Abstract
Purpose/Background:
Hamstring injuries are common at all levels of sport, however recurrence rates are disproportionate compared to other soft tissue injuries. Age and previous injury are supported in the literature as risk factors for hamstring injury; nonetheless, debate exists regarding modifiable risk factors. Restoration of peak torque length using lengthening eccentrics and core stability interventions appear to reduce incidence of re‐injury. The purpose of this clinical commentary is to review examination techniques and rehabilitation considerations in order to identify important risk factors to reduce recurrence after hamstring strain and total rupture.
Discussion/Relation to Clinical Practice:
Novel clinical examination techniques both at time of acute injury and prior to return to sport may provide valuable prognostic information. Restoration of core stability, neuromuscular control and lengthening eccentric hamstring interventions are proposed key components to reduce hamstring re‐injury.
Levels of Evidence:
Level 5
Keywords: Eccentrics, hamstring injury, recurrence risk factors
INTRODUCTION
Hamstring strain injuries (HSI) are among the most common injuries in the active population, and are notorious for their high rates of re‐injury. In the American National Football League for example, HSIs have been reported to account for 12%1 of all primary injuries, and their recurrence rate is remarkable, at 32%.2 They are the most common injury reported in professional soccer and account for 29% of track and field injuries in sprinters.3 Additionally, HSIs are reported with high frequency in sports that require sprinting, kicking, acceleration, and change of direction including rugby,4 and Australian Rules Football.5 The average amount of time missed from sport is 18 days, however, actual time missed is often greater and costly.7 Several authors have identified that the best predictor for a hamstring injury is a prior hamstring injury.8-10 There are other risk factors involved in predicting vulnerability to hamstring injury, but none have proven more consistent than prior injury. This is not to say that if one suffers a hamstring injury they will definitively suffer another. However, the probability of re‐injuring the same hamstring in the future becomes considerably higher.2,4,5,8,
Recurrence rates following hamstring injuries are high with the greatest incidence for re‐injury occurring within the first two weeks after return to sport.5,11,12 Increased recurrence rates within this timeframe may indicate continued impairments and functional limitations not be easily identified with traditional return to sport testing.7,12,13 Many non‐modifiable and modifiable risk factors for recurrent hamstring injuries exist including, but not limited to; previous injury,5,9,14-16 increasing age,5,7,9,14-17 ethnicity,4,7,17 strength imbalances,2,6,19-22 inflexibility,23-25 and fatigue.2,25-27
Researchers have determined that the most consistent non‐modifiable factors for hamstring strains are age and the history of a prior hamstring injury.8,9,25,28 Modifiable factors include hamstring weakness, fatigue, decreased flexibility and quadriceps and hamstring muscular imbalance.25 Additional factors for the predisposition toward HSI include limited quadriceps flexibility and deficient strength and coordination of pelvic and trunk muscles.29,30
HSI can occur in either a high speed state where the muscle is overstrained or in a slow speed state where the muscle is overstretched.31,32 The two mechanisms of injury contrast one another and generally occur in different locations. The most common mechanism of injury to the hamstring is during sprinting and is believed to occur during the terminal swing phase of the gait cycle.31,32 Biomechanically, during the second half of the swing phase, the hamstrings are actively lengthening (eccentrically contracting) and absorbing energy from the decelerating limb to prepare for ground contact.33-35 The biceps femoris is required to contract forcefully while lengthening to decelerate the extending knee and flexing hip.35 At this point, the biceps femoris is placed under the greatest amount of stretch compared to the medial hamstring reaching almost 110%36 of its length present during upright standing. Terminal swing is a particularly vulnerable position for bicep femoris injury due to it's high activation in a lengthened state.37 HSIs that occur during slow movements such as dancing or stretching involve simultaneous hip flexion and knee extension placing the hamstrings in an extremely lengthened position.38 The proximal semimembranosus is normally implicated in this condition.39,40 Although this mechanism of injury is often less painful at onset, it tends to require a longer recovery period than a HSI incurred in a high speed state.39-41 Despite a difference in recovery time and mechanism of injury, the rehabilitation process typically remains the same. Further research is needed to determine if alternative approaches should be employed for each mechanism, in order to improve outcomes.The purpose of this clinical commentary is to discuss risk factors associated with hamstring injuries and to identity effective treatment strategies and methods to assess readiness to return to sport, in order to avoid recurrence.
ANATOMY
The hamstrings are comprised of three muscles, located on the posterior thigh. The biceps femoris, semimembranosus, and semitendinosus are two‐joint muscles that function to extend the hip and flex the knee. They share a common origin at the ischial tuberosity but have distinct insertion sites. The semimembranosus and semitendinosus insert on the proximal tibia and therefore have the capacity to internally rotate the distal leg. The biceps femoris, which has a short head (single joint muscle) originating at the posterolateral shaft of the femur, converges with the long head and inserts on the head of the fibula. The biceps femoris portion of the hamstrings is able to externally rotate the distal leg. The most frequently injured muscle of the hamstring group is the largest of the three muscles, the biceps femoris. It is important to note that the two heads of the biceps femoris have different innervations, and this has been identified as a possible contributor to injury.2,7 The semitendinosus, semimembranosus and long head of the biceps femoris receive their innervation from the tibial nerve (L5, S1, S2),7 while the short head of the biceps femoris is innervated by the common fibular nerve (L5, S1, S2).7
Clinical Examination
Magnetic resonance imaging (MRI) and ultrasonography (US) are commonly used to assess tissue integrity after HSI with moderate to strong diagnostic and prognostic values.42-45 In recent years, US has been advocated due to lesser cost and increased availability.46 Connell, et al demonstrated equal versatility comparing both MRI and US in professional Australian Rules Football for identifying acute hamstring injuries, however, as healing progresses, its sensitivity in detecting injury decreases.47 Their analysis did demonstrate that the longitudinal length of the hamstring tear was correlated with recovery and return to sport. Contrary to this finding, Petersen did not find any correlation between the length of injury and severity indicating that US alone does not provide significant prognostic value with regard to return to sport.48
A thorough history is the hallmark of hamstring injury evaluation and provides the clinician valuable information for both diagnostic and prognostic decisions. A mechanism of injury is almost always reported and typically occurs during high velocity contractions and/or excessive stretching.5,3,38 The majority of injuries are due to the former occurring during participation in sports that require quick changes of direction and explosive maneuvers.3-6 Incidence of hamstring injuries may be higher towards the end of contests due to muscle fatigue, however this supposition has not been substantiated.4,7,25,31
A clinical exam consists of palpation, resistance, and mobility testing in order to provide the practitioner valuable information regarding the site of injury and prognostic information regarding return to sport. Following hamstring injury, athletes often demonstrate an altered gait pattern as well as localized tenderness, pain with resisted movement (knee flexion and hip extension), and pain with passive knee extension.9,12,30,50 Impairments in mobility and strength following initial injury indicate a greater degree of damage and potential delay in returning to activity.12,50,51 Warren determined that athletes requiring greater than one day to ambulate without pain are more likely to take longer than 3 weeks to return to sport.51 Additionally, Malliaropoulos et al correlated a greater reduction in knee active range of motion (ROM) with longer delay in return to activity.12 Within this study, a clinically‐based classification system (Table 1) was found to provide an effective clinical tool to assess risk of re‐injury and return to play time, with Grade II injuries having the great risk for recurrence (24%) followed by Grade I (9.3%).12 This however may have been partly due to a shorter return to play timeframe with moderate soft tissue disruption with grade II injuries. Scheider‐Kolsky et al also found a correlation between results from clinical clinical testing and delayed return to play time in athletes with mobility and strength deficits further supporting the value of the clinical exam for prognostic decision making.50
Table 1.
