Abstract
Rehabilitation following hip arthroscopy for femoroacetabular impingement (FAI) and labral‐chondral dysfunction has evolved rapidly over the past 15 years. There have been multiple commentaries published on rehabilitation following hip arthroscopy without any published standardized objective criteria to address the advancement of the athlete through the phases of rehabilitation. The purpose of this clinical commentary is to describe a criteria driven algorithm for safe integration and return to sport rehabilitation following hip arthroscopy. The criteria based program allows for individuality of the athlete while providing guidance from early post‐operative phases through late return to sport phases of rehabilitation. Emphasis is placed on the minimum criteria to advance including healing restraints, patient reported outcomes, range of motion, core and hip stability, postural control, symmetry with functional tasks and gait, strength, power, endurance, agility, and sport‐specific tasks. Evidence to support the criteria will be offered as available. Despite limitations, this clinical commentary will offer a guideline for safe return to sport for the athlete while identifying areas for further investigation.
Level of Evidence:
5
Keywords: Arthroscopy, hip, rehabilitation
INTRODUCTION
Despite a slight downward trend in youth participation of the four most popular U.S. team sports from 2008‐2012 and increasing high school sport participation, health and wellness awareness is a reason for an increasing athletic population. This population includes anyone with goals to return to participation at any level of organized or recreational sporting activity. In the absence of arthritis, acetabular labral tears and femoroacetabular impingement (FAI) has received significant attention as a potential etiology of hip pain in this athletic population.1-3 Advancements in diagnostic imaging and understanding of the hip clinical examination have lead to more definitive diagnoses of FAI and labral pathology as a source of non‐arthritic hip pain than in the past.4-7 The evolution of surgical instruments and techniques utilized to correct labral pathology and FAI has led to improved patient outcomes, and arthroscopic intervention outcomes are similar to open techniques which has historically been considered the gold standard for treatment of these disorders.1,8-12 Hunt et al found conservative treatment in non‐arthritic hip pain patients with high levels of pre‐operative function was less successful than surgery.13 In this study, the more active a subject was, the more likely they chose to undergo surgery and those subjects who were more active prior to surgery tended to have better outcomes.13
Positive outcomes occur following hip arthroscopy to correct FAI and labral pathology given the appropriate rehabilitation.9,10,12-18 Post‐operative rehabilitation following hip arthroscopy has been described in clinical commentaries and case reports or series.9,18-29 Most authors describe the rehabilitation process by the utilization of a phased program. While the majority of programs describe four‐phases, three and five‐phase programs are also described.23,26 The initial phase is consistently time based and dependent on the procedures performed, with the subsequent phases described as individualized and criteria driven. Progression through each phase must address certain goals, be based on objective criteria, and follow certain precautions. The specific goals of each of the phases were described by several authors23,24 and only a few also included objective criteria in order to advance through the phases.18-20,22,26,29 To the authors’ knowledge, no paper has emphasized, focused on, or described in detail an objective, evidence‐based and criteria‐based progression through all phases of rehabilitation to return to sport.
Rehabilitation protocols provided in the current literature describe broad transitional periods during the rehabilitation process. These transitional periods include the elimination of the early post‐operative precautions, changes in weight‐bearing restrictions, increasing activities of daily living (ADLs), walking distance and speed; changes from endurance to power to agilities; single to tri‐planar and functional exercises; and sport specific progressions including running, skating, throwing, hitting, and kicking.
Complications or delays in the rehabilitation process tend to occur during transitional periods.24 Tendonitis of the hip flexor or adductors, joint edema and irritation, soft tissue imbalance and faulty movement patterns, and low back or sacral‐iliac pain are common rehabilitation complications.9,24 These complications may be failure of the patient or therapist to follow precautions or prescribed treatments; but have also been found to be the result of unintentionally overloading the joint and soft tissues during these transitional periods.
It is critical to monitor the amount and type of loads that are applied to the joint during the transitional periods. In order to determine whether the joint and soft tissues can sustain the loads being applied it is crucial to have subjective and objective criteria for the athlete's readiness to progress and the rehabilitation specialist's ability to safely guide the rehabilitation. The athletically active population is already predisposed to joint overloading by their eagerness to return to sport. Consequently, the goal of this clinical commentary is to offer an objective, evidence‐based, criteria based progression through all critical transitional stages from surgery to return to sport.
The traditional phases of rehabilitation as described in literature will not be utilized in this commentary. Instead the authors will describe the transitional periods during the rehabilitation process that should require minimal criteria to advance. The rehabilitation specialist has the ability to utilize these criteria within the framework of their three‐, four‐, or five‐phased program.
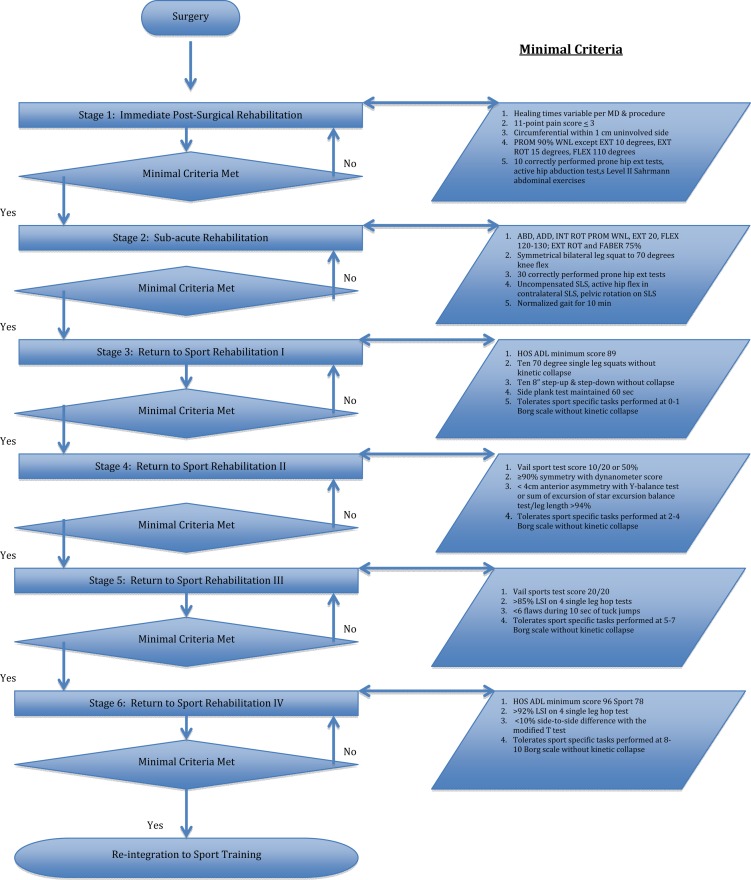
The stages the authors will describe include immediate post‐surgical rehabilitation (traditionally phase 1); the transition to sub‐acute rehabilitation and normalization of gait and ADLs (traditionally phase 2); and the transition to the return to sport stages with multiple levels (traditionally phase 3, phases 3‐4, or phases 3‐5). The goals of each stage are briefly described followed by the minimal criteria to advance.
Immediate post‐operative rehabilitation
Stage 1: Starts immediately from the operating room until the first transition occurs when physician and procedure guided timelines allow. Goals: The overall goal is to address articular and soft tissue deficits expected immediately following surgery. Specific goals include: (1) Protection of healing tissues, (2) reduction of pain and inflammation, (3) reducing the risks of scar adhesions, (4) restoring passive and active ranges of motion (ROM) within the prescribed guidelines and (5) re‐establishing proper neuromuscular firing patterns during single‐planar movements. Elimination of post‐surgical swelling and inflammation contributes to decreased pain, increased ROM, and reduced muscle guarding and inhibition while increased mobility reduces the risks of scar adhesions.30 Faulty motor control and muscular imbalances of the lumbo‐pelvic‐hip region reduces stability and can create shearing forces detrimental to proper healing of the repaired tissue especially during the transition to weight‐bearing activities.31
Stage 1 Criteria to Advance: Proper assessment of the joint, soft tissues, and motor control is achieved utilizing: (1) basic science healing time recommendations, (2) verbal 11‐point pain scale < 3, (3) circumferential measures within 1cm uninvolved side, (4) passive ROM 90% WNL except extension to be equal to 10 degrees, external rotation 15 degrees, flexion 110 degrees, (5) correct performance of 10 prone hip extension tests, 10 active hip abduction tests, and 10 level II Sahrmann abdominal exercises.
Rationale and Descriptions for Stage 1 Criteria: Timelines for specific ROM restrictions and weight‐bearing precautions are extremely variable in the literature, due to physician preference and surgical procedure. It is beyond the scope of this commentary to provide all reported timelines; however, the authors feel it is imperative to follow all precautions provided by the surgeon before transitioning to Stage 2. Of importance when considering timelines, arthroscopically repaired labrums in the ovine model may take up to 12 weeks without immobilization to adequately heal.32 Controlled stresses within and surrounding the hip joint prevent shortening of developing scar tissue and forces applied ensure appropriate fiber alignment and strength.33 These forces applied need to be controlled to prevent re‐injury, an abnormal inflammatory response, and resultant joint edema. Increased edema decreases activation firing of the gluteal muscles,34 which is essential for proper stabilization and propulsion during human locomotion.
The verbal 11‐point pain scale is a reliable measure used to quantify pain levels.35 The verbal 11‐point scale was chosen due to its sensitivity to detect change and as a more user‐friendly pain assessment tool than the VAS during the immediate post‐operative period.35,36 A score of one to four represents mild pain or distress and should not provoke muscular inhibition due to pain.37 The authors’ therefore recommend a score of 3 or less. It is not uncommon for the athlete to report mild complaints of discomfort from extra‐articular symptoms, muscle soreness or a pinching sensation when progressing to Stage 2.
Inflammation increases the risks of arthrogenic neuromuscular inhibition that produces selective inhibition of the extensor musculature complemented by flexor musculature hyper‐activation in the knee.38 Freeman et al. showed hip joint effusion is a significant contributor to gluteal inhibition in the hip.34 The gluteal muscle group is critical in hip stability during gait; therefore ensuring minimal to no joint effusion prior to weight bearing is critical. Accumulating intra‐articular volume measurements are not feasible in the clinical setting. Although circumferential measurements may be performed, they may only detect fluid within the superficial layers of soft tissue surrounding the hip and not within the joint itself. However they are currently the best available tool to assess for swelling in the clinical setting. The authors recommend less than one centimeter difference between the involved and the uninvolved hip measured greater trochanter to lesser trochanter parallel to the inguinal ligament. (Figure 2)
Figure 2.
Circumferential measurement used to determine swelling status.
Figure 1.
Flowchart to illustrate the stages of the rehabilitation process and the minimal criteria for progression throughout the stages.
Maximizing passive ROM and joint space while protecting the integrity of the repaired tissues until adequate healing has occurred is important. Passive ROM restrictions to reduce labral and capsular stress include extension, external rotation, and flexion.29,39 The authors recommend passive ROM 90% WNL for abduction (normal 30‐50 degrees), adduction (25‐30 degrees), and internal rotation (30‐40 degrees) and within functional limits (WFL) for walking and sitting for the restricted motions.33 Eighty‐four degrees of flexion is required for sitting in a standard chair and 104 degree average for transitioning sit to stand; therefore, the authors recommend minimal criteria of 110 degrees of passive flexion.40 During gait, 30 degrees of flexion is required at the end of the swing phase and 10 degrees of extension at terminal stance.41 Nine degrees of external rotation is necessary for terminal stance.42 The authors recommend minimal criteria of 10 degrees of passive extension and 15 degrees of passive external rotation in neutral extension.
A 24% increase in anterior hip joint force is generated with muscle force at the hip extension angle that occurs during the terminal stance phase of gait.43 Muscular imbalances and weakness increase these anterior hip forces.43 Assessment for adequate muscle strength during maximum isometrics using dynamometry or manual muscle testing is not recommended. The ability of the key muscle groups to adequately activate, the timing of the muscle firing patterns, and the ability to repeat these patterns is of greater importance than maximal isometric contractions. The prone hip extension test assesses the ability to fire the gluteus maximus while maintaining lumbo‐pelvic‐hip control by performing 10 repetitions of gluteus maximus contraction followed by hamstring activation during prone hip extension from 0‐10 degrees. Activation of the hamstring muscle group prior to the gluteal muscle group contributes to hip dysfunction and increased anterior hip forces.44 The abductor force contributions needed to stabilize a level pelvis during single leg weight‐bearing is 70% from the gluteal muscles inserting into the greater trochanter and 30% from muscles influencing tension in the ITB.45 The active hip abduction test assesses the ability to fire the gluteus medius while maintaining lumbo‐pelvic‐hip control during a sidelying frontal plane leg lift (description and scoring provided in Table 1).46 The authors recommend the athlete score 0 or 1 on 10 consecutive repetitions for adequate firing of the gluteus medius. Proper assessment for pelvic stability and minimal contribution from the tensor fascia latae (TFL) is critical. Increased anterior hip joint forces occur with the hip in extension if the iliacus and psoas muscle is weakened.43 Sufficient iliopsoas muscle activation is just as critical as the gluteal muscle groups during gait. A straight leg raise with a weakened iliopsoas muscle significantly increases anterior hip joint forces therefore is not recommended.44 Adequate iliopsoas activation can be safely assessed by requiring the athlete to properly perform 10 repetitions of the Sahrmann level II abdominal exercise.47 The primary contribution of hip flexion by the iliopsoas verses the rectus abdominus and TFL should be assessed with palpation during this test.
Table 1.
Scoring Criteria for the active Hip Abduction Test
| Score | Cues for Examiner |
|---|---|
| 0: Able to maintain position of pelvis in the frontal plane | Smoothly and easily performs movement; lower extremities, pelvis, trunk and shoulder remain aligned in the frontal plane |
| 1: Minimal loss of pelvis position in the frontal plane | Slight wobble at initiation or throughout movement; may show noticeable effort or "ratcheting" of moving limb |
| 2: Moderate loss of pelvis position in the frontal plane | Has at least 2 of the following: noticeable wobble through movement; tipping of pelvis, trunk, or shoulder rotation; increased hip flexion and/or rotation of the moving limb; rapid or uncontrolled movement |
| 3: Severe loss of pelvis position in the frontal plane | Has more than 3 of the above characteristics and/or unable to regain control of movement once lost or may lose balance by placing hand on table |
| Resource: Davis AM, Bridge P, Miller J, Nelson‐Wong E. Interrater and Intrarater Reliability of the Active Hip Abduction Test. JOSPT. 2011; 41(12}: 953‐960 |
Sub‐acute rehabilitation
Stage 2: Starts when the athlete begins crutch weaning through normalized gait, weight‐bearing ADLs, and reciprocal pattern ascending and descending stairs. Goals: The overall goal is to wean off crutches, normalize gait, and maintain neuromuscular control during weight‐bearing ADLs. Specific goals include: (1) restoration of full passive and active ROM, (2) demonstration of progressively improved strength of the gluteus maximus, gluteus medius, iliopsoas, and deep rotators, (3) demonstration of progressively improved postural and pelvic control with double leg and single leg balance activities, (4) normalized gait at athlete's preferred walking speed demonstrating good trunk, pelvic, and lower extremity neuromuscular control for 10 min.
Stage 2 Criteria to Advance: Proper assessment of gait and ADLs is achieved utilizing: (1) abduction, adduction, and internal rotation ROM WNL, passive extension 20 degrees, flexion 120‐130 degrees without an anterior pinching sensation, external rotation 75% (of 40‐60 degrees) and 75% FABER (flexion‐abduction‐external rotation), (2) symmetrical bilateral leg squat at 70 degree knee depth, (3) 30 correctly performed reps of prone hip extension test, (4) uncompensated single leg stance (SLS), active hip flexion in contralateral SLS, pelvic rotation on SLS (5) normalized gait 10 minutes.
Rationale and Descriptions for Stage 2 Criteria: The bilateral leg squat is a good assessment for adequate mobility of the ankles, knees and hips maintaining neutral spine and a precursor for the tuck jump. The authors recommend the ability to perform 10 symmetrical bilateral leg squats to 70 degrees of knee flexion without femoral adduction or internal rotation, pelvic hiking or posterior rotation, and postural control. The athlete should report no pinching sensation throughout the performance of this assessment.
Maximum isometric resistance assessment using dynamometry or manual muscle testing is still not recommended during this stage due to unnecessary stress on the muscles and joint. The authors recommend testing the gluteus maximus with the prone hip extension test from 0‐20 degrees extension, maintaining proper firing patterns, and pelvic control for 30 repetitions.
Challenging postural and pelvic control using variations of single limb stance allows for greater insight into weaknesses and proprioceptive concerns. The first SLS maneuver is the Trendelenburg test performed for 60 seconds with eyes open then eyes closed. The Trendelenberg test may not be useful for athletes demonstrating gluteus medius strength >30% body weight; however, marked weakness is commonly present at this stage and testing is useful.48 Contralateral pelvic drop, pelvic hike (compensated Trendelenburg), or pelvic rotation as seen with gluteus medius weakness is unacceptable. The second maneuver assesses the ability of the iliopsoas to flex the involved hip while in SLS on the uninvolved leg by performing 10 reps of active hip flexion from 20 degrees hip extension to 90 degrees flexion. Twenty degrees of extension is utilized to assess the iliopsoas' ability to initiate swing during gait through 90 degrees of flexion for stairs and pre‐athletic movements. Critical assessment includes no posterior rotation of the ipsilateral innominate or excessive pelvic rotation on the stance leg. The iliopsoas muscle should be the primary mover with minimal activation of the TFL and rectus femoris. The third maneuver assesses pelvic rotation on a fixed femur (closed kinetic chain rotation). This action of the acetabulum moving on the femur is common in many athletic movements of sport. The athlete internally then externally rotates the pelvis on the fixed stance leg 10 times through full range without compensation, pain, or kinetic collapse as noted above.
The athlete should demonstrate the ability to ambulate with a normalized gait including a symmetrical stride and good neuromuscular control for 10 minutes with no discomfort. Common gait abnormalities include early heel‐rise and shortened contralateral swing or increased anterior pelvic rotation and lumbar extension. Both are due to gluteal weakness in hip extension and the inability to stabilize the lumbo‐pelvic‐hip region from mid‐stance to toe‐off. Prior to introducing speed during ambulation and running progressions emphasis is placed on increasing endurance of the hip musculature with normal, overground ambulation. Muscle activation patterns are different and hip extensor and peak flexion moments are greater when walking on the treadmill versus overground walking.49 There is also the potential for differences in the peak ground reaction forces although there were inconsistencies in the methods of the studies.49-51 Walking over ground versus using a treadmill is recommended for increasing endurance.
Return to Sport Stages
Stage 3: The remaining 4 stages focus on re‐integration into sport. Neuromuscular control in SLS and gait has been achieved and emphasis is initially placed on sagittal, frontal, and transverse plane concentric/eccentric movements. The loads and volume of increasing ADLs, ambulation, and functional sport specific exercises beyond rehabilitation need to be carefully monitored and controlled, and timing between stages varies greatly. Goals: The overall goal is for the athlete to tolerate single limb support, single planar concentric/eccentric loading, and introduction of sport specific tasks. Specific goals include: (1) increase endurance with ambulation at the athlete's preferred walking speed for 30 min, (2) increase single leg squat strength to a depth of 70 degrees of knee flexion, (3) normalize ascending and descending an 8‐inch step demonstrating good neuromuscular control, (4) introduction and tolerance of basic functional sport specific tasks performed at a 0‐1 on the Borg rate of perceived exertion (RPE) scale.25,52-54
Stage 3 Criteria to Advance: Proper assessment of single plane concentric/eccentric movements is achieved utilizing: (1) Hip Outcome Score ADL minimal score of 89%, (2) 10 repetitions of a single leg squat to a depth of 70 degrees of knee flexion, (3) 10 repetitions of 8” step up and step down, (4) completion of a 60 second side plank test, (5) toleration of sport specific tasks without pain, loss of symmetry, and maintaining neuromuscular control at an intensity 0‐1 Borg RPE scale.
