- 108.Thorborg K Branci S Nielsen MP Tang L Nielsen MB Holmich P Eccentric and isometric hip‐adduction strength in soccer players with and without adductor‐related groin pain. An assessor‐blinded comparison. Orthopedic Journal of Sportsmedicine 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Beasley WC Influence of method on estimates of normal knee extensor force among normal and postpolio children. Phys Ther Rev. 1956;36(1):21‐41. [DOI] [PubMed] [Google Scholar]
- 110.Thorborg K Petersen J Magnusson SP Holmich P Clinical assessment of hip strength using a hand‐held dynamometer is reliable. Scand. J. Med. Sci. Sports. 2010;20(3):493‐501. [DOI] [PubMed] [Google Scholar]
- 111.Stratford PW Balsor BE A comparison of make and break tests using a hand‐held dynamometer and the Kin‐Com. J. Orthop. Sports Phys. Ther. 1994;19(1):28‐32. [DOI] [PubMed] [Google Scholar]
- 112.Bohannon RW Make tests and break tests of elbow flexor muscle strength. Phys. Ther. 1988;68(2):193‐194. [DOI] [PubMed] [Google Scholar]
- 113.Bohannon RW Hand‐held compared with isokinetic dynamometry for measurement of static knee extension torque (parallel reliability of dynamometers). Clin. Phys. Physiol. Meas. 1990;11(3):217‐222. [DOI] [PubMed] [Google Scholar]
- 114.Friden J Sjostrom M Ekblom B Myofibrillar damage following intense eccentric exercise in man. Int. J. Sports Med. 1983;4(3):170‐176. [DOI] [PubMed] [Google Scholar]
- 115.Friden J Sfakianos PN Hargens AR Muscle soreness and intramuscular fluid pressure: comparison between eccentric and concentric load. J Appl Physiol (1985). 1986;61(6):2175‐2179. [DOI] [PubMed] [Google Scholar]
- 116.Ramskov D Pedersen MB Kastrup K et al. Normative values of eccentric hip abduction strength in novice runners: an equation adjusting for age and gender. Int J Sports Phys Ther. 2014;9(1):68‐75. [PMC free article] [PubMed] [Google Scholar]
- 117.Augustsson J Thomee R Karlsson J Ability of a new hop test to determine functional deficits after anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2004;12(5):350‐356. [DOI] [PubMed] [Google Scholar]
- 118.Orchard J Best TM Verrall GM Return to play following muscle strains. Clin. J. Sport Med. 2005;15(6):436‐441. [DOI] [PubMed] [Google Scholar]
- 119.Thorborg K Couppe C Petersen J Magnusson SP Holmich P Eccentric hip adduction and abduction strength in elite soccer players and matched controls: a cross‐sectional study. Br. J. Sports Med. 2011;45(1):10‐13. [DOI] [PubMed] [Google Scholar]
- 120.Casartelli NC Maffiuletti NA Item‐Glatthorn JF et al. Hip muscle weakness in patients with symptomatic femoroacetabular impingement. Osteoarthritis Cartilage. 2011;19(7):816‐821. [DOI] [PubMed] [Google Scholar]
- 121.Loureiro A Mills PM Barrett RS Muscle weakness in hip osteoarthritis: A systematic review. Arthritis Care Res (Hoboken). 2012. [DOI] [PubMed] [Google Scholar]
- 122.Grimaldi A Assessing lateral stability of the hip and pelvis. Man Ther. 2011;16(1):26‐32. [DOI] [PubMed] [Google Scholar]
- 123.Grimaldi A Richardson C Durbridge G Donnelly W Darnell R Hides J The association between degenerative hip joint pathology and size of the gluteus maximus and tensor fascia lata muscles. Man Ther. 2009;14(6):611‐617. [DOI] [PubMed] [Google Scholar]
- 124.Grimaldi A Richardson C Stanton W Durbridge G Donnelly W Hides J The association between degenerative hip joint pathology and size of the gluteus medius, gluteus minimus and piriformis muscles. Man Ther. 2009;14(6):605‐610. [DOI] [PubMed] [Google Scholar]
- 125.Kivlan BR Martin RL Functional performance testing of the hip in athletes. A systematic review for reliability and validity. Int J Sports Phys Ther. 2012;7(4):402‐412. [PMC free article] [PubMed] [Google Scholar]
