Abstract
Background
Minimally invasive plate osteosynthesis (MIPO) is an established technique for fixation of fractures of the distal third tibia. Our study aimed to manage intra articular and extraarticular fractures of the distal third tibia by the minimally invasive plate osteosynthesis technique and follow them prospectively. Clinical and radiological outcomes were studied and clinical indications & efficacy of the procedure reviewed. Though many studies on the subject have been done previously, these have been retrospective reviews or small series.
Methods
From May 2010 to May 2013, 50 patients of closed distal tibial fractures were operated by MIPO technique with a distal tibial anatomical locking plate having 4.5/5 proximal and 3.5/4 distal screw holes. The follow up duration was for 3 years.
Results
The mean fracture healing time was 21.4 weeks (range 16–32 weeks) and average AOFAS score 95.06 was out of a total possible 100 points. At last follow up, superficial infection occurred in 5 patients (10%); deep infection, implant failure and malunion in 1-patient each (2%).
Conclusion
MIPO technique provides good, though slightly delayed bone healing and decreases incidence of nonunion and need for bone grafting. This technique should be used in distal tibia fractures where locked nailing cannot be done like fractures with small distal metaphyseal fragments, vertical splits, markedly comminuted fractures and in fractures with intra-articular extension.
Keywords: Distal tibia fracture, Pilon fracture, Percutaneous plating, Locking compression plate (LCP)
1. Introduction
Fractures of the distal third tibia are unique in that the bone is subcutaneous with depleted muscular cover; the consequent decreased vascularity leads to complications like delayed bone union, wound complications such as dehiscence and infection. These fractures can be managed with various techniques. Small wire fixators,1–3 and Open reduction and plating,4,5 have been used with varying results.
In current orthopaedic practice, minimally invasive plating osteosynthesis (MIPO) and interlocking nailing are the preferred techniques for fractures of the distal third tibia. The intramedullary nail spares the extraosseous blood supply, allows load sharing, and avoids extensive soft tissue dissection.6,7 However, proximal and distal shaft fractures can be difficult to control with an intramedullary device, increasing the frequency of malalignment.8 Concerns regarding difficulties with reduction/loss of reduction, inappropriate fixation in fractures with articular extension, anterior knee pain9 and hardware failure have slowed the acceptance of intramedullary nailing as a treatment of fractures of the distal tibia. The recent innovation of nails with tip locking is a testimony that earlier nails were insufficient fixation tools for distal tibia; however tip locking is technically difficult and fractures that require it are essentially difficult to fix with nails.6,8,10
Minimally invasive submuscular and subcutaneous plate fixation (MIPO) can address several of the issues associated with intramedullary nailing, while amalgamating all biological benefits of closed reduction and fixation.11,12 We reviewed the clinical indications and efficacy of MIPO in distal third tibia.
2. Patients and methods
From May 2010 to May 2013, we conducted a prospective case series at our Level 1 trauma centre. A total of 50 patients with a mean age of 36 years were included. The study was approved by our institutional ethics committee and written informed consent was obtained from all patients. All closed fractures and Gustilo and Anderson Grade I compound fractures of the distal third tibia, with or without intra articular extension, upto 2 weeks old were included in the study. Informed consent for both the surgery and inclusion in the study were taken before the procedure. We excluded patients with pathological fractures, fractures older than 2 weeks, Gustilo and Anderson Type II and Type III fractures, and patients who were unfit for surgery.
After stabilising the traumatised patient, routine pre-anaesthetic investigations were carried out. Standard antero-posterior and lateral radiographs of the affected leg with knee and ankle joint were taken. The leg was immobilised in a plaster slab till definitive surgery. Patients with precarious skin condition were managed with limb elevation, regular dressing care and prophylactic intravenous antibiotics; surgery was delayed till appearance of the ‘wrinkle sign’, but performed within 2 weeks from trauma.
X-rays taken were evaluated for fracture morphology, level and extent of comminution. The fibular fracture was noted and surgical plan decided accordingly. The type and likely length of the plate was calculated.
-
1.