Rationale and Descriptions for Stage 3 Criteria: Patient‐reported outcome questionnaires for the athletic population must report higher levels of function without the potential of ceiling effects and be sensitive to change. The Western Ontario and McMaster Universities Arthritis Index (WOMAC), Hip disability and Osteoarthritis Outcome Score (HOOS), Lower Extremity Functional Scale (LEFS) have no evidence to support their use on patients following hip arthroscopy. The Modified Harris Hip Score (MHHS) and Non‐arthritic Hip Score is unable to detect changes at higher levels of function and the Copenhagen Hip and Groin Outcome Score (HAGOS) has been validated for conservative treatment of non‐arthritic hip pain. The International Hip Outcome Tool (iHOT‐33) is reliable, has construct validity, and responsive to change;55 however, it is long for clinical use. The iHOT‐12 was considered;56 however, the Hip Outcome Score (HOS) was chosen because it contained both ADL and Sports subscales so it could be utilized in the early stages of rehabilitation as well as the advanced stages.9,57-59 It was also chosen for its ability to be responsive during higher levels of physical ability.57,58 In the HOS validation study the authors compared reported activity levels by patients with their HOS ADL and Sport scores.58 The Sports subscale is not appropriate at stage 3 due to the athlete is not yet functioning at a high enough level in sport activities. The ADL subscale however would be appropriate at Stage 3 and therefore the authors recommend a score of >89% which correlated with the patient's self reported activity levels as near normal as the criteria to advance.
The single leg squat and a stepping maneuver (forward, retro, or lateral step up or down) are both clinical tests that are easy to administer and require no elaborate equipment. Test‐retest reliability of these two tests has been shown with three dimensional tracking systems (ETS);60 however, the use of electromyography (EMG) and ETS by researchers to track human movement is not practical in the clinical setting. These tests have been shown to be reliable tools in identifying patients with motor control deficits or muscle weakness.61,62 To the authors' knowledge there are no other easy to administer, reliable, valid, objective tests for the clinical setting used to assess the kinematics and muscle activation of the lower extremity during single leg weight‐bearing sagittal plane movements. These two tests are functional and provide the cornerstone for progression to advanced rehabilitation exercises and athletic movements.60,63,64 The percent of the maximum voluntary isometric contraction required by the gluteus maximus and medius during the single limb squat and forward step up are high when compared to exercises such as lunges, unilateral bridges, clams, and planks commonly utilized during rehabilitation.65 The potential risks of injury from the faster decelerating force absorbing requirements of more advanced tests such as agility or single leg hop assessments are not acceptable at Stage 3. Critical observation of a single leg squat includes equal weight‐bearing on the calcaneus, first and fifth metatarsal heads and no kinetic collapse described as excessive medial knee valgus moment, femoral adduction and internal rotation motion, contralateral pelvic drop, external or internal rotation, trunk forward or lateral lean. Depth of the squat obtained should be 70 degrees knee flexion allowing fingertip touch for balance while the athlete completes 10 repetitions.
The stepping maneuvers are safe, easy to administer, demonstrate test‐retest reliability, rank high for requiring high activation intensity for the gluteals.65 The patterns of muscle activation of the gluteus maximus, medius, and quadricep muscle groups during these exercises are consistent between the differing stepping maneuvers and therefore a good assessment using different movements.66 The authors recommend that the athlete should be able to complete 10 step‐ups and 10 step‐downs from an 8” step with fingertip touch for balance without collapse.
Frontal plane stability is assessed utilizing the side plank. In a literature review of studies evaluating gluteus medius activation during rehabilitation exercises by Reiman et al. the side plank had the highest maximum voluntary contraction and therefore a good assessment of the lumbo‐pelvic‐hip stability in the frontal plane.65 The authors recommend maintaining side plank position (while maintaining a neutral spine) for 60 seconds without compensation in the sagittal or transverse plane.
The demands of the athlete's sport can be broken down into simple tasks and performed at carefully prescribed repetitions, sets, distances, and speeds to monitor loads. Examples of basic functional sport specific tasks include tossing a ball; a light swing of bat; easy skating and gliding on the ice. Intensity is monitored with the Borg RPE scale. Specific examples for different sports are beyond the scope of this commentary; however refer to Pierce et al for an example of incorporating sport specific functional progressions throughout the latter stages of rehabilitation.25 Being present and/or videotaping the athlete perform these tasks is ideal. Working with the trainer and coaches to assist in identifying deficits and understanding the mechanics of these tasks is important as they will be your eyes and ears in monitoring the athlete. The authors recommend that the athlete be able to sustain a set program of tasks that are sport and position specific, appropriate for the level of the athlete, at an effort of 0‐1 on the Borg RPE scale without fatigue, pain, and loss of symmetry and neuromuscular control.25,52-54
Stage 4: This transitional period occurs as single plane controlled movements are replaced with multi‐planar dynamic movements requiring increased load accepting capabilities to absorb the forces through the lower extremity. Goals: Specific goals for this stage include: (1) restoration of isolated muscular strength, (2) restoration of single leg squat endurance for 90 seconds at a depth of 70 degrees of knee flexion with sport‐cord resistance placed under stance foot and hand‐held at the ipsilateral hip, (3) restoration and optimization of balance and proprioception in single leg stance at variable hip angles and visual inputs, (4) demonstration of multi‐planar movements and increased eccentric loading without kinetic collapse, (5) demonstration of functional sport specific tasks of increase volume and performed at an intensity of 2‐4 on the Borg RPE scale without kinetic collapse.
Stage 4 Criteria to Advance: Proper assessment of multi‐planar dynamic movements is achieved utilizing: (1) Vail Hip Sport Test Score of 10/20, (2) 90% symmetry with dynamometer strength testing of the hip in all planes including flexion, extension, abduction, adduction, internal and external rotation, (3) either composite Star Excursion Balance Test (SEBT) (normalized by the athlete's leg length) of >94% or <4 cm. anterior asymmetry on the Y‐Balance Test (LE YBT), (4) toleration of sport specific tasks without pain, loss of symmetry, and maintaining neuromuscular control at an intensity 2‐4 on Borg RPE scale.
