Abstract
Background
Few HIV/STI interventions exist for African American adolescent girls in juvenile detention.
Objective
The objective was to evaluate the efficacy of an intervention to reduce incident STIs, improve HIV-preventive behaviors, and enhance psychosocial outcomes.
Methods
We conducted a randomized controlled trial among African American adolescent girls (13-17 years, N=188) in juvenile detention from March 2011 to May 2012. Assessments occurred at baseline and 3- and 6-months post-randomization and included: audio computer-assisted self-interview, condom skills assessment, and self-collected vaginal swab to detect Chlamydia and gonorrhea.
Intervention
The Imara intervention included three individual-level sessions and four phone sessions; expedited partner therapy was offered to STI-positive adolescents. The comparison group received the usual care provided by the detention center: STI testing, treatment and counseling.
Results
At the 6-month assessment (3-months post-intervention) Imara participants reported higher condom use self-efficacy (p<0.001), HIV/STI knowledge (p<0.001), and condom use skills (p<0.001) compared to control participants. No significant differences were observed between trial conditions in incident Chlamydia or gonorrhea infections, condom use, or number of vaginal sex partners.
Conclusions
Imara for detained African American adolescent girls can improve condom use skills and psychosocial outcomes; however, a critical need for interventions to reduce sexual risk remains.
Introduction
Adolescent girls make up a significant proportion of juvenile arrests in the US. In 2009, law enforcement agencies reported 578,500 arrests of girls under age 18, comprising 30% of overall juvenile arrests (OJJDP 2011a). Despite increases in the proportion of female juvenile arrests over the past 4 decades (OJJDP 2011a), girls in the juvenile justice system have often been referred to as a “neglected population” (Snyder and Sickmund 2006).
Adolescent girls in the juvenile justice system are at high risk for sexually transmitted infections (STIs), including human immunodeficiency virus (HIV) (Chesney-Lind and Sheldon 1998; Lederman et al. 2004). They also report a high prevalence of risk factors associated with STIs and HIV infection, such as family dysfunction, trauma and sexual abuse, mental health and substance abuse problems, and risky sexual behaviors.(Chesney-Lind and Sheldon 1998; Teplin et al. 2006; Lederman et al. 2004; Robertson et al. 2011; Voisin et al. 2012). For example, one study identified 73% of adolescent girls entering the juvenile justice system with a history of sexual abuse (Chesney-Lind and Sheldon 1998). Many of these adolescent girls have experienced trauma, with estimates indicating 84% have experienced a major trauma (Lederman et al. 2004), and 65% having experienced post-traumatic stress disorder at some point in their lives (Cauffman et al. 1998). They also have high rates of depression, anxiety and substance abuse (Staples-Horne 2006; Morris and DiClemente 2007; Voisin et al. 2008; Crosby, Salazar, and DiClemente 2004). Adolescent girls in the juvenile justice system are more likely to affiliate with peers who are delinquent (Snyder and Sickmund 2006; Hubbard and Pratt 2002) and substance users (Morris, Baker, and Huscroft 1992). Collectively, this social, psychological, and behavioral epidemiologic profile indicates substantial risk for HIV/STI acquisition and transmission among girls in the juvenile justice system.
Marked disparities are the over-representation of African American girls in juvenile detention facilities (OJJDP 2011b) and the disproportionate impact of HIV/STI on African American adolescent girls (CDC 2012a, 2012b). In 2008, it was estimated that, nationwide, 1.9% of incarcerated women were HIV-positive (Maruschak and Beavers 2009); this is 13 times as high as the HIV prevalence estimate of 0.15% among adolescent females and adult women (CDC 2012a).
Although substantial empirical evidence indicates the need to develop HIV/STI risk-reduction interventions for African American adolescent girls in the juvenile justice system, evidence-based gender-specific interventions that reduce risk behaviors have not been identified to address the unique needs of this population (CDC 2011; Tolou-Shams et al. 2010). Given the dearth of demonstrated efficacious HIV/STI interventions specifically for adolescent girls in the juvenile justice system, the over-representation of African American adolescent girls in US detention facilities, and their markedly higher HIV/STI risk profile relative to non-detained African American adolescent girls, it is critical to design, implement, and evaluate HIV/STI prevention interventions tailored to the needs of these adolescents.
Adapting existing evidence-based interventions (EBIs) to meet the needs of new target populations and settings is one way to reduce the resources needed to develop new interventions. CDC, through the Adopting and Demonstrating the Adaptation of Prevention Techniques (ADAPT-2), funded Emory University Rollins School of Public Health to use a systematic adaptation process to develop, implement, and evaluate a culturally and gender-relevant HIV/STI risk-reduction intervention for detained African American adolescents girls (CDC 2007). The objective of this study was to test the efficacy of the adapted intervention for incident STIs, HIV/STI-preventive behaviors, and psychosocial outcomes.
Methods
Participants
From March 2011 to February 2012, African American adolescent girls, 13-17 years of age, detained in a short-term juvenile detention facility in Atlanta, Georgia, were recruited to participate in an HIV/STI prevention trial. Detention facility staff escorted all potentially eligible adolescent girls for confidential screening by an African American woman recruiter. The recruiter described the study, solicited participation, and assessed adolescents’ eligibility and interest in participating in the project. Eligibility criteria included self-identifying as African American, being 13-17 years of age, and reporting ever willingly had vaginal intercourse with a male. Adolescents who were married, pregnant, Wards of the State of Georgia, or would be placed in a restricted location upon release (i.e., group home) were excluded from the study. Written informed assent was obtained from adolescents and verbal consent was obtained from parents/guardians prior to implementation of study procedures. Following receipt of consent, adolescents meeting eligibility criteria completed baseline assessments and were randomized to trial conditions. Participants were not compensated for their participation while in the detention facility and were given up to $150 for completion of all intervention sessions and scheduled assessments over the 6-month follow-up period subsequent to their release from the detention facility. Intervention sessions were implemented from March 2011 to May 2012. The Emory University Institutional Review Board (IRB) approved all study protocols.
Study Procedures
Study Design
The study used a two-arm randomized controlled trial design (Piantadosi 2005). Assignment to study conditions was implemented subsequent to baseline assessment using concealment of allocation procedures, defined by protocol and compliant with published recommendations (Schulz and Grimes 2002). Adolescent girls randomized to the intervention condition participated in the Imara intervention. Adolescent girls randomized to the control condition received the usual care provided by the detention facility, which included usual care/counseling for STI treatment.
Intervention Methods
Overview of the Imara intervention
Imara was developed through the adaptation of an existing CDC-defined Tier I EBI, HORIZONS, that was gender- and culturally congruent for African American girls. HORIZONS has demonstrated significant changes in STI incidence, sexual risk behaviors, and hypothesized mediators of sexual behavior in a randomized controlled trial (DiClemente et al. 2009). The ADAPT-ITT model (Wingood and DiClemente 2008) was used to guide the systematic adaptation process tailoring HORIZONS to address the unique needs of detained girls. This process is described in detail elsewhere (Latham et al. 2010).
Imara is a multi-faceted intervention consisting of individual counseling in the detention facility and in adolescent girls’ homes to maintain continuity of prevention services following release from the detention facility. Three individual counseling intervention sessions were each conducted by a trained African American female health educator and were approximately 1.5 hours in duration. The first (baseline) session occurred at the detention facility. The second session occurred in the participants’ homes following discharge from detention, an average of 15 days after the first session. The third session was conducted in participants’ homes at 3-months post-randomization.
The counseling sessions used a combination of approaches including, skills development, HIV/STI risk assessment leading to sexual health goal setting, and interactive computer activities to address multiple aspects of sexual behavior. Intervention sessions were designed to foster a sense of cultural and gender pride and emphasized diverse factors contributing to adolescents’ HIV/STI risk, including individual factors (e.g., HIV/STI risk-reduction knowledge, perceived peer norms supportive of condom use, condom use skills), and relational factors (e.g., persuasive communication techniques to enhance male partner responsibility for condom use). Participants discussed and practiced, via role-plays, partner notification about STIs and treatment. In addition to addressing multiple aspects of sexual risk behavior, the intervention included an emphasis on key issues specific to detained youth identified during study development, including goal setting, decision-making skills, emotion regulation, trauma, and recognizing the relationship between substance use and risky behavior (Latham et al. 2012).
To reinforce prevention concepts discussed in individual counseling sessions, health educators administered 4-brief (20 minute) telephone counseling sessions to adolescents between their release from the detention facility and the 3-month final individual counseling session. These sessions were theory-driven, based on a problem-solving and goal-setting approach designed to identify sexual behavior change goals and strategies, and reinforce prevention concepts discussed in Imara (Beck 1995; Locke and Latham 2002).
In addition, adolescents assigned to the Imara condition were offered Expedited Partner Therapy (EPT) (CDC 2006). EPT was included in the Imara intervention to address the issue of male partner risk, STI reinfection, and sexual network risk for STI. EPT was exclusively offered to Imara participants as it is not standard of care for STI treatment. Participants with a positive laboratory-confirmed test for Chlamydia or gonorrhea were offered single-dose, orally administered medications to give to their male sex partner(s) along with a packet of instructional materials, including a detailed instruction sheet regarding medications and potential adverse reactions, without requiring the male sex partner to be physically examined (CDC 2006). At the time of STI notification, participants were asked if they were comfortable providing STI treatment medication to their male sex partner(s). If participants opted for EPT, a nurse delivered medication for her male sex partner(s) to her home or to a convenient location where she also received directly observed treatment. EPT was provided for up to three male sex partners following each assessment.
Usual Care Control Condition
Adolescents randomized to the usual care control condition received standard services provided by the facility staff, which included weekly, 1-hour, group-based HIV/STI information sessions provided to all youth. Adolescents in the Usual Care condition completed all study assessments on the same schedule as Imara participants, received monthly calls only to reconfirm contact information and schedule follow-up visits, were notified if they had a positive laboratory-confirmed test for Chlamydia or gonorrhea, and received usual care/counseling for STI treatment (but were not provided EPT).
Data Collection
Data collection occurred at baseline (in the detention facility) and at 3- and 6-months post-randomization at participants’ homes or other convenient location. The 3-month assessment occurred immediately prior to the final intervention session to assess interim intervention effects. The 6-month assessment captured the main study outcomes at 3-months post-intervention. Data collection consisted of four components: (1) a urine pregnancy screen, (2) a self-collected vaginal swab assay to assess Chlamydia and gonorrhea, (3) an audio computer-assisted self-interview (ACASI) to assess behavioral and psychosocial variables, and (4) an objective condom skills assessment.
Participants testing positive for pregnancy at baseline were excluded; girls who became pregnant over the course of the follow-up were retained in the study. Staff instructed participants how to self-collect a vaginal swab specimen and specimens were delivered to the Emory University Pathology Laboratory and assayed for C. trachomatis and N. gonorrhoeae using the BDProbeTec ET C. trachomatis and N. gonorrhoeae Amplified DNA assay (Becton Dickinson and Company, Sparks, MD) (Van Der Pol et al. 2001). The study nurse provided directly observed single-dose antimicrobial treatment and risk-reduction counseling per CDC recommendations to all participants with a positive STI test, regardless of study condition assignment. Participants in the Usual Care condition were encouraged to refer sex partners for treatment. Participants in the Imara condition were offered EPT (CDC 2006). The County Health Department was notified of reportable STIs.
Immediately following vaginal swab collection, participants were administered the ACASI. ACASI was used to enhance data accuracy, increase participants’ comfort answering sexually explicit questions, and eliminate low literacy as a potential barrier to completing the interview (Estes et al. 2010; Zimmerman, Atwood, and Cupp 2006). The ACASI assessed sociodemographics, detention history, sexual history, attitudes, and psychosocial constructs associated with HIV/STI-preventive behaviors. Sexual behaviors were assessed for two time periods: the 30 days and 90 days preceding assessments. Multiple strategies were used to enhance accuracy and validity of the self-reported sexual behaviors, including reporting behaviors over relatively brief time intervals (McFarlane and St. Lawrence 1999) and using a modified Timeline Follow-back methodology. This method effectively facilitates retrospective recall of HIV/STI sexual behaviors using a calendar to orient the participant to the relevant timeframes (Carey et al. 2001). To enhance perceived confidentiality participants were informed that only code numbers were used to identify records and data would not be shared with detention staff. Finally, a member of the Imara assessment team administered an observational condom skills assessment objectively, rather than through self-report measuring participants’ condom use skills (DiClemente et al. 2004).
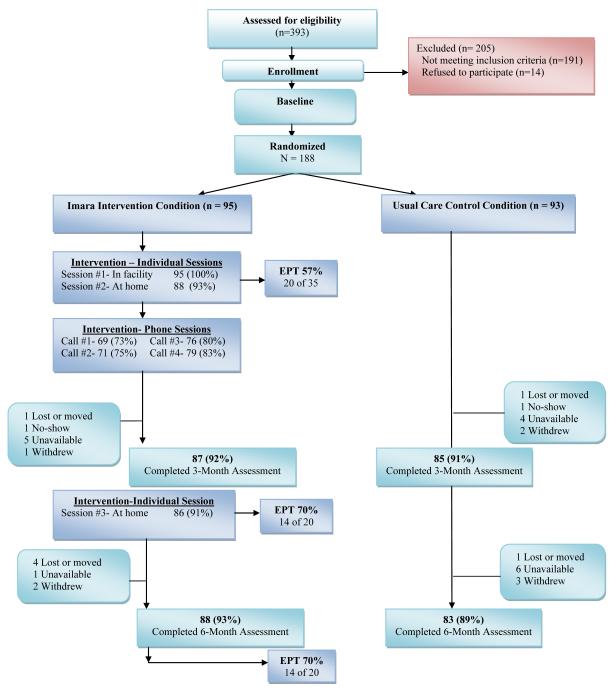
Participant recruitment, allocation, retention, and participation in trial conditions
As described in Figure 1, recruiters approached and screened 393 adolescents, 202 (51%) were eligible and 188 enrolled in the study (93% participation rate). One hundred ninety-one young women did not meet eligibility criteria; primary reasons included no vaginal intercourse (45%), release to a secure location (10%) and pregnancy (9%).
Figure 1.
Participant allocation to Imara trial study conditions
Outcome Measures
Intervention efficacy was assessed using biological, behavioral and psychosocial outcomes.
Primary Biological Outcome
The primary outcome was number of participants detected with a laboratory-confirmed incident infection of Chlamydia or gonorrhea at the 3- or 6-month assessment.
Behavioral Outcome Measures
The primary behavioral outcome was the proportion of condom-protected sex acts in the 30 and 90 days prior to 3- and 6-month assessments; a measure frequently used to evaluate HIV/STI interventions (Sales, Milhausen, and DiClemente 2006). This outcome was calculated as the number of times a condom was used during vaginal intercourse, divided by the total number of vaginal intercourse occasions (DiClemente et al. 2004; DiClemente et al. 2009). Other behaviors assessed included consistent condom use during vaginal, anal and oral sex, having unprotected vaginal sex and number of vaginal sex partners in the 30 and 90 days prior to the 3- and 6-month assessments and condom use skills (DiClemente et al. 2004; DiClemente et al. 2009). Another behavioral indicator, condom skills, was objectively assessed using a checklist of correct condom use (DiClemente et al. 2004). Seven skills were observed while putting a male condom on a penis model: package was opened at top corner carefully, air removed from condom, condom placed right side up on tip of penis, condom rolled correctly downward, condom rolled to base of penis, space left at tip of condom, condom remained intact (no rips or punctures). The observer’s ratings of the presence or absence of condom use skills were summed to obtain a total condom use score with higher scores representing more condom skill proficiency.
Psychosocial Outcomes
Psychosocial constructs associated with HIV/STI-preventive behaviors were derived from the underlying theoretical frameworks, our qualitative research, and a review of the empirical literature. Constructs were assessed using scales with satisfactory psychometric properties previously used with African American adolescent females (Wingood and DiClemente 2002). HIV/STI prevention knowledge was measured using an 11-item index modified from Sikkema (Sikkema et al. 2000). Knowledge items which were incorrectly answered were assigned a value of 1 whereas correctly answered items were assigned a value of 2. Items were then summed; thus higher scores are indicative of greater HIV/STI prevention knowledge. Condom use self-efficacy was measured using a 9-item scale (α = 0. 91) and partner communication self-efficacy was assessed with a 6-item index (α=0. 79) (Wingood and DiClemente 1998).
Baseline Measures
In addition to the outcome measures, participant characteristics measured at baseline included family aid index, neighborhood quality and having a boyfriend with concurrent sexual partners. Family aid was assessed with a 4-item index (Salazar, Crosby, and Diclemente 2009). Participants reported whether anyone in their household received the following services during the past year: a) welfare, b) food stamps, c) Women, Infants and Children (WIC) and d) Section 8 housing subsidies (yes/no). The number of “yes” responses were summed with higher scores indicating receipt of a greater number of forms of government assistance. Neighborhood quality was assessed with 3 questions about the physical condition of participants’ neighborhood (Cohen 2000). A sample item is, “On your street, are there abandoned homes or apartments?” Responses to all three Yes/No questions were summed to create an index of neighborhood quality with higher scores indicative of poorer neighborhood quality. Girls who reported having a boyfriend/ main partner and having sex with that partner were asked, “During your relationship with your boyfriend, has he had vaginal sex with another woman?” (yes/no) (Brown et al. 2012). Participants who answered yes were categorized as perceiving their boyfriend to have concurrent sexual partners.
Statistical Methods
T-tests and chi-square statistics assessed baseline differences between study conditions. Differences significant at p<0.05 were eligible for inclusion in multivariable models as potential confounders; however, none of the factors assessed significantly differed between study conditions. Efficacy analyses were performed using an intention-to-treat protocol. Differences in the outcome measures at the 3- and 6-month assessments were evaluated for participants assigned to the Imara condition relative to participants assigned to the Usual Care control condition. Linear and logistic regression models compared outcomes by trial condition at the 3- and 6-month assessments. The efficacy of the Imara intervention over the 6-month follow-up period was also assessed using linear and logistic generalized estimating equations (GEE). Planned a priori, all models adjusted for the baseline measure of the outcome variable. Statistical associations were significant for estimates with p<.05. Analyses were performed using SAS software version 9.3 (SAS Institute, Cary, NC).
RESULTS
Study Sample and Retention
The 188 participants were randomized to one of two conditions; 95 to the Imara intervention and 93 to the Usual Care control condition (Figure 1). Of the 95 participants allocated to the Imara HIV risk-reduction intervention, 87 (92%) completed the 3-month assessment and 88 (93%) completed the 6-month assessment. Of the 93 participants allocated to the Usual Care control condition, 85 (91%) completed the 3-month assessment and 83 (89%) completed the 6-month assessment. No significant differences were observed in attrition between the Imara intervention and the Usual Care control condition (p=.71). The overall study retention rate was 91% (n=172) at the 3-month assessment and 91% (n=171) at the 6-month assessment.
Of the 95 Imara participants, 100% received the first intervention session, 93% (n=88) received the second session, and 91% (n=86) received the third session. Time of release affected call completion rates, which ranged from 73% at the first call to 83% at the fourth call. Acceptance of EPT among Imara participants who tested positive for an STI varied markedly; 57% (20/35) elected EPT at baseline, 70% (14/20) at 3-months, and 70% (14/20) at 6-months. Directly observed therapy for Imara participants who tested positive for an STI was high, with 94% (33/35) at baseline, 100% (21/21) at 3-months, and 90% (18/20) at 6-months. All 93 participants in the Usual Care control condition received services provided by the detention facility as the standard of care. Directly observed therapy for Usual Care control participants who tested positive for an STI was 97% (29/30) at baseline, 95% (19/20) at 3-months, and 69% (11/16) at 6-months.
Baseline Characteristics
On average, participants were 15.3 years of age at baseline (Table 1). The mean number of days participants had been detained was 3.75. The sample had a high prevalence of HIV/STI-associated risk factors, including emotional (56%), physical (43%), and sexual (24%) abuse. Over one-third (35%) of the sample was infected with Chlamydia and/or gonorrhea at baseline. No statistically significant differences were observed between trial conditions at baseline.
Table 1.
Baseline characteristics of detained African American girls participating in the Imara HIV/STI prevention trial, Atlanta, GA, 2011-2012
| Characteristic | Overall (n=188) |
Imara Intervention Condition (n = 95) |
Usual Care Control Condition (n = 93) |
p- value |
|---|---|---|---|---|
|
| ||||
| Sociodemographics, mean (SD) | ||||
|
| ||||
| Age in years | 15.31 (1.06) | 15.29 (1.10) | 15.34 (1.02) | 0.750 |
|
| ||||
| Family aid index | 1.10 (0.91) | 1.01 (0.91) | 1.18 (0.91) | 0.194 |
|
| ||||
| Poor neighborhood quality | 0.97 (1.14) | 0.84 (1.10) | 1.11 (1.17) | 0.111 |
|
| ||||
| Incarceration | ||||
|
| ||||
| Number days detained for current offense, mean (SD) |
3.75 (4.92)a | 4.07 (5.71)b | 3.42 (3.93)c | 0.365 |
|
| ||||
| Type of offense committed, n (%) | d | e | f | |
| Status | 108 (57) | 54 (58.06) | 54 (59.34) | 0.525 |
| Property offense | 15 (8.15) | 10 (10.75) | 5 (5.49) | |
| Personal larceny | 10 (5.43) | 6 (6.45) | 4 (4.40) | |
| Weapons | 3 (1.63) | 0 | 3 (3.30) | |
| Violent offense | 38 (20.65) | 18 (19.35) | 20 (21.98) | |
| Non-violent sexual offense | 2 (1.09) | 1 (1.08) | 1 (1.10) | |
| Violation of parole | 8 (4.35) | 4 (4.30) | 4 (4.40) | |
|
| ||||
| Relationship characteristics | ||||
|
| ||||
| Current boyfriend, n (%) | 166 (88.30) | 84 (88.42) | 82 (88.17) | 0.958 |
|
| ||||
| Length of current relationship, months, mean (SD) | 10.80 (11.32)g | 10.95 (12.09)h | 10.65 (10.54)i | 0.862 |
|
| ||||
| Perceived boyfriend concurrency, (n %) | 53 (37.59)j | 22 (31.88)k | 31 (43.06)l | 0.171 |
|
| ||||
| Sex partners generally ≥2 years older, n (%) | 110 (58.51) | 52 (54.74) | 58 (62.37) | 0.288 |
|
| ||||
| History of abuse, n (%) | ||||
|
| ||||
| Emotional | 106 (56.38) | 50 (52.63) | 56 (60.22) | 0.294 |
|
| ||||
| Physical | 80 (42.55) | 37 (38.95) | 43 (46.24) | 0.312 |
|
| ||||
| Sexual | 45 (23.94) | 24 (25.26) | 21 (22.58) | 0.666 |
|
| ||||
| Other factors, n (%) | ||||
|
| ||||
| History of alcohol use | 148 (78.72) | 72 (75.79) | 76 (81.72) | 0.320 |
|
| ||||
| History of marijuana use | 140 (74.47) | 70 (73.68) | 70 (75.27) | 0.803 |
|
| ||||
| Ever member of a gang | 51 (27.13) | 23 (24.21) | 28 (30.11) | 0.363 |
|
| ||||
| Immediate family member ever incarcerated | 130 (69.15) | 61 (64.21) | 69 (74.19) | 0.138 |
|
| ||||
| Sexually transmitted infections, n (%) | ||||
|
| ||||
| Chlamydia | 64 (34.04) | 34 (35.79) | 30 (32.26) | 0.609 |
|
| ||||
| Gonorrhea | 23 (12.23) | 13 (13.68) | 10 (10.75) | 0.540 |
|
| ||||
| Any bacterial STI | 65 (34.57) | 35 (36.84) | 30 (32.26) | 0.509 |
|
| ||||
| Sexual behaviors and Condom Use Skills | ||||
|
| ||||
| Proportion condom use, past 30 days, mean (SD) | 0.48 (0.42)m | 0.48 (0.42)n | 0.49 (0.43)n | 0.972 |
|
| ||||
| Proportion condom use, past 90 days, mean (SD) | 0.55 (0.41)o | 0.55 (0.40)e | 0.55 (0.42)p | 0.922 |
|
| ||||
| Consistent condom use during vaginal, anal and oral sex, past 30 days, n (%) |
41 (27.33)q | 20 (26.32)r | 21 (28.38)s | 0.777 |
|
| ||||
| Consistent condom use during vaginal, anal and oral sex, past 90 days, n (%) |
48 (28.57)t | 23 (27.38)u | 25 (29.76)v | 0.733 |
|
| ||||
| Unprotected vaginal sex, past 30 days, n (%) | 101 (53.72) | 52 (54.74) | 49 (52.69) | 0.778 |
|
| ||||
| Unprotected vaginal sex, past 90 days, n (%) | 110 (58.51) | 55 (57.89) | 55 (59.14) | 0.862 |
|
| ||||
| Condom use skills, mean (SD) | 3.76 (1.05) | 3.69 (1.08) | 3.82 (1.01) | 0.410 |
|
| ||||
| Number of sex partners, past 30 days, mean (SD) | 1.86 (3.65) | 2.31 (5.10) | 1.41 (0.66) | 0.135 |
|
| ||||
| Number of sex partners, past 90 days, mean (SD) | 2.16 (4.32) | 2.58 (5.86) | 1.73 (1.55) | 0.179 |
|
| ||||
| Psychosocial outcomes, mean (SD) | ||||
|
| ||||
| Condom use self-efficacy | 34.60 (9.00) | 34.38 (9.28) | 34.82 (8.75) | 0.740 |
|
| ||||
| Partner sexual communication self-efficacy | 20.56 (3.53) | 20.29 (3.60) | 20.83 (3.46) | 0.302 |
|
| ||||
| Partner sexual communication frequency | 11.27 (5.04) | 11.19 (5.10) | 11.35 (5.01) | 0.823 |
|
| ||||
| Parental sexual communication frequency | 13.86 (6.25) | 14.11 (6.36) | 13.61 (6.16) | 0.591 |
|
| ||||
| Refusal self-efficacy | 23.25 (4.43) | 23.24 (4.12) | 23.26 (4.74) | 0.980 |
|
| ||||
| Fear of condom negotiation | 8.46 (3.67) | 8.12 (2.78) | 8.82 (4.38) | 0.191 |
|
| ||||
| Depressive symptoms | 17.86 (7.68) | 17.63 (7.33) | 18.09 (8.05) | 0.686 |
|
| ||||
| Sexual sensation seeking | 18.63 (5.53) | 19.03 (5.89) | 18.23 (5.14) | 0.319 |
|
| ||||
| HIV/STI knowledge | 17.67 (2.37) | 17.85 (2.25) | 17.48 (2.48) | 0.288 |
n=185;
n=94;
n=91;
n=184;
n=93;
n=91;
n=166;
n=84;
n=82;
n=141;
n=69;
n=72;
n=156;
n=73;
n=165;
n=83;
n=150;
n=74;
n=76;
n=171
n=86;
n=85
Summary of Outcome Variables
Of note, the baseline means and proportions for HIV/STI-protective behaviors and incident STIs (Table 1) suggested a higher risk profile at baseline than at 3- and 6-month assessments for both the intervention and control groups (Table 2). Statistically significant differences were observed in the means between the intervention and control groups for condom use self-efficacy, HIV/STI knowledge, and condom use skills at both the 3- and 6-month assessments.
Table 2.
Summary of biological, behavioral and psychosocial outcomes at 3- and 6-month assessments by trial condition, Atlanta, GA 2011-2012
| Outcome | 3-month Assessment | 6-month Assessment | ||||
|---|---|---|---|---|---|---|
| Imara Intervention Condition (n=87) |
Usual Care Control Condition (n=85) |
p-value | Imara Intervention Condition (n=88) |
Usual Care Control Condition (n=83) |
p-value | |
| Mean (SD) | Mean (SD) | |||||
| Partner sexual communication self- efficacy |
20.38 (3.69) | 19.71 (4.11) | 0.260 | 20.74 (3.53) | 20.54 (3.76) | 0.725 |
| Condom use self- efficacy |
39.60 (7.00) | 36.07 (8.28) | 0.003 | 40.91 (6.89) | 36.41 (7.93) | <0.001 |
| HIV/STI knowledge | 18.74 (2.19) | 17.58 (2.56) | 0.002 | 19.22 (1.63) | 17.65 (2.79) | <0.001 |
| Proportion condom- protected vaginal sex acts, past 30 days |
0.66 (0.41)a | 0.62 (0.43)b | 0.606 | 0.51 (0.45)a | 0.55 (0.42)c | 0.681 |
| Proportion condom- protected vaginal sex acts, past 90 days |
0.65 (0.38)d | 0.64 (0.40)e | 0.879 | 0.62 (0.40)f | 0.65 (0.39)g | 0.710 |
| Number of vaginal sex partners, past 30 days |
1.38 (0.67)a | 1.56 (1.56)b | 0.469 | 1.48 (1.17)a | 1.45 (1.10)c | 0.896 |
| Number of vaginal sex partners, past 90 days |
1.83 (2.64) | 1.76 (5.44) | 0.923 | 1.61 (2.03) | 1.39 (1.49) | 0.402 |
| Condom use skills | 5.51 (1.57)h | 4.19 (1.48)i | <0.001 | 5.94 (1.24)j | 3.88 (1.22)k | <0.001 |
| n (%) | n (%) | |||||
| Consistent condom use during vaginal, anal and sex, past 30 days |
20 (40.82)c | 21 (42.86)c | 0.838 | 18 (33.96)l | 20 (38.46)m | 0.632 |
| Consistent condom use during vaginal, anal and oral sex, past 90 days |
23 (35.38)n | 23 (38.98)o | 0.679 | 26 (37.68)f | 30 (44.78)g | 0.401 |
| Unprotected vaginal sex, past 30 days |
24 (27.59) | 23 (27.06) | 0.938 | 29 (32.95) | 29 (34.94) | 0.784 |
| Unprotected vaginal sex, past 90 days |
38 (43.68) | 33 (38.82) | 0.518 | 40 (45.45) | 36 (43.37) | 0.784 |
| Chlamydia | 17 (19.54) | 16 (19.05)h | 0.935 | 16 (18.18) | 8 (9.64) | 0.108 |
| Gonorrhea | 6 (6.90) | 5 (5.95)h | 0.801 | 9 (10.23) | 8 (9.64) | 0.898 |
| Any bacterial STI | 20 (22.99) | 19 (22.62)h | 0.954 | 20 (22.73) | 14 (16.87) | 0.34 |
n=48;
n=47;
n=49;
n=64;
n=58;
n=69;
n=67;
n=84;
n=81;
n=83;
n=77;
n=53;
n=52;
n=65;
n=59
Intervention Effects on Biological and Behavioral Outcomes
The regression models showed no statistical significance in the effects on the intervention group for consistent condom use, unprotected vaginal sex, the proportion of condom-protected sex acts, number of vaginal sex partners, or incidence of chlamydial or gonorrheal infections at the 3- or 6-month assessments, or across the 6-month follow-up period (Table 3). Importantly, condom use skills were significantly higher among participants in the intervention condition than control participants (Table 3). At the 6-month assessment, adjusting for baseline condom use skills score, the mean difference in condom use skills for participants assigned to the intervention condition relative to the control condition was 2.12 (95% CI: 1.76, 2.49).
Table 3.
Effect estimates of Imara intervention condition with biological, behavioral and psychosocial outcomes, Atlanta, GA 2011-2012
| Outcome | Regression 1a* | Regression 2b* | GEE Modelc* | |||
|---|---|---|---|---|---|---|
| Linear Models | Beta Coefficient (95% CI) |
p-value | Beta Coefficient (95% CI) |
p-value | Beta Coefficient (95% CI) |
p-value |
| Partner sexual communication self-efficacy |
1.13 (0.11, 2.15) |
0.030 | 0.52 (−0.48, 1.52) |
0.307 | 0.84 (−0.002, 1.68) |
0.050 |
| Condom use self-efficacy | 3.68 (1.76, 5.61) |
<0.001 | 4.43 (2.26, 6.60) |
<0.001 | 3.99 (2.35, 5.63) |
<0.001 |
| HIV/STI knowledge | 1.04 (0.43, 1.64) |
0.001 | 1.33 (0.78, 1.88) |
<0.001 | 1.19 (0.71, 1.68) |
<0.001 |
| Proportion condom-protected vaginal sex acts, past 30 days |
−0.0004 (−0.16, 0.16) |
0.996 | −0.04 (−0.22, 0.15) |
0.699 | −0.02 (−0.14, 0.10) |
0.719 |
| Proportion condom-protected vaginal sex acts, past 90 days |
0.001 (−0.13, 0.13) |
0.989 | −0.001 (−0.13, 0.13) |
0.986 | 0.001 (−0.10, 0.10) |
0.981 |
| Number of vaginal sex partners, past 30 days |
−0.33 (−0.87, 0.21) |
0.226 | −0.10 (−0.57, 0.36) |
0.668 | −0.22 (−0.56, 0.13) |
0.219 |
| Number of vaginal sex partners, past 90 days |
−0.31 (−1.53, 0.92) |
0.621 | −0.003 (−0.46, 0.46) |
0.991 | −0.17 (−0.90, 0.55) |
0.635 |
| Condom use skills | 1.39 (0.93, 1.85) |
<0.001 | 2.12 (1.76, 2.49) |
<0.001 | 1.75 (1.44, 2.06) |
<0.001 |
| Logistic Models |
AOR
(95% CI) |
p-value |
AOR
(95% CI) |
p-value |
AOR
(95% CI) |
p-value |
| Consistent condom use during vaginal, anal and oral sex, past 30 days |
0.83 (0.34, 2.00) |
0.675 | 0.97 (0.37, 2.54) |
0.954 | 0.89 (0.46, 1.72) |
0.736 |
| Consistent condom use during vaginal, anal and oral sex, past 90 days |
0.99 (0.42, 2.32) |
0.979 | 0.88 (0.42, 1.85) |
0.733 | 0.91 (0.48, 1.70) |
0.761 |
| Unprotected vaginal sex, past 30 days |
0.98 (0.49, 1.95) |
0.946 | 0.86 (0.45, 1.64) |
0.636 | 0.92 (0.55, 1.53) | 0.740 |
| Unprotected vaginal sex, past 90 days |
1.28 (0.66, 2.49) |
0.472 | 1.06 (0.57, 1.99) |
0.852 | 1.15 (0.68, 0.94) |
0.610 |
| Chlamydia | 1.03 (0.48, 2.22) |
0.935 | 2.02 (0.81, 5.06) |
0.131 | 1.37 (0.76, 2.47) |
0.291 |
| Gonorrhea | 1.07 (0.28, 4.02) |
0.919 | 1.01 (0.37, 2.80) |
0.976 | 1.03 (0.44, 2.39) |
0.944 |
| Any bacterial STI | 1.01 (0.49, 2.09) |
0.974 | 1.41 (0.66, 3.03) |
0.38 | 1.19 (0.69, 2.06) |
0.532 |
Regression models for 3-month outcomes;
Regression models for 6-month outcomes;
Generalized estimating equation;
All models adjusted for baseline measure of outcome variable
Intervention Effects on Psychosocial Outcomes
Participants assigned to the Imara intervention condition reported greater condom use self-efficacy (p<0.005) and HIV/STI knowledge (p<0.005) than control participants at the 3-month and 6-month assessments, and over the entire study period (Table 3). At the 6-month assessment, adjusting for baseline condom use self-efficacy, the mean difference in condom use self-efficacy for participants assigned to the intervention condition relative to the control condition was 4.43 (95% CI: 2.26, 6.60). At the 6-month assessment, adjusting for baseline HIV/STI knowledge, the mean difference in HIV/STI knowledge for participants assigned to the intervention condition relative to the control condition was 1.33 (95% CI: 0.78, 1.88). In adjusted analyses, participants assigned to the intervention condition reported greater partner communication self-efficacy (p=0.03) at the 3-month assessment relative to the control condition; however, the effect did not remain statistically significant at the 6-month assessment (p=0.30) or throughout the entire study period (p=0.05).
Comment
The threat of HIV/STI among African Americans adolescent girls in detention facilities is a major health crisis that reflects a longstanding racial disparity (Belenko et al. 2008). The present study was an effort to develop, implement, and evaluate a culturally and gender-congruent HIV/STI intervention, one that addresses a broad array of factors that influence detained African American adolescent girls’ sexual risk behaviors, including communication skills, condom skills, emotion regulation, decision-making, and goal setting (Latham et al. 2010). Overall, significant intervention effects in behavioral outcomes (consistent condom use, proportion unprotected sex and number of partners) or in incident laboratory-confirmed chlamydial or gonococcal infections were not observed. However, significant intervention effects were observed for psychosocial outcomes, condom use self-efficacy and HIV/STI knowledge, which may mediate the association with HIV/STI-preventive behaviors, and a behavioral measure of condom skills, suggesting some promise for this intervention approach. The high retention rates indicate adolescent girls were engaged and motivated to participate even after release from the detention facility. In addition, EPT appeared to be acceptable in this sample although we are unable to make conclusions about the role of EPT on the overall findings of the Imara intervention since the study was not designed to facilitate a principal components analysis. The lack of significant behavioral and biological intervention effects, however, demonstrates the need to intensify future HIV/STI interventions.
Suggestions for future interventions
Myriad behavioral, psychological, social, familial and environmental challenges confronting adolescent girls in detention facilities are important to adequately address. This would likely involve delving deeper into the existing Imara content (individual risk behavior, male partner risk, emotion regulation, decision-making, substance use), incorporating new content (managing fear/anxiety related to trauma and abuse, linkages to social service agencies), and considering multilevel intervention models involving families, peers, and/or social networks. These adjustments may enhance individuals’ ability to sustain newly acquired protective behaviors over time.
A more in-depth focus on trauma, in particular, would be beneficial given the lifetime prevalence of this risk factor for HIV/STI. For example, similar to successful interventions designed to reduce traumatic stress and sexual risk behaviors among people living with HIV who have histories of abuse or trauma (Sikkema et al. 2007), interventions for detained adolescent girls may consider providing more in-depth content on specific strategies to manage and overcome fear or anxiety related to past trauma or abuse and about being assertive in sexual situations. Doing so may improve the efficacy of STI/HIV prevention programs for adolescents who have trauma histories.
Although individual-level interventions have demonstrated prevention value, the range, magnitude and consistency of intervention effects may be limited and may not be sufficient to support the adoption and maintenance of HIV/STI prevention behaviors. Other combination behavioral models, which are integrated across multiple levels of intervention to create prevention synergies, may maximize the likelihood of adolescent girls’ adopting and sustaining HIV preventive behaviors (Wingood et al. 2013). These models may include concurrent individual and family-based interventions (Brody et al. 2012) that increase awareness of HIV/STI risk among both the adolescent and her parent or caregiver to support and reinforce prevention behaviors. This model has the added advantage of potentially changing the familial environment, enhancing parent/caregiver skills for monitoring their adolescent’s whereabouts and affiliations. Parental monitoring has been identified as a key predictor of HIV-associated risk behaviors among adolescents (Nappi et al. 2009; DiClemente, Crosby, and Wingood 2002).
Other multilevel intervention models may include social network approaches designed to target peers, male partners, and the social network of adolescent girls. Dyadic interventions involving male partners have multiple benefits. Incarceration interrupts sexual partnerships resulting in non-detained male sex partners engaging in concurrent sex partnerships (Nunn et al. 2012). While Imara discussed male partner risk (i.e., partner’s STI history and partner concurrency) future interventions can more intensively focus on partner- and relationship-level HIV/STI risk in dyads. Addressing risk in detained girls’ sexual networks is also useful, given that approximately 37% of girls in Imara were concerned about their male partners having concurrent sexual partners while they were in detention. None of these intervention approaches is designed to be implemented singularly; but rather, they are designed to be used as part of a combination approach in which interventions complement each other and provide synergy-enhancing HIV/STI prevention.
While intervention models may benefit from utilizing a multilevel approach, there is utility in having a range of implementation modalities. Thus, while individual counseling may be important to address a girls’ specific challenges, other modalities, such as group-formatted interventions have value in enhancing prosocial norