Abstract
Background:
Evaluation and treatment of groin pain in athletes is challenging. The anatomy is complex, and multiple pathologies often coexist. Different pathologies may cause similar symptoms, and many systems can refer pain to the groin. Many athletes with groin pain have tried prolonged rest and various treatment regimens, and received differing opinions as to the cause of their pain. The rehabilitation specialist is often given a non‐specific referral of “groin pain” or “sports hernia.” The cause of pain could be as simple as the effects of an adductor strain, or as complex as athletic pubalgia or inguinal disruption. The term “sports hernia” is starting to be replaced with more specific terms that better describe the injury. Inguinal disruption is used to describe the syndromes related to the injury of the inguinal canal soft tissue environs ultimately causing the pain syndrome. The term athletic pubalgia is used to describe the disruption and/or separation of the more medial common aponeurosis from the pubis, usually with some degree of adductor tendon pathology.
Treatment:
Both non‐operative and post‐operative treatment options share the goal of returning the athlete back to pain free activity. There is little research available to reference for rehabilitation guidelines and creation of a plan of care. Although each surgeon has their own specific set of post‐operative guidelines, some common concepts are consistent among most surgeons. Effective rehabilitation of the high level athlete to pain free return to play requires addressing the differences in the biomechanics of the dysfunction when comparing athletic pubalgia and inguinal disruption.
Conclusion:
Proper evaluation and diagnostic skills for identifying and specifying the difference between athletic pubalgia and inguinal disruption allows for an excellent and efficient rehabilitative plan of care. Progression through the rehabilitative stages whether non‐operative or post‐operative allows for a focused rehabilitative program. As more information is obtained through MRI imaging and the diagnosis and treatment of inguinal disruption and athletic pubalgia becomes increasingly frequent, more research is warranted in this field to better improve the evidence based practice and rehabilitation of patients.
Levels of Evidence:
5
Keywords: Adductor strain, athletic pubalgia, groin pain, rehabilitation, sports hernia transversus abdominis
INTRODUCTION AND BACKGROUND
Evaluation and treatment of groin pain in athletes is challenging. The anatomy is complex, multiple pathologies often coexist, different pathologies may cause similar symptoms, and many systems can refer pain to the groin. Many athletes with groin pain have tried prolonged rest and various treatment regimens, and receive differing opinions as to the cause of their pain.1,2 The rehabilitation specialist is often given a non‐specific referral of “groin pain” or “sports hernia.” As the vocabulary is still inconsistent, the data evolving, and the treatment protocols progressing, understanding the specific injury patterns at an anatomic level is the first step in creating a therapeutic protocol in both the non‐operative, and post‐operative patient.
Differential Diagnosis
A thorough history and a physical examination is needed to differentiate groin strains from athletic pubalgia, osteitis pubis, hernia, hip‐joint osteoarthrosis, rectal or testicular referred pain, piriformis syndrome or presence of a coexisting fracture of the pelvis or the lower extremities. Many of these diagnoses may exist in the active patient and present with similar symptoms and pain patterns. Although significant data regarding the myriad of terms used to describe groin injuries was gathered in the last three decades, core injury specialists, mainly surgeons, are relying heavily upon new data obtained from magnetic resonance imaging (MRI). MRI technology has advanced to the point where specific injury patterns can be recognized. This imaging has added to the understanding of, and even redefined the term “sports hernia”, and to a large degree has made the name obsolete. For the most part, the term “sports hernia” encompasses two patterns of injury: inguinal disruption and athletic pubalgia.
The term “sports hernia” which has been adopted by the media, public, and the medical community alike, is falling out of favor with specialists who take care of this group of injuries. The reason is twofold. First, the injury is not a hernia, as there is no actual defect in the abdominal wall. Second, although the injury does occur frequently in the athlete, it is not limited to this population. The term is simply a misnomer. It does, however, have staying power, and despite many attempts by consensus conferences attendees, the term remains in use.