Classification for Acute Hamstring Strains with Recovery Time*
| Clinical Grade | AROM Deficit (Compared to uninvolved limb) | Return to Sport, days |
| I | <10° | 6.9 |
| II | 10°‐19° | 11.7 |
| III | 20°‐29° | 25.4 |
| IV | ≥30° | 55.0 |
Table adapted from Malliaropoulos, 2011
Utilization of palpation, mobility, and/or resistance testing to diagnose hamstring strain has been suggested in the literature, however diagnostic accuracy has not been validated.52 In a recent systematic review, Reiman et al, found few studies assessing psychometric properties of special tests used to diagnosis HSI.52 Their results found limitations in the diagnostic accuracy of for both single and composite special testing and recommend using a battery of tests to improve assessment and rule out other potential pain generators. As mentioned previously, the prognostic ability of these tests may be useful in predicting return to play time planning strategies for rehab.12,50
RANGE OF MOTION
The hamstrings are biarticular muscles, therefore, range of motion measurements and testing should be conducted taking both the hip and knee joints into account. This screen will normally take place post‐injury, so it is important to note that the extent of available motion may be limited by discomfort, stiffness, or pain leading to a deficient measurement. For this reason, testing should be done bilaterally.
Passive Straight Leg Raise Test30,42: The patient is positioned in supine with the clinician standing on the test side. The lower extremity is held in knee extension and the hip passively flexed until restriction occurs or the patient reports tension. Attention must also be paid to the contralateral limb for hip or knee flexion as compensation to achieve greater hip flexion on the test side. The normal range for hip flexion with the knee extended is 808‐1408.54 A measurement of less than 80º is considered deficient.54
Active Knee Extension Test30,50,12: The patient is positioned in supine with the clinician standing on the test side. The test side lower extremity is then passively flexed at the hip to 908 with the knee flexed. The patient is then asked to actively extend the knee to end range. Once the knee meets restriction, this measurement should be taken at the knee as this would be a true reflection of hamstring length. The knee should be able to extend to at least 208.55
PALPATION
The ability to discern differences in muscle tissue aids in making a proper diagnosis of this injury. Although not every patient with a HSI will present with a palpable defect in the muscle, tenderness, fullness/tension, and pain to the touch should also be documented38.
Hamstrings: In order to help locate the different muscles in the group, light resisted knee flexion with the patient in prone can be performed. Be mindful that this may be painful for the patient. Once muscles have been identified, palpation should begin distally and work toward the proximal attachment. This will allow for the clinician to feel consistency along the muscle fibers making it easier to identify a defect. If the defect is distal, the clinician should notice an immediate to early change in consistency or the patient's report of pain during palpation.
The location and severity of pain with palpation about the ischial tuberosity can give information about the length of the recovery period.38 The more distal pain is located from the ischial tuberosity, the better the prognosis.38
STRENGTH TESTING
Isometric muscle testing should be conducted as part of a HSI examination to establish a baseline post‐injury measurement. These tests should be carried out bilaterally to gauge deficiencies between limbs. Due to the bi‐articular anatomy, testing should be conducted in multiple test positions to account for changes that arise with hip and knee movement.38
Knee Flexion: Patient should be positioned in the prone position with the hip in 08 of extension. While stabilizing the hip, the clinician's opposite hand should be placed just proximal to the medial and lateral malleoli on the posterior shaft of the tibia. Knee flexion should then be resisted at both 158 and 908.38 By internally or externally rotating the tibia, bias can be applied to the medial or lateral hamstrings.7
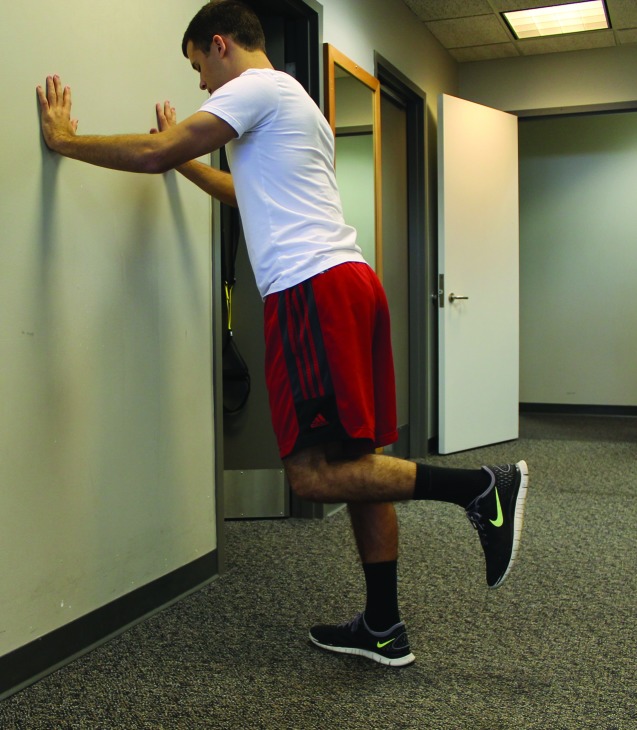
Single Leg Hamstring Bridge: This activity is performed with the injured limb propped on a 60 cm surface at 208 knee flexion, (plyo box, chair, exercise ball) while the unaffected limb is held in the air.57 The pelvis is then lifted off the ground in the motion of a bridge. This places demand directly on the hamstring to contract to support the body during the bridge. The pelvis is then returned to the floor to complete the repetition. A single leg hamstring bridge to assess functional strength of the hamstring group has been proposed in the literature as a reliable measure to predict strength deficits associated with future HSI.90,57 (Figure 1)
Figure 1.
Single leg bridge – Described by Freckleton,57 the athlete performs single leg bridge on a 60cm box with knee in 208 flexion until failure.
