Abstract
Background:
The recent studies show that Rotavirus is important cause of the acute gastroenteritis. The aim of this review is to estimate the number of Rotavirus infection among Iranian children by performing a systematic review and estimating a pooled data.
Methods:
We performed a systematic literature review in relevant databases including PUBMED, MEDLINE, OVID, SID, MAGIRAN, and IRANMEDEX. Search in databases was done in October 10, 2013. Meta-analysis was performed using the STATA statistical package version 11. We assessed heterogeneity by Q-test and used random model for pooling measures of proportion of Rotavirus infection among Iranian children with diarrhea (and 95% confidence intervals [CI]). Sub group analysis between in-patient and outpatient group were done and publication bias was assessed by Egger and Begg tests.
Results:
A total of 154 records were identified in our searching. There were 36 studies including a total of 15,368 children with diarrhea. Out of 15,368 children, 6,338 were positive for Rotavirus gastroenteritis. Overall pooled estimate of infection with Rotavirus among cases of gastroenteritis was 0.35 (95% CI, 0.28-0.41). Pooled estimates for hospitalized children and outpatient subgroups were 0.39 (95% CI, 0.30-0.48), and 0.31 (95% CI, 0.23-0.38), respectively.
Conclusions:
This study supports the importance of Rotavirus in the Iranian population such as common cause of diarrhea among children. Therefore, decision to adopt immunization programs to prevent Rotavirus infection might be helpful in Iran.
Keywords: Acute gastroenteritis, children, and diarrhea, Rotavirus infection
INTRODUCTION
Acute diarrhea can be particularly detrimental to children, every day killing 2200 infants and children worldwide.[1] Rotavirus infection among uner-5-year-old children is a common cause of childhood gastroenteritis, especially in those countries which has not launched a Rotavirus vaccination program. The initial symptoms associated with Rotavirus infection include watery diarrhea and vomiting, which sometimes aggravates resulting in severe dehydration requiring hospitalization. Every child encounters at least one episode of Rotavirus gastroenteritis by the age of 5 years. Each year, about 2 million subjects have to be hospitalized for developing severe Rotavirus gastroenteritis while about 25 million patients seek medical help by visiting a physician's office or clinic and 111 million cases require care at home.[2,3] Rotavirus infection also causes 527000 deaths annually among children up to 5 years of age worldwide and most of these deaths occur in the developing countries.[4] Rotavirus can be detected in high concentrations in the stool of children suffering from gastroenteritis (1012 viruses/gram). Control measures such as improved sanitation is not effective in preventing this disease.[5,6] Several studies performed in the Middle East showed that approximately 40% of hospitalized patients suffering from gastroenteritis were infected with Rotavirus.[2,7] In Iran, data collected from different geographical regions revealed that the proportion of Rotavirus infection among children with gastroenteritis ranges from 11.6% to 64.67%.[8,9] The emergence of two Rotavirus vaccines (Rotarix® by Glaxo Smith Kline and RotaTeq® by Merck) have markedly reduced the morbidity and mortality associated with severe Rotavirus diarrhea. Therefore, at present, the vaccination strategy to prevent Rotavirus infection has gained tremendous importance. The implementation of universal vaccination program worldwide can decrease the medical and other costs associated with the hospital stay and clinic visits,[10,11] however the epidemiology of Rotavirus is an important element for making decision for such vaccination.
Although, several studies related to Rotavirus infection have been conducted in Iran, precise data for making accurate prediction of the benefits associated with a preventive program required for policy making is not available. The primary aim of this study was to perform a systematic review and meta-analysis on the data published from previous studies in order to calculate pooled estimates of Rotavirus gastroenteritis magnitude (incidence in general population of children and/or proportion of infection in cases with gastroenteritis who admitted to hospitals or visited in the outpatient clinics.
METHODS
We performed a systematic review and meta-analysis of observational studies of Rotavirus, according to the (Meta-analysis Of Observational Studies in Epidemiology) guidelines.[12] Different phases of the study included searching, screening, selecting of studies, extracting data, data cleaning and analyzing.
Search strategy
To retrieve related studies, we used a sensitive librarian-assisted search strategy (follicle stimulating hormone) in relevant databases including, PubMed Medline, Ovid, SID (Scientific information Database), Magiran and Iranmedex since 1/1/1997 onward, in which reported indicators of Rotavirus magnitude were targeted. The last round of search in databases was performed in October 10; 2013. We used sensitive search queries to avoid unwanted loss of information. The following search strategy was developed for MEDLINE via Ovid SP and then adapted to the other resources:
(“Rotavirus Infections/epidemiology” OR “Gastroenteritis/epidemiology” OR “Diarrhea/epidemiology” AND Iran AND (“humans” AND “infant” OR “infant, newborn” OR “infant” OR “child, preschool”[MeSH Terms]).
We did not limit our search to a certain language or time period to avoid missing possible related works. In addition, we did a manual reference checking and citation tracking of related papers thorough Thomson Reuters’ Web of Science, Elsevier's Scopus and Google Scholar.
Inclusion criteria
In this review, cross-sectional or longitudinal studies involving children up to 6 years of age have been included. The infection with Rotavirus in these children were assessed by one of the acceptable laboratory diagnostic tests including the enzyme immunoassay (EIA), rapid test, latex agglutination (LA) test or polyacrylamide gel electrophoresis (PAGE).