Nevertheless, inguinal disruption is meant to convey terms such as sports hernia, incipient hernia, Gilmore's groin, groin disruption and sportsman's groin3. The British Hernia Society's 2014 position statement based on the Manchester Consensus Conference delineated this group of pathologies from MRI findings at the symphysis pubis where two observations are commonly noted: bone marrow edema, which often indicates injury in the area of the pubis, and “symphysis capsular and adductor change, which involves the anterior capsule, capsular ligaments and the enthesis of the common aponeuroses of the adductor longus and rectus abdominis”3 Although exact terminology is not universally agreed upon, for the purposes of clarity in this clinical commentary, the term inguinal disruption is used to describe the syndromes which are related to the injury of the inguinal canal soft tissue environs ultimately causing the pain syndrome. The term athletic pubalgia will be used to describe the disruption and/or separation of the more medial common aponeurosis from the pubis, usually with some degree of adductor tendon pathology.3
Typically athletic pubalgia is believed to be multifaceted, occurring with a twisting motion exacerbated by planting the foot at high speeds, sudden sharp changes in direction, repetitive kicking, and lateral motion.4-6 Diagnosis is often made by conducting an accurate history and physical examination, and then often confirmed with MRI. Specific MRI protocols are currently in use to assess the area to determine the degree of aponeurotic plate disruption and adductor tendinopathy. Additionally, sequences with and without the performance of the Val Salva maneuver can assist in assessment of the integrity of the transversalis fascia, which can be attenuated as described by Gilmore, one of the findings seen in inguinal disruption.
Despite the fact that inguinal disruption and athletic pubalgia are separated in description, the injury often involves both pathologies, and the symptoms can be very similar. Pain is often described as chronic, with point tenderness near the lower abdominal insertion, at the pubic tubercle, and can involve the adductor longus tendon origin as well.4,7 A typical physical exam will often reveal palpable tenderness over the pubic tubercle and overall pelvic weakness in the floor as well as surrounding musculature. The patient will often experience increased symptoms when asked to perform a resisted sit‐up, as the abdominal area pushes outward upon execution of this movement. In addition, the patient may present with adductor and hip flexor weakness with dynamic movement.5 Upon completion of an observational gait analysis, dysfunction can often be noted with the movement of the pelvis and femoral alignment of the lower extremities. The hallmark complaint of athletic pubalgia is a “deep” groin or lower abdominal pain with exertion. This pain tends to be deeper and more intense than an adductor or iliopsoas strain and is ipsilateral in nature. According to Kachingwe et al6 there are five signs that are indicative of a “sports hernia” now termed athletic pubalgia as seen in Table 1.
Table 1.
Five signs that are indicative of athletic pubalgia
| 1-A subjective complaint of deep groin/lower abdominal pain |
| 2-The pain is exacerbated with increased exertion such as sprinting, cutting, sit-up and is relieved with rest |
| 3-Palpable tenderness over the pubic ramus at the insertion of the rectus abdominus and/or conjoined tendon |
| 4-Pain with resisted hip adduction at 0,45, and/or 90 degrees of hip flexion |
| 5-Pain with resisted abdominal curl up. |
TREATMENT OPTIONS
Non‐operative conservative treatment is often advocated as the first type of intervention. Treatment mainstays include rest, abstention from the aggravating sport and similar activities, and focused rehabilitation. There is little evidence supporting the effectiveness of conservative care, however, the majority of studies that have been conducted showed significant improvement after 6‐8 weeks of physical therapy intervention.6,7 With little evidence to guide clinicians with the differential diagnosis and effective treatment of patients with athletic pubalgia or inguinal disruption, management of this condition has been diverse. Table 2 outlines a typical non‐operative rehabilitation protocol addressing both athletic pubalgia and inguinal disruption pathologies. While this lack of evidence based research may not seem like a problem with non‐operative treatment, various pathological injuries may present with similar signs and symptoms with overlapping findings upon exam and evaluation.6,8
Table 2.
Non‐operative Management of Athletic Pubalgia; Phases I‐IV
Phase I (1‐2 weeks)
|
Phase II (2‐4 weeks)
|
Phase III (4‐6 weeks)
|
Phase IV (Week 6‐8)
|
Pain control and reduction of any edema is the focus of phase one non‐operative care. Inability to reduce or control the pain prevents the patient from progressing to Phase II (Table 2). The patient at this point should be able to move throughout the day conducting daily activities with little to no pain present. Patients should not have reports of deep groin pain with increase intensity but may experience occasional “twinges” with new activity additions.