Plate Screw Density (SD) ratio – We preferred an SD ratio of 0.5 in the proximal fragment and inserted a minimum of three screws in each fragment.13 Thus preoperatively we planned for a plate which had 6 holes proximal to the fracture line. Due to the small distal metaphyseal fragment, this plate-screw ratio of 0.5 had to be compromised in the distal fragment, although we followed the principle where we could.
-
2.
Comminution – In comminuted fractures, the plate span ratio was kept to 3 and in case of fractures with a simple fracture configuration, a plate 8–10 times longer than the fracture was planned for.13,14
-
3.
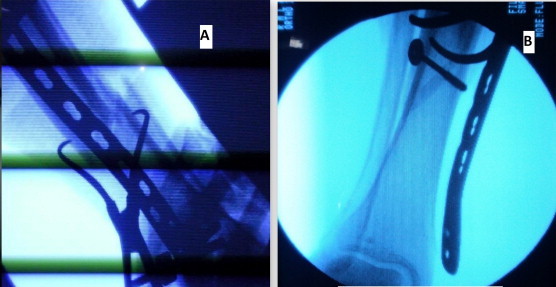
LCP design – The choice of design of the plate was decided by the fracture anatomy in each individual patient. We used the distal tibial anatomical locked plate in distal fourth fractures with a small metaphyseal fragment since the metaphyseal flare of the plate allowed placement of the three minimum requisite screws (Fig 1A). In more proximal fractures where the distal fragment was large enough, we used the medial tibial locked plate which did not have a metaphyseal flare and thus had a lower plate profile (Fig. 1B).
Fig. 1.

(A) Distal tibial anatomical locking plate with metaphyseal flares used for distal metaphyseal fractures to allow the placement of the three requisite distal screws. (B) Distal tibial anatomical plate without metaphyseal flare used for more proximal fractures.
Surgery was performed in our tertiary care trauma centre under regional anaesthesia with a tourniquet in the supine position on a radiolucent table. In the distal tibia, the locking compression plate was applied on the antero-medial surface. A locking compression plate of adequate length so that 6–8 cortices are obtained on either side of the fracture was kept on the leg and visualised under C-arm.
The fracture was reduced by indirect means without opening the fractured area.
-
i.
Gentle manual traction/traction with calcaneal Denham pin and external manipulation e.g. a bolster under the ankle to correct the posterior displacement and angulation were adequate to reduce AO43A1 fractures.
-
ii.
Use of percutaneous pointed reduction forceps and fixation of preliminary reduction by K-wires was needed in some cases (Fig 2A).
-
iii.
Schanz pins inserted into the fracture fragments can be used to externally manipulate the fracture under radiographic control to achieve reduction.
-
iv.
For type 43-A1 fractures a percutaneous lag screw from lateral to medial side was inserted under radiographic control so as not to jeopardise plate application on the medial side. A percutaneous pointed reduction forceps was used to make this feasible (Fig 2B).
-
v.
In severely comminuted fractures, a femoral distractor was used.
Fig. 2.
(A) AO 43 A1 fracture reduced with a percutaneous reduction clamp and LCP slid into place. (B) C-arm picture showing a percutaneous lag screw inserted from lateral to medial and plate in place.
The reduction was assessed repeatedly using visual and fluoroscopic control. Angulation, length of tibia and fibula, rotation and integrity of the ankle mortise were considered. The mechanical axis and anatomical axis of the lower limb was checked with the cautery cord. If the associated fracture fibula required fixation, it, was fixed by rush nail or one third tubular plate according to the fracture type, before fixation of the tibia.
After provisional reduction, a 3–4 cm vertical incision was given at the centre of the medial malleolus and a subcutaneous tunnel was opened with a haemostat or artery forceps. Then the selected locking compression plate with a locking sleeve screwed into its distal hole was held with a pen-like grip. The plate was tunnelled proximally subcutaneously across the fracture site, using the locking sleeve as the handle with a dagger hold. Smooth and gentle supination-pronation motions were used while inserting the plate. The thumb was kept anteriorly on the tibial crest and was used to guide the proximal part of the plate onto the antero-medial surface of the tibia.