Exclusion criteria
Laboratory studies conducted on animals were excluded. Furthermore, studies using nonstandardized methods or clinical outcomes without laboratory confirmation were excluded from this study.
Study selection
Full-texts of the relevant studies were critically appraised for eligibility criteria by two researchers independently (SSH and MML). Unrelated and duplicated articles were excluded based on title and abstract. Flow diagram of articles included in the systematic review is shown in Figure 1.
Figure 1.
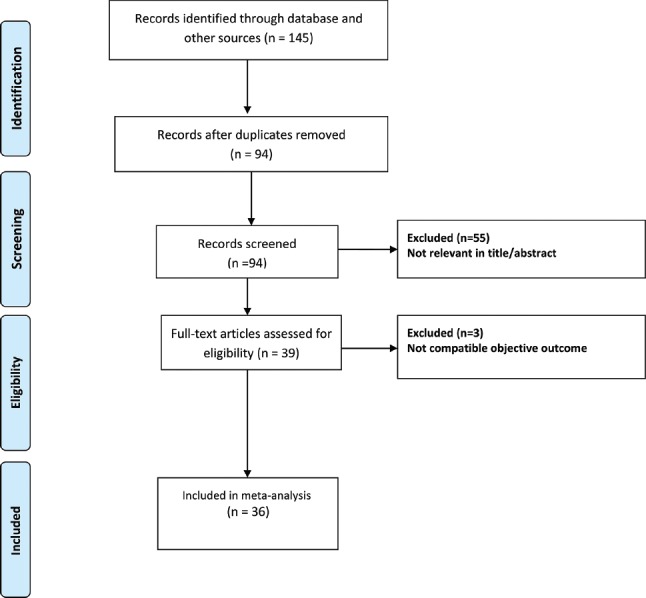
Flow chart of the selection process records
Data extraction
Data extraction was carried out by two researchers (SSH and MML). Bibliographic data, background data (such as sample characteristics), methodological data and epidemiologic data were collected. As the epidemiologic data, we collected nominators and denominators and reported confidence intervals (CI).
Quality assessment
The quality of articles was assessed by the researchers with a checklist of STROBE (Strengthening the Reporting of Observational studies in Epidemiology).[13] The majority of studies selected for this review had been assessed to be of moderate to good quality, but articles thought to be of lower quality were not excluded. The quality of the studies documented in the articles was assessed primarily based on the techniques used for detecting Rotavirus in the reported proportion of gastroenteritis.
Data synthesis
We collected and cleaned data in a Microsoft excel sheet. The data then transferred to statistical package; Meta-analysis was performed using the STATA statistical package version 11. First, we assessed heterogeneity based on the presence of at least one of these two criteria: P value for Cochran's Q-test < 0.1 or Higgins’ I2 statistic of more than 50%. We used random or fixed model for pooling measures of proportion of Rotavirus infection in case of heterogeneous and homogenous studies, respectively. All pooled estimates were reported with 95% CI. Subgroups were determined based on health care utilization type (inpatient and outpatient). Potential publication bias was assessed by Egger regression asymmetry test and Begg adjusted rank correlation test.
RESULTS
Study selection
The electronic searching identified 132 studies from databases and we found 13 other studies by manual searching. Out of these 145 studies, 51 studies were duplicates. After screening of titles and abstracts, 54 studies were excluded from the analysis. The full-texts of 39 relevant articles were checked for eligibility criteria after investigating the full reports, and consequently, 3 studies were excluded. Finally, 36 studies with a total number of 15368 participants were evaluated the proportion of infection with Rotavirus in cases of gastroenteritis [Figure 1]. We found no report about the incidence of Rotaviral infection among healthy children.
Out of total 36 studies selected for this review, 15 studies were conducted in children in outpatient settings[8,9,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28] and 21 studies involved inpatient cases.[8,18,19,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47] Furthermore, three studies involved both inpatient and outpatient settings[8,18,19] A number of studies conducted in the same setting bear similar number and date.
A total of 15,368 children up to 6 years of age were diagnosed with symptoms of acute gastroenteritis, and out of them, the stool samples of 5,884 children were positive for Rotavirus. Out of 15,368 children, 11,371 and 3,997 children were treated in hospitals (inpatient population) and outpatient settings, respectively. Among these cases, 5,166 children of the inpatient population and 1,172 children of the outpatient population were positive for Rotavirus. The range of Rotavirus infection proportions were between 11.36%[8] and 79.0%.[9] The median of Rotavirus positive cases was estimated 0.33 for all studies which was 0.35 and 0.26 for inpatient and outpatient, respectively. The trend showing the median proportion of Rotavirus infection over the calendar time is depicted in [Figure 2]. High proportion of Rotavirus infection was observed form 2006 to 2009 for children in the inpatient setting while similar trend was reported for outpatient setting from 2009 to 2010.
Figure 2.