Non‐operative rehabilitation can be performed on its own or coupled with steroid injections of the pubic symphysis or the adductor tendon origins, anti‐inflammatories, and rest from activity. Clinical assessment of core stability, hip strength and flexibility, and identification of muscular compensation and imbalances are crucial. Treatment should target strengthening and neuromuscular reeducation regarding timing and recruitment patterns during functional motion in addition to manual therapy techniques to manage soft tissue and fascial restrictions.7 A comprehensive rehabilitation program to develop coordination and strength of the hip adductors, flexors, internal rotators, extensors, core stabilizers and lumbopelvic spinal musculature is important for an effective recovery. Table 3 provides a list of examples of core and proprioceptive exercises to include in the beginning stages of a conservative rehabilitation program.
Table 3.
Core & proprioceptive exercises for early stages of conservative treatment
| Examples of Beginner Lower Abdominal, Core Exercises |
| Posterior pelvic tilts with completion of exhalation |
| Posterior pelvic tilts with exhalation and bridging |
| Front and side planks with exhalation and maintaining pelvic neutral |
| Examples of Proprioceptive Exercises |
| Balance on unstable surface maintaining pelvic neutral |
| (Progress from double‐leg to single leg stance) |
| Balance on unstable surface while throwing and catching a ball |
| (Progress from double‐leg to single leg stance) |
| Balance on unstable surface using a BodyBlade® |
| (Progress from double‐leg to single leg stance) |
Progression to incorporation of single leg activities on an unstable surface activates deep pelvic and core stabilization as well as developing proprioception and kinesthetic awareness.7,13 Active stretching of the spine and lower extremities to ensure the preservation of flexibility and full range of motion should be added targeting the muscles around the pelvis. The progression to the final stage places the patient back into the sports specific activity that they wish to return to in a light and modified manner with a focus on core stabilization and proper body mechanics.
Effective rehabilitation of the high level athlete to pain free return to play, requires addressing the differences in the biomechanics of the dysfunction when comparing athletic pubalgia and inguinal disruption. After approximately six months, an assessment is made as to whether non‐operative measures have been effective. Beyond this point, the injury is chronic, and more aggressive options may be entertained.
POST OPERATIVE REHABILITATION
Post‐operative and non‐operative conservative treatments have similar guidelines and stages of recovery. Post‐operative rehabilitation following “sports hernia” repair (encompassing both athletic pubalgia and inguinal disruption) should be based on the physiology of soft tissue healing. It is imperative that the rehabilitation does not excessively stress the repair too early. Although each surgeon has their own specific set of post‐operative guidelines, some common concepts are consistent among most surgeons and are defined in phases (Table 4). An initial rest period of four weeks is typically recommended post‐operatively before physical therapy is initiated. The main objectives and clinical milestones for progression between stages are outlined in the tables.
Table 4.
Post‐Operative Rehabilitation Protocol
Week 1
|
Week 2‐3
|
Week 4
|
Week 5‐6
|
Week 6‐8
|
The first week of post‐operative rehabilitation is for management of pain and swelling, with relative rest recommended. Daily walking on flat surfaces is encouraged. Therapeutic massage around adductors and surrounding tissue away from the incision site may begin as soon as two weeks after surgery and progress to scar management over the abdominal incision area by 3‐4 weeks after surgery (when rehabilitation typically is initiated). The patient should avoid excessive trunk extension and rotation.9 Neuromuscular reeducation and muscle activation and recruitment exercises are initiated in the next phase, as well as mild resistive exercise of the lower extremities in the form of progressive resistive exercises (PREs). Abdominal crunches or sit ups are contraindicated at his time but initial contraction of the abdominal muscles is started in the form of activating and increasing the recruitment in the transversus abdominis muscle [Fig. 1]. Light stationary biking is introduced at this time. The following stage starts the resistive exercises. Additionally, open chain exercises of the lower extremities are initiated reminding the patient to continue to contract the transversus abdominis muscle during the movements, ensuing proximal stability for distal mobility [Figures 2‐4]. Both dynamic and static abdominal exercises are initiated and sports specific movements start to enter into the guidelines (Table 4).