The plate was centred on the proximal fracture fragment in both antero-posterior and lateral views with the help of a locking sleeve inserted into the most proximal hole. Following confirmation, a drill bit or K-wire was used to fix the plate onto the tibia. Non locking screws were inserted first in either the proximal or distal fragment as required to aid in the reduction of the fracture so as to pull the bone to the plate.
The locking screws were inserted only and only when the fracture reduction was satisfactory. The proximal holes can be located in thin patient by palpation through the skin. A similar sized LCP placed over the skin helped localise the hole in the inserted plate (Mirror plate technique15). Only in an overweight or obese patient, was C-arm assistance necessary to localise the locking hole. In the pilon plate, all the distal screws were inserted under direct vision through the incision over the medial malleolus without need for further incisions. At least 6–8 cortices were held proximal and distal to fracture site.
In case of distal tibial fractures with intra-articular extension, the articular fragments were reduced first. The fragments were reduced percutaneously or by a limited lateral incision with pointed reduction forceps under radiographic control; and fixed with screws separately or by screws through the locking compression distal tibial pilon plate (Video). The distal incision was closed in two layers and the proximal stab wounds in a single layer. A well-padded plaster slab was applied.
Post operatively the limb was elevated and a removable below knee slab was given. Toe touch weight bearing and knee range of motion was started on the 2nd postoperative day. Sutures were removed alternate at 2 weeks and all at 3 weeks, slab was continued for 4–6 weeks. Weight bearing was increased depending on the progress of clinical and radiological fracture healing. Full weight bearing was allowed at fracture union, which was defined as union in 3 cortices and painless weight bearing (Fig. 3A and B).
Fig. 3.

(A) Preoperative X ray of patient no. 24 with an isolated fracture tibia. The patient was operated by Mipo technique with 2 percutaneous lag screws and distal tibial LCP. (B) X ray showing union at 23 weeks.
3. Results
The age of the patients ranged from 20 to 56 years with mean age of 36 years. Most of the patients (i.e. 35) were in the age group of 20–40 years. There were 35 male and 15 female patients included in the study. The mode of injury in the majority of the patients was road traffic accidents. The majority of the fractures operated in our study were extra-articular fractures, i.e. AO/OTA 43-A (90%). We also operated three (6%) partially articular AO-OTA 43-B and two (4%) intra articular AO/OTA 43-C fracture in our study. 35 patients (70%) had a both bone leg fracture, with majority of the fibular fractures occurring at the level of the tibial fracture, suggesting a bending mechanism. Out of the 35 patients with an associated fibular fracture, only 8 patients needed fixation of the fibula (22.8%). Of these, 4 fractures were fixed with one third tubular plates and 4 with rush nails.
The average duration between trauma and surgery was 4.36 days with a range of 0–12 days. Most of the cases were operated upon within 7 days of injury (86%). The average operative time was 86.233 min with a range of 70–123 min. The majority of the fractures were operated within 100 min of operative time (90.0%). Operative time was longer in fractures with intra-articular extension or which needed fixation of the fibula. The average fluoroscopy time was 30.33 s with a range of 15 s–60 s. 90% of the cases were completed within the fluoroscopy time of 40 s.
The mean time for radiological union was 21.4 weeks with a range of 16–32 weeks. 16 fractures (32%) healed at 20 weeks and 48 fractures (96%) united within a period of 25 weeks.
On union, all of the 50 patients had an AOFAS score of 90 or greater out of a possible 100 points. The mean score was 95.06.
We encountered superficial infection in 5 (10%) of our patients which were managed with dressings and appropriate antibiotics. As the study progressed we realised that the key to preventing infection was gentle handling of the soft tissues. On long term follow up of these patients the superficial infection healed well.
Patient 16 was a 20 year old smoker who had implant failure 16 weeks post-operatively. There was breakage of plate and screw. In this patient, a tibial interlocking was planned but we encountered deep infection per-operatively and had do apply a temporary external fixator instead. After infection resolved, interlocking was done and fracture healed subsequently. There was no non-union in our series.