NEURAL TENSION TESTING
Testing to clear the sciatic nerve should be conducted as symptoms of a neural origin can cause posterior thigh pain. Neural tension can be present for patients who present with posterior thigh pain without a mechanism of injury.56 Neural tension is tested through the implementation of a slump test. The reproduction of symptoms from a positive slump test indicates a more proximal cause for the posterior thigh pain.50,58 Increased neural tension due to residual inflammation and scar tissue from recurrent hamstring injuries can affect normal sciatic nerve mobility.59
Slump Test: The patient should be positioned in sitting with legs dangling off the edge of the plinth, and asked to place their hands behind their back in internal rotation. The patient is then passively brought into neck and trunk flexion to their perceived limit. The clinician instructs the patient extend the knee and passively dorsiflex the foot. If pain presents in the posterior thigh, have the patient extend the neck. If pain then alleviates, the test is positive for neural tension.
PRINCIPLES OF REHAB
Non‐Operative Treatment
If clinical testing is consistent with a HSI, management to address impairments and risk factors is warranted. The main goal of physical therapy for a hamstring strain injury is to return the athlete to sport at the prior level of function, without pain, and with nominal risk of re‐injury.38 Recurrence is of serious concern particularly within the first 2 weeks returning to sports.60 As mentioned earlier, many factors of HSI and recovery have been found to contribute to the rate of re‐injury.11 Persistent weakness in the injured muscle, reduced extensibility of the tissue due to residual scar tissue and adaptive changes in the biomechanics and motor patterns of sporting movements following the original injury should be addressed.11
Due to the fact that HSIs commonly occur during eccentric contraction of the muscle, rehabilitation involving eccentric strength training of the hamstrings has been encouraged. Several researchers have suggested residual scar tissue present at the muscle attachment site contributes to a shorter optimum length for active tension than in the previously injured muscle.61,62 This is due to scar tissue that less extensible than the contractile tissue of the hamstring musculature and may alter the biomechanical function of the muscle by decreasing the peak musculotendon length.38 Eccentric strength training has been shown to assist in shifting the peak force development to longer musculotendon lengths, thus reducing the risk of re‐injury.63 Another concept proposed to be relevant for non‐operative treatment of HSIs is to promote increased coordination of the lumbopelvic region. By doing this, it allows the hamstrings to function at safe lengths during sports motions, thus reducing the risk of re‐injury.30 These theories have been supported by recent research and appear to show the most promise with regard to quicker return (within two weeks) to sport and prevention of recurrent injury.30,38 Optimal treatment parameters that are evidence based do not exist, therefore, this clinical commentary provides recommendations based upon available information.
THERAPEUTIC DRY NEEDLING
A fairly recent addition to physical therapy intervention is therapeutic dry needling. Dry needling involves the application of a fine filiform needle to soft tissues to treat intramuscular trigger points.64 Intramuscular needling mechanically disrupts taut bands of muscle tissue found in areas of muscular dysfunction, allowing for normalized tone via decreases in both pain and muscle tension.65,66 Dry needling of trigger points in areas of pain and dysfunction are commonly associated with reduced local and referred pain, improved range of motion (ROM) and decreased trigger point irritability both locally and remotely.67 Dry needling is best used as an adjunct to other methods of treatment to aid in decreasing dysfunction in the muscle tissue and improving function. In the case of a hamstring injury, disruption of dysfunctional tissue to improve flexibility and ROM can strongly aid in a shortened return to sport as evidenced in recent case study reports.65,68 Further high quality studies are needed to control variables and determine efficacy with regard to long‐term outcomes in patients who have sustained HSI.
REHAB PROGRESSION
Non‐Operative
Rehabilitation of a HSI is broken down into three phases with goals and progression criteria for advancement and return to sport.38 (Appendix A) Phase one focuses on minimizing pain and edema while protecting the healing area, especially directly following insult.69 Low intensity, pain‐free activity encompassing the entire leg and core region are initiated through the pain free range in order to reduce atrophy and increase neuromuscular control of lumbopelvic stablizers.38 Range of motion and intensity of the interventions as well as eccentric strengthening are progressed according to the patient's tolerance and transition into phase two of rehabilitation.38 Phase three integrates return to sport activity with more sport specific treatment interventions through the full, pain free ROM.38 At this point the patient should be ready to begin assimilating back into their sport without restriction.
Providing a patient with a precise prediction of when they can return to sport is challenging. Prognoses are generally given in ranges to account for variation in individual responses to treatment. However, with the highly variable nature of a hamstring strain injury between individuals, ranges tend to be wider, dependent on severity of the injury. Following an optimal physical therapy regiment, return to activity timeframes range from; 1‐3 weeks (Grade I); 4‐8 weeks (Grade II); and 3‐6 months (Grade III).50
OPERATIVE MANAGEMENT
While the majority of hamstring injuries are treated conservatively, severe hamstring disruptions warrant a surgical approach.70-72 Hamstring injuries with a tear and/or avulsion occur 12% of the time with 9% resulting from complete rupture of the proximal origin, often due to a violent eccentric load.73-75 Although hamstring avulsions have been reported in various sports, most occur while water skiing.76 The most common site of rupture occurs at the proximal attachment on the ischial tuberosity and are almost exclusively treated surgically with good outcomes reported in the literature.77,78 A positive bowstring sign is typically seen whereby no tension is palpated in the distal hamstring tendon with knee actively flexed at 908; a prominent finding indicating disruption of the hamstring.73 Operative management is advocated for 1) Avulsions with 2 cm retraction, 2) Complete tears of all three hamstring tendons with or without retraction, and 3) Partial tears that do not respond to conservative management.42,79,80 Without surgical correction, prolonged weakness, neurologic symptoms, and resultant functional impairments often limit long‐term outcomes.42,76
Excellent surgical outcomes have been reported following a hamstring avulsion with greater than 80% returning to pre‐injury level of sport.73,81,82 Harris et al found significantly better subjective outcomes, return to pre‐injury level of sport, and greater strength/endurance in a surgical versus non‐surgical approach following hamstring avulsion/rupture.83 While outcomes improve after operative intervention regardless of when surgery is performed, significantly better results were found after acute repairs (within 4 weeks) compared to chronic repairs.83 Barnett et al also reported better outcomes with acute repair; however no significant correlation between time to repair, type of injury (complete or partial tear), and functional outcomes were noted after a 2‐yr follow up.70
PRINCIPLES OF REHAB
Operative Management
Immediate goals following surgery of the hamstring complex are protection and facilitation of soft tissue healing. Protected weight bearing with use of crutches for 6‐8 weeks is recommended and patients are instructed to avoid deep hip flexion positions to avoid excessive strain through healing tissue. Generally, no bracing is required, however if surgery is performed beyond 5 weeks from injury it may be warranted.78 Patients are instructed to avoid striding beyond the contralateral limb during gait and ambulation and to maintain a pain‐free range.
A conservative home exercise program to avoid ST atrophy and development of deep vein thrombosis (DVT) is utilized with formal physical therapy beginning approximately two weeks post‐op. The initial phase of rehabilitation focuses on conservative mobility and muscle activation including both hip and lumbopelvic stabilizers. Pain‐free, submaximal isometric exercise of the hamstring complex, progressive weight bearing, and neuromuscular control in functional positions are hallmarks of the initial rehabilitation phase. Progressive strengthening, neuromuscular stability, and balance activities are advanced through intermediate stages based on soft tissue healing guidelines with a focus on continued protection. Isolated hamstring strengthening exercises may begin at 5‐6 weeks following surgery, if the patient is pain‐free with resistance. At this time, the patient's gait should normalize and use of visual cueing is encouraged to facilitate correct movement patterns. Functional stages of rehab focus on single leg stability and neuromuscular balance in order to restore pre‐injury levels of strength and correction of risk factors for re‐current injury. Sport‐specific interventions focusing on eccentric strength, high load, and eventually speed‐oriented drills are implemented to prepare the athlete for return to participation. Objective outcome testing is used to ensure a safe return to activity and mitigating risk for re‐injury and will be discussed.30,85
OPERATIVE REHAB PROGRESSION
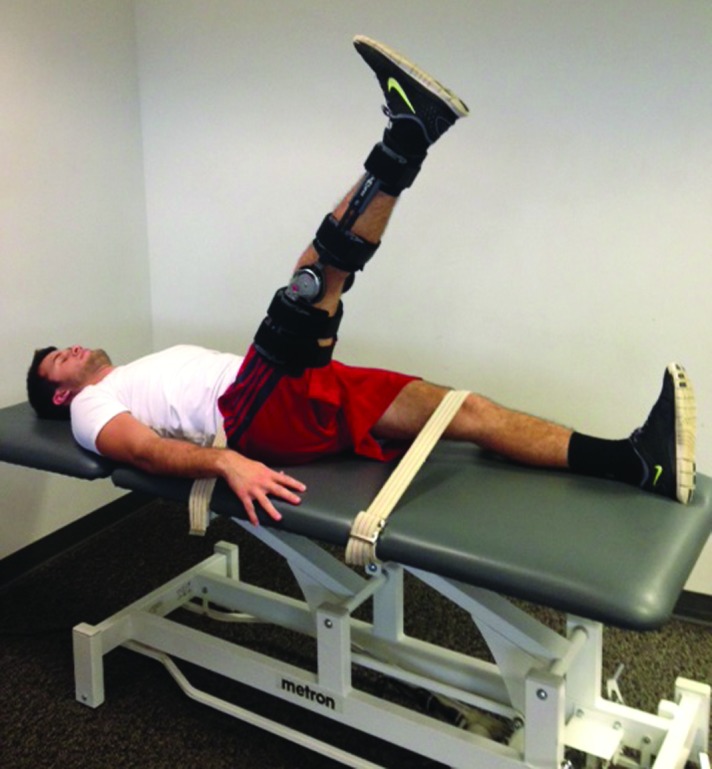
Phase I (0‐4 weeks)
Protection and soft‐tissue healing are hallmarks of this stage in rehabilitation.85 Isometric activation of gluteal muscles, transversus abdominis, and gentle hamstring contractions are recommended during the first week following surgery.85 Hamstring activation at approximately 30‐458 can be performed to prevent unnecessary inhibition.85 Standing balance exercise with the knee flexed and aquatic exercises can be implemented in weeks 2‐3 respectively to facilitate activation and functional mobility. Soft tissue mobilizations to improve scar mobility can be implemented in rehab and at home to facilitate healing and prevent formation of adhesions. Active ROM against gravity in a protected range is performed in either a standing or prone position pain‐free to ensure functional hamstring activation facilitate normal gait patterns. (Figure 2). Criteria to advance to the next stage include hip flexion ROM greater than 708 with 908 of knee flexion.
Figure 2.
Standing hamstring curl
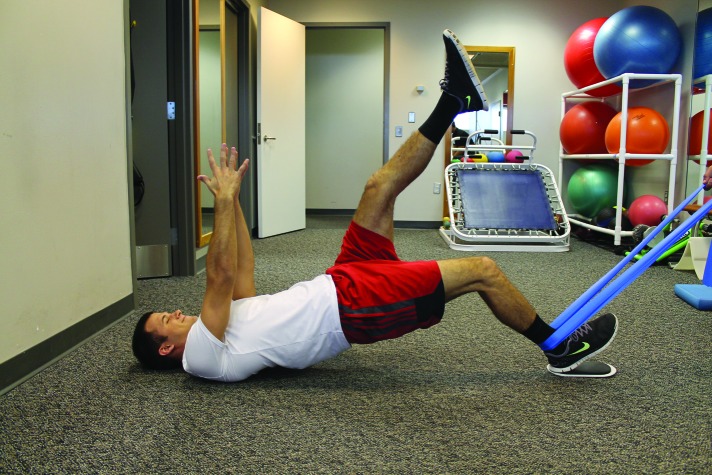
Phase II (5‐8 weeks)
Once the patient has achieved greater than 708 of knee motion, biking with low resistance and high seat position can be utilized to begin mobility and endurance work. Normalization of gait should be achieved within the first two weeks of this stage. Lumbopelvic stabilization, single leg balance, and neuromuscular control activities can be advanced including initiation of bridging, as well as progression from double to single leg positions. (Figures 3 and 4) Isolated hamstring strengthening avoiding end range positions can be performed if pain‐free. Pelvic bracing through activation of lumbopelvic stabilizers during hamstring strengthening should be utilized to ensure appropriate hamstring length and activation. Criteria to advance to Phase III include normalization of gait, less than 20% difference in hamstring mobility with active knee extension test and greater than 50% isometric hamstring strength compared to uninvolved limb with dynamometry measures.
Figure 3.
Double leg bridges
Figure 4.
Single leg dead lift
Phase III (8‐12 weeks)
Eccentric hamstring strengthening in a position of increased muscle length and lumbopelvic stability progression are main components of Phase III. Following injury, optimal peak torque values have a tendency to shift towards shorter muscle lengths. Brockett et al compared injured to uninjured hamstrings using isokinetic testing and found torque peaked at shorter muscle lengths.61 This shift in peak torque towards a shorted position may predispose the hamstring to injury during eccentric and lengthening movements inherent in sport. Schmitt et al described a strength test position with the hamstring in a maximally lengthened position of full hip flexion and knee extension.86 While this test has not been validated, it does provide a novel way to assess hamstring strength in a fully lengthened position. Isolated hamstring strengthening in a lengthened state seems to be an important consideration in this stage in order to restore length specific eccentric loading capacity limiting injury recurrence. Askling et al demonstrated a significantly quicker return to sport (49 vs 86 days) utilizing a lengthening compared to conventional rehabilitation protocol in both Swedish football and track athletes utilizing the same protocol.40,87 Only one re‐injury and two re‐injuries respectively were reported in this study, both of whom completed the conventional (non‐lengthened exercise position) program.40,87 These outcomes suggest that an emphasis be placed on lengthening exercises that may lessen return to sport time and prevent a re‐injury. Lengthening exercises such as single leg dead lifts, retro slides (Figure 5), and single leg hamstring curls in a lengthened position with bridge is beneficial in restoring the hamstring loading capacity in a lengthened state common in athletic movements (Figure 6).
Figure 5.

Retro slides
Figure 6.
Hamstring curl in lengthened range – Athlete performs hamstring curl at end range using slider and resistance band.
Lumbopelvic stability is also an important consideration during the rehabilitation process. 30 Sherry, et al completed a randomized controlled trial investigating a lumbopelvic and agility program compared to a conventional program consisting of ice, stretching and strengthening.30 The athletes’ who participated in the core stability program significantly reduced both the time to return to sport (22.2 vs 37.4 days) and re‐injury rates two weeks and 12 months following injury compared to athletes’ in the conventional program. Compared to the Askling study mentioned previously, these time frames are markedly shorter, however this may be due to the difference in athletic level (recreational versus elite) between the two studies.40 Employing lumbopelvic stability interventions theoretically enhances the length tension capacity of the hamstring muscle group by stabilizing proximal attachments and avoids unnecessary tension in the early phases of rehab that may limit tissue healing.32 Single leg windmills (Figure 7) can be utilized to simultaneously enhance stability of both hamstring and lumbopelvic muscles. Addition of rotational movements and single leg positions to hamstring lengthening exercise challenges both lumbopelvic stability and eccentric loading. Standard planks can be progressed to single leg positions that enhance unilateral and rotational stability. Single leg planks (The Bunkie Test) have been described in the literature as both and intervention and advanced measure of functional stability (Figure 8).88 A case study has correlated this test with quantitative and a qualitative strength measures, however future research is required to determine reliability and validity of this test.89 Jumping and landing tasks to correct compensatory patterns and introduce rapid hamstring activation should be utilized to prepare the tissue for the demands of jogging and sport‐specific activity. Considering the dual innervation of the biceps femoris, rapid movements, such as speed kick‐backs (Figure 9) and foot catches (Figure 10) should be considered to train muscle activation at a higher velocity specific to sport.
Figure 7.

Single leg windmills
Figure 8.

Single leg planks – The “Bunkie” test utilizes 5 single leg plank testing positions performed bilaterally with the goal to reach 40s for endurance athletes.88
Figure 9.
Rapid kickbacks – Athlete uses a free motion treadmill to rapidly kick back in a running motion. Emphasis is placed on quick turn over.
Figure 10.

Foot catches ‐ Described by Worrell10 and Sherry30, the athlete stands with the involved leg in extended position. The athlete is able to touch the wall for balance and rapidly contracts the quadriceps in order “catch” the foot using eccentric hamstring contraction.
If the clinical exam demonstrates no signs of lingering HSI, high‐speed dynamic testing can be used to assess the muscle's response to quick lengthening movements. One such test described by Askling and colleagues has been proposed.39 The H‐test utilizes a rapid active straight leg raise of the involved limb while the pelvis and opposite leg is stabilized. (Figure 11) Three trials are performed with the athlete grading the subjectively reported level of insecurity on a 0‐100 scale. If any insecurity is reported by the athlete, the rehabilitation program is extended and testing is performed every 3‐5 days until no insecurity is reported. The H‐test has been shown to have good reliability and construct validity, however its prognostic value to for HSI recurrence has not been reported.39 Although limited evidence exists for this test, it does help extend rehabilitation time for those athletes that appear normal with clinical testing, but demonstrate impairments with high velocity movements. Considering the high recurrence rate of HSI, this may be a useful tool for the healthcare providers to lessen the risk of premature return to sport. Criteria to advance into sport include a normal clinical exam, active knee extension less than 108 in supine testing position, less than 10% limb symmetry difference with isokinetic and functional testing, and no insecurity (0/100) on the H‐test.
Figure 11.
H‐test described by Askling39, the athlete is instructed to perform a rapid SLR for 3 trials.
CONCLUSION
Hamstring injuries and recurrence continue to challenge healthcare professionals and athletes. Both non‐modifiable and modifiable risk factors have been reported in the literature, however high quality studies are needed to identify important modifiable risk factors and preventative programs aimed at reducing recurrence.29,37 Rehabilitation programs focused on eccentric loading in a lengthened position and lumbopelvic stability demonstrate effective strategies in reducing recurrence after injury.30,38,85,87 Dynamic and functional testing techniques may be useful in predicting return to injury time and identifying impairment when clinical exam appears normal.12 Further research is warranted to identify effective preventative interventions, prognostic indicators, and comprehensive return to sport criteria that could be used to reduce high rates of HSI recurrence.
Appendix A
Rehab Progression for Hamstring Injuries.
| Non‐operative Progression* | Operative Progression* |
|---|---|
| Phase I | Phase I (0‐4 wks) |
| Goals: Minimize pain and edema, scar development protection, minimize atrophy. | Goals: Protection, soft_tissue healing |
| Precautions: End range stretching | Precautions: Avoid deep hip flexion and combined hip flexion and knee extension movements |
Suggested interventions:
|
Suggested interventions:
|
Criteria to advance to Phase II:
|
Criteria to advance to Phase II:
|
| Phase II: | Phase II (5‐12 wks) |
| Goals: Increase neuromuscular control of trunk and pelvis, increase pain free hamstring flexibility | Goals: Protected strengthening. balance/stability progression |
| Precautions: Early progression | Precautions: Avoid eccentric load in lengthened position, no dynamic stretching |
Suggested interventions:
|
Suggested interventions:
|
Criteria to progress to Phase III:
|
Criteria to progress to Phase III:
|
| Phase IE | Phase III (12wks ‐ 16wks): |
| Goals: Asymptomatic with all activities, normal strength through full ROM, combine postural control and sports specific motions. | Goals: Eccentric and lengthen loading, slowly increase velocity of exercise |
| Precautions: Premature return to sport | Precautions: No provocation of symptoms with exercise |
Suggested Interventions:
|
Suggested Interventions:
|
Criteria for progression to Phase IV:
|
Criteria to progress to Phase IV:
|
| Phase IV: Return to sport, maintenance and prevention | Phase IV (4‐6 mths): |
| Goals: Sports specific and rapid movements, correct modifiable risk factors | Follow non‐op Phase IV recommendations |
Precautions: No provocation with training Suggested interventions:
|
|
Return to Sport Criteria
| |
Non‐operative timeframes based on criterion, operative timeframes based on criterion and soft tissue healing guidelines.
REFERENCES
- 1.Feeley BT Kennelly S Barnes RP Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;236(8):1597‐1603. [DOI] [PubMed] [Google Scholar]
- 2.Heiser TM Weber J Sullivan G, et al. Prophylaxis and management of hamstring muscle injuries in intercollegiate football players. Am J Sports Med 1984;12(5):368‐70. [DOI] [PubMed] [Google Scholar]
- 3.Brughelli M Cronin J Levin G Chaouachi A Understanding change of direction ability in sport. Sports Medicine 2008; 38 (12): 1045‐1063 [DOI] [PubMed] [Google Scholar]
- 4.Brooks JH Fuller CW Kemp SP, et al. Incidence, risk, and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34 (8):1297‐306. [DOI] [PubMed] [Google Scholar]
- 5.Orchard JW Intrinsic and extrinsic risk factors for muscle strains in Australian football. Am J Sports Med. 2001;29:300–3. [DOI] [PubMed] [Google Scholar]
- 6.Bennell KL Crossley K Musculoskeletal injuries in track and field: incidence, distribution and risk factors. Aust J Sci Med Sport. 1996;28(3):69‐75 [PubMed] [Google Scholar]
- 7.Woods C Hawkins RD Maltby S, et al. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of hamstring injuries. Br J Sports Med. 2004;38:36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Foreman TK Addy T Baker S Burns J Hill N Madden T Prospective studies into the causation of hamstring injuries in sport: a systematic review. Phys Ther in Sport. 2006;7:101‐109. [Google Scholar]
- 9.Gabbe BJ Bennell KL Finch CF Why are older Australian football players at greater risk of hamstring injury? J Sci Med Sport. 2006;9:327‐333. [DOI] [PubMed] [Google Scholar]
- 10.Worrell TW Factors associated with hamstring injuries. An approach to treatment and preventative measures. Sports Med. 1994;17:338‐345. [DOI] [PubMed] [Google Scholar]
- 11.Orchard JW Best TM The management of muscle strain injuries: an early return versus the risk of recurrence. Clin J Sport Med. 2002;12:3‐5. [DOI] [PubMed] [Google Scholar]
- 12.Malliaropoulos N Isinkaye T Tsitas K, et al. Re‐injury after acute posterior thigh muscle injuries in elite track and field athletes. Am J Sports Med 2011;39:304–10. [DOI] [PubMed] [Google Scholar]
- 13.Petersen J Thorborg K Nielsen MB, et al. Acute hamstring injuries in Danish elite football: a 12‐month prospective registration study among 374 players. Scand J Med Sci Sports 2010;20:588–92. [DOI] [PubMed] [Google Scholar]
- 14.Verrall GM Slaotinek Barnes PG, et al. Clinical risk factors for hamstring muscle strain injury: a prospective study with correlation of injury by magnetic resonance imaging. Br J Sports Med. 2001;35(6):435‐439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arnason A Sigurdsson SB Gudmundsson A, et al. Risk factors for injuries in football. Am J Sports Med 2004; 32 (1 Suppl.):5S‐16S. [DOI] [PubMed] [Google Scholar]
- 16.Hägglund M Waldén M Ekstrand J Previous injury as a risk factor for injury in elite football: a prospective study over two consecutive seasons. Br J Sports Med. 2006; 40 (9): 767‐772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henderson G Barnes CA Portas MD Factors associated with increased propensity for hamstring injury in English Premier League soccer players. J Sci Med Sport. 2010;13(4):397‐402. [DOI] [PubMed] [Google Scholar]
- 18.Bennell K Wajswelner H Lew P, et al. Isokinetic strength testing does not predict hamstring injury in Australian Rules footballers. Br J Sports Med. 1998;32(4):309‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Croisier JL Forthomme B Namurois MH, et al. Hamstring muscle strain recurrence and strength performance disorders. Am J Sports Med. 2002;30(2):199‐203. [DOI] [PubMed] [Google Scholar]
- 20.Croisier JL Ganteaume S Binet J, et al. Strength imbalances and prevention of hamstring injury in professional soccer players: a prospective study. Am J Sports Med. 2008;36(8):1469‐75. [DOI] [PubMed] [Google Scholar]
- 21.Orchard JW Marsden J Lord S, et al. Preseason hamstring muscle weakness associated with hamstring muscle injury. Am J Sports Med. 1997;25(1):81‐5. [DOI] [PubMed] [Google Scholar]
- 22.Sugiura Y Saito T Sakuraba K, et al. Strength deficitsidentified with concentric action of the hip extensors and eccentric action of the hamstrings predispose to hamstring injury in elite sprinters. J Orthop Sports Phys Ther. 2008;38(8):457‐464. [DOI] [PubMed] [Google Scholar]
- 23.Hennessey L Watson AW Flexibility and posture assessment in relation to hamstring injury. Br J Sports Med 1993;27(4):243‐246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bradley PS Portas MD The relationship between preseason range of motion and muscle strain injury in elite soccer players. J Strength Cond Res. 2007; 21(4):1155‐9. [DOI] [PubMed] [Google Scholar]
- 25.Worrell TW Perrin DH Hamstring muscle injury: the influence of strength, flexibility, warm‐up, and fatigue. J Orthop Sports Phys Ther. 1992; 16 (1): 12‐18. [DOI] [PubMed] [Google Scholar]
- 26.Mair SD Seaber AV Glisson RR, et al. The role of fatigue in susceptibility to acute muscle strain injury. Am J Sports Med 1996;24(2):137‐43. [DOI] [PubMed] [Google Scholar]
- 27.Devlin L Recurrent posterior thigh symptoms detrimental to performance in rugby union: predisposing factors. Sports Med. 2000;29 (4): 273‐287. [DOI] [PubMed] [Google Scholar]
- 28.Freckleton G Pizzari T Risk factors for hamstring muscle strain injury in sport: a systematic review and meta‐analysis. Br J Sports Med. 2013;47(6):351‐358. [DOI] [PubMed] [Google Scholar]
- 29.Cameron ML Adams RD Maher CG Mission D Effect of HamSprint drills training programme on lower limb neuromuscular control in Australian football players. J Sci Med Sport. 2007;12:24‐30. [DOI] [PubMed] [Google Scholar]
- 30.Sherry MA Best TM A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Ortho Sports Phys Ther. 2004;34:116‐125. [DOI] [PubMed] [Google Scholar]
- 31.Garrett WE Jr. Muscle strain injuries. Am J Sports Med. 1996;24:S2–8. [PubMed] [Google Scholar]
- 32.Orchard JW Biomechanics of muscle strain injury. New Zealand J Sports Med. 2002;30:92‐98. [Google Scholar]
- 33.Chumanov ES Heiderscheit BC Thelen DG The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40:3555‐3562. [DOI] [PubMed] [Google Scholar]
- 34.Thelen DG Chumanov ES Best TM Swanson SC Heiderscheit BC Simulation of biceps femoris musculotendon mechanics during the swing phase of sprinting. Med Sci Sports Exerc. 2005;37:1931‐1938. [DOI] [PubMed] [Google Scholar]
- 35.Yu B Queen RM Abbey AN Liu Y Moorman CT Garrett WE Hamstring muscle kinematics and activation during overground sprinting. J Biomech. 2008;41:3121‐3126. [DOI] [PubMed] [Google Scholar]
- 36.Thelen DG Chumanov ES Hoerth DM, et al. Hamstring muscle kinematics during treadmill sprinting. Med Sci Sports Exerc. 2005;37:108‐114. [DOI] [PubMed] [Google Scholar]
- 37.Opar DA Williams MD Shield AJ Hamstring strains: factors that lead to injury and re‐injury. Sports Med. 2012;42(3):209‐226. [DOI] [PubMed] [Google Scholar]
- 38.Heiderscheit BC Sherry MA Slider A, et al. Hamstring strain injuries: recommendations for diagnosis, rehabilitation and injury prevention. J Ortho Sports Phys Ther. 2010;40(2):67‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Askling CM Nilsson J Thorstensson A A new hamstring test to complement the common clinical examination before return to sport after injury. Knee Surg Sports Traumatol Arthrosc. 2010;18:1798–803. [DOI] [PubMed] [Google Scholar]
- 40.Askling CM Tengvar M Tarassova Thorstensson A Acute hamstring injuries in Swedish elite sprinters and jumpers: a prospective randomized controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2014;48(7):532‐9. [DOI] [PubMed] [Google Scholar]
- 41.Askling CM Tengvar M Saartok T Thorstensson A Proximal hamstring strains of stretching type in different sports: injury situations, clinical and magnetic resonance imaging characteristics, and return to sport. Am J Sports Med. 2008;36:1799‐1804. [DOI] [PubMed] [Google Scholar]
- 42.Cohen SB Towers JD Zoga A, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3:423‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fuller CW Ekstrand J Junge A, et al. Consensus statement on injury definitions and data collection procedures in studies of football (soccer) injuries. Scand J Med Sci Sports. 2006;16:83‐92. [DOI] [PubMed] [Google Scholar]
- 44.Slavotinek JP Verrall GM Fon GT Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol. 2002;179(6):1621‐1628. [DOI] [PubMed] [Google Scholar]
- 45.Verrall GM Slavotinek JP Barnes PG, et al. Diagnostic and prognostic value of clinical findings in 83 athletes with posterior thigh injury: comparison of clinical findings with magnetic resonance imaging documentation of hamstring muscle strain. Am J Sports Med. 2003;31:969‐973. [DOI] [PubMed] [Google Scholar]
- 46.Parker L Nazarian LN Carrino JA, et al. Musculoskeletal imaging: Medicare use, costs, and potential for cost substitution. J Am Coll Radiol. 2008;5:182‐188. [DOI] [PubMed] [Google Scholar]
- 47.Connell DA, ME Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975‐984. [DOI] [PubMed] [Google Scholar]
- 48.Petersen J Thoborg Nielsen MB, et al. The diagnostic and prognostic value of ultrasonography in scocer players and actue hamstring injuries. Am J Sports Med, 2014;42(2):399‐404. [DOI] [PubMed] [Google Scholar]
- 49.Gabbe BJ Bennell KL Wajswelner et al. , Reliability of common lower extremity musculoskeletal screening tests. Phys Ther Sport. 2004;5:90–97. [Google Scholar]
- 50.Schneider‐Kolsky ME Hoving JL Warren P, et al. A comparison between clinical assessment and magnetic resonance imaging of acute hamstring injuries. Am J Sports Med. 2006;34:1008‐1015. [DOI] [PubMed] [Google Scholar]
- 51.Warren P Gabbe BJ Scheider‐Kolsky M et al. Clinical predictors of time to return to competition and of recurrence following hamstring strain in elite Australian footballers. Br J Sports Med. 2010;44(6):415‐419. [DOI] [PubMed] [Google Scholar]
- 52.Reiman MP Loudon JK Goode AP Diagnostic accuracy of clinical tests for assessment of hamstring injury: a systematic review. J Orthop Sports Phys Ther. 2013;43(4):223‐231. [DOI] [PubMed] [Google Scholar]
- 53.Cohen S Bradley J Acute proximal hamstring rupture . J Am Acad Orthop Surg. 2007;15:350–355. [DOI] [PubMed] [Google Scholar]
- 54.Kendall FP McCreary EK Provance PG Rodgers MM Romani WA 5th. Muscles: Testing and Posture with Function and Pain. Baltimore: Lippincott, Williams & Wilkins; 2005. [Google Scholar]
- 55.Magee DJ 5th. Orthopedic Physical Assessment. St. Loius: Saunders; 2008. [Google Scholar]
- 56.Kornberg C Lew P The effect of stretching neural structures on grade on hamstring injuries. J Ortho Sports Phys Ther. 1989;10:481‐487. [DOI] [PubMed] [Google Scholar]
- 57.Freckleton G Cook J Pizzari T The predictive validity of a single leg bridge test for hamstring injuries in Australian rules football players. Br J Sports Med. 2014;48:713‐717. [DOI] [PubMed] [Google Scholar]
- 58.Orchard JW Farhart P Leopold C Lumbar spine region pathology and hamstring and calf injuries in athletes: is there a connection? Br J Sports Med. 2004;38:502‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Turl SE George KP Adverse neural tension: a factor in repetitive hamstring strain? J Ortho Sports Phys Ther. 1998;27:16‐21. [DOI] [PubMed] [Google Scholar]
- 60.Lorenz D Reiman M The role and implementation of eccentric training in athletic rehabilitation: tendinopathy, hamstring strains, and acl reconstruction. Int J Sports Phys Ther. 2011:6(1):27‐44. [PMC free article] [PubMed] [Google Scholar]
- 61.Brockett CL Morgan DL Proske U Predicting hamstring strain injury in elite athletes. Med Sci Sports Exerc. 2004;36:379‐87. [DOI] [PubMed] [Google Scholar]
- 62.Proske U Morgan DL Brockett CL Percival P Identifying athletes at risk of hamstring strains and how to protect them. Clin Exp Pharmacol Physio. 2004;31:546‐550. [DOI] [PubMed] [Google Scholar]
- 63.Brockett CL Morgan DL Proske U Human hamstring muscles adapt to eccentric exercise by changing optimum length. Med Sci Sports Exerc. 2001;33:783‐790 [DOI] [PubMed] [Google Scholar]
- 64.Kietrys DM Palombaro KM Azzaretto E, et al. Effectiveness of dry needling for upper quarter myofascial pain: a systematic review and meta‐analysis. J Ortho Sports Phys Ther. 2013;43: 620‐634. [DOI] [PubMed] [Google Scholar]
- 65.Dembowski SC Westrick RB Zylstra E Johnson MR Treatment of hamstring strain in a collegiate pole‐vaulter integrating dry needling with an eccentric training program: a resident's case report. Int J Sports Phys Ther. 2013;8(3):328‐339. [PMC free article] [PubMed] [Google Scholar]
- 66.Dommerholt J Huijbregts P Myofascial Trigger Points: Pathophysiology and Evidence‐infromed Diagnosis and Management. Sudbury, MA: Jones and Bartlett; 2011 [Google Scholar]
- 67.Feeley BT Kennelly S Barnes RP, et al. Epidemiology of national football league training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597‐1603. [DOI] [PubMed] [Google Scholar]
- 68.American Physical Therapy Association Description of Dry Needling in Clinical Practice: An Educational Resource Paper. Alexandria, Virginia: 2013 [Google Scholar]
- 69.Jayaseelan DJ Mosts N Ricardo CR Rehabilitation of proximal hamstrings tendinopthy utilizing eccentric training, lumbopelvic stabilization, and trigger point dry needling:2 case reports. J Orthop Sports Phys Ther. 2014;44(3):198‐205. [DOI] [PubMed] [Google Scholar]
- 70.Jarvinen TA Jarvinen TL Kaariainen M, et al. Muscle injuries: optimizing recovery. Best Pract Res Clin Rheumatol. 2007;21:317‐331. [DOI] [PubMed] [Google Scholar]
- 71.Barnett AJ Negus JJ Barton T Reattachment of the proximal hamstring origin: outcome in patients with partial and complete tears. Knee Surg Sports Traumatol Arthrosc. 2014. access at pubmed.gov [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 72.Brucker PU Imhoff AB Functional assessment after acute and chronic complete ruptures of the proximal hamstring tendons. Knee Surg Sports Traumatol Arthrosc. 2005;13:411–418. [DOI] [PubMed] [Google Scholar]
- 73.Cross MJ Vandersluis R Wood D, et al. Surgical repair of chronic complete hamstring tendon rupture in the adult patient. Am J Sports Med. 1998;26:785–788. [DOI] [PubMed] [Google Scholar]
- 74.Birmingham P Muller M Wickiewicz T, et al. Functional outcome after repair of proximal hamstring avulsions. J Bone Joint Surg Am. 2011;93(19):1819‐1826. [DOI] [PubMed] [Google Scholar]
- 75.De Smeet AA Best TM MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am J Roentgenol. 2000;174:393–399. [DOI] [PubMed] [Google Scholar]
- 76.Koulouris G Connell D Evaluation of the hamstring muscle complex following acute injury. Skeletal Radiol. 2003;32:582‐9. [DOI] [PubMed] [Google Scholar]
- 77.Sallay PI Friedman RL Coogan PG, et al. Hamstring muscle injuries among water skiers functional outcome and prevention. Am J Sports Med. 1996;24:130–136. [DOI] [PubMed] [Google Scholar]
- 78.Anzel J Covey K Weiner A Disruption of muscles and tendons. An analysis of 1014 cases. Surgery 1959;45:406–414. [PubMed] [Google Scholar]
- 79.Carmichael J Packham I Trikha S Wood D Avulsion of the proximal hamstring origin. Surgical technique. J Bone Joint Surg Am. 2009;91:249–256. [DOI] [PubMed] [Google Scholar]
- 80.Wood DG Packham I Trikha SP, et al. Avulsion of the proximal hamstring origin. J Bone Joint Surg Am. 2008;90:2365‐2374. [DOI] [PubMed] [Google Scholar]
- 81.Sarimo J Lempainen L Mattila K, et al. Complete proximal hamstring avulsions: A series of 41 patients with operative treatment. Am J Sports Med. 2008;36:1110‐1115. [DOI] [PubMed] [Google Scholar]
- 82.Konan S Haddad F Successful return to high level sports following early surgical repair of complete tears of the proximal hamstring tendons. Int Orthop. 2010;34:119‐123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lempainen L Sarimo J Heikkilä J Mattila K Orava S Surgical treatment of partial tears of the proximal origin of the hamstring muscles. Br J Sports Med. 2006;40:688‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Harris JD Griesser MJ Best TM Ellis TJ Treatment of proximal hamstring rupture‐a systematic review. Int J Sports Med. 2011;32:490‐495. [DOI] [PubMed] [Google Scholar]
- 85.Domb BG Linder D Sharp KG, et al. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013;2(1):e35‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Askling CM Koulouris G Saartok T Werner S Best TM Total proximal hamstring ruptures: clinical and MRI aspects including guidelines for postoperative rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2013;21(3):515‐33. [DOI] [PubMed] [Google Scholar]
- 87.Schmitt B Tyler T McHugh Hamstring injury rehabilitation and prevention of re‐injury using lengthened state eccentric training: a new concept. Int J Sports Phys Ther. 2010;7(3):333‐341. [PMC free article] [PubMed] [Google Scholar]
- 88.Askling CM Tengvar M Thorstensson A Acute injuries in Swedish elite football: a prospective randomized controlled clinical trial comparing two rehabilitation protocols. Br J Sports Med. 2013;47(15):953‐9. [DOI] [PubMed] [Google Scholar]
- 89.de Witt B Venter R The ‘Bunkie Test’ test: assessing functional strength to restore function through fascia manipulation. J Body Mov Ther. 2009;13(1):81‐88. [DOI] [PubMed] [Google Scholar]
- 90.Brumitt J Successful rehabilitation of recreational endurance runner: interial validation for the Bunkie test. J Bodyw Mov Ther. 2011;15(3):384‐390. [DOI] [PubMed] [Google Scholar]
- 91.Hallet P A reliability study examining the inter‐ and intra‐observer reliability of the muscle capacity tests included in the ECB musculoskeletal screening protocol [Masters]. University of Nottingham, 2010. [Google Scholar]