Figure 1.
Core‐stabilized FABER test.
Figure 1. Posterior pelvic tilt. (A) Lying on your back relaxed with your hands placed over the anterior superior iliac spine (ASIS) on each side and tips of fingers applying a slight pressure to the soft tissue just medial to the ASIS. (B) Start the motion by drawing the pubic symphysis towards the umbilicus with emphasis on anterior musculature contracting. The fingers should feel the transversus abdominis contract equally on each side, the rib cage should depress and the lumbar spine should flatten with little effort applied.
Figure 4.
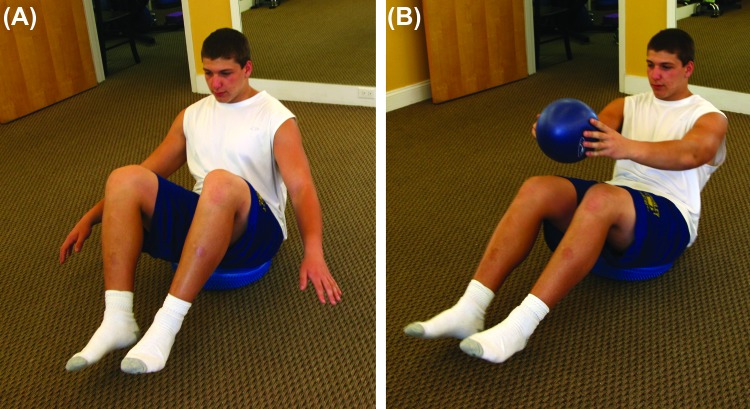
Pelvic stability on unstable surface progression. (A) Sitting on an air filled balance disc, place knees and feet together in midline and find pelvic stabilizers with feet on ground. (B) With arms outstretched, maintain midline as you lift one knee towards chest attempting to hold pelvis and trunk stable. (C) Progress to lifting both legs off and balancing for a prolonged hold. (D) Once prolonged holds are achieved progress to the addition of a ball toss.
Figure 2.
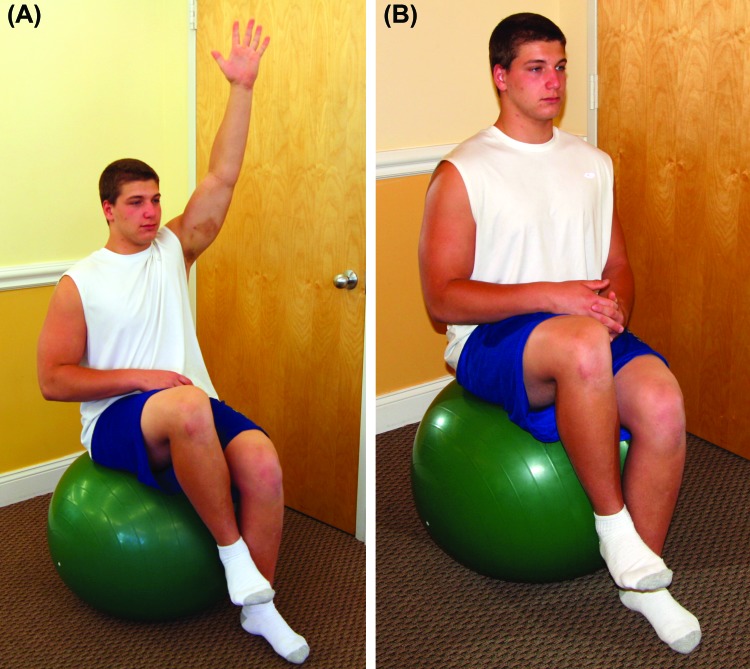
Hip conditioning and core stabilization exercise. (A) Start sitting on a ball positioning the knees and hips at 90 degrees with hands on the hips or thighs. (B) Place knees and feet together in midline and lift one knee while trying to maintain pelvic and trunk stability. (C) Once pelvic and trunk stability is achieved with the hands on the thighs, progress to opposite upper extremity (UE) placing opposing pressure on raised knee while other UE is raised in the air for additional stabilization challenge.
Figure 3.