Rationale and Descriptions for Stage 4 Criteria: The Vail Hip Sport Test is a sport‐cord resisted series of dynamic multi‐planar functional exercises utilized as a return to sport test (description and scoring provided in Table 2). The four exercises of the test include a single leg squat for 3 min (Video 1), lateral bounding for 100 seconds (Video 2), diagonal bounding for 100 seconds (Video 3), and forward lunge onto height for 2 minutes (Video 4). The original Vail Sport Test is the knee version of the test and is similar, using two of the four exercises. After modifying the scoring system of the original Vail Sport Test, Garrison et al. showed excellent inter‐intra tester reliability of the test.67 The Vail Hip Sport Test has not been shown to be reliable as currently scored; however clinically it has been an excellent and safe method to observe muscular strength, endurance, and the ability to produce and absorb multi‐planar forces without kinetic collapse. The authors recommend a score of 10/20 on the Vail Hip Sport Test as minimal criteria to advance.
Table 2.
Vail Hip Sports Test, with scoring criteria
| Exercise Type | Cues for Examiner | Goal | Score | Total |
|---|---|---|---|---|
| Single leg squat | Knee flexion 30‐70 degrees; reps without knee valgus [patella falls medial to great toe); avoids locking knee into extension; avoids patella beyond toe during flexion; maintain upright trunk | 3 min | 1 point every 30 seconds of proper performance | ____/6 |
| Lateral Bounding | Knee flexion > 30 at landing; reps without knee valgus; reps within landing boundaries; landing phase not exceeding 1 sec in duration | 100 sec | 1 point every 20 seconds of proper performance | ____/5 |
| Diagonal Bounding | Knee flexion > 30 at landing; reps without knee valgus; reps within landing boundaries; landing phase not exceeding 1 sec in duration | 100 sec | 1 point every 20 seconds of proper performance | ____/s |
| Forward Box Lunge | Hip flexion >110 at forward position; hip extension >10 degrees at back position; reps without pelvic hike or rotation | 2 min | 1 point every 30 seconds of proper performance | ____/4 |
| ____/20 |
The hand held dynamometer (HHD) is a device used during this stage in order to assess isolated muscular strength. The HHD has been proven reliable when clinically assessing the strength of the hip musculature.68,69 The single‐planar isolated muscle strength testing of the hip in all planes is now indicated and safe. Although not capable of addressing dynamic or functional ability, isolated isometric testing precedes functional assessments and the tri‐planar functional integration with all athletic demands. The testing should find the involved hip to be >90% of the uninvolved hip with isolated isometric testing in all planes including flexion, extension, abduction, adduction, internal and external rotation. There currently is no available research for describing the relationship between dynamometer hip strength and levels of function.
The authors recommend either the use of the SEBT or the LE YBT. Three reach directions of the original SEBT including anterior, posteromedial, and posterolateral are recommended based on an analysis study by Hertel et al to reduce redundancy and time to perform the test.70 The LE YBT is conducted on a commercially available device or using tape on the floor in order to measure the three directions. Both the SEBT with only three measures and the LE YBT are executed similarly; however, the supporting research for this criteria utilized the different test therefore the authors offer either as an option for this criteria. Plisky et al found that if the sum of the reach distance of the anterior, posteromedial and posterolateral direction of the SEBT (normalized by the patient's leg length) was <94% the athlete was 6.5 times more likely to sustain a lower extremity injury.71 Smith et al found that an anterior asymmetry >4 cm on the LE YBT was associated with increased risk of non‐contact injury in Division 1 collegiate athletes.72 Therefore if using the SEBT the authors recommend the minimal criteria to advance of this score is >94% and if using the LE YBT the authors recommend less than 4 cm anterior asymmetry.
The simple tasks of the athlete's sport initiated during stage three are continued with increased repetitions, sets, distances and speeds. The number of functional sport specific tasks being performed may also be increased although the authors recommend adding them one at a time. The authors recommend the athlete tolerate this increase in volume of their sport specific tasks performed at an intensity of 2‐4 on the Borg scale without pain and kinetic collapse.
Stage 5: This transitional period occurs as increasing dynamic multi‐planar load accepting capabilities are reinforced and power and speed are introduced. Goals: Specific goals for this stage include: (1) restoration of single leg resisted squat to 70 degree depth for 3 min, (2) restoration of dynamic resisted tri‐planar single limb movements, (3) restoration of power and introduction of plyometric strengthening tasks, (4) demonstration of advanced functional sport specific tasks of increased volume and performed at an intensity of 5‐7 on the Borg RPE scale without kinetic collapse.
Stage 5 Criteria to advance: Proper assessment of endurance and power is achieved utilizing: (1) Vail Hip Sports Test score 20/20, (2) >85% limb symmetry index (LSI) on single limb hop test(s), (3) <6 flaws in 10 seconds with tuck jump assessment, (4) toleration of sport specific tasks without pain, loss of symmetry, and maintaining neuromuscular control at an intensity 5‐7 on Borg RPE scale.
Rationale and Descriptions for Stage 5 Criteria: A 100% score of 20/20 on the previously described Vail Hip Sport Test is recommended. An excellent method to measure lower extremity functional performance is by utilizing the single limb hop tests.73 These tests are used because of their reliability and ease of execution. Each hop test is performed on a single limb and includes the (1) single leg hop for distance, (2) the triple cross over hop for distance, (3) the triple hop for distance, and (4) a 6‐meter timed hop. The athlete's test performance is described as the LSI and is expressed as a percentage of the involved limb score to the uninvolved limb score. A score of 85% LSI or less is considered abnormal.74 Therefore a recommendation of >85% LSI on each of the four hop tests prior to maximizing forces during demanding agility‐based activities and power training is recommended. It is difficult to assess tri‐planar athletic movement for asymmetry and biomechanical faults. The tuck jump exercise and assessment tool has been presented as a “clinician friendly” procedure.75 The plyometric nature of this assessment lends itself to a wide variety of potential biomechanical faults and compensations as well as apparent weaknesses. Identifying these faults is an important aspect of this test, but maybe more important is monitoring and identifying the mechanical improvements seen during the test as the training has progressed from the earlier phases. The test is administered by having the athlete perform repeated tuck jumps for 10 seconds while the clinician visually grades the outlined criteria. (Table 3) It has been recommended that athletes who demonstrate 6 or more flawed techniques should continue their functional training, so the criteria for advancement is less than 6 flaws. Additionally, the athlete should tolerate advanced movements and volume of their sport specific tasks at an intensity of 5‐7 on the Borg scale without kinetic collapse.
Table 3.
Tuck Jump Assessment
| Tuck Jump Assessment | Pre | Mid | Post |
|---|---|---|---|
| Knee and Thigh Motion | |||
| 1. Lower extremity valgus at landing | ____ | ____ | ____ |
| 2. Thighs do not reach parallel (peak of jump] | ____ | ____ | ____ |
| 3. Thighs not equal side‐to‐side (during flight] | ____ | ____ | ____ |
| Foot Position During Landing | |||
| 4. Foot placement not shoulder width apart | ____ | ____ | ____ |
| 5. Foot placement not parallel (front to back] | ____ | ____ | ____ |
| 6. Foot contact timing not equal | ____ | ____ | ____ |
| 7. Excessive landing contact noise | ____ | ____ | ____ |
| Plyometric Technique | ____ | ____ | ____ |
| 8. Pause between jumps | |||
| 9. Technique declines prior to 10 seconds | ____ | ____ | ____ |
| 10. Does not land in same footprint (excessive in‐flight motion] | ____ | ____ | ____ |
| TOTAL: | ____ | ____ | ____ |
Stage 6: The athlete has demonstrated good neuromuscular control with tri‐planar, eccentric activities and increasing power and speed. The last transitional period occurs as the athlete maximizes multi‐planar dynamic movements, power, speed and agilities. Goals: Specific goals include: (1) restoration of power and maximization of plyometric strength, (2) demonstration of all sport specific tasks at game speeds and volume and an intensity of 8‐10 on the Borg RPE scale without kinetic collapse.
Stage 6 Criteria to advance: Proper assessment of full speed, power, and agility to meet the sport specific demands is achieved utilizing: (1) HOS ADL score of >96% and Sport score of >78%, (2) >92% LSI on single leg hop tests, (3) <10% side‐to‐side difference with the modified T agility test score, (4) careful assessments of sport specific tasks.
Rationale and Descriptions for Stage 6 Criteria: The authors recommend a normal ADL score of >96 and a near normal sport score of >78 based on the averages of the HOS validity study. A near normal sport score is utilized to be reflective of the athlete's perception of their current status because they are not fully integrated into sport participation. The authors recommend a score of >92% LSI for each of the four hop tests presented earlier.
Agility testing for return to sport offers useful information to the clinician. While the standard T‐test is used for the assessment of agility, it may not adequately measure side‐to‐side differences because of the equal requirements of cutting directions bilaterally.76 Therefore adjustments have been made to the standard T‐test in order to make the test more reliant on a single limb during testing and able to discern side‐to‐side agility differences.77 These modifications to the standard T test incorporates four 90 degree cuts isolated to a single direction thereby more accurately identifying differences between an athlete's involved and uninvolved leg.77 The authors recommend <10% side‐to‐side difference with the modified T test.The athlete should tolerate all sport specific tasks at game speeds and volume at an intensity of 8‐10 on the Borg RPE scale without kinetic collapse.
Re‐integration into Sport Participation: If the preceding minimum criteria have been met and the minimum scores achieved the athlete can be confidently re‐integrated into sport participation. As in any return to a high level of performance where there are such varied physical demands between sports, a detailed needs analysis must be performed by a sports medicine professional that is intimately involved in the rehabilitating athlete's particular sport. This is where functional progressions can be implemented with the particular aspects of the sport replicated taking into account the athlete's readiness mentally and the injury is steadily being pushed from the athlete's conscious decision making process while in the field of play.
CONCLUSION
There is clearly a directive in sports medicine to rely on an evidenced based approach with regard to rehabilitation and the safe return to athletic participation. The problem lies in the fact there is little evidence to support exact decisions on how and when an athlete should be returned to a particular sport. The authors have outlined several testing scenarios to attempt to help professionals to determine an athlete's readiness to handle the physical rigors of sport. The paradox is that sport requires much more than just the athlete being prepared to handle the physical demands of their particular sport. There are things such as mental preparedness as well as the so‐called “timing” or high‐level performance aspects that are required for an athlete to perform the particular sport at a near subconscious level, and eliminating the rehabilitated injury from conscious thought. Functional progressions were created for athletic therapists to begin to make this bridge from moving a rehabilitated injury from the conscious to the subconscious.
References
- 1.Bedi A Chen N Robertson W Kelly BT The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24(10):1135‐1145. [DOI] [PubMed] [Google Scholar]
- 2.Kelly BT Williams RJ 3rd Philippon MJ Hip arthroscopy: current indications #treatment |options, and management issues. Am J Sports Med. 2003;31(6):1020‐1037. [DOI] [PubMed] [Google Scholar]
- 3.Narvani AA Tsiridis E Kendall S Chaudhuri R Thomas P A preliminary report on prevalence of acetabular labrum tears in sports patients with groin pain. Knee Surg Sports Traumatol Arthrosc. 2003;11(6):403‐408. [DOI] [PubMed] [Google Scholar]
- 4.Byrd JWT Diagnostic Accuracy of Clinical Assessment, Magnetic Resonance Imaging, Magnetic Resonance Arthrography, and Intra‐articular Injection in Hip Arthroscopy Patients. Am J Sports Med. 2004;32(7):1668‐1674. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC Carlisle JC Beaule PE, et al. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008;90 Suppl 4:47‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martin HD Kelly BT Leunig M, et al. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26(2):161‐172. [DOI] [PubMed] [Google Scholar]
- 7.Philippon MJ Maxwell RB Johnston TL Schenker M Briggs KK Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15(8):1041‐1047. [DOI] [PubMed] [Google Scholar]
- 8.Byrd JW Jones KS Hip arthroscopy for labral pathology: prospective analysis with 10‐year follow‐up. Arthroscopy. 2009;25(4):365‐368. [DOI] [PubMed] [Google Scholar]
- 9.Enseki KR Martin R Kelly BT Rehabilitation after arthroscopic decompression for femoroacetabular impingement. Clin Sports Med. 2010;29(2):247‐255, viii. [DOI] [PubMed] [Google Scholar]