- 126.Plisky PJ Rauh MJ Kaminski TW Underwood FB Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J. Orthop. Sports Phys. Ther. 2006;36(12):911‐919. [DOI] [PubMed] [Google Scholar]
- 127.Hubbard TJ Kramer LC Denegar CR Hertel J Correlations among multiple measures of functional and mechanical instability in subjects with chronic ankle instability. J Athl Train. Jul‐2007;42(3):361‐366. [PMC free article] [PubMed] [Google Scholar]
- 128.Norris B Trudelle‐Jackson E Hip‐ and thigh‐muscle activation during the star excursion balance test. J Sport Rehabil. 2011;20(4):428‐441. [DOI] [PubMed] [Google Scholar]
- 129.Crossley KM Zhang WJ Schache AG Bryant A Cowan SM Performance on the single‐leg squat task indicates hip abductor muscle function. Am. J. Sports Med. 2011;39(4):866‐873. [DOI] [PubMed] [Google Scholar]
- 130.Reiman MP Manske RC Functional Testing in Human Performance. Champaign, IL.: Human Kinetics; 2009. [Google Scholar]
- 131.Wahoff M Ryan M Rehabilitation after hip femoroacetabular impingement arthroscopy. Clin. Sports Med. 2011;30(2):463‐482. [DOI] [PubMed] [Google Scholar]
- 132.Tijssen M van Cingel R van Melick N de Visser E Patient‐Reported Outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskelet Disord. 2011;12:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Thorborg K Roos EM Bartels EM Petersen J Holmich P Validity, reliability and responsiveness of patient‐reported outcome questionnaires when assessing hip and groin disability: a systematic review. Br. J. Sports Med. 2010;44(16):1186‐1196. [DOI] [PubMed] [Google Scholar]
- 134.Mohtadi NG Griffin DR Pedersen ME et al. The Development and validation of a self‐administered quality‐of‐life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT‐33). Arthroscopy. 2012;28(5):595‐605; quiz 606‐510 e591. [DOI] [PubMed] [Google Scholar]
- 135.Griffin DR Parsons N Mohtadi NG Safran MR A short version of the International Hip Outcome Tool (iHOT‐12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611‐616; quiz 616‐618. [DOI] [PubMed] [Google Scholar]
- 136.Thorborg K Holmich P Christensen R Petersen J Roos EM The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br. J. Sports Med. 2011;45(6):478‐491. [DOI] [PubMed] [Google Scholar]
- 137.Thomee R Jonasson P Thorborg K et al. Cross‐cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro‐acetabular impingement. Knee Surg. Sports Traumatol. Arthrosc. 2014;22(4):835‐842. [DOI] [PubMed] [Google Scholar]
- 138.Jonasson P Baranto A Karlsson J et al. A standardised outcome measure of pain, symptoms and physical function in patients with hip and groin disability due to femoro‐acetabular impingement: cross‐cultural adaptation and validation of the international Hip Outcome Tool (iHOT12) in Swedish. Knee Surg. Sports Traumatol. Arthrosc. 2014;22(4):826‐834. [DOI] [PubMed] [Google Scholar]
- 139.Sansone M Ahlden M Jonasson P et al. A Swedish hip arthroscopy registry: demographics and development. Knee Surg. Sports Traumatol. Arthrosc. 2014;22(4):774‐780. [DOI] [PubMed] [Google Scholar]
- 140.Thorborg K Branci S Stensbirk F Jensen J Holmich P Copenhagen hip and groin outcome score (HAGOS) in male soccer: reference values for hip and groin injury‐free players. Br. J. Sports Med. 2014;48(7):557‐559. [DOI] [PubMed] [Google Scholar]
- 141.Hedbeck CJ Tidermark J Ponzer S Blomfeldt R Bergstrom G Responsiveness of the Short Musculoskeletal Function Assessment (SMFA) in patients with femoral neck fractures. Qual. Life Res. 2011;20(4):513‐521. [DOI] [PubMed] [Google Scholar]