Patient 5 an osteoporotic elderly patient with a comminuted fracture both bone leg suffered mal-reduction with posterior angulation of 11° despite plating of the associated fracture fibula. He was offered re-surgery but refused. The fracture united at 22 weeks with an AOFAS score of 90 on follow up.
Implant removal was done in 9 patients. Eight patients had their distal tibial locking plate removed due to symptomatic skin impingement over the medial malleolus. Another plate was removed secondary to implant failure at re-surgery. The other 41 patients did not report any trouble at follow-up due to symptomatic hardware.
4. Discussion
Distal tibial fractures remain one of the most substantial therapeutic challenges that confront the orthopaedic traumatologist. Though conservative management of these fractures has been described,16,17 these methods have been largely superseded by operative techniques for displaced or irreducible fractures, and fractures with intra-articular extension.
MIPO is by now an established technique of management of fractures of the distal third tibia. A comprehensive review of the technique is lacking, though some very good attempts have been made. Table 1 reviews the results of 13 such studies vis a vis our own.
Table 1.
A comparison of the findings of various studies.
| Publication | No of patients | Average age of patient (in yrs) | Average operative time (in mins) | Average fluoroscopy time | Average time to union | Post operative infection (%) | Malalignment (%) | Delayed/Nonunions (%) | Mean AOFAS score at union (Max 100) | Implant removal (% of patients) |
|---|---|---|---|---|---|---|---|---|---|---|
| Borg et al18 | 21 | – | 82 min | – | 5.44 m | 14.3% | 28.5% | 19% | – | 9.5% |
| Bahari et al19 | 42 | 35 yrs | – | 22.4 wks | 7.14% | 7.14% | ||||
| Mafulli et al20 | 20 | – | – | 0 | 36.8% | 5.3% | ||||
| Redfern et al21 | 20 | 38.3 yrs | – | – | 23 wks | 5% | 5% | 0 | – | 15% |
| Hasenbohler at al22 | 32 | 45 yrs | 86.6 min | – | 75% at 6 m, 84% at 9 m | 3.4% | 0 | 17.2% | – | 65.6% |
| aWilliams et al23 | 20 | – | – | – | – | 10.5% | – | 31.5% | – | – |
| Lau et al24 | 48 | – | – | – | 18.7 wks | 16.7% | – | 10.4% | – | – |
| Gupta et al25 | 71 | – | – | – | – | 3.8% | 2.5% | 12.7% | – | – |
| Ronga et al26 | 21 | – | – | – | – | 42.3% | 19% | 4.8% | – | – |
| aSitnik et al27 | 80 | 43 yrs | – | – | 87.5% by 6 m | 9% | 6% | 13% | – | |
| Hazarika et al28 | 20 | 44.7 yrs | – | – | 58.3% at 6 m (closed #) | 5% | – | 10% (open fractures) | – | 15% |
| J J Guo et al7 | 54 | 44.4 yrs | 97.9 min | 3 min | 17.6 wks | 14.6% | – | – | 83.9 | 92.7% |
| Collinge et al29 | 38 | – | – | – | 21 wks | All inf. Superficial | 2.63% | 8% | 85 | 5% |
| Current study | 50 | 36 yrs | 86.23 min | 30.33 sec | 21.4 wks | 12% | 2% | 2% | 95.06 | 18% |
Included AO-41, 42, 43 fractures.
In the present study, the mean age of 36 years is comparable to the studies by Bahari et al.19 and Redfern, Syed, Davies.21 The age of the patient had no bearing on the time to union in our study.
In our study, there were associated injuries in only 2 patients (4%). Patient 3 had an ipsilateral undisplaced fracture patella and a contralateral undisplaced fracture both bone leg. The fracture patella had no articular incongruency or articular step, and active extension was possible without any extensor lag. Both the associated fractures were therefore managed non-operatively. The operated fracture tibia united at 16 weeks. Patient 22 had ipsilateral fracture femur and fracture humerus which were operatively managed. Because of the associated fractures, mobilisation was delayed but the tibia united at 20 weeks.
The mean operative time of 86 min compares favourably with other studies (82–97.9 min).7,18,22 Operative time was longer in AO 43A1 fractures in which a percutaneous lag screw was inserted, in intra-articular fractures needing reduction and provisional fixation of the tibial pilon, and in the 8 patients with a concomitant fibular fracture needing fixation. We recommend one or preferably two percutaneous lag screws of adequate length in all spiral/oblique fractures from lateral to medial side before MIPO so as not to jeopardise medial plate application. This provisional fixation makes further MIPO easier. For this we have used cannulated screws (4.5 mm). If possible lag screws can be inserted through plate and they provide better strength to the fixation construct (Fig. 4A and B).
Fig. 4.

(A) Preoperative X rays of patient no.42 showing AO 43-C1 fracture. (B) Post operative X rays showing lag screw across fracture site through the plate.
In the fractures operated within 1 week of injury, the operative time was 85.4 min and time to union was 21.6 weeks. In the cases operated in the second week of trauma, the operative time was 91.2 min and time to union was 19.5 weeks. These findings were not statistically significant. As the time interval between surgery and the injury increase it becomes more and more difficult to indirectly reduce the fracture fragments. Our operative time is comparable with other studies.
In our study, in the majority of the cases, the fluoroscopy time was 30 s or less (66%). 90% of the cases were completed within the fluoroscopy time of 40 ss. The average radiation exposure was 30.33 s with a range of 15 s–50 s. The fluoroscopy time in fractures fixed within 1-week of injury was 29.4 s while the fluoroscopy time in fractures fixed in the second week was 36.2 s. Thus older fractures necessitated greater fluoroscopic assistance.
Intra-articular fractures needed a mean fluoroscopic exposure of 44.8 s while in extra-articular fractures, the mean fluoroscopic time was 28.9 s (Table 2). In comparison, in the study of J J Guo et al.,7 the mean fluoroscopy time was 3.0 min. J J Guo et al.7 used continuous fluoroscopy. We attribute our fluoroscopy time to careful clinical evaluation of the fracture, proper positioning of the C-arm before exposure and conscious reduction of radiation exposure by curbing the use of continuous fluoroscopy.
Table 2.
A table detailing average fluoroscopy time and time to union according to fracture anatomy.
| Fracture classification | Mean fluoroscopy time (s) | Mean time to union (in weeks) |
|---|---|---|
| A1 | 29.93 | 20.8 |
| A2 | 26.88 | 22.22 |
| A3 | 30 | 21.33 |
| B1 | 34 | 18 |
| B2 | 50 | 20 |
| C1 | 45 | 23 |
There was failure to achieve reduction (>5 degrees of varus/valgus; >10 degrees of procurvatum/recurvatum) in one case of distal tibial fracture (patient 5). This patient had a comminuted osteoporotic fracture both bone leg and refused re-surgery. The same distal tibial fracture had malunion (recurvatum of 11 degrees), although the functional results were good and the patient was satisfied with the results. In the study by Collinge and Protzman,30 out of a total 38 fractures, they had one malalignment with >5° angulation and 1 cm shortening. Redfern et al.21 had 1 malunion in a series of 20 patients treated with MIPO with DCP. In their study on Minimally Invasive Plate Osteosynthesis in distal tibial fractures. Stefano Ghera et al.30 (2004) reported one malunion out of 18 cases. Helfet et al.31 in their series of 20 patients of distal tibial fractures treated by MIPO reported 4 cases of malunion; 2 with >5 degrees of varus and 2 with >10 degrees of recurvatum. Our study is comparable to these findings.
In the present study, 5 patients (10.0%) had post-operative superficial wound infection and 1-patient had a deep infection. In all the five cases with superficial infection, the pilon plate had been used. All the cases healed after treatment with appropriate antibiotics and aseptic dressings and the infection did not appear to have any long term effect on fracture healing or the rehabilitation of the patient. The mean time to union in these patients was 21 weeks. The infection rate in the current series is similar to other studies (Table 1).