- 10.Philippon M Schenker M Briggs K Kuppersmith D Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):908‐914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Philippon MJ Weiss DR Kuppersmith DA Briggs KK Hay CJ Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99‐104. [DOI] [PubMed] [Google Scholar]
- 12.Nho SJ Magennis EM Singh CK Kelly BT Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high‐level athletes. Am J Sports Med. 2011;39 Suppl:14s‐19s. [DOI] [PubMed] [Google Scholar]
- 13.Hunt D Prather H Harris Hayes M Clohisy JC Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra‐articular hip disorders. PM R. 2012;4(7):479‐487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byrd JW Femoroacetabular Impingement in Athletes, Part II: Treatment and Outcomes. Sports Health. 2010;2(5):403‐409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larson CM Pierce BR Giveans MR Treatment of athletes with symptomatic intra‐articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27(6):768‐775. [DOI] [PubMed] [Google Scholar]
- 16.Byrd JWT Hip arthroscopy in athletes. Oper Tech Sports Med. 2005;13(1):24‐36. [Google Scholar]
- 17.Draovitch P Maschi RA Hettler J Return to sport following hip injury. Curr Rev Musculoskelet Med. 2012;5(1):9‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Philippon MJ Christensen JC Wahoff MS Rehabilitation after arthroscopic repair of intra‐articular disorders of the hip in a professional football athlete. J Sport Rehabil. 2009;18(1): 118‐134. [DOI] [PubMed] [Google Scholar]
- 19.Cheatham SW Kolber MJ Rehabilitation after hip arthroscopy and labral repair in a high school football athlete. Int J Sports Phys Ther. 2012;7(2):173‐184. [PMC free article] [PubMed] [Google Scholar]
- 20.Edelstein J Ranawat A Enseki KR Yun RJ Draovitch P Post‐operative guidelines following hip arthroscopy. Curr Rev Musculoskelet Med. 2012;5(1):15‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Enseki KR Martin RL Draovitch P Kelly BT Philippon MJ Schenker ML The hip joint: arthroscopic procedures and postoperative rehabilitation. J Orthop Sports Phys Ther. 2006;36(7):516‐525. [DOI] [PubMed] [Google Scholar]
- 22.Garrison JC Osler MT Singleton SB Rehabilitation after arthroscopy of an acetabular labral tear. N Am J Sports Phys Ther. 2007;2(4):241‐250. [PMC free article] [PubMed] [Google Scholar]
- 23.Griffin KM Rehabilitation of the hip. Clin Sports Med. 2001;20(4):837‐850, viii. [DOI] [PubMed] [Google Scholar]
- 24.Malloy P Malloy M Draovitch P Guidelines and pitfalls for the rehabilitation following hip arthroscopy. Curr Rev Musculoskelet Med. 2013;6(3):235‐241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pierce CM Laprade RF Wahoff M O'Brien L Philippon MJ Ice hockey goaltender rehabilitation, including on‐ice progression, after arthroscopic hip surgery for femoroacetabular impingement. J Orthop Sports Phys Ther. 2013;43(3):129‐141. [DOI] [PubMed] [Google Scholar]
- 26.Spencer‐Gardner L Eischen JJ Levy BA Sierra RJ Engasser WM Krych AJ A comprehensive five‐phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2013. [DOI] [PubMed] [Google Scholar]
- 27.Stalzer S Wahoff M Scanlan M Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25(2):337‐357, x. [DOI] [PubMed] [Google Scholar]
- 28.Voight ML Robinson K Gill L Griffin K Postoperative rehabilitation guidelines for hip arthroscopy in an active population. Sports Health. 2010;2(3):222‐230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wahoff M Ryan M Rehabilitation after hip femoroacetabular impingement arthroscopy. Clin Sports Med. 2011;30(2):463‐482. [DOI] [PubMed] [Google Scholar]
- 30.Willimon SC Briggs KK Philippon MJ Intra‐articular adhesions following hip arthroscopy: a risk factor analysis. Knee Surg Sports Traumatol Arthrosc. 2013. [DOI] [PubMed] [Google Scholar]
- 31.McGill SM Cholewicki J Biomechanical basis for stability: an explanation to enhance clinical utility. J Orthop Sports Phys Ther. 2001;31(2):96‐100. [DOI] [PubMed] [Google Scholar]
- 32.Philippon MJ Arnoczky SP Torrie A Arthroscopic repair of the acetabular labrum: a histologic assessment of healing in an ovine model. Arthroscopy. 2007;23(4):376‐380. [DOI] [PubMed] [Google Scholar]
- 33.M D. Dutton's orthopedic survival guide: managing common conditions. New York: McGraw‐Hill Medical; c2011. [Google Scholar]
- 34.Freeman S Mascia A McGill S Arthrogenic neuromusculature inhibition: a foundational investigation of existence in the hip joint. Clin Biomech (Bristol, Avon). 2013;28(2):171‐177. [DOI] [PubMed] [Google Scholar]
- 35.Williamson A Hoggart B Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798‐804. [DOI] [PubMed] [Google Scholar]
- 36.DeLoach LJ Higgins MS Caplan AB Stiff JL The visual analog scale in the immediate postoperative period: intrasubject variability and correlation with a numeric scale. Anesth Analg. 1998;86(1):102‐106. [DOI] [PubMed] [Google Scholar]
- 37.Serlin RC Mendoza TR Nakamura Y Edwards KR Cleeland CS When is cancer pain mild, moderate or severe?. Grading pain severity by its interference with function. Pain. 1995;61(2):277‐284. [DOI] [PubMed] [Google Scholar]
- 38.Hopkins JT Ingersoll CD Arthrogenic muscle inhibition: a limiting factor in joint rehabilitation. J Sport Rehabil. 2000(9):135‐159. [Google Scholar]
- 39.Safran MR Giordano G Lindsey DP, et al. Strains across the acetabular labrum during hip motion: a cadaveric model. Am J Sports Med. 2011;39 Suppl:92S‐102S. [DOI] [PubMed] [Google Scholar]
- 40.Clark HM Joint motion and function assessment: a research‐based practical guide. Philadelphia: Lippincott Williams & Wilkins; c2005. [Google Scholar]
- 41.Levangie PK Norkin CC Joint structure and function: a comprehensive analysis. 3rd ed. ed. Philadelphia: F.A. Davis; c2001. [Google Scholar]
- 42.Johnston RC Smidt GL Measurement of hip‐joint motion during walking. Evaluation of an electrogoniometric method. J Bone Joint Surg Am. 1969;51(6):1082‐1094. [PubMed] [Google Scholar]
- 43.Lewis CL Sahrmann SA Moran DW Effect of hip angle on anterior hip joint force during gait. Gait Posture. 2010;32(4):603‐607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lewis CL Sahrmann SA Moran DW Anterior hip joint force increases with hip extension, decreased gluteal force, or decreased iliopsoas force. J Biomech. 2007;40(16):3725‐3731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kummer B Is the Pauwels’ theory of hip biomechanics still valid? A critical analysis, based on modern methods. Ann Anat. 1993;175(3):203‐210. [DOI] [PubMed] [Google Scholar]
- 46.Davis AM Bridge P Miller J Nelson‐Wong E Interrater and intrarater reliability of the active hip abduction test. J Orthop Sports Phys Ther. 2011;41(12):953‐960. [DOI] [PubMed] [Google Scholar]
- 47.Sahrmann S Diagnosis and treatment of movement impairment syndromes / Shirley Sahrmann. St. Louis, Mo: Mosby; c2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kendall KD Patel C Wiley JP Pohl MB Emery CA Ferber R Steps toward the validation of the Trendelenburg test: the effect of experimentally reduced hip abductor muscle function on frontal plane mechanics. Clin J Sport Med. 2013;23(1):45‐51. [DOI] [PubMed] [Google Scholar]
- 49.Lee SJ Hidler J Biomechanics of overground vs. treadmill walking in healthy individuals. J Appl Physiol (1985). 2008;104(3):747‐755. [DOI] [PubMed] [Google Scholar]
- 50.White SC Yack HJ Tucker CA Lin HY Comparison of vertical ground reaction forces during overground and treadmill walking. Med Sci sports Exerc. 1998;30(10):1537‐1542. [DOI] [PubMed] [Google Scholar]
- 51.Riley PO Paolini G Della Croce U Paylo KW Kerrigan DC A kinematic and kinetic comparison of overground and treadmill walking in healthy subjects. Gait Posture. 2007;26(1):17‐24. [DOI] [PubMed] [Google Scholar]
- 52.Scherr J Wolfarth B Christle JW Pressler A Wagenpfeil S Halle M Associations between Borg's rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol. 2013;113(1):147‐155. [DOI] [PubMed] [Google Scholar]
- 53.Foster C Monitoring training in athletes with reference to overtraining syndrome. Med Sci Sports Exerc. 1998;30(7):1164‐1168. [DOI] [PubMed] [Google Scholar]
- 54.Day ML McGuigan MR Brice G Foster C Monitoring exercise intensity during resistance training using the session RPE scale. J Strength Cond Res. 2004;18(2):353‐358. [DOI] [PubMed] [Google Scholar]
- 55.Mohtadi NG Griffin DR Pedersen ME, et al. The Development and validation of a self‐administered quality‐of‐life outcome measure for young, active patients with symptomatic hip disease: the International Hip Outcome Tool (iHOT‐33). Arthroscopy. 2012;28(5):595‐605. [DOI] [PubMed] [Google Scholar]
- 56.Griffin DR Parsons N Mohtadi NG Safran MR A short version of the International Hip Outcome Tool (iHOT‐12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611‐616. [DOI] [PubMed] [Google Scholar]
- 57.Martin RL Kelly BT Philippon MJ Evidence of validity for the hip outcome score. Arthroscopy. 2006;22(12):1304‐1311. [DOI] [PubMed] [Google Scholar]
- 58.Martin RL Philippon MJ Evidence of validity for the hip outcome score in hip arthroscopy. Arthroscopy. 2007;23(8):822‐826. [DOI] [PubMed] [Google Scholar]
- 59.Tijssen M van Cingel R van Melick N de Visser E Patient‐Reported Outcome questionnaires for hip arthroscopy: a systematic review of the psychometric evidence. BMC Musculoskelet Disord. 2011;12:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nakagawa TH Moriya ET Maciel CD Serrao FV Test‐retest reliability of three‐dimensional kinematics using an electromagnetic tracking system during single‐leg squat and stepping maneuver. Gait Posture. 2014;39(1):141‐146. [DOI] [PubMed] [Google Scholar]
- 61.Crossley KM Zhang WJ Schache AG Bryant A Cowan SM Performance on the single‐leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866‐873. [DOI] [PubMed] [Google Scholar]
- 62.Ageberg E Bennell KL Hunt MA Simic M Roos EM Creaby MW Validity and inter‐rater reliability of medio‐lateral knee motion observed during a single‐limb mini squat. BMC Musculoskelet Disord. 2010;11:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dwyer MK Boudreau SN Mattacola CG Uhl TL Lattermann C Comparison of lower extremity kinematics and hip muscle activation during rehabilitation tasks between sexes. J Athl Train. 2010;45(2):181‐190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Olson TJ Chebny C Willson JD Kernozek TW Straker JS Comparison of 2D and 3D kinematic changes during a single leg step down following neuromuscular training. Phys Ther Sport. 2011;12(2):93‐99. [DOI] [PubMed] [Google Scholar]
- 65.Reiman MP Bolgla LA Loudon JK A literature review of studies evaluating gluteus maximus and gluteus medius activation during rehabilitation exercises. Physiother Theory Pract. 2012;28(4):257‐268. [DOI] [PubMed] [Google Scholar]
- 66.Ayotte NW Stetts DM Keenan G Greenway EH Electromyographical analysis of selected lower extremity muscles during 5 unilateral weight‐bearing exercises. J Orthop Sports Phys Ther. 2007;37(2):48‐55. [DOI] [PubMed] [Google Scholar]
- 67.Garrison JC Shanley E Thigpen C Geary R Osler M Delgiorno J The reliability of the vail sport test as a measure of physical performance following anterior cruciate ligament reconstruction. Int J Sports Phys Ther. 2012;7(1):20‐30. [PMC free article] [PubMed] [Google Scholar]
- 68.Bohannon RW Test‐retest reliability of hand‐held dynamometry during a single session of strength assessment. Phys Ther. 1986;66(2):206‐209. [DOI] [PubMed] [Google Scholar]
- 69.Thorborg K Petersen J Magnusson SP Holmich P Clinical assessment of hip strength using a hand‐held dynamometer is reliable. Scand J Med Sci Sports. 2010;20(3):493‐501. [DOI] [PubMed] [Google Scholar]
- 70.Hertel J Braham RA Hale SA Olmsted‐Kramer LC Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131‐137. [DOI] [PubMed] [Google Scholar]
- 71.Plisky PJ Rauh MJ Kaminski TW Underwood FB Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911‐919. [DOI] [PubMed] [Google Scholar]
- 72.Smith CA Chimera NJ Warren M Association of Y Balance Test Reach Asymmetry and Injury in Division I Athletes. Med Sci Sports Exerc. 2014. [DOI] [PubMed] [Google Scholar]
- 73.Noyes FR Barber SD Mangine RE Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513‐518. [DOI] [PubMed] [Google Scholar]
- 74.Barber SD Noyes FR Mangine RE McCloskey JW Hartman W Quantitative assessment of functional limitations in normal and anterior cruciate ligament‐deficient knees. Clin Orthop Rel Res. 1990(255):204‐214. [PubMed] [Google Scholar]
- 75.Myer GD Ford KR Hewett TE Tuck Jump Assessment for Reducing Anterior Cruciate Ligament Injury Risk. Athl Ther Today. 2008;13(5):39‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Myer GD Schmitt LC Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377‐387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Myer GD Paterno MV Ford KR Quatman CE Hewett TE Rehabilitation after anterior cruciate ligament reconstruction: criteria‐based progression through the return‐to‐sport phase. J Orthop Sports Phys Ther. 2006;36(6):385‐402. [DOI] [PubMed] [Google Scholar]