Abstract
This study examined whether executive function and theory of mind mediate the effects of pediatric traumatic brain injury (TBI) on social adjustment, relative to children with orthopedic injury (OI). Participants included 19 children with severe TBI, 41 children with complicated mild/moderate TBI, and 57 children with OI. They completed measures of executive function, as well as cognitive, affective, and conative theory of mind. Parents provided ratings of children's social adjustment. Children with severe TBI performed more poorly than children with OI on executive function and theory of mind tasks and were rated by parents as having more behavioral symptoms and worse communication and social skills. Executive function and theory of mind were positively correlated with social skills and communication skills, and negatively correlated with behavioral symptoms. In multiple mediator models, theory of mind and executive function were not significant direct predictors of any measure of social adjustment, but mediated the association between injury and adjustment for children with severe TBI. Theory of mind was a significant independent mediator when predicting social skills, but executive function was not. TBI in children, particularly severe injury, is associated with poor social adjustment. The impact of TBI on children's social adjustment is likely mediated by its effects on executive function and theory of mind.
Key words: : executive function, pediatric, social adjustment, traumatic brain injury
Introduction
Traumatic brain injury (TBI) is a common childhood brain disorder that is associated with poor social adjustment, as reflected in the judgments of both peers and adults.1 Social adjustment “reflects the extent to which children attain socially desirable and developmentally appropriate goals. [It] encompasses the quality of children's relationships as perceived by others but also includes self-perceptions of loneliness, social support, or social self-esteem” (p. 358).1
Childhood TBI is also linked to deficits in social information processing (SIP) across domains that include executive function,2 theory of mind,3 and social problem-solving.4 For example, children with TBI exhibit problems making inferences about the mental states of others and show impairments on traditional theory of mind tasks.3 Theory of mind is closely linked with executive functions such as working memory and inhibitory control, especially early in childhood.5 Disruption of the normal development of SIP as a result of TBI may place children at risk for social isolation, difficulties with peer and family relationships, and decreased quality of life.6
Although previous research has documented specific deficits in executive function, SIP, and social adjustment after TBI, few studies have addressed the associations among these domains. Dennis and colleagues7 concluded that early-onset TBI is associated with deficits in multiple regulatory and adaptive skills (i.e., vigilance, selective attention, response manipulation), but did not examine how these predictors interact in accounting for social adjustment.7 Caregiver ratings of executive functions in the daily environment, including self-regulatory and metacognitive skills, have been linked with impairments in school and community-based behavioral functioning.8 These associations remained even after controlling for performance-based measures of cognitive functioning (e.g., processing speed and memory). These findings supported the utility of measures of executive function in predicting functional outcomes.
Other studies have suggested that specific neurocognitive skills, including executive functions, and social problem-solving skills account for significant variance in long-term social adjustment after childhood TBI, over and above demographic and injury-related factors.9 Theory-driven research that clarifies the relation among domains of social competence in TBI is clearly needed to better understand the long-term social problems faced by children with TBI and to design interventions to promote their social competence.
A recent theoretical model of social competence within the context of childhood brain disorder takes a multilevel approach to social competence that distinguishes between SIP, social interaction, and social adjustment (see Supplementary Appendix A for a schematic of the theoretical model; see online supplementary material at ftp.liebertpub.com).1 The model proposes that SIP involves both social-affective and cognitive-executive processes that are broadly subsumed by the social brain network and that contribute to social interaction and adjustment. The model has received support from our recent study of social outcomes in children with TBI, which has documented deficits in theory of mind10 and classroom peer relationships11 that are related to one another and to broader aspects of social adjustment.12 We have not yet examined, however, the collective and individual contributions of social-affective (i.e., cognitive, affective, and conative theory of mind) and cognitive-executive (i.e., inhibitory control, working memory, cognitive flexibility) functions to social adjustment.
The current article, therefore, examines the relationship of executive function and theory of mind with respect to social adjustment in children with complicated mild to severe TBI and children with orthopedic injuries (OI). The study relied on data collected as part of our larger project.12 The larger project, which was cross-sectional in design, compared the social outcomes of 8- to 13-year-old children with complicated mild to severe TBI with those of children with OI. Participants completed an assessment on average 2.5 years post-injury that included direct measures of executive functions and theory of mind and parent ratings of social adjustment.
Previous articles from this study showed that children with TBI display significant deficits in theory of mind10 and social adjustment11,12 relative to children with OI, and that group differences were most pronounced for children with a history of severe TBI. The present analyses contribute to the existing literature by testing a portion of the theoretical model proposed by Yeates and colleagues.1 Specifically, we examined the individual and collective contributions of executive function and theory of mind as predictors of social adjustment. We predicted that executive function and theory of mind would both individually and collectively predict social adjustment, across both groups of children, and act as significant mediators of the effects of TBI on social adjustment.
Methods
Participants and procedures
Participants included children and adolescents who had been hospitalized for either a TBI or OI at least 12 months, but no greater than 63 months, before study participation. Participants were at least 3 years of age at the time of the injury, and the vast majority of children were at least 4 years of age. Children were 8 to 13 years old at the time of participation. The TBI group was restricted to children with complicated mild to severe TBI. Severe TBI was classified based on a lowest post-resuscitation Glasgow Coma Scale (GCS) score of 8 or less, and moderate TBI was classified based on a GCS score from 9 to 12. Complicated mild TBI was classified based on a GCS score of 13 to 15 in association with trauma-related abnormalities on neuroimaging at the time of hospitalization; children with GCS scores of 13 to 15 without neuroimaging abnormalities were not eligible.
The OI group consisted of children who sustained fractures without loss of consciousness or other indications of brain injury (e.g., facial fracture). For the current study, children were grouped into those with severe TBI (STBI), those with complicated mild to moderate TBI (MTBI), and those with OI.
The following exclusion criteria were applied to all participants: (a) history of more than one injury necessitating hospitalization; (b) premorbid neurological disorder or mental retardation; (c) injury from child abuse or assault; (d) history of severe psychiatric disorder necessitating hospitalization before the injury; (e) sensory or motor impairment that prevented valid administration of the measures included in the study; (f) primary language other than English; (g) full-time placement in a special education classroom; and (h) medical contraindication to magnetic resonance imaging.
Participants were recruited at children's hospitals at three metropolitan sites: Toronto, Canada, Columbus, Ohio, and Cleveland, Ohio. All procedures were approved by the Institutional Review Boards at participating institutions. Children and their parents were invited to participate only after parents gave informed consent. The study used a cross-sectional design with two study visits. Some parent ratings of social adjustment were initially obtained at the second study visit, but they were subsequently elicited during the first visit to reduce missing data.
Of those eligible for recruitment and approached about the study, 82 (47%) of those with TBI and 61 (26%) of those with OI agreed to enroll. Despite significant differences in participation rate between groups, participants and nonparticipants did not differ in terms of age at injury or age at study contact, sex, race, or socioeconomic status (SES) based on census tract median family income. Among children with TBI, participants and nonparticipants did not differ on measures of injury severity.
Inclusion in the current article was limited to participants for whom at least one measure of social adjustment (i.e., Adaptive Behavior Assessment System-Second Edition [ABAS-II] or Behavior Assessment System for Children-Second Edition [BASC-2]; see below) was available. Of the 143 participants in the overall study, 19 children with STBI, 41 children with MTBI, and 57 children with OI met this requirement, for a total sample of 117 (81.8% of the total sample). No differences were found between those included versus those excluded from analyses in terms of age at injury or age at study participation, sex, SES (measured using a standardized composite based on parental education, parent occupational status, and census tract median family income), mechanism of injury, maternal education, or maternal marital status.
Children with TBI were more likely to be excluded than children with OI (24.4% vs. 6.6%). This is partly because children with TBI were recruited earlier than those with OI, when measures of social adjustment were collected at the second study visit rather than the first, and also because children with TBI had more difficulty arranging for a friend to accompany them to the second visit. Race was also related to exclusion, with white children less likely to be excluded than black children or children from a multiracial background (11.9% vs. 41.7% and 57.1%, respectively).
Demographic characteristics of the three groups are presented in Table 1. The groups did not differ in terms of sex, race, age at injury, or age at study participation. The groups differed significantly in terms of SES. The groups also differed in distribution of mechanism of injury, with motor vehicle accidents being most common among the children with STBI and sports/recreational injuries being most common among children with OI. Group differences in SES were not significant when injury mechanism was taken into account, consistent with epidemiological studies showing that the risk of TBI, particularly those linked to motor vehicles, is highest for children of lower SES and minority status.13–15 For that reason, we did not treat SES as a covariate in data analyses, because the SES differences appeared to be intrinsic to the injury groups.16
Table 1.
Group Demographics and Injury Characteristics*
| STBI (n=19) | MTBI (n=41) | OI (n=57) | F/X2 | p | η2/V | |
|---|---|---|---|---|---|---|
| Child age at testing | 10.12 (1.54) | 10.75 (1.47) | 10.64 (1.69) | 1.05 | 0.35 | 0.02 |
| Child age at injury | 7.46 (2.19) | 8.29 (1.91) | 7.79 (1.80) | 1.45 | 0.24 | 0.03 |
| Child sex | 11 boys (58%) | 26 boys (63%) | 34 boys (60%) | 0.22 | 0.90 | 0.04 |
| Child race | 88% White | 93% white | 91% white | 1.80 | 0.77 | 0.09 |
| SESa | −0.66 (0.51) | −0.08 (0.90) | 0.29 (0.99) | 8.37 | <0.01 | 0.13 |
| Injury mechanism | 29.67 | <0.01 | 0.36 | |||
| MVA | 52.6% | 26.8% | 1.8% | |||
| Sports/Rec | 26.3% | 41.5% | 71.9% | |||
| Fall | 21.1% | 31.7% | 26.3% |
Measured using a standardized composite based on parental education, parent occupational status, and census tract median family income
Values in parentheses indicate standard deviation.
STBI, severe traumatic brain injury; MTBI, mild to moderate traumatic brain injury; OI, orthopedic injury; SES, socioeconomic status; MVA, motor vehicle accident.
Measures
Executive functions
Executive functions were assessed using two Processing Speed Index subtests (i.e., Cancellation, Symbol Search) from the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV), and selected subtests from the Test of Everyday Attention for Children (TEA-Ch).17,18 The WISC-IV Processing Speed Index provided a measure of response speed and focused attention that is known to be sensitive to childhood TBI.19 Three subtests of the TEA-Ch were administered. The Walk/Don't Walk subtest was used to assess inhibitory control, and requires a child to mark footprints on a path for a “go” tone and inhibit marking for a “stop” tone. The Code Transmission subtest assesses working memory and requires a child to listen to a series of single-digit numbers and recall the digit presented immediately before two consecutive 5s. The Creature Counting subtest was administered to assess cognitive flexibility and requires a child to count creatures with one-to-one correspondence, but to use up and down arrows as cues to count forward or backward. The TEA-Ch has been shown to be sensitive to childhood TBI.20,21
Theory of mind
Children were administered three measures assessing different aspects of theory of mind.10 The first measure assessed cognitive theory of mind, which is the original mindreading sense of theory of mind, as reflected in understanding of false beliefs. In the Jack and Jill task, children were shown sequences of three cartoon frames on a computer screen.22 Each frame included a character (Jack and/or Jill), two hats (red and blue), and a ball. Frame A of the sequence showed Jack placing the ball in a hat, an event witnessed by Jill. In Frame B, Jack either dropped the ball further down into the hat, or switched the ball to the second hat. This event was sometimes witnessed, and sometimes not witnessed, by Jill. Frame C showed Jill “thinking” about either the red or blue hat. Children responded “yes” if Frame C represented what was now in Jill's mind about the ball's location, and they responded “no” if it did not. The task measured cognitive theory of mind by presenting switched, unwitnessed trials that measured false belief, as compared with a series of switched, witnessed trials that measured true belief. The percent accuracy for switched, unwitnessed trials was the primary measure of cognitive theory of mind.
The Emotional and Emotive Faces Task (EFFT) was used to assess affective theory of mind, or the child's understanding of the distinction between felt versus displayed emotion.23 It evaluated children's appreciation of the distinction between emotional expression (how a character actually feels) and emotive communication (the emotion a character expresses socially, which may be different from the felt emotion). Children listened to short narratives that described a character in situations that were meant to evoke one of five basic emotions: happiness, sadness, fear, disgust, and anger. In each situation, a discrepancy existed between the emotion felt “inside” and the character's facial expression. Children were asked in all trials how the character felt inside and how the character looked on his/her face. The percent accuracy for emotive communication trials (i.e., “on his/her face”) was the primary measure of affective theory of mind.
The Ironic Criticism and Empathic Praise task was used to assess conative theory of mind, which refers to forms of social communication in which we try to influence the mental and emotional state of others.24 In this task, children were presented with six pictured situations involving two children, one of whom was engaged in an activity and another who commented on their performance of the activity. The pictures were accompanied by a narrative and an audiotape of the speaker's utterances with neutral, ironic, or empathic intonation. Children were told the goal of the child engaged in the activity (e.g., to build a tower), the outcome (e.g., “the tower was…”), the speaker's character (e.g., “she liked to cheer people up”), and what the speaker said (e.g., “You made a great tower”). Children were asked two factual questions, two belief questions, and two intent questions. The percent accuracy for indirect speech acts, which reflected the understanding of belief and intent for empathic praise and ironic criticism conditions, was the primary measure of conative theory of mind.
Social adjustment
Parents rated their child's emotional and behavioral adjustment using the BASC-2.25 The BASC-2 assesses both adaptive and problem behaviors, which are rated on a four-point scale from “never” to “almost always.” For the present study, the BASC-2 Social Skills subscale and the overall Behavioral Symptom Index were used as measures of social adjustment.
Parents also rated their child's social functioning using the ABAS-II.26 The ABAS-II is a parent report measure of behavioral skills that are important in coping with the demands of daily life across multiple settings (e.g., home, school, community). The measure is normed for young children through adults and consists of ratings of behaviors on a scale from “is not able” to perform a given action to performs the action “always or almost always when needed.” For the purposes of the current study, social adjustment was assessed using the Social, Self-Direction, and Communication subscales, which are those that most directly assess social functioning.
Data reduction and analysis
Pooled within-group correlations were computed to examine the associations among the measures of executive function and theory of mind (Table 2). In general, the measures of executive function were significantly correlated with one another, as were the measures of theory of mind. Exploratory factor analysis was also largely consistent with these groupings. Therefore, individual scores on subtests comprising each domain were transformed to the same metric (i.e., % correct for theory of mind tasks; standard scores for executive function tasks), and composite scores were generated for each participant by averaging performance across tasks within domains. This yielded overall indicators of executive function and theory of mind for use in subsequent analyses.
Table 2.
Pooled within-group Correlations among Individual Measures of Executive Function and Theory of Mind
| Measure | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
|---|---|---|---|---|---|---|---|
| Executive Function: | |||||||
| 1. WISC-IV PSI | - | ||||||
| 2. TEA-Ch Walk Don't Walk | 0.36* | - | |||||
| 3. TEA-Ch Code Transmission | 0.15 | 0.42* | - | ||||
| 4. TEA-Ch Creature Counting | 0.27* | 0.22** | 0.35* | - | |||
| Theory of Mind: | |||||||
| 5. Jack and Jill | 0.28* | 0.38* | 0.16 | 0.10 | - | ||
| 6. Faces | 0.17 | 0.25* | 0.08 | 0.09 | 0.40* | - | |
| 7. Irony and empathy | 0.15 | 0.20** | -0.02 | 0.09 | 0.35* | 0.22** | - |
p<0.01; **p<0.05.
WISC-IV PSI, Wechsler Intelligence Scale for Children, Fourth Edition, Processing Speed Index; TEA-Ch, Test of Everyday Attention for Children.
One-way analyses of variance and planned contrasts were used to examine whether groups differed on executive function and theory of mind, as well as on measures of social adjustment. We then examined multiple mediator models using ordinary least squares path analysis to determine the relative contributions to social adjustment accounted for by group, executive function, and theory of mind.27 This analytic strategy was selected because it allows for the simultaneous inclusion of multiple mediators, but reports individual effects for each mediator while controlling for others. Further, this approach allows for the inclusion of covariates, as well as the use of categorical predictors.
The procedure yields unstandardized path coefficients (betas) for each individual path of the model. Unstandardized path coefficients are scaled according to the measurement of variables included in each path of the model and are preferable over standardized coefficients in this type of modeling, particularly when independent variables are categorical.28 The procedure yields tests of direct, indirect, and total effects (i.e., combined direct and indirect effects) within each model. Indirect effects are examined using 95% bias-corrected confidence intervals based on 10,000 bootstrap samples; if the intervals for a specific effect do not contain zero, the effect is considered significant.
We computed models for each measure of social adjustment. In each model, group was first entered as an independent variable, coded as two dichotomous dummy variables (STBI vs. OI; MTBI vs. OI), and the executive function and theory of mind composites were entered simultaneously as mediators of the group effects on social adjustment. Age at testing was added as a covariate in each model given the significant correlation between age at testing and the theory of mind composite (r=0.59, p<0.001). In the presentation of results, the direct effects of each included variable are presented in Figures 1 a–e. Indirect effects of group on adjustment via the proposed mediators (i.e., theory of mind and executive function) are presented in Table 5, below. Finally, the total effects of each overall model are summarized in the text.
FIG. 1.
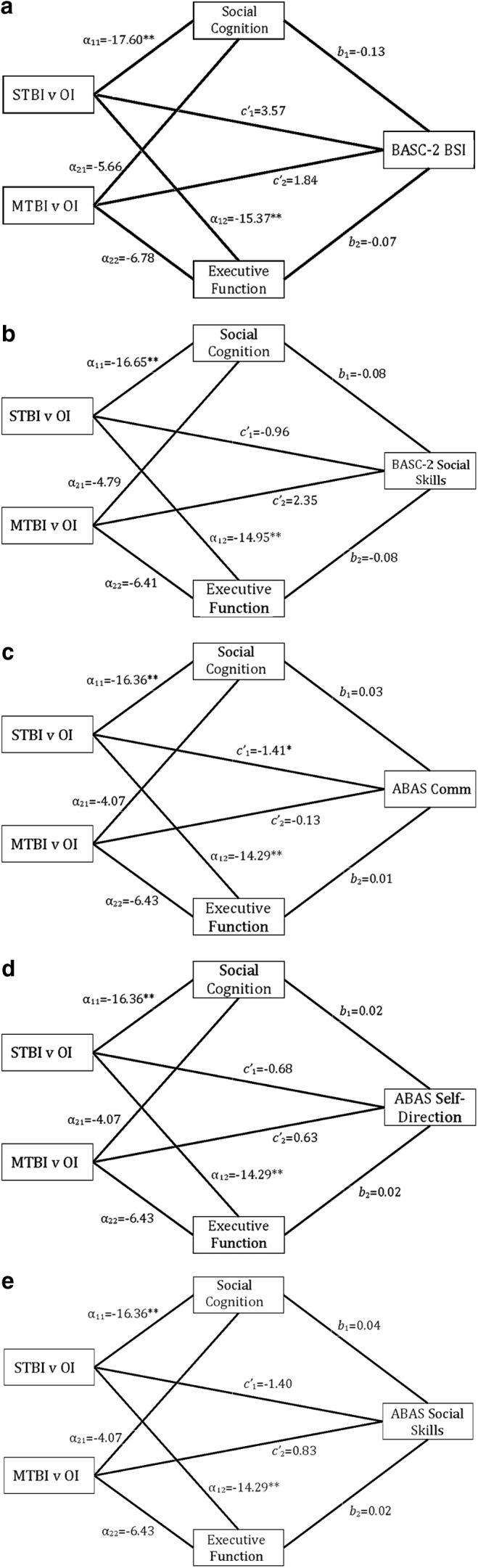
Direct effect pathways of group and mediator variables. a=direct effect of group on proposed mediators; b=direct effect of mediator variables on social adjustment outcome; c′=direct effect of group on social adjustment outcome. *p<.05; **p<.01.
Table 5.
Model Summary Information: Indirect Effects of Group on Outcome
| Indirect Effects | |||
|---|---|---|---|
| Effect | Lower CI | Upper CI | |
| BASC-2 BSI | |||
| STBI | |||
| Total Model* | 3.42 | 0.60 | 7.72 |
| Social Cognition | 2.37 | −0.07 | 5.92 |
| Executive Function | 1.05 | −0.74 | 4.04 |
| MTBI | |||
| Total Model | 1.22 | −0.09 | 4.13 |
| Social Cognition | 0.76 | −0.06 | 2.95 |
| Executive Function | 0.46 | −0.27 | 2.21 |
| BASC-2 Social Skills | |||
| STBI | |||
| Total Model | −2.44 | −5.82 | 0.02 |
| Social Cognition | −1.27 | −4.17 | 0.96 |
| Executive Function | −1.17 | −4.21 | 0.35 |
| MTBI | |||
| Total Model | −0.87 | −3.13 | 0.12 |
| Social Cognition | −0.37 | −2.11 | 0.22 |
| Executive Function | −0.50 | −2.11 | 0.16 |
| ABAS-II Social Skills | |||
| STBI | |||
| Total Model* | −0.92 | −1.88 | −0.21 |
| Social Cognition* | −0.68 | −1.59 | −0.02 |
| Executive Function | −0.24 | −1.05 | 0.16 |
| MTBI | |||
| Total Model | −0.28 | −0.94 | 0.04 |
| Social Cognition | −0.17 | −0.69 | 0.04 |
| Executive Function | −0.11 | −0.58 | 0.07 |
| ABAS-II Self-Direction | |||
| STBI | |||
| Total Model | −0.62 | −1.60 | 0.05 |
| Social Cognition | −0.33 | −1.24 | 0.33 |
| Executive Function | −0.29 | −1.18 | 0.23 |
| MTBI | |||
| Total Model | −0.21 | −0.86 | 0.05 |
| Social Cognition | −0.08 | −0.56 | 0.06 |
| Executive Function | −0.13 | −0.65 | 0.08 |
| ABAS-II Communication | |||
| STBI | |||
| Total Model* | −0.53 | −1.12 | −0.05 |
| Social Cognition* | −0.46 | −1.12 | −0.02 |
| Executive Function | −0.07 | −0.57 | 0.28 |
| MTBI | |||
| Total Model | −0.15 | −0.53 | 0.05 |
| Social Cognition | −0.11 | −0.48 | 0.02 |
| Executive Function | −0.03 | −0.29 | 0.12 |
CI, confidence interval; BASC-2, Behavior Assessment System for Children, Second Edition; BSI, Behavioral Symptom Index; STBI, severe traumatic brain injury, contrast term representing effect of severe TBI versus complicated mild/moderate TBI (MTBI) or orthopedic injury; MTBI, contrast term representing effects of complicated MTBI versus STBI or orthopedic injury; ABAS-II, Adaptive Behavior Assessment System-Second Edition.
significant indirect effect.
Results
Group differences
Group means and standard deviations for the theory of mind and executive function composites and for the measures of social adjustment are presented in Table 3. Groups differed significantly on the executive function and theory of mind composites. Planned contrasts indicated that the STBI group performed significantly more poorly than the OI group on both composites, t(114)=−2.89, p=0.005, d=0.74, and t(114)=−4.18, p<0.001, d=1.10, but no differences were found between the MTBI and OI groups, t(114)=−1.53, p=0.128, d=0.32, and t(114)=−0.92, p=0.362, d=0.19.
Table 3.
Group Means and Standard Deviations on Executive Function, Theory of Mind, and Social Adjustment
| Severe TBI (n=19) | Mild/Mod TBI (n=41) | OI (n=57) | ||||
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | F (116) | p | η2 | |
| Executive Function | 77.99 (21.29) | 86.94 (19.67) | 93.18 (19.54) | 4.37 | 0.02 | 0.07 |
| Theory of Mind | 45.29 (18.66) | 61.77 (18.51) | 65.13 (17.27) | 8.83 | <0.01 | 0.13 |
| Social Adjustment | ||||||
| BASC-2 Social Skills | 47.84 (12.93) | 52.73 (11.42) | 51.24 (9.81) | 1.28 | 0.28 | 0.02 |
| BASC-2 BSI | 55.42 (14.83) | 51.53 (12.85) | 48.46 (8.14) | 2.79 | 0.07 | 0.05 |
| ABAS-II Communication | 9.37 (3.20) | 11.00 (2.27) | 11.28 (2.27) | 4.47 | 0.01 | 0.07 |
| ABAS-II Social Skills | 7.68 (4.31) | 10.49 (3.04) | 9.95 (3.06) | 4.90 | <0.01 | 0.08 |
| ABAS-II Self-Direction | 8.11 (4.05) | 9.93 (3.09) | 9.49 (3.22) | 1.97 | 0.14 | 0.03 |
TBI, traumatic brain injury; OI, orthopedic injury; M, mean; SD, standard deviation; BSI, Behavioral Symptom Index; BASC-2, Behavior Assessment System for Children-Second Edition; ABAS-II, Adaptive Behavior Assessment System-Second Edition. Executive Function is presented as a standard score, with a normative mean of 100 and a standard deviation of 15, averaged across four measures of executive function. Theory of Mind is presented as percent correct, averaged across three measures of theory of mind. BASC-2 subscales are presented as T scores, with a normative mean of 50 and standard deviation of 10; higher scores on the BSI, and lower scores on the Social Skills scale, indicate more problematic functioning. ABAS subscales are presented as scaled scores, with a normative mean of 10 and standard deviation of 3; lower scores indicate more problematic functioning.
The groups did not differ in ratings of self-direction on the ABAS-II or social skills on the BASC-2. The groups differed marginally on the BASC-2 Behavioral Symptom Index; planned contrasts indicated that the STBI group were reported by parents to display more behavioral symptoms than the OI group, t(108)=2.30, p=0.023, d=0.58, but no difference was found between the MTBI and OI groups, t(108)=1.29, p=0.200, d=0.29. The groups also differed significantly in communication and social skills as rated on the ABAS-II. On each outcome measure, the STBI group members were rated worse than the OI group members, t(114)=−2.96, p=0.004, d=0.69 and t(114)=−2.60, p=0.011, d=0.61, but no significant differences were found between the MTBI and OI groups, t(114)=−0.56, p=0.575, d=0.12, and t(114)=0.80, p=0.423, d=0.18.
Prediction of social adjustment
As Table 4 shows, the executive function composite was significantly and positively correlated with the theory of mind composite. The executive function composite also showed a significant positive correlation with parent-reported social skills and a significant negative correlation with overall behavioral symptoms. The theory of mind composite, covarying for age at testing, showed a significant positive correlation with parent reported social skills and communication, and a significant negative correlation with overall behavioral symptoms.
Table 4.
Pooled Within-Group Correlations among Executive Function, Theory of Mind, and Social Adjustment
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
| 1. Executive Function | - | |||||
| 2. Theory of Mind | 0.41* | - | ||||
| 3. BASC-2 Social Skills | 0.18** | 0.19** | - | |||
| 4. BASC-2 BSI | −0.19** | −0.29* | −0.59* | - | ||
| 5. ABAS-II Communication | 0.13 | 0.29* | 0.66* | −0.59* | - | |
| 6. ABAS-II Social Skills | 0.17 | 0.28* | 0.70* | −0.66* | 0.70* | - |
| 7. ABAS-II Self-Direction | 0.18 | 0.18 | 0.59* | −0.64* | 0.57* | 0.68* |
p<0.01; **p<0.05.
BASC-2, Behavior Assessment System for Children, Second Edition; ABAS-II, Adaptive Behavior Assessment System-Second Edition.
The results from the multiple mediator models are presented in Figures 1 a–e and Table 5. In each model, the dummy variable representing the STBI versus OI group contrast was significant, indicating that the STBI group performed significantly worse than the OI group on the theory of mind and executive function composites; in contrast, the dummy variable representing the MTBI versus OI group contrast was not significant in any model, indicating that the MTBI group did not differ from the OI group on either composite. In predicting adjustment, the STBI group showed a significant direct effect when predicting the ABAS-II Communication and Social Skills subscales and the BASC-2 Behavioral Symptom Index. STBI did not directly predict ABAS-II Self-Direction or BASC-2 Social Skills, and MTBI did not directly predict any outcome measure. These results are consistent with the group comparisons presented above.
The theory of mind and executive function composites were not significant direct predictors of any measure of social adjustment. Analyses of the BASC-2 Behavioral Symptom Index and ABAS-II Communication and Social Skills scales, however, provided evidence for mediation of the effects of severe TBI. For the BASC-2 Behavioral Symptom Index, the test of the overall indirect effect of group on outcome, when mediators were included in the model, was significant for the STBI group, c=6.98, t=2.28, p=0.02, but not for the MTBI group, c=3.06, t=1.28, p=0.20 (Fig. 1a). Neither theory of mind nor executive function emerged as a significant mediator independently of the other.
For the ABAS-II Communication scale, the test of the overall indirect effect was significant for the STBI group, c=−1.94, t=−2.96, p<0.01, but not for the MTBI group, c=−0.28, t=−0.55, p=0.58 (Fig. 1c). Theory of mind was a significant independent mediator, but executive function was not. A similar result was obtained for the ABAS-II Social Skills scale. That is, the overall indirect effect was significant for the STBI group, c=−2.32, t=−2.65, p<0.01, but not for the MTBI group, c=0.55, t=0.82, p=0.41 (Fig. 1e). Theory of mind was again a significant independent mediator, but executive function was not.
The models predicting the BASC-2 Social Skills, STBI: c=−3.40, t=−1.15, p=0.25; MTBI: c=1.49, t=0.65, p=0.52 (Fig. 1b) and ABAS-II Self-Direction scales, STBI: c=−1.30, t=−1.46, p=0.14; MTBI: c=0.42, t=0.61, p=0.54 (Fig. 1d) did not provide evidence of mediation of the effects of TBI on social adjustment by theory of mind or executive function.
Discussion
TBI in childhood is associated with deficits in executive function and SIP, as well as with a range of problematic psychosocial outcomes. In this study, as expected, children with STBI performed significantly more poorly than children with OI on composite measures of executive function and theory of mind. This is consistent with previous analyses from the full sample from this study using individual measures of theory of mind,10 as well as research clearly documenting that children with TBI, especially those with more severe injuries, are at risk for such deficits.6
Children with STBI also demonstrated deficits on several parent-rated measures of social adjustment. Children with STBI were reported to have significant overall behavioral symptoms on the BASC-2, as well as problematic social skills and communication on the ABAS-II. Although no significant differences were found on other indicators of adjustment, each group comparison was in the same direction, with small to medium effect sizes. Rates of impairment (i.e., greater than one standard deviation from the normative mean) exceeded 20% on each outcome measure for the STBI group, and surpassed 60% on the Social Skills scale of the ABAS-II. These results indicate the importance of social adjustment in children after TBI and the need to be able to identify which children are at greatest risk for these difficulties.
Correlations among executive function, theory of mind, and psychosocial adjustment were in predicted directions. Generally, children who performed more poorly on measures of executive functioning also performed less accurately on theory of mind tasks. This is not surprising, as theory of mind tasks necessitate basic cognitive and executive skills (e.g., working memory).29–31 Further, both sets of skills are thought to rely on similar neuroanatomical substrates. Neuroimaging studies indicate that the “social brain network” and regions underlying core executive functions overlap substantially.32–35 In turn, better executive function and theory of mind were associated with better social adjustment. The extent to which skills in each specific domain might be useful in predicting psychosocial adjustment in children with TBI, however, had until now remained largely untested. Accordingly, we examined the relative predictive value of executive functioning versus theory of mind toward adaptive and behavioral outcomes.
Multiple mediator model analyses indicated that, despite significant group differences, the direct effects of STBI on adjustment became nonsignificant after including theory of mind and executive function as mediators in the models. These findings indicate that executive function and theory of mind are likely to play a significant role in the emergence of psychosocial difficulties in children after STBI. Some previous research has demonstrated a shared or overlapping impact of executive function and theory of mind on social outcomes, whereas other studies suggest that aspects of neuropsychological functioning may impact social outcomes both directly and via the impact of TBI on SIP and social problem solving.9,36,37
In the current study, theory of mind was an independent mediator of social adjustment, while executive function was not. Thus, our findings suggest that theory of mind may uniquely mediate the effect of severe TBI on social functioning. This may be because of the more direct link between deficits in theory of mind and children's ability to engage in social interactions and maintain peer relationships.
Notably, evidence of mediation was found when predicting social skills on the ABAS-II, but not on the BASC-2. The ABAS-II social scale, however, may be a better indicator of social functioning than the social skills subscale on the BASC-2 because the latter places more emphasis on social problems than on social adaptation. The mediation models also indicated that neither theory of mind nor executive function accounted for the association between group and self-direction on the ABAS-II. The specific items on the latter subscale largely assess a child's ability to function independently, and only a few items are specifically social in nature. This ability may be less dependent on theory of mind and executive function than the other aspects of adjustment measured here.
Although some research has recommended that mediator models be tested only in instances where independent, dependent, and mediating variables are mutually associated,38 an emerging statistical literature has leveled a variety of criticisms at this approach.39 Namely, the traditional approach disregards the possibility that an indirect, intervening effect on a dependent variable may indeed exist, although a direct association between independent and dependent variables does not. In the context of the current study, this implies that group may not significantly predict adjustment, and the mediators may not directly predict adjustment, yet mediation can still exist.
The study has several strengths that highlight its unique contribution to this area of research. First, the study relied on multiple, independent methods for measurement of executive function, theory of mind, and social adjustment. This makes the results more robust given that the findings are not likely to be magnified by shared source variance. In addition, the combination of several correlated indicators of executive function and theory of mind into composites increases confidence that the mediators used in the mediation models encompass a variety of aspects of the constructs they purport to measure.
Several limitations of the study also require acknowledgment. First, the small size of the STBI group limited statistical power in subgroup analyses, and the cross-sectional design of the study precluded an examination of the temporal emergence of deficits in executive function and theory of mind and their relationship to adjustment. Demographically, nonwhite children were more likely to be excluded from analyses because of missing data, reducing the diversity of the sample. Our assessment of executive function relied on four TEA-Ch subtests and was not exhaustive of all facets of executive function, but is reflective only of the measures chosen. The tasks may also reflect variability in language abilities in addition to executive function.
Although we used multiple methods of assessments across model components, adjustment was assessed based solely on parent report. The measures are norm-referenced and have been well validated, but they provide an indirect and potentially biased indicator of social functioning. Moreover, parent ratings in general may not be especially sensitive to the effects of TBI40 and may differ substantially from ratings provided by others (e.g., teachers, children).41 The use of ecologically valid measures of social functioning (e.g., observations of peer interactions) and/or multiple reporters would be a useful extension of the current study.
Conclusion
The current study provides evidence that TBI affects social adjustment at least in part via its impact on theory of mind and executive function. The findings provide direction for further research in this area. Specifically, further research should incorporate a variety of measures of social adjustment that extend beyond parent report. Longitudinal studies would help to clarify the causal relationships among executive function, theory of mind, and social adjustment, and thereby better inform the development of interventions aimed at ameliorating the effects of TBI on social outcomes. Overall, the findings point to significant associations among theory of mind, executive function, and social adjustment after TBI, and highlight the importance of attending to these areas of functioning in this vulnerable population.
Supplementary Material
Acknowledgment
The preparation of this article was supported in part by grant 5 R01 HD048946 from the National Institute of Child Health and Human Development to Keith Yeates.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Yeates K.O., Bigler E.D., Dennis M., Gerhardt C.A., Rubin K.H., Stancin T., Taylor H.G., and Vannatta K. (2007). Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychol. Bull. 133, 535–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Crowe L.M., Catroppa C., Babl F.E., and Anderson V. (2013). Executive function outcomes of children with traumatic brain injury sustained before three years. Child Neuropsychol. 19, 113–126 [DOI] [PubMed] [Google Scholar]
- 3.Bibby H., and McDonald S. (2005). Theory of mind after traumatic brain injury. Neuropsychologia 43, 99–114 [DOI] [PubMed] [Google Scholar]
- 4.Hanten G., Cook L., Orsten K., Chapman S.B., Li X., Wilde E.A., Schnelle K.P., and Levin H.S. (2011). Effects of traumatic brain injury on a virtual reality social problem solving task and relations to cortical thickness in adolescence. Neuropsychologia 49, 486–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moses L.J. (2001). Executive accounts of theory-of-mind development. Child Dev. 72, 688–690 [DOI] [PubMed] [Google Scholar]
- 6.Rosema S., Crowe L., and Anderson V. (2012). Social function in children and adolescents after traumatic brain injury: A systematic review 1989–2011. J. Neurotrauma 29, 1277–1291 [DOI] [PubMed] [Google Scholar]
- 7.Dennis M., Guger S., Roncadin C., Barnes M., and Schachar R. (2001). Attentional-inhibitory control and social-behavioral regulation after childhood closed head injury: Do biological, developmental, and recovery variables predict outcome? J. Int. Neuropsychol. Soc. 7, 683–692 [DOI] [PubMed] [Google Scholar]
- 8.Kurowski B.G., Wade S.L., Kirkwood M.W., Brown T.M., Stancin T., Cassedy A., and Taylor H.G. (2013). Association of parent ratings of executive function with global- and setting-specific behavioral impairment after adolescent traumatic brain injury. Arch. Phys. Med. Rehabil. 94, 543–550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeates K.O., Swift E., Taylor H.G., Wade S.L., Drotar D., Stancin T., and Minich N. (2004). Short- and long-term social outcomes following pediatric traumatic brain injury. J. Int. Neuropsychol. Soc. 10, 412–426 [DOI] [PubMed] [Google Scholar]
- 10.Dennis M., Simic N., Bigler E.D., Abildskov T., Agostino A., Taylor H.G., Rubin K., Vannatta K., Gerhardt C.A., Stancin T., and Yeates K.O. (2013). Cognitive, affective, and conative theory of mind (ToM) in children with traumatic brain injury. Dev. Cogn. Neurosci. 5, 25–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yeates K.O., Gerhardt C.A., Bigler E.D., Abildskov T., Dennis M., Rubin K.H., Stancin T., Taylor H.G., and Vannatta K. (2013). Peer relationships of children with traumatic brain injury. J. Int. Neuropsychol. Soc. 19, 518–527 [DOI] [PubMed] [Google Scholar]
- 12.Yeates K.O., Bigler E.D., Abildskov T., Dennis M., Gerhardt C.A., Vannatta K., Rubin K.H., Stancin T., and Taylor H.G. (2014). Social competence in pediatric traumatic brain injury: From brain to behavior. Clin Psychol Sci 2, 97–107 [Google Scholar]
- 13.Brown R.L. (2010). Epidemiology of injury and the impact of health disparities. Curr. Opin. Pediatr. 22, 321–325 [DOI] [PubMed] [Google Scholar]
- 14.Howard I., Joseph J.G., and Natale J.E. (2005). Pediatric traumatic brain injury: Do racial/ethnic disparities exist in brain injury severity, modality, or medical disposition? Ethn. Dis. 15, Suppl 5, 51–56 [PubMed] [Google Scholar]
- 15.Langlois J.A., Rutland-Brown W., and Thomas K.E. (2005). The incidence of traumatic brain injury among children in the United States: Differences by race. J. Head Trauma Rehabil. 20, 229–238 [DOI] [PubMed] [Google Scholar]
- 16.Dennis M., Francis D.J., Cirino P.T., Schachar R., Barnes M.A., and Fletcher J.M. (2009). Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. J. Int. Neuropsychol. Soc. 15, 331–343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wechsler D. (2003). Wechsler Intelligence Scale for Children-Third Edition manual. The Psychological Corporation: San Antonio, TX [Google Scholar]
- 18.Manly T., Robertson I.H., Anderson V., and Nimmo-Smith I. (1999). TEA-Ch: The Test of Everyday Attention for Children Manual. Thames Valley Test Company Limited: Bury St. Edmunds, UK [Google Scholar]
- 19.Donders J. and Warschausky S. (1997). WISC-III factor index score patterns after traumatic head injury in children. Child Neuropsychol. 3, 71–78 [Google Scholar]
- 20.Anderson V., Fenwick T., Manly T., and Robertson I. (1998). Attentional skills following traumatic brain injury in childhood: a componential analysis. Brain Inj. 12, 937–949 [DOI] [PubMed] [Google Scholar]
- 21.Heaton S.C., Reader S.K., Preston A.S., Fennell E.B., Puyana O.E., Gill N., and Johnson J.H. (2001). The Test of Everyday Attention for Children (TEA-Ch): Patterns of performance in children with ADHD and clinical controls. Child Neuropsychol. 7, 251–264 [DOI] [PubMed] [Google Scholar]
- 22.Dennis M., Simic N., Gerry Taylor H., Bigler E.D., Rubin K., Vannatta K., Gerhardt C.A., Stancin T., Roncadin C., and Yeates K.O. (2012). Theory of mind in children with traumatic brain injury. J. Int. Neuropsychol. Soc. 18, 908–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dennis M., Agostino A., Taylor H.G., Bigler E.D., Rubin K., Vannatta K., Gerhardt C.A., Stancin T., and Yeates K.O. (2013). Emotional expression and socially modulated emotive communication in children with traumatic brain injury. J. Int. Neuropsychol. Soc. 19, 34–43 [DOI] [PubMed] [Google Scholar]
- 24.Dennis M., Simic N., Agostino A., Taylor H.G., Bigler E.D., Rubin K., Vannatta K., Gerhardt C.A., Stancin T., and Yeates K.O. (2013). Irony and empathy in children with traumatic brain injury. J. Int. Neuropsychol. Soc. 19, 338–348 [DOI] [PubMed] [Google Scholar]
- 25.Reynolds C.R. and Kamphaus R.W. (2004). Behavior Assessment System for Children, Second Edition. American Guidance Service: Circle Pines, MN [Google Scholar]
- 26.Harrison P.L. and Oakland T. (2003). Adaptive Behavior Assessment System Second Edition Manual. Psychological Corporation: San Antonio, TX [Google Scholar]
- 27.Preacher K.J., and Hayes A.F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 40, 879–891 [DOI] [PubMed] [Google Scholar]
- 28.Deegan J. (1978). On the occurrence of standardized regression coefficients greater than one. Educ. Psychol. Meas. 38, 873–888 [Google Scholar]
- 29.Carlson S.M., Moses L.J., and Claxton L.J. (2004). Individual differences in executive functioning and theory of mind: an investigation of inhibitory control and planning ability. J. Exp. Child Psychol. 87, 299–319 [DOI] [PubMed] [Google Scholar]
- 30.Gordon A.C., and Olson D.R. (1998). The relation between acquisition of theory of mind and the capacity to hold in mind. J. Exp. Child Psychol. 68, 70–83 [DOI] [PubMed] [Google Scholar]
- 31.Dennis M., Agostino A., Roncadin C., and Levin H. (2009). Theory of mind depends on domain-general executive functions of working memory and cognitive inhibition in children with traumatic brain injury. J. Clin. Exp. Neuropsychol. 31, 835–847 [DOI] [PubMed] [Google Scholar]
- 32.Adolphs R. (2001). The neurobiology of social cognition. Curr. Opin. Neurobiol. 11, 231–239 [DOI] [PubMed] [Google Scholar]
- 33.Adolphs R. (2003). Cognitive neuroscience of human social behavior. Nat. Rev. Neurosci. 4, 165–178 [DOI] [PubMed] [Google Scholar]
- 34.Johnson M.H., Griffin R., Csibra G., Halit H., Farroni T., de Haan M., Tucker L.A., Baron-Cohen S., and Richards J. (2005). The emergence of the social brain network: evidence from typical and atypical development. Dev. Psychopathol. 17, 599–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Levin H.S., and Hanten G. (2005). Executive functions after traumatic brain injury in children. Pediatr. Neurol. 33, 79–93 [DOI] [PubMed] [Google Scholar]
- 36.Dodge K.A., Laird R., Lochman J.E., Zelli A., and Conduct Problems Prevention Research Group. (2002). Multidimensional latent-construct analysis of children's social information processing patterns: correlations with aggressive behavior problems. Psychol. Assess. 14, 60–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lemerise E.A., and Arsenio W.F. (2000). An integrated model of emotion processes and cognition in social information processing. Child Dev. 71, 107–118 [DOI] [PubMed] [Google Scholar]
- 38.Baron R.M., and Kenny D.A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51, 1173–1182 [DOI] [PubMed] [Google Scholar]
- 39.Hayes A.F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Commun. Monogr. 76, 408–420 [Google Scholar]
- 40.Drotar D., Stein R.E., and Perrin E.C. (1995). Methodological issues in using the Child Behavior Checklist and its related instruments in clinical child psychology research. J. Clin. Child Psychol. 24, 184–192 [Google Scholar]
- 41.De Los Reyes A., and Kazdin A.E. (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol. Bull. 131, 483–509 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