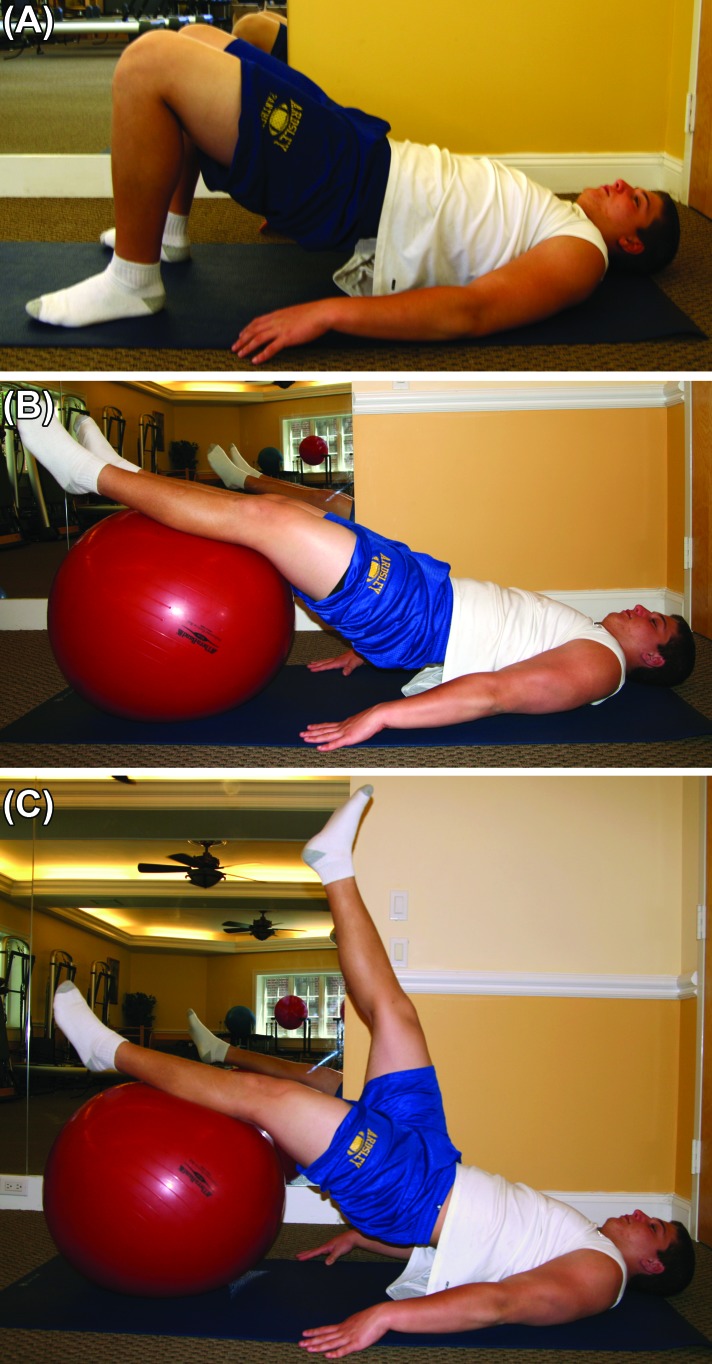
Bridging coupled with lower extremity lift. (A) Lie on floor and bridge from pressure applied to the lower extremities against the floor. (B) Place a physioball under the legs and apply downward pressure to the ball as the legs straighten allowing the pelvis to rise from the surface. (C) Once able to bridge on ball, lift one leg into the air, keeping knee extended and trunk stabilized.
The final stage is based on an 8‐12 week projection for return to sport; rehabilitation may take longer in some instances depending on the involvement, including the extent of the surgical procedure and the patient's tolerance to recovery. Balance and proprioceptive exercises are progressed to activity specific level with the addition of perturbations and uneven surfaces. Balance progressions on an unstable surface are performed in all directions [Fig. 5]. Increased emphasis on dynamic and functional training with both concentric and eccentric strengthening is included in this phase [Figures 6‐9]. Lastly, early stages of plyometrics, integrating upper and lower extremities are added at the end of this stage in preparation for the athlete to return to play (Week 8‐12).
Figure 5.
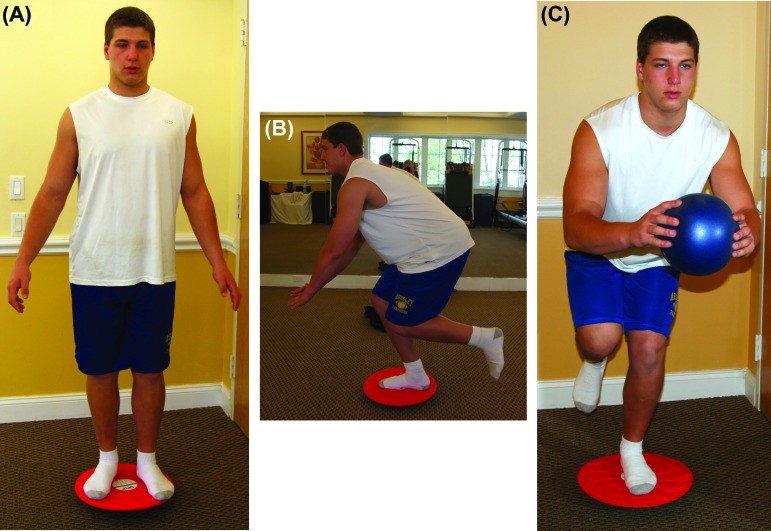
Double leg & single leg balance and proprioceptive training. (A) Standing on a 360 degree balance board (Fitter International, Calgary, Canada) with knees and hips flexed try to maintain balance. (B) Progress to single leg activity with hips and knee flexed once bilateral is mastered. (C) Add a ball toss once single leg balance and control is achieved.
Figure 9.
Quadruped Training (A) Align the knees under the hips and the hands under the shoulders and maintain pelvic alignment as one leg is outstretched. (B) Once aligned extend one leg and the opposite arm maintaining pelvic and shoulder girdle alignment.
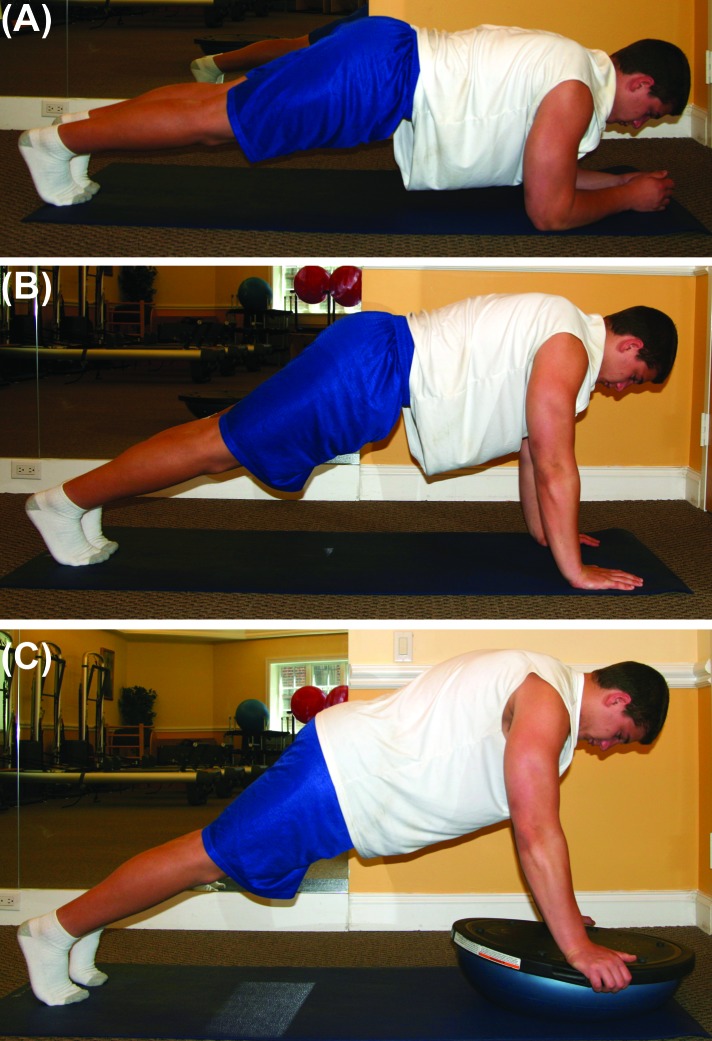
Figure 6.

Wall squat with pelvic stabilization. Place ball behind low back and squat to 90 degrees hip flexion, holding trunk and pelvis in place. Then, raise up one knee to lift foot from ground.
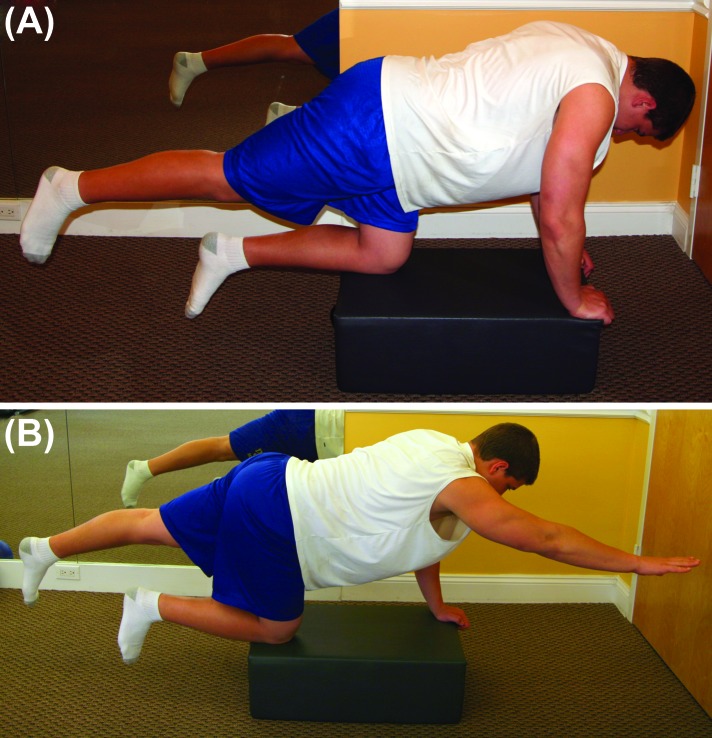
Figure 7.

Side plank. Lying on side. align shoulder, elbow, hips and ankles and raise up into plank maintaining alignment.
Figure 8.
Front plank progression (A) align shoulders with elbows and lift into forearm plank keeping pelvis in alignment (B) Progress to placing hands aligned with shoulders and fingers pressing into surface keeping pelvis aligned with plank position (C) Place hands on BOSU® (BOSU, Ashland, OH) and balance with the body held in plank position keeping pelvic alignment.
The possibility of coexisting injuries exists, where more than one affliction causes groin pain, thereby making it difficult to establish which injury is the main contributor to pain and which is secondary. In fact, Larson et al10 found that when an athlete had a “sports hernia” repair and an intra‐articular hip surgery concomitantly the success rate was much better than performing surgery on just one of the pathologies.
SUMMARY
The importance of achieving the proper muscle activation and recruitment pattern training is crucial for proper recovery with both conservative and post‐operative rehabilitation. Often patients will compensate giving the illusion of abdominal and pelvic control. The ability to properly recruit and contract the core musculature with proper timing creates a supportive “cylinder” around the spine.11 Delayed onset and poor transversus abdominis muscle activation has been shown to be associated with long‐standing groin pain.12
Typically these symptoms have existed for months if not longer by the time a diagnosis is determined. Given that the majority of cases of athletic pubalgia/inguinal disruption cases are insidious onset, determining the mechanism of injury is difficult and the patient may experience periods of improvement and episodic exacerbations making long term success sometimes difficult. The main commonality of this injury is typically increased repetitive torque on the pubic symphysis during aggressive thigh abduction/adduction. This motion can lead to disruption of the aponeurosis of the rectus abdominis and the adductor longus tendon.1,2,8
CONCLUSION
In general, treatment and rehabilitation are designed to relieve pain, restore range of motion, restore strength, and return function. Although these guidelines are outlined for progression, not all individuals will respond in the same manner. Clinical experience and judgment with sound clinical reasoning should be factored in when executing a patient's specific plan of care. Proper evaluation and diagnostic skills for identifying and specifying the difference between athletic pubalgia and inguinal disruption allows for an effective and efficient rehabilitative plan of care. Applying protocols for stages of operative and non‐operative rehabilitation helps to ensure that all aspects of function are addressed and re‐injury is prevented. As more information is obtained through MRI imaging and the diagnosis and treatment of inguinal disruption and athletic pubalgia becomes increasingly frequent, rehabilitation specialists are afforded a better understanding to the mechanism of injury and the proper biomechanics required to allow for a full recovery and return to pain free function. As with any new development in the medical and rehabilitative field, more research is warranted to better improve the evidence based practice and rehabilitation of patients.
REFERENCES
- 1.Schilders E Dimitrakopouiou A Cooke M et al. Effectiveness of a selective partial release for chronic adductor‐related groin pain in professional athletes. Am J Sport Med. 2013;43:603‐607. [DOI] [PubMed] [Google Scholar]
- 2.Minnich JM Hanks JB Muschaweck U et al. Sports Hernia: Diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sport Med. 2013;39:1341‐1349. [DOI] [PubMed] [Google Scholar]
- 3.Sheen AJ Stephenson BM Lloyd DM et al. Treatment of the Sportsman's groin: British Hernia Society's 2014 position statement based on the Manchester Consensus Conference. Br J Sports Med. 2013. 10.1136/bjsports-2013-092872. [DOI] [PubMed] [Google Scholar]
- 4.Ahumada LA Ashruf S Espinosa‐de‐los‐Monteros A et al. Athletic pubalgia: Definition and surgical treatment. Ann Plast Surg. 2005;55(4):393‐396. [DOI] [PubMed] [Google Scholar]
- 5.Joesting DR Diagnosis and treatment of sportsman's hernia. Curr Sports Med Rep. 2002;1(2):121‐124. [DOI] [PubMed] [Google Scholar]
- 6.Kachingwe AF Grech S Proposed algorithm for the management of athletes with athletic pubalgia (Sports Hernia): A case series. J Ortho Sports Phys Ther. 2008;38(12):768‐781. [DOI] [PubMed] [Google Scholar]
- 7.Woodward JS Parker A MacDonald RM Non‐surgical treatment of a professional hockey player with the signs and symptoms of sports hernia: A case report. Int J Sports Phys Ther. 2012;7(1):85‐100. [PMC free article] [PubMed] [Google Scholar]
- 8.Rabe SB Oliver GD Athletic pubalgia: Recognition, treatment, and prevention. Athl Train Sports Health Care. 2010;2:25‐30. [Google Scholar]
- 9.Litwin DE Sneider EB McEnaney PM et al. Athletic pubalgia (sports hernia) Clin Sports Med. 2011; 30(2):417‐434. [DOI] [PubMed] [Google Scholar]
- 10.Larson CM Pierce BR Giveans MR Treatment of athletes with symptomatic intra‐articular hip pathology and athletic pubalgia/sports hernia: A case series. Arthroscopy. 2011;27(6):768‐775. [DOI] [PubMed] [Google Scholar]
- 11.Drysdale CL Earl JE Hertel J Surface electromyographic activity of the abdominal muscles during pelvic‐tilt and abdominal hollowing exercises. J Athl Train. 2004;39(1):32‐36. [PMC free article] [PubMed] [Google Scholar]
- 12.Cowan SM Schache AG Brunker P et al. Delayed onset of transversus abdominus in long‐standing groin pain. Med Sci Sport Exerc. 2004; 2040‐2045. [DOI] [PubMed] [Google Scholar]
- 13.Tyler TF Silvers HJ Gerhardt MB Nicholas SJ Groin injuries in sports medicine. SportsHealth. 2010;2(3):231‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Omar IM Zoga AC Kavanogh EC et al. Athletic pubalgia and “Sports Hernia” optimal MR imaging technique and findings. Radiographics. 2008; 1415‐1438. [DOI] [PubMed] [Google Scholar]
- 15.Meyers WC Ricciardi R Busconi BD et al. Groin Pain in the Athlete. In Arendt EA (ed). Orthopaedic Knowledge Update Sports Medicine 2. Rosemont, IL, American Academy of Orthopaedic Surgeons 1999; 281–289. [Google Scholar]