Abstract
Background:
Nowadays, there has been a growing trend of caesarean sections in Iran. One reason would be the mother's desire. Increased maternal self-efficacy can be an important step to reduce percentage of cesarean. This study aimed to determine the effectiveness of training-based strategies to increase the self-efficacy for choosing delivery method among pregnant women in Shahrekord city.
Methods:
This quasi-experimental study was conducted on 130 pregnant women who attended urban health centers in Shahrekord city in 2013. Intervention was applied in the experimental group in three sessions in about 60-90 min while control group did not receive any intervention. Fear of childbirth and self-efficacy questionnaire was completed before and after training.
Results:
While mean scores of the fear of childbirth, expectations and childbirth self-efficacy before the intervention between the two groups were not significantly different (P > 0.05), mean scores of childbirth in intervention group was reduced and expectation and childbirth self-efficacy had a significant increase after intervention (P < 0.05). In this study, 71.4% of mothers in intervention group and 53.8% of control mothers naturally delivered their children. Most of intervention group mothers desired to deliver through cesarean and had more fear (P < 0.001) but lower childbirth expectation (P > 0.05) and self-efficacy (P < 0.001) than those who chose normal method.
Conclusions:
Our findings showed that training-based self-efficacy procedure has been effective in encouraging mothers to choose natural childbirth. Therefore, the design and implementation of curriculum-based strategies for increasing self-efficacy is suggested for pregnant women.
Keywords: Cesarean delivery, efficacy, elective cesarean, natural delivery
INTRODUCTION
Pregnancy is the most important physiological phenomenon which ends with childbirth, associated with the fear and worries.[1] Therefore, mother and child health system is a sensitive and important health care issue in all communities (with or without concern of cesarean delivery).[2] Although cesarean has had an important role in reducing the complications of childbirth as well as mortality and morbidity of mother and fetus in past centuries; however, the present concern is the high rate of cesarean.[1] World Health Organization (WHO) has predicted the rate of cesarean delivery about 10-15% of total deliveries; however, this rate varies in different parts of the world; and indeed it is increasingly rising.[2] The cesarean rates differ from 5-25% during the last 20 years which was different at the national and international levels as well.[3] For example, cesarean rates ranged from 4.5% to 38% of all births in the United States from 1970 to 2007.[2] Based on the 2004 report of WHO, the rate is approximately 20-25% in Canada, 32.6% in India, 21% in UK, 10.7% in Sweden, almost 10% in United Arabic Emirates and 35% in Iran.[3] In 2007, the cesarean rate of Iran was 42.3[3] and about 50-65% of all deliveries were cesarean in 2010.[4] Even, in Chaharmahal and Bakhtiari province, a relatively small province in southwest of Iran, the cesarean rate was 44% of total deliveries.[5]
Many factors can lead to cesarean section such as medical problems; however, nowadays the most common non-medical reason which may increase the rate of cesarean is maternal request,[6] despite its huge cost for families as well as potential problems of personnel and medical supplies for hospitals.[1] According to Lewis theory, pain and fear associated with cesarean section could affect mother's decision, because they think that they will experience less pain in cesarean delivery.[7] In a study conducted by Rayding on Swedish women, 36% of them had a fear of labor pain which was their main reason to have a cesarean delivery.[8] In addition, Zafarghandi and colleagues reported the higher prevalence of childbirth's fear (about 59%) as well as anxiety among women who had requested a cesarean section compared to those who chose natural childbirth.[9] In fact, many women are afraid of labor pain and they think that its pain is out of their capability to deliver a baby naturally as well as their concerning about their health; if the mother feels to have enough ability to cope with stress as well, she will be protected from adverse impacts of stress on her health.[8,10,11]
Training and giving guidelines to pregnant women can indeed help them through rising their awareness about childbirth and the related psychological readiness improvement to cope with labor pain;[1] which, in turn, is important to choose the best delivery method; and may reduce the unnecessary cesarean sections which is usually done by health educators.[12] The self-efficacy could be the most important prerequisite for behavior in stressful situations. For example, Bandura, a psychologist, expressed self-efficacy in his social learning theory which states that self-efficacy includes self-assessment of one's own ability to cope with stressful situations.[13] In fact, a relationship between fear of childbirth, self-efficacy and natural childbirth may exist; if a pregnant woman thinks that she cannot control labor situation, her fear and anxiety will lead her to choose cesarean delivery without medical reasons.[13,14] Moreover, due to the importance of self-efficacy in controlling fear and pain of labor and suitable delivery method, educational intervention strategies designated to increase self-efficacy could reduce the fear and may enhance the ability of mothers to overcome the pain of labor and cesarean cut. Therefore, the aim of present study was to find out the effect of educational intervention based on self-efficacy on the delivery choice among pregnant women in Shahrekord city, Iran in 2013.
METHODS
Study design and participants
This quasi-experimental study was conducted in 2013. The participants were 130 randomly selected pregnant women of 24-32 weeks of gestation referred to the urban health centers. Using stratified random sampling, pregnant women referring to all eight urban health centers of Shahrekord city were randomly classified into two groups (intervention and control) and based on the population distribution of each center were randomly divided into two equal groups (n = 65 for each group). Inclusion criteria was all pregnant women at 24-32 weeks of pregnancy, centers who were willing to participate in the study. Exclusion criteria included medical indications for cesarean section (previous cesarean, dystocia, embryonic distress and breech view) and the cases of premature delivery or emergency caesarean delivery and cases who did not want to cooperate. Two of the mothers in the intervention group were excluded from the study due to premature birth.
This proposal was approved by the Research Council of Isfahan University of Medical Sciences in terms of ethical points and all mothers entered the study filled a consent form. Also the questionnaires were given anonymously in order to assure confidentiality.
Variable assessment and study instruments
We used a questionnaire which its validity and reliability of self-efficacy questionnaire has been examined and verified by Khorsandi and colleagues.[15] In another study, the validity and reliability of the questionnaire titled childbirth fear were also examined and verified by Khorsandi and colleagues.[13] The questionnaires were completed in both intervention and control groups at the first visit. Then the educational intervention was conducted in the intervention group and the control group received routine care during pregnancy. The questionnaire administered consisted of three parts: Demographic information (age, age at marriage, education, occupation and history of cesarean among relatives), questions related to childbirth fear and questions about the self-efficacy of delivery. The questionnaire titled with delivery fear included 14 questions using Likert score. Delivery self-efficacy questionnaire itself consisted of two parts: The first part with 17 questions on outcome expectation and the second part on expected delivery self-efficacy with another 17 questions. Validity and reliability of self-efficacy questionnaire has been examined and verified by Khorsandi and colleagues in Iran.[15] In another study, the validity and reliability of the questionnaire titled childbirth fear were examined and verified by Khorsandi and colleagues in Iran.[13] Outcome and self-efficacy expectations could be considered as “a belief on that the expected behavior would result in special outcome” and “a belief that one enables to do necessary behaviors in special situations”, respectively.[13]
The intervention group participated in three 60-90 min sessions during a week (including 8-10 persons in each session) which in sessions, they have received extra education (more than routine prenatal care they usually received). Educational content was developed based on strategies of self-efficacy increase (success in performance, replace experience, verbal persuasion and physiological or emotional states). In first session, mothers were introduced to each other, and each of the mothers were allowed to talk about the causes of childbirth fear as well as their maternity imagination and also the reason of program and panel discussion and the participants were given equal opportunity for free expression of their ideas and their viewpoints. After collection of childbirth fear causes, the educational content was prepared based on it. At second session, by inviting a successful normal (vaginal) birth delivered mother to express her experience, the participants were practically familiar with the normal method. Then, the training were continued with explaining maternal anxiety and its effects on the fetus, stating the benefits of natural childbirth, cesarean side-effects, reasons for emergency caesarean section and Kegel exercise training; pelvic floor exercise, or Kegel exercise, consists of repeatedly contracting and relaxing the muscles that form part of the pelvic floor, now sometimes colloquially referred to as the “Kegel muscles”.[3,16] Finally, at third session, the Kegel's exercises were illustrated to ensure that it is perform in a correct way. Full interpretation of natural childbirth, labor characteristics, childbirth stages and effective actions during these stages and natural childbirth education using instructional videos were also applied. At the end of each training session, it has been given enough time to mothers to answer their questions.
Instruction was performed by Lecture, group discussion and question and answer. In addition, the educational pamphlets about the characteristics of the labor and natural delivery process were placed at mother's disposal. After the above mentioned three sessions, through two further telephone conversations, mothers were given some tips about doing Kegel exercises and mothers were encouraged to do exercises 2-3 times a day and their potential questions were answered. The final evaluation was done by recompleting questionnaire 1-month after training in both groups. Information about the actual method of delivery was collected by calling mothers in both groups.
Statistical analysis
Data analysis was performed using SPSS 16 Software (Chicago, SPSS Inc.) by using descriptive statistics (mean, frequency and standard deviation) and inferential statistics such as independent t-test, paired t-test, Chi-square and Mann–Whitney tests. P < 0.05 was considered as the level of significance.
RESULTS
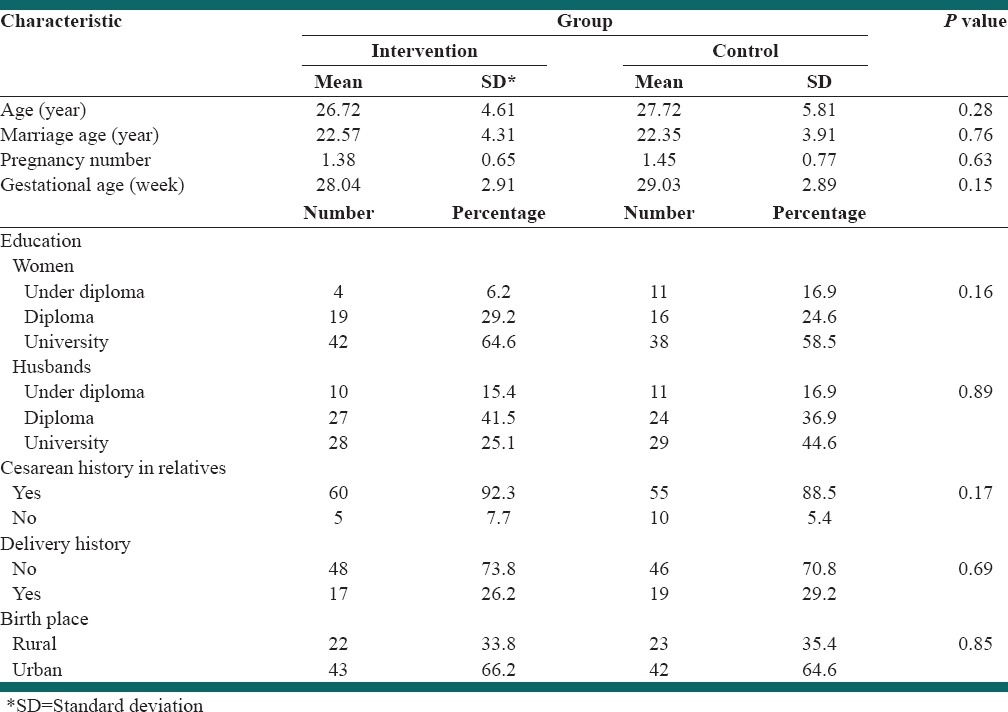
The mean age of mothers were 26.72 ± 4.61 and 27.72 ± 5.81 year in intervention and control groups, respectively [Table 1]. The mean marriage age, pregnancy number and gestational age in intervention group were 22.57 ± 4.31 year, 1.38 ± 0.65 times and 28.04 ± 2.91 week, respectively. The figures in control group were 22.35 ± 3.91 year, 1.45 ± 0.77 times and 29.03 ± 2.89 week, respectively, with no significant difference (P > 0.05). Education of most of women in both groups were university level; however, for husbands, the university level of education was more in control group (P > 0.05). Most of the mothers in both groups had cesarean history in relatives, no history of delivery and belonged to urban area.
Table 1.
Main characteristics of participants
Most of intervention group mothers desired to deliver through cesarean [Table 2]. They had more fear (P < 0.001) but lower childbirth expectation (P > 0.05) and self-efficacy (P < 0.001) than those who chose normal method.
Table 2.
Distribution of mother's delivery in both groups
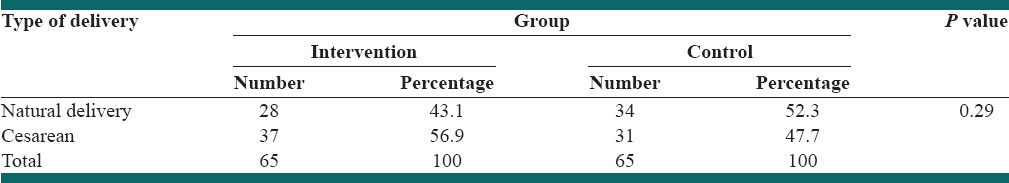
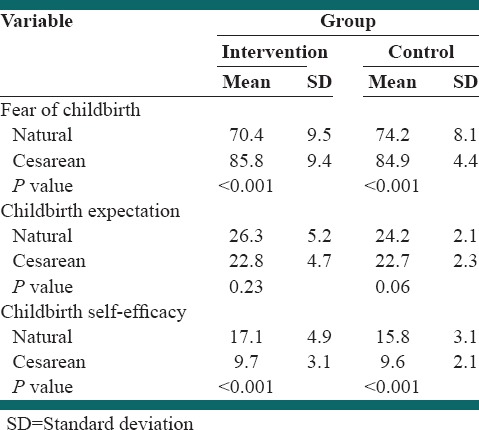
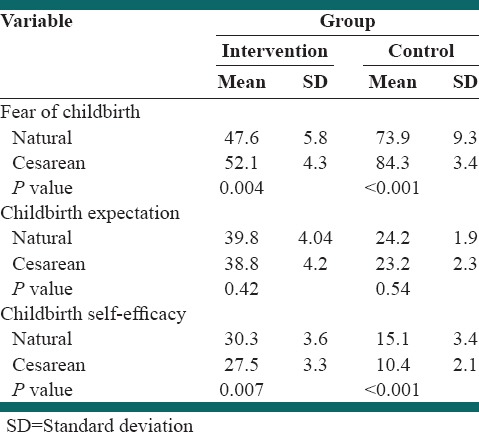
Table 3 demonstrates the comparison of baseline mean scores on fear of childbirth, childbirth expectation and childbirth self-efficacy in both intervention and control groups with two delivery methods. While there was no difference in delivery method and mean scores of childbirth expectation in both groups (P > 0.05); there was a statistically significant difference in mean scores of fear of childbirth and childbirth self-efficacy in both groups with delivery method (P < 0.001).
Table 3.
Comparison of baseline (before intervention) fear of childbirth, childbirth expectation and childbirth self-efficacy mean scores and delivery method in both groups
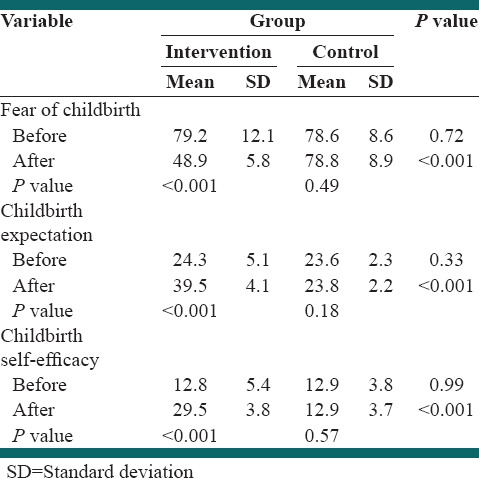
There was a significant difference between two groups in terms of childbirth fear, childbirth expectation and childbirth self-efficacy after (P < 0.001) but not before intervention (P > 0.05) [Table 4]. There was a statistically significant difference before and after intervention only in intervention group (P < 0.001) but not in control group (P > 0.05).
Table 4.
Comparison of fear of childbirth, childbirth expectation and childbirth self-efficacy mean scores before and after the educational intervention
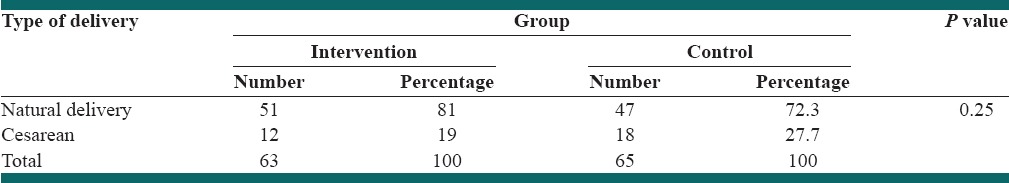
This study showed 71.4% of mothers in the intervention group and 53.8% of control group mothers used NVD [Table 5].
Table 5.
Comparison of fear of childbirth, childbirth expectation and childbirth self-efficacy mean scores before and after the educational intervention
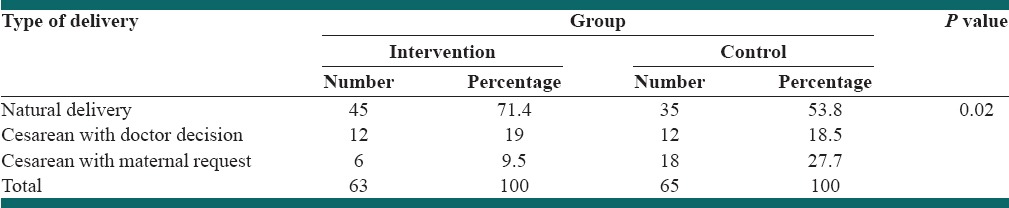
Table 6 shows the mean scores of childbirth fear, childbirth expectation and childbirth self-efficacy between mothers with natural and cesarean delivery. Our findings showed that the childbirth fear mean score of women who chose natural childbirth was less than in those who have had a cesarean section in both groups (P < 0.05) while the higher self-efficacy was observed in the mean scores (P < 0.05). There was no significant difference in expected childbirth scores (P > 0.05).
Table 6.
Comparison of fear of childbirth, childbirth expectation and self-efficacy mean scores with final delivery method selection in both intervention and control groups after educational intervention
Based on the results, only 23.4% of women said they would choose cesarean delivery next time, as there was no significant difference between intervention and control groups [Table 7].
Table 7.
Distribution of desire for future delivery in both intervention and control groups
DISCUSSION
Our study showed a significant difference between intervention and control groups in terms of mean scores of childbirth fear, childbirth expectation and childbirth self-efficacy after the intervention. In addition, more mothers in intervention group than mothers in control group had a natural delivery which represents the effectiveness of our educational intervention to encourage women to have natural childbirth.
Our results are similar to the findings of the study of Khorsandi and colleagues who reported a decrease in delivery fear after intervention in intervention group.[11] Ghaffari also found that the higher self-efficacy mean score of intervention group in comparison with control group is due to the educational intervention effect.[17] In addition, Rahimikian and Fathian reported that the effectiveness of an educational intervention on reducing cesarean rates as well.[18,19] Similarly, Ajh and colleagues found that the cesarean section rate in the intervention group was 16.7% and 60.5% in the control group, which proves the effectiveness of training in reducing caesarean section selection.[20] However, Chularat Howharn indicated that the impact of training on self-efficacy may increase for both intervention and control groups.[21] Moreover, the results of Khani and colleages also showed that 44.8% of intervention group mothers and 46.6% of the control group mothers had cesarean delivery, indicating no effect of the educational intervention on reducing cesarean section.[22]
We found that there is a significant difference between maternal desire for the delivery method at the beginning and the delivery method they chose at the end of study and cesarean delivery rate in the intervention group was less than the control group. This finding is similar to the study of Tofighi and colleagues who reported that 61.8% of mothers chose natural delivery versus cesarean section before training which changed to 80.6% after training and only 57.6% of them were successful in natural delivery at the end.[23] Furthermore, Lashkari reported that 40% of intervention and control group mothers preferred cesarean section and no significant difference was observed between groups.[24]
Our study indicated lower childbirth fear and higher self-efficacy scores in women with natural delivery but the childbirth expectation scores had no significant differences. We also found that mothers who were able to distinguish between the concept of self-efficacy and outcome of labor, a well as having similar thoughts about the benefits of the treatment, would cope with labor pain during childbirth much better than the others, the finding which is similar to the results of Australian and Chinese women.[25,26] Khorsandi and colleagues found no significant difference between nulliparous and multiparous women,[13] a result similar to the findings of intellectual property and Sinclair.[26,27] Dilks and colleagues concluded that women who choose cesarean delivery repeatingly have lower self-efficacy score.[28] Zamani and colleagues reported that self-efficacy mean score in natural delivery group was higher than women who choose the cesarean delivery with a statistically significant difference.[6]
In Katri Nieminen's study, having cesarean section was associated with childbirth fear and mothers who had a cesarean section, had higher levels of fear of childbirth.[29] In another study, Negahban reported that the occurrence rate of emergency cesarean was higher among those who had had higher fear level.[30] Bagheri also showed that the fear of labor is an important factor in encouraging women choosing cesarean section.[31] These results are also consistent with the findings of a Ryding and Jane Drummond's study.[8,25] In a study conducted by Moeni, 74.4% of mothers in the elective cesarean group, 26.7% in cesarean section for medical reasons group and 7.9% in the vaginal delivery group stated that cesarean delivery would certainly be their selection next time.[32] The results of Chong's study indicated that only 2% of the mothers demonstrated that they will recommend cesarean delivery to friends after their childbirth.[33]
One limitation of the present study was that the choice of delivery is not merely a personal matter and other factors, including doctor opinion, hospitals and social conditions and influential people as well as the opinion of husband may affect on the rise of caesarean sections, which are recommended to be considered in future studies. Since each self-efficacy program along with position analysis is more efficient, it is recommended to be considered in future studies. However, due to the low sample size and lack of evaluation of pregnant women living in rural areas, it would be more useful and extensile to study a larger sample size and adding the pregnant women in rural area to the sample.
CONCLUSIONS
As a conclusion, the results of this study confirms the role of self-efficacy as a key element in the choice of childbirth method and natural childbirth fear control and may illustrate the effectiveness of an educational intervention based on self-efficacy in reducing cesarean section in the intervention group after the end of the study. Therefore, the broad educational interventions based on self-efficacy can be effective in encouraging mothers to natural childbirth.
ACKNOWLEDGEMENTS
This article is a dissertation of Master's degree in Health Education, Isfahan University of Medical Sciences. Hereby, the authors express their gratitude to Social Health Determinants Research Center at Shahrekrod University of Medical Sciences, Health Staff of health care centers and all mothers who collaborated with researchers.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Besharati F, Hazavhei SM, Moeini B, Beigi AM. Effect of educational interventions based on theory of planned behavior (TPB) in selecting delivery mode among pregnant women referred to rasht health centers. J Zanjan Univ Med Sci. 2011;19:94–106. [Google Scholar]
- 2.Shakeri M, Mazlomzade S, Mohamadian F. Factors affecting the rate of cesarean section in Zanjan maternity hospitals in 2008. J Zanjan Univ Med Sci. 2012;20:98–104. [Google Scholar]
- 3.Movahed M, Enayat H, Nasab EG, Alborzi S, Mozafari R. Related factors to choose cesarean rather than normal delivery among Shirazian pregnant women. J Fasa Univ Med Sci. 2012;2:278–83. [Google Scholar]
- 4.Ganji F, Raeisi R, Khosravi S, Soltani P, Kasiri K, Jafarzadeh L, et al. Effect of a participatory intervention to reduce the number of unnecessary cesarean sections performed in Shahrekord, Iran. Shahrekord Univ Med Sci. 2006;8:14–8. [Google Scholar]
- 5.Shakerian B. Prevalence and causes of cesarean section in Chahar Mahal and Bakhtiari. Shahrekord Univ Med Sci. 2004;6:69–73. [Google Scholar]
- 6.Zamani-Alavijeh F, Shahry P, Kalhory M, Haghighizadeh MH, Sharifirad GR, Khorsandi M. Identification of factors related to elective cesarean labor: A theory-based study. Sci Res J Shahed Univ. 2012;19:1–11. [Google Scholar]
- 7.Ghooshchian S, Dehghani M, Khorsandi M, Farzad V. The role of fear of pain and related psychological variables in prediction of cesarean labor. Arak Med Univ J. 2011;14:45–54. [Google Scholar]
- 8.Ryding EL, Wijma B, Wijma K, Rydhström H. Fear of childbirth during pregnancy may increase the risk of emergency cesarean section. Acta Obstet Gynecol Scand. 1998;77:542–7. [PubMed] [Google Scholar]
- 9.Zafarghandi M, Hadavand F, Torkestani A, Zaeri F, Variji F. Evaluation of anxiety and fear of labor in postpartum period. J Med Counc Islam Repub Iran. 2005;2:155–60. [Google Scholar]
- 10.Atghaee M, Nouhi E. Imagine the pain of labor and cesarean and vaginal delivery in pregnant women tend to be referred to clinics in Kerman University of Medical Sciences. J Obstet Gynecol Infertil. 2011;14:44–50. [Google Scholar]
- 11.Khorsandi M, Ghofranipour F, Hidarnia A, Faghihzadeh S, Vafaei M, Rousta F, et al. Relaxation effect on reducing fear and vaginal delivery in nulliparous women. J Arak Univ Med Sci. 2008;11:29–36. [Google Scholar]
- 12.Sanavi FS, Navidian A, Rakhshani F, Ansari-Moghaddam A. The effect of education on base the Theory of Planned Behavior toward normal delivery in pregnant women with intention elective cesarean. J Hormozgan Univ Med Sci. 2012;7:531–9. [Google Scholar]
- 13.Khorsandi M, Ghofranipoor F, Heidarneia A, Fagheihzade S, Akbarzadeh A, Vafaeei M. Efficacy of delivery in pregnant women. J Med Counc Islam Repub Iran. 2008;26:89–95. [Google Scholar]
- 14.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 15.Khorsandi M, Asghari Jafarabadi M, Jahani F, Rafiei M. Cultural adaptation and psychometric testing of the short form of Iranian childbirth self efficacy inventory. Iran Red Crescent Med J. 2013;15:e11741. doi: 10.5812/ircmj.11741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cunningham FG, Kenneth LJ, Steven BL, John HC, Dwight R, Catherine SY. Williams Pregnancy and Childbirth. In: Ebrahimi AT, Khalilipour M, translators. 2nd ed. Tehran: Sobhan; 2010. pp. 254–68. [Google Scholar]
- 17.Ghaffari M, Sharifirad GR, Akbari Z, Khorsandi M, Hassanzadeh A. Health belief model-based education and reduction of cesarean among pregnant women: An interventional study. Res Med. 2010;7:200–8. [Google Scholar]
- 18.Rahimikian F, Mirmohammadaliee M, Mehran A, Abozari K, Salmani N. The impact of education on health belief model based on the chosen method of delivery. J Nurs Midwifery Tehran Univ Med Sci (HAYAT) 2009;14:25–32. [Google Scholar]
- 19.Fathian Z, Sharifi Rad G, Hasanzadeh A, Fathian Z. Study of the effects of behavioral intention Model education on reducing the cesarean rate among pregnant women of Khomeiny-Shahr, Isfahan, in 2006. Tabibe Shargh. 2006;9:123–31. [Google Scholar]
- 20.Ajh N, Sabet ghadam S, Unesyan M. The effect of health education on the rate of cesarean section. J Ghazvin Univ Med Sci. 2011;14:71–6. [Google Scholar]
- 21.Chularat Howharn. Effects of childbirth preparation classes on self-efficacy in coping with labor pain in Thai primiparas. Univ Tex Austin Sch Nurs. 2001;15:179–94. [Google Scholar]
- 22.Khani S, Shaabankhani B. Is it possible to reduce cesarean section rates in Mazandaran. J Mazandaran Univ Med Sci. 2004;14:43–50. [Google Scholar]
- 23.Niaki MT, Behmanesh F, Mashmuli F, Azimi H. The effect of prenatal group education on knowledge, attitude and selection of delivery type in primiparous women. Iran J Med Educ. 2010;10:124–9. [Google Scholar]
- 24.Lashgari MH, Delavari S, Moghaddam NM, Gorouhi F. Effects of training programs of pregnant women on their delivery type selection: A single blind, randomized control trial. J Mil Med Sci Iran. 2006;3:679–84. [Google Scholar]
- 25.Drummond J, Rickwood D. Childbirth confidence: Validating the Childbirth Self-Efficacy Inventory (CBSEI) in an Australian sample. J Adv Nurs. 1997;26:613–22. doi: 10.1046/j.1365-2648.1997.t01-24-00999.x. [DOI] [PubMed] [Google Scholar]
- 26.Ip WY, Chan D, Chien WT. Chinese version of the childbirth self-efficacy inventory. J Adv Nurs. 2004;51:625–33. doi: 10.1111/j.1365-2648.2005.03548.x. [DOI] [PubMed] [Google Scholar]
- 27.Sinclair M, O’Boyle C. The Childbirth Self-Efficacy Inventory: A replication study. J Adv Nurs. 1999;30:1416–23. doi: 10.1046/j.1365-2648.1999.01230.x. [DOI] [PubMed] [Google Scholar]
- 28.Dilks FM, Beal JA. Role of self-efficacy in birth choice. J Perinat Neonatal Nurs. 1997;11:1–9. doi: 10.1097/00005237-199706000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Nieminen K, Stephansson O, Ryding EL. Women's fear of childbirth and preference for cesarean section – A cross-sectional study at various stages of pregnancy in Sweden. Acta Obstet Gynecol Scand. 2009;88:807–13. doi: 10.1080/00016340902998436. [DOI] [PubMed] [Google Scholar]
- 30.Negahban T, Ansari A. Do not be afraid of emergency cesarean delivery in nulliparous pregnant women can predict? J Nurs Midwifery Tehran Univ Med Sci (HAYAT) 2008;14:73–81. [Google Scholar]
- 31.Aazam B, Negin AM, Fateme A. Effective factors for choosing the delivery method among the pregnant women in Kashan. J Kashan Univ Med Sci. 2012;16:146–53. [Google Scholar]
- 32.Moeini B, Besharati F, Hazavei MM, Moghimbeigi A. Women's attitudes toward elective delivery mode based on the theory of planned behavior. J Guilan Univ Med Sci. 2011;20:68–76. [Google Scholar]
- 33.Chong ES, Mongelli M. Attitudes of Singapore women toward cesarean and vaginal deliveries. Int J Gynaecol Obstet. 2003;80:189–94. doi: 10.1016/s0020-7292(02)00391-0. [DOI] [PubMed] [Google Scholar]