In our series of fractures the mean time to union was 21.4 weeks with a range of 16–32 weeks. 96% fractures united within a period of 25 weeks. We defined union as painless full weight bearing and radiological union of 3 cortices in standard antero-posterior and lateral X-rays. Lau et al.24 reported the average time to radiological bony union as 18.7 weeks, which ranged from the shortest 12 weeks to the longest 44 weeks. Oh CW et al.32 in their study of twenty-one patients with fractures of the distal tibial metaphyses, treated by percutaneous plate osteosynthesis with a narrow limited contact-dynamic compression plate reported the average time to union as 15.2 weeks. In the study of Bahari et al.19 mean fracture healing in distal tibial fractures was found at 22.4 weeks postoperatively Redfern, Syed and Davies 21 in their study reported that the mean time to union for distal tibial fractures was 23 weeks (range: 18–29 weeks), without need for further surgery.
The mean time to union in smokers was 22.63 weeks while the mean time to union in non-smokers was 20.68 weeks, which was found statistically significant at 10% level of significance. The time to union varied from 18 weeks in AO 43-B1 fractures to 23 weeks in AO 43-C1 fractures (Table 2).
The mean time to union in patients with fracture isolated tibia was 21.11 weeks, while fractures with the fibula fractured at the same level united at a mean of 21.57 weeks. Of the 35 patients who had an associated fracture fibula, only 8 fractures were fixed, the indication being a fracture in the distal 5–7 cm of the fibula. The mean time to union of the tibia in fixed fractures of the fibula was 21.2 weeks. The mean time to union of the tibia in unfixed fractures of the fibula was 21.62 weeks. Thus in our study, there was no relevance of the status of the fracture fibula in the time to union.
In the present study clinical results were evaluated according to the AOFAS score chronologically and at union. On union, all of the 50 patients had an AOFAS score of 90 or greater out of a possible 100 points. The mean score was 95.06. Collinge and Protzman29 reported a good to excellent result with a mean AOFAS score of 85. In the study undertaken by Redfern et al.,21 all patients returned to their pre-injury occupation or level of activity. The mean AOFAS score in the MIPO group of the study by J J Guo et al.7 was 83.9. Vasu Pai, Gareth Coulter and Vishal Pai33 (2007) in their study of minimally invasive plate fixation of the distal tibia reported excellent results in11 patients, good in 9, fair in 2 and poor result in one patient. On follow up, implant removal was needed in eight patients with symptomatic hardware in our study (16%), compared to 5%–92.7% in other studies (Table 1).
The ability to maintain a mechanically stable reduction with intramedullary nailing becomes more difficult the further a fracture extends distally. The wide medullary canal in the metaphyseal area, results in reduced stability due to the large diameter of distal part of the tibia in relation to the diameter of nail. Fractures with minimal involvement of the ankle can be treated successfully by intramedullary nailing but this technique is inappropriate for pilon fractures with significant articular involvement.34 Modern tibial nail designs have interlocking holes that enable distal placement of screws in close proximity to the tip of the nail, but these screws have less purchase in metaphyseal bone; there is increased stress on the screws to maintain fracture alignment.35 Consequently late complications, in particular loss of reduction, are attributed to implant failure at the distal locking sites of the intramedullary nail.35
The locking compression platen (LCP) is part of a new plate generation requiring an adapted surgical technique and new thinking about commonly used concepts of internal fixation using plates. Understanding of the mechanical background for choosing the proper implant length and the type and number of screws is essential to obtain a sound fixation with a high plate span ratio and a low plate screw density. A high plate span ratio decreases the load onto the plate. A high working length of the plate reduces the screw loading, thus fewer screws need to be inserted and the plate screw density can be kept low. Selection of mono or bi-cortical screws is done according to the quality of the bone structure and it is important to avoid problems at the screw thread bone interface with potential pullout of screws and secondary displacement. We recommend bicortical locking screws for the tibia, since the working length of the monocortical screw depends only on the thickness of the bone cortex.13,14
5. Conclusion
The MIPO technique is a reliable fixation approach to fractures of the distal third tibia, preserving most of the osseous vascularity and fracture haematoma and thus providing for a more biological repair. The bone healing, though slightly delayed, was universal with this type of fixation. This technique can be used in fractures where locked nailing cannot be done like distal tibial fractures with small distal metaphyseal fragments, vertical split and markedly comminuted fractures. Due to preserved vascularity, there is lesser incidence of delayed union and non-union. There was reduced incidence of infection due to limited exposure. Infection can also be prevented by careful handling of soft tissues and by minimising the operating time.
Conflicts of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Bonkar S.K., Marshall J.L. Unilateral external fixation for severe pilon fractures. Foot Ankle. 1993;14:57–64. doi: 10.1177/107110079301400201. [DOI] [PubMed] [Google Scholar]
- 2.Anglen J.O. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999;13:92–97. doi: 10.1097/00005131-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Pugh K.J., Wolinsky P.R., McAndrew M.P., Johnson K.D. Tibial pilon fractures: a comparison of treatment methods. J Trauma. 1999;47:937–941. doi: 10.1097/00005373-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Teeny S.M., Wiss D.A. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993;292:108–117. [PubMed] [Google Scholar]
- 5.Wrysch B., McFerran M.A., McAndrew M. Operative treatment of fractures of the tibial plafond. A randomised, prospective study. J Bone Jt Surg Am. 1996;78:1646–1667. doi: 10.2106/00004623-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Nork S.E., Schwartz A.K., Agel J., Holt S.K., Schrick B.S., Winquist R.A. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Jt Surg Am. 2005;87-A:1213–1221. doi: 10.2106/JBJS.C.01135. [DOI] [PubMed] [Google Scholar]
- 7.Guo J.J., Tang N., Yang H.L., Tang T.S. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Jt Surg Br. 2010;92-B:984–988. doi: 10.1302/0301-620X.92B7.22959. [DOI] [PubMed] [Google Scholar]
- 8.Dogra A.S., Ruiz A.L., Thompson N.S., Nolan P.C. Dia-metaphyseal distal tibia fractures-treatment with a shortened intramedullary nail: a review of 15 cases. Injury. 2000;31:799–804. doi: 10.1016/s0020-1383(00)00129-7. [DOI] [PubMed] [Google Scholar]
- 9.Court-Brown C.M., Gustilo T., Shaw A.D. Knee pain after intramedullary tibial nailing: its incidence, etiology, and outcome. J Orthop Trauma. 1997;11:103–105. doi: 10.1097/00005131-199702000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Mohammed A., Saravanan R., Zammit J., King R. Intramedullary tibial nailing in distal third tibial fractures: distal locking screws and fracture non-union. Int Orthop. 2008;32:547–549. doi: 10.1007/s00264-007-0356-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cantu R.V., Koval K.J. The use of locking plates in fracturecare. J Am Acad Orthop Surg. 2006;14:183–190. doi: 10.5435/00124635-200603000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Farouk O., Krettek C., Miclau T., Schandelmaier P., Guy P., Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997;28(suppl 1):A7–A12. doi: 10.1016/s0020-1383(97)90110-8. [DOI] [PubMed] [Google Scholar]
- 13.Gautier E., Sommer C. Guidelines for the clinical application of the LCP. Inj Int J Care Inj. 2003;34:S-B63–S-B76. doi: 10.1016/j.injury.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 14.Wagner M. General principles for the clinical use of the LCP. Inj Int J Care Inj. 2003;34:S-B31–S-B42. doi: 10.1016/j.injury.2003.09.023. [DOI] [PubMed] [Google Scholar]
- 15.Guven M., Ünay K., Çakici H., Ozturan E.K., Ozkan N.K. A new screw fixation technique for minimally invasive percutaneous plate osteosynthesis. Acta Orthop Belg. 2008;74:846–850. [PubMed] [Google Scholar]
- 16.Digby J.M., Holloway G.M.N., Webb J.K. A study of function after tibial cast bracing. Injury. 1983;14:432–439. doi: 10.1016/0020-1383(83)90094-3. [DOI] [PubMed] [Google Scholar]
- 17.Sarmiento A., Latta L.L. 450 closed fractures of the distal third of the tibia treated with a functional brace. Clin Orthop Relat Res. 2004;428:261–271. doi: 10.1097/01.blo.0000137550.68318.f8. [DOI] [PubMed] [Google Scholar]
- 18.Borg T., Larsson S., Lindsjo U. Percutanous plating of distal tibial fractures- preliminary results in 21 patients. Injury. 2004;35:608–614. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 19.Bahari S., Lenehan B., Khan H., Mcelwain J.P. Minimally invasive percutaneous plate fixation of distal tibia fractures. Acta Orthop Belg. 2007;73:635–640. [PubMed] [Google Scholar]
- 20.Maffuli N., Toms A., McMurtie A., Oliva F. Percutaneous plating of distal tibia fractures. Int Orthop. 2004;28:159–162. doi: 10.1007/s00264-004-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Redfern D.J., Syed S.U., Davies S.J.M. Fractures of the distal tibia: minimal invasive plate osteosynthesis. Injury. 2004;35:615–620. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Hasenboehler E., Rikli D., Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38:365–370. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 23.Williams T., Schenk W. Bridging- minimally invasive locking plate osteosynthesis (Bridging-MILPO): technique description with prospective series of 20 tibial fractures. Injury. 2008;39:1198–1203. doi: 10.1016/j.injury.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Lau T.W., Leung F., Chan C.F., Chow S.P. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008;32(5):697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta R.K., Rohilla R.K., Sangwan K., Singh V., Walia S. Locking plate fixation in distal metaphyseal tibial fractures: series of 79 patients. Int Orthop. 2010;34:1285–1290. doi: 10.1007/s00264-009-0880-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ronga M., Longo U.G., Mafilli N. Minimally invasive locked plating of distal tibia fractures is safe and effective. Clin Orthop Relat Res. 2010;468:975–982. doi: 10.1007/s11999-009-0991-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sitnik A.A., Beletsky A.V. Minimally invasive percutaneous plate fixation of tibia fractures: results in 80 patients. Clin Orthop Relat Res. 2013;471:2783–2789. doi: 10.1007/s11999-013-2841-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hazarika S., Chakravarthy J., Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia. Results in 20 patients. Injury. 2006;37:877–887. doi: 10.1016/j.injury.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 29.Collinge C., Protzman R. Outcomes of minimally invasive plate osteosynthesis for metaphyseal distal tibia fractures. J Orthop Trauma. 2010;24(1):24–29. doi: 10.1097/BOT.0b013e3181ac3426. [DOI] [PubMed] [Google Scholar]
- 30.Stefano G., Santorini F.S., Calderaro M., Giorgini T.L. Minimally invasive plate osteosynthesis in distal tibial fractures: pitfalls and surgical guidelines. Orthopedics. 2004;27(9):903–905. doi: 10.3928/0147-7447-20040901-09. [DOI] [PubMed] [Google Scholar]
- 31.Helfet D.L., Shonnard P.Y., Levine D., Borreli J., Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(suppl 1):A42–A48. doi: 10.1016/s0020-1383(97)90114-5. [DOI] [PubMed] [Google Scholar]
- 32.Oh C.W., Kyung H.S., Park I.H., Kim P.T., Ihn J.C. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003;408:286–291. doi: 10.1097/00003086-200303000-00038. [DOI] [PubMed] [Google Scholar]
- 33.Pai Vasu, Coulter Gareth, Pai Vishal. Minimally invasive plate fixation of the tibia. Int Orthop. 2007;31(4):491–496. doi: 10.1007/s00264-006-0228-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robinson C.M., McLaughlan G.J., McLean I.P., Court-Brown C.M. Distal metaphyseal fractures of the tibia with minimal involvement of the ankle: classification and treatment by locked intramedullary nailing. J Bone Jt Surg Br. 1995;77-B:781–787. [PubMed] [Google Scholar]
- 35.Varsalona R., Liu G.T. Distal tibial metaphyseal fractures: the role of fibular fixation. Strat Traum Limb Recon. 2006;1:42–50. [Google Scholar]