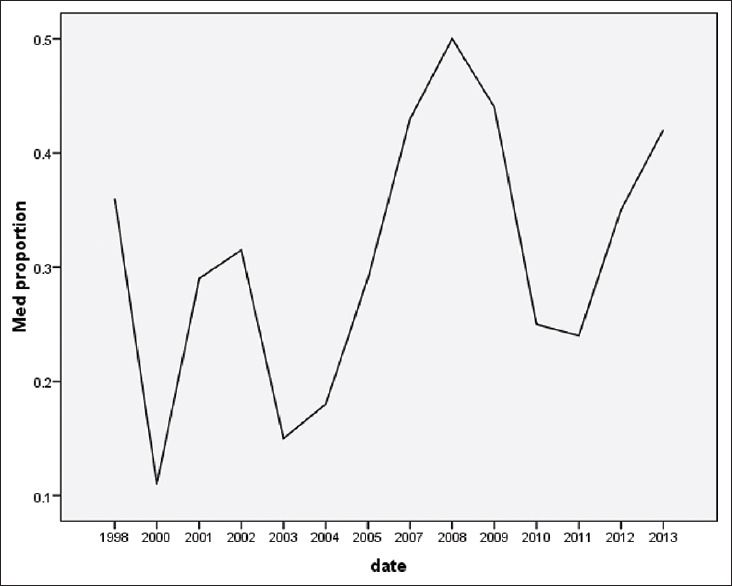
Median proportion Rotavirus gastroenteritis in over time of the study
Our findings showed that there was moderate heterogeneity among these studies (I2 = 50%, Moment-based estimate of between studies variance = 0.03). As a result, statistical analysis was done by random effect model with 95% CI, also subgroup analysis was performed. The results of Meta-analysis using a random effect model revealed an estimate of 0.36 (95% CI: 0.30-0.42) [Figure 3] pooled estimate for inpatient and outpatient population was 0.39 (95% CI: 0.30-0.48) [Figure 4] and 0.31 (95% CI: 0.23-0.38) respectively [Figure 5].
Figure 3.
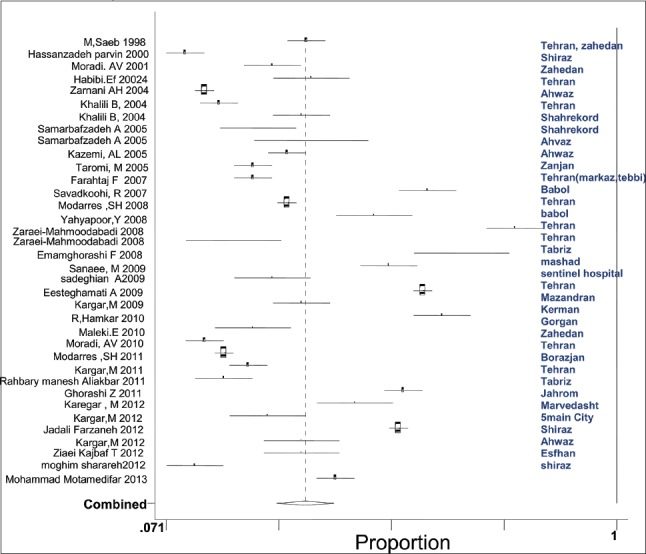
Forest plot of the studies overall combined effects proportion Rotavirus infection in the Iranian children with gastroenteritis for total studies
Figure 4.
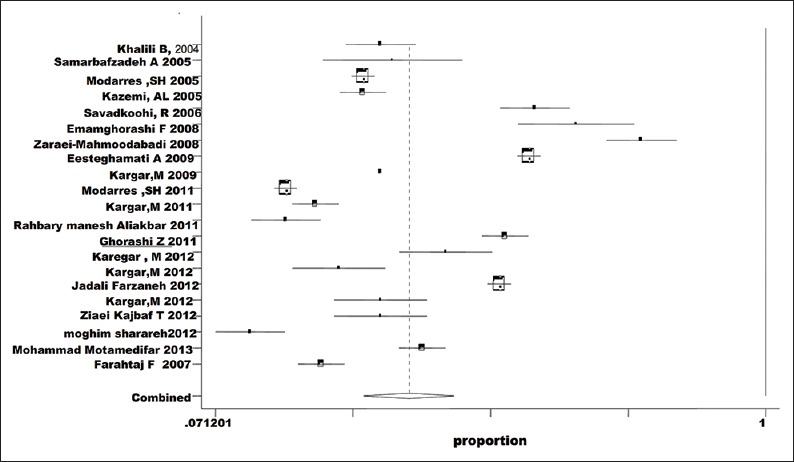
Forest plot of the studies, combined effects proportion rate Rotavirus infection in the hospitalized Iranian children with gastroenteritis
Figure 5.
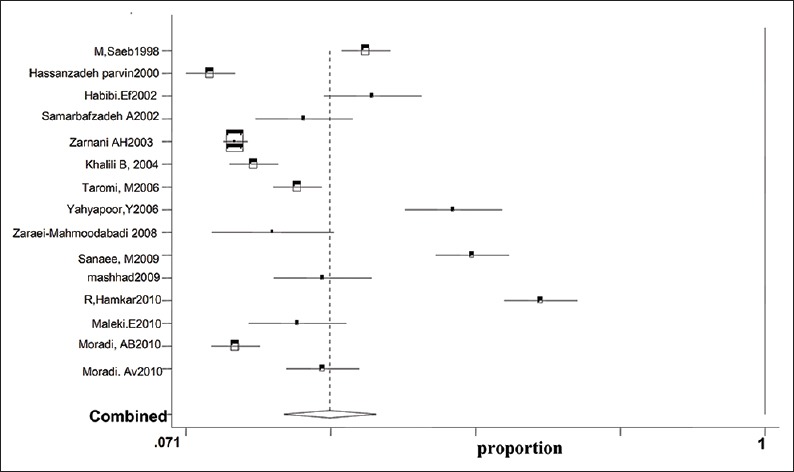
Forest plot of the studies, combined effects proportion Rotavirus infection in the community based Iranian children with gastroenteritis
Publication bias for proportion of cases with Rotavirus was assessed by Eager and Begg test that were not significant. P values for Begg and Egger test were 0.238 and 0.894 respectively.
Seasonal and geographical distribution is demonstrated in Table 1 27 studies have reported seasonal prevalence among which the highest rate of prevalence was found in cold and hot seasons in 21 studies and 6 studies respectively. In addition, the highest prevalence was found in children <2 years.
Table 1.
Details of the studies included in the meta-analysis

In order to minimize bias we use lab test with high sensitivity and specificity for diagnosis virus such as ELISA, PAGE of Rotavirus double-stranded RNA and LA test. Studies using less sensitive methods such as chromatography were excluding from review. 26 studies have used ELISA and EIA method to diagnose the virus [Table 1]. Most studies did not report genotype of the virus, genotype was identified in 13 studies and most frequent genotypes were G1 and G4.
DISCUSSION
According to our study results, the overall proportion of Rotavirus infection among cases of gastroenteritis was 0.36 (95% CI, 0.30-0.42). In addition, this study investigated Rotavirus gastroenteritis occurrences covering a wide region in the country, and the estimated proportion of infection varied from 11.36% in Shiraz to 67.64% in Mazandaran and 79% in Tehran.[8,9,30] There are several variables in these studies that might explain the variance such as different geographical locations, different time periods and seasons, different methods of virus detection, age group, and gender. Furthermore, the proportion can be influenced by the control level of other pathogens of diarrheal diseases. High-percentage of Rotavirus in some provinces might be simply the result of better control of other pathogens. Unfortunately, we did not find useful information for calculating the incidence of Rotaviral diarrhea. In addition, most of these studies have not incorporated enough findings based on molecular epidemiology and the most commonly used method for virus detection has been EIA, ELIZA.
Using ELIZA and EIA method with high sensitivity and specificity leads to reduction bias in virus detection in 76% of studies (26 studies).[51,52] Molecular analysis was performed in 13 studies in which most common types (G1 and G4) have been reported. These types are more similar to the identified types in Europe. Epidemiological surveys in the Mediterranean countries have been variable, and so that increase in a particular genotype has not been found in this area. For instance, G1 has increased in Turkey as well as Iran, but G4 has decreased, on the other hand in Saudi Arabia G2 has increased.[2] Molecular identification of virus types is an important component of incidence and prevalence studies, because it has been considered as a strategy to select type of vaccine. There were no facilities for molecular identification of the virus in this review. Furthermore, the included studies were not designed to do so, well designed epidemiological study in order to investigate the type of the virus seems necessary.
Among 75% of studies in which reported seasonal outbreak, 21 studies have shown an increased prevalence of disease in the cold season. Seasonal prevalence is higher in cold seasons in some countries such as Tunisia, Pakistan and Saudi Arabia and in hot season in Jordan. According to Malek et al., Iran and Egypt does not follow any seasonal trend, but in this review it was demonstrated that most infections occur in the cold season in Iran.[7]
In many cases concurrent infection with Rotavirus included Adenovirus, Astrovirus and some enteric pathogen have been seen that need to correct the approach for diagnostic and treatment.[53]
Four studies have mentioned co-infection with Adenovirus and Astrovirus[25,32,48,50] Ziaei Kajbaf et al., showed that most cases of co-infection with Adenovirus were at 7-12 months and seasonal peak of diseases has been reported in the fall.[48] Co-infection with adenovirus was seen in another study in Shiraz, specific in 24-59 months. Although co-infection rate has reached 29%in some months, Rotavirus infection was higher at all of age.[50] In two studies conducted in Mazandaran, concurrent infection with Adenovirus and Astrovirus were also noted.[21,23]
Many epidemiologic studies have been performed worldwide. In 2010, Malek et al.[7] conducted a review study featuring 20 countries in the Eastern Mediterranean Region (EMR). The median proportion rate of Rotavirus diarrhea in hospitalized children with acute gastroenteritis infection was determined to be 40% (99% CI, 17-46%). The same proportion rate in an outpatient setting was calculated to be 23% (99% CI, 6-41%). Although this review included just one study from Iran in the inpatient category and two studies in the outpatient setting, a high degree of heterogeneity was observed. Findings from recent studies conducted in the EMR by “WHO” indicated that the mortality rate associated with Rotavirus disease and the burden of developing severe Rotavirus infection remain high, in countries with the lowest per capita income, such as Pakistan, Afghanistan, Sudan, Yemen, and Somalia. Countries with higher per capita income have fewer deaths reported from Rotavirus diarrhea. Overall, severe Rotavirus disease among children under 5 years is prevalent in the EMR resulting in higher economic costs.[2]
In another study covering the Middle East Region, Khoury et al.[2] determined the overall percentage of Rotavirus detection among gastroenteritis cases ranging from 16% to 61%.[7] This report showed that the overall detection of Rotavirus in gastroenteritis episodes was lowest in countries such as Saudi Arabia, Tunisia and Egypt (16-23%) and countries with higher detection of Rotavirus infection included Syria (61%) and Oman (51%).[7] The overall annual detection of Rotavirus gastroenteritis reported by WHO in the EMR was 42%, and this included Egypt, Iran, Iraq, Jordan, Libya, Morocco, Oman, Syria, Tunisia and Yemen.[7]
The estimated range (30-42%) derived from our study is similar to the results observed in some of the Middle East countries such as Iraq, Jordan, and Morocco. Furthermore, Khoury et al.[2] showed that in Iran and Egypt, the proportion of Rotavirus gastroenteritis have increased over time (15% in 2003-2004 vs. 59% in 2005-2006). However, in this review only two studies were included from Iran. The mentioned figure is not completely compatible with our results (from 36 different studies) [Figure 2].
One of the limitations associated with the present study is the lack of adequate data because of limited access to databases. As illustrated in [Figure 2], the proportion of Rotavirus detection in cases with gastroenteritis increased over time from 2006 to 2010, although, the median proportion rate of Rotavirus infection did not show any specific trend with respect to time. We did not stratified results based on age, gender and virus genotype and this shortcoming was mainly due to lack of adequate information on these factors in most of the articles used for this review. However, findings from a study conducted in the regions of Mazandaran, Zahedan, Gorgan and Babol indicated that in children <2 years of age are a higher proportion of Rotavirus infection especially in the cold season.
Another important factor that can cause underestimation of Rotavirus infection is the display of symptoms. Rotavirus associated diarrhea was the ubiquitous symptom reported among children admitted to clinics or hospitals, other symptoms of gastroenteritis such as vomiting or abdominal pain without diarrhea were hardly reported. Phillips et al.[54] indicated that the prevalence of asymptomatic Rotavirus infection was 11% from the general population of England. In addition, Abiodun et al.[55] showed that the incidence of asymptomatic Rotavirus infection was 19.1% and 15.1% in boys and girls respectively in Nigeria.
In our review, Rotavirus infection in 86% of cases was higher in boys than girls.
Conducting virus detection tests for all the associated symptoms of gastroenteritis might change Rotavirus infection particularly in community-based studies. In addition, the lack of reliable epidemiologic data involving nosocomial and home care cases can also affect our estimated proportion. Information obtained from worldwide reports indicated that nearly 111 million cases of Rotavirus gastroenteritis were treated at home only.[2] In cases of limited access, the proportion of people who do not seek care from an outpatient or inpatient facility will be higher. The care seeking behavior is not influenced balanced for all pathogens, because of the difference in severity of symptoms.
CONCLUSIONS
The present review showed the importance of Rotavirus in children with diarrhea in Iran. Among the various pathogens causing gastroenteritis, Rotaviruses leads to the most severe form of acute gastroenteritis among children <6 year of age.[56] Preventive measures such as improved sanitation are not sufficient to combat Rotavirus transmission.
Based on the IrMIDHS, 13.5% of under-5-year-old children had experiences diarrheal diseases within 2 weeks before the survey, and 59.5% were visited in an outpatient or inpatient facility.[57] Although, Rotavirus might not be the causal pathogen in all children with laboratory proven Rotavirus infection, it certainly has important quota among total cases of diarrhea. To be more useful, the present study should be completed by prevalence of Rotavirus in the general population of asymptomatic children. We think the results of this study can be used in combination with other evidences for making decision regarding the introduction of the vaccine against Rotavirus.
Since, once infected with Rotavirus does not provide permanent safety, implementing vaccination program against Rotavirus not only could be averted Rotavirus infection disease, but also it could be saved medical and social cost. Performing cost effectiveness study and the priority setting investigation seem necessary. Due to variety type of vaccine could be effected certain genotype, high level evidence should be determined in order to make a decision about certain type of vaccination.
ACKNOWLEDGMENTS
We express our appreciation to Dr. Arash Rashidian, head of the NIHR and also to our colleagues Ms. Saeedeh Babashahi and Mr. Mohammad Reza Mobinizadeh for their participation in reviewing studies.
Footnotes
Source of Support: This study was supported by the Iran National Institute of Health Research (Iran NIHR, grant number: 241/M/471)
Conflict of Interest: None declared.
REFERENCES
- 1.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: An updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 2.Khoury H, Ogilvie I, El Khoury AC, Duan Y, Goetghebeur MM. Burden of rotavirus gastroenteritis in the Middle Eastern and North African pediatric population. BMC Infect Dis. 2011;11:9. doi: 10.1186/1471-2334-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) Rotavirus surveillance – Worldwide, 2001-2008. MMWR Morb Mortal Wkly Rep. 2008;57:1255–7. [PubMed] [Google Scholar]
- 4.Glass RI, Bresee JS, Turcios R, Fischer TK, Parashar UD, Steele AD. Rotavirus vaccines: Targeting the developing world. J Infect Dis. 2005;192(Suppl 1):S160–6. doi: 10.1086/431504. [DOI] [PubMed] [Google Scholar]
- 5.WHO. Estimated rotavirus deaths for children under 5 years of age. [Last accessed on 2006 Mar 31]. Available from: http://www.who.int/immunization/monitoring_surveillance/burden/estimates/rotavirus/Global_national_estimates_2004_deaths_under_age_five_attributable_to_rotavirus_infection_2004.pdf .
- 6.Bhan A, Green SK. Balancing safety, efficacy and cost: Improving rotavirus vaccine adoption in low-and middle-income countries. J Glob Health. 2011;1:148–53. [PMC free article] [PubMed] [Google Scholar]
- 7.Malek MA, Teleb N, Abu-Elyazeed R, Riddle MS, Sherif ME, Steele AD, et al. The epidemiology of rotavirus diarrhea in countries in the Eastern Mediterranean Region. J Infect Dis. 2010;202(Suppl):S12–22. doi: 10.1086/653579. [DOI] [PubMed] [Google Scholar]
- 8.Mahmoodabadi BZ, Kargar M, Tabatabaei H, Saedegipour S, Ghaemi A, Nategh R. Determination of annual incidence, age specific incidence rate and risk of rotavirus gastroenteritis among children in Iran. Iran J Virol. 2009;3:39–42. [Google Scholar]
- 9.Hassanzadeh P, Al-e-Yasin F. The prevalence of bacterial and viral agents in fecal specimens of children in Shiraz. J Kerman Univ Med Sci. 1379;1:11–6. [Google Scholar]
- 10.Ruiz-Palacios GM, Pérez-Schael I, Velázquez FR, Abate H, Breuer T, Clemens SC, et al. Safety and efficacy of an attenuated vaccine against severe rotavirus gastroenteritis. N Engl J Med. 2006;354:11–22. doi: 10.1056/NEJMoa052434. [DOI] [PubMed] [Google Scholar]
- 11.Vesikari T, Matson DO, Dennehy P, Van Damme P, Santosham M, Rodriguez Z, et al. Safety and efficacy of a pentavalent human-bovine (WC3) reassortant rotavirus vaccine. N Engl J Med. 2006;354:23–33. doi: 10.1056/NEJMoa052664. [DOI] [PubMed] [Google Scholar]
- 12.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007;370:1453–7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 14.Saeb M, Morady A, Mokhtariazad T, Sajedianfard J. Determination of electrophoretype of Rotaviruses causative agents of diarrhea in children under two years old referred to Tehran and Zahedan hospitals. J Kerman Univ Med Sci. 1997;4:101–6. [Google Scholar]
- 15.Moradi AV, Mokhtari-Azad T. Rotavirus infection in under 6 years old children with acute diarrhea. Tabib-e-Shargh. J Zahedan Univ Med Sci Health Serv. 2001;1:28–3. [Google Scholar]
- 16.Habibi E, Ghorbani Sh, Jarollahi, Zali MR. Serotyping of group a Rotaviruses in children less than 7 years old in Tehran. Pejouhesh. 2004;28:211–4. [Google Scholar]
- 17.Zarnani AH, Modarres Sh, Jadali F, Sabahi F, Moazzeni SM, Vazirian F. Role of Rotaviruses in children with acute diarrhea in Tehran, Iran. J Clin Virol. 2004;29:189–93. doi: 10.1016/S1386-6532(03)00123-9. [DOI] [PubMed] [Google Scholar]
- 18.Samarbafzadeh A, Tehrani EM, Makvandi M, Taremi M. Epidemiological aspects of Rotavirus infection in Ahwaz, Iran. J Health Popul Nutr. 2005;23:245–9. [PubMed] [Google Scholar]
- 19.Khalili B, Cuevas LE, Reisi N, Dove W, Cunliffe NA, Hart CA. Epidemiology of Rotavirus diarrhoea in Iranian children. J Med Virol. 2004;73:309–12. doi: 10.1002/jmv.20092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taremi M, Farahtaj F, Gachkar L, Adalatkhah H, Zali MR, Fayaz A. Epidemiological survey of Rotavirus infection among children less than 5 years with acute diarrhea admitted in markaz tebbi pediatric hospital, Tehran 2003-4. Iran J Infect Dis Trop Med. 2005;10:13–21. [Google Scholar]
- 21.Savadkoohi RB, Ahmadpour-Kacho M, Yahyapour Y. Prevalence of viral gastroenteritis in children with acute gastroenteritis in Babol, Iran. J Pediatr Infect Dis. 2007;2:211–4. [Google Scholar]
- 22.Farahtaj F, Gallimore CI, Iturriza-Gomara M, Taremi M, Zali MR, Edalatkhah H, et al. Rotavirus VP7, VP4 and VP6 genotypes co-circulating in Tehran, Iran, between 2003 and 2004. Epidemiol Infect. 2007;135:834–8. doi: 10.1017/S0950268806007485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yahyapour Y, Savadkoohi R, Hajian K, Somayyeh J, Rasool H. Prevalence of Rota, adeno and astrovirus in children with acute gastroenteritis in Babol, Iran. J Gorgan Univ Med Sci. 2008;10:67–70. [Google Scholar]
- 24.Hamkar R, Yahyapour Y, Noroozi M, Jalilvand S, Adibi L, Vaziri S. Prevalence of viral agents in, children with acute gastroenteritis in Mazandaran Province during 1383-1384. Iran J Infect Dis Trop Med. 2008;12:35–40. [Google Scholar]
- 25.Sanaei M, Radpour H, Steghamati AA, Keshtkar AA, Nasiri M, Nochi Z. A survey on prevalence and genotyping Rotavirus in children with acute gastroenteritis in Tabriz. J Kurdistan Univ Med Sci. 2009;13:69–77. [Google Scholar]
- 26.Sadeghian A, Hamedi A, Sadeghian M, Sadeghian H. Incidence of rotavirus diarrhea in children under 6 years referred to the Pediatric Emergency and Clinic of Ghaem Hospital, Mashhad, Iran. Acta Med Iran. 2010;48:263–5. [PubMed] [Google Scholar]
- 27.Maleki E, Daie-Parizi MH, Arabzadeh SA. Relative frequency of Rotavirus gastroenteritis in children belo3 years old with acute gastroenteritis referred to Afzalipour hospital in autumn. J Kerman Univ Med Sci. 2010;17:130–6. [Google Scholar]
- 28.Moradi AV, Tabarrae A, Roshandel Gh, Ghaemi EZ, Bazoori M. Rotavirus infection in under 6 years old children with acute diarrhea in Gorgan, Iran. Iran J Infect Dis Trop Med. 2010;15:55–9. [Google Scholar]
- 29.Modarres SH, Manesh AA, Modarres SH, Faghihzadeh S, Jamafzon F. The role of Rotavirus in acute gastroenteritis and molecular epidemiology pattern of Rotavirus infection in hospitalized children in Tehran. Iran J Infect Dis Trop Med. 2005;10:21–7. [Google Scholar]
- 30.Kazemi A, Sofiani AZ, Zadeh AE, Shykhi A, Movsavinasab N. The comparison of clinical and laboratory findings in gasteroenteritis of Rotavirus and others etiology in 2 months to 5 years old admitted patients, Zanjan 1383. J Zanjan Univ Med Sci Health Serv. 1385;57:32–8. [Google Scholar]
- 31.Emamghorashi F, Rajabi SH, Shadmand A, Zendegani N, Rabiee S, Tajarod Z. Frequency of Rotavirus infection in children with acute gastroenteritis in Jahrom, South of Iran. Iran J Med Sci. 2008;33:84–7. [Google Scholar]
- 32.Eesteghamati A, Gouya M, Keshtkar A, Najafi L, Zali MR, Sanaei M, et al. Sentinel hospital-based surveillance of rotavirus diarrhea in iran. J Infect Dis. 2009;200(Suppl 1):S244–7. doi: 10.1086/605050. [DOI] [PubMed] [Google Scholar]
- 33.Kargar M, Jaafarpour T, Yaghobi R, Kargar M, Ghodsi M, Homaun M. Proceeding of 3rd Congress of Iranian Clinical Microbiology. Shiraz, Iran: 2009. Oct, Detection and genetic characterization of group a Rotavirus strains circulating among children with acute gastroenteritis in Shiraz during 2006-2007. [Google Scholar]
- 34.Kargar M, Zare M. High frequency of mixed genotypes Rotavirus among children hospitalized with acute gastroenteritis in Marvdasht during 2007-2008. Iran J Infect Dis Trop Med. 2010;15:1–5. [Google Scholar]
- 35.Kargar M, Abadi BZ, Tabatabaei H. Genotyping of VP7 protein with nested RT-PCR in children hospitalized in Tehran. Iran J Infect Dis Trop Med. 2008;12:11–7. [Google Scholar]
- 36.Modarres S, Rahbarimanesh AA, Karimi M, Modarres S, Motamedi-Rad M, Sohrabi A, et al. Electrophoretic RNA genomic profiles of Rotavirus strains prevailing among hospitalized children with acute gastroenteritis in Tehran, Iran. Arch Iran Med. 2008;11:526–31. [PubMed] [Google Scholar]
- 37.Kargar M, Akbarzadeh A, Yaghobi R. Molecular and serological characterization of group a rotavirus isolates obtained from hospitalized children in Jahrom. J Shahrekord Univ Med Sci. 2010;12:15–21. [Google Scholar]
- 38.Kargar M, Najafi A, Zandi K, Barazesh A. Frequency and demographic study of Rotavirus acute gastroenteritis in hospitalized children of Borazjan city during 2008-2009. J Shahid Sadoughi Univ Med Sci Health Serv. 2011;19:94–103. [Google Scholar]
- 39.Kargar M, Akbarzadeh A, Yaghobi R. Epidemiological features of Rotaviral, bacterial, and parasitic infections among hospitalized children in Jahrom during 2006-2007, Iran. J Qazvin Univ Med Sci. 2011;14:34–41. [Google Scholar]
- 40.Modaress S, Rahbarimanesh AA, Edalat R, Sohrabi A, Modarres S, Gomari H, et al. Human rotavirus genotypes detection among hospitalized children, a study in Tehran, Iran. Arch Iran Med. 2011;14:39–45. [PubMed] [Google Scholar]
- 41.Manesh AA, Saberi H, Modarres SH, Salamati P, Akhtarkhavari H, Hagshenas Z. A study of genetic diversity and phylogenetic analysis of Rotavirus genotypes VP4 [P] in hospitalized children with acute diarrhea in pediatric Bahrami Hospital. Tehran Univ Med J. 2011;69:455–45. [Google Scholar]
- 42.Ghorashi Z, Behbahan AG, Oskouei SA. Rotavirus enteric infection in children of northwest Iran. Pediatr Infect Dis J. 2011;30:616–8. doi: 10.1097/INF.0b013e31820a45cb. [DOI] [PubMed] [Google Scholar]
- 43.Jadali F, Karimi A, Fallah F, Zahraei M, Esteghamati A, Navidinia M, Adabian S. A survey on Rotavirus associated Diarrhea in 5 main cities of Iran. Arch Pediatr Infect Dis. 2012;1:23–6. [Google Scholar]
- 44.Moghim SH, Manesh SH, Nafise SH, Azadani H. Frequency of Rotavirus in children under 3 years of old with gastroenteritis in ALZAHRA Hospital. J Isfahan Med Sch. 2012;30:210. [Google Scholar]
- 45.Kargar M, Akbarzadeh A. Prevalence and molecular genotyping of group a Rotaviruses in Iranian children. Indian J Virol. 2012;23:24–8. doi: 10.1007/s13337-012-0070-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Najafi A, Kargar M, Jafarpour T. Burden and typing of rotavirus group a in children with acute gastroenteritis in Shiraz, Southern Iran. Iran Red Crescent Med J. 2012;14:531–40. [PMC free article] [PubMed] [Google Scholar]
- 47.Kargar M, Zare M, Najafi A. Molecular epidemiology of Rotavirus strains circulating among children with gastroenteritis in Iran. Iran J Pediatr. 2012;22:63–9. [PMC free article] [PubMed] [Google Scholar]
- 48.Ziaei Kajbaf T, Shamsizadeh A, Kalvandi GH, Macvandi M. Relative Frequency of Rotavirus and adenovirus among children aged 1-60 months hospitalized with acute Diarrhoea in South-Western, Iran. Jundishapur J Microbiol. 2012;6:47–50. [Google Scholar]
- 49.Kargar M, Jafarpour T, Najafi A. Epidemiology survey of group a Rotavirus infection among children under 5 years with acute diarrhea. Zahedan J Res Med Sci. 2013;14:43. [Google Scholar]
- 50.Motamedifar M, Amini E, Talezadeh Shirazi P. Frequency of rotavirus and adenovirus gastroenteritis among children in Shiraz, Iran. Iran Red Crescent Med J. 2013;15:729–33. doi: 10.5812/ircmj.4415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Raboni SM, Nogueira MB, Hakim VM, Torrecilha VT, Lerner H, Tsuchiya LR. Comparison of latex agglutination with enzyme immunoassay for detection of Rotavirus in fecal specimens. Am J Clin Pathol. 2002;117:392–4. doi: 10.1309/MUR1-05A4-184Q-QCTR. [DOI] [PubMed] [Google Scholar]
- 52.Atchison CJ, Lopman BA, Harris CJ, Tam CC, Iturriza Gómara M, Gray JJ. Clinical laboratory practices for the detection of Rotavirus in England and Wales: Can surveillance based on routine laboratory testing data be used to evaluate the impact of vaccination? Euro Surveill. 2009;14:19217. doi: 10.2807/ese.14.20.19217-en. [DOI] [PubMed] [Google Scholar]
- 53.Akan H, Izbirak G, Gürol Y, Sarikaya S, Gündüz TS, Yilmaz G, et al. Rotavirus and adenovirus frequency among patients with acute gastroenteritis and their relationship to clinical parameters: A retrospective study in Turkey. Asia Pac Fam Med. 8:8. doi: 10.1186/1447-056X-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Phillips G, Lopman B, Rodrigues LC, Tam CC. Asymptomatic Rotavirus infections in England: Prevalence, characteristics, and risk factors. Am J Epidemiol. 2010;171:1023–30. doi: 10.1093/aje/kwq050. [DOI] [PubMed] [Google Scholar]
- 55.Abiodun PO, Ihongbe JC, Ogbimi A. Asymptomatic rotavirus infection in Nigerian day-care centres. Ann Trop Paediatr. 1985;5:163–5. doi: 10.1080/02724936.1985.11748385. [DOI] [PubMed] [Google Scholar]
- 56.Mathew MA, Paulose SA, Chitralekha, Nair MK, Kang G, Kilgore P. Prevalence of Rotavirus diarrhea among hospitalized children less than 5 years in Kerala, South India. Indian Pediatr. 2014;51:27–31. doi: 10.1007/s13312-014-0329-8. [DOI] [PubMed] [Google Scholar]
- 57.Rashidian A, Karimi-Shahanjarini A, Khosravi A, Elahi E, Beheshtian M, Shakibazadeh E, et al. Iran Multiple Indicator Demographic and Health Survey (IrMIDHS-2010): Study protocol. Int J prev Med. 2014;5:632–42. [PMC free article] [PubMed] [Google Scholar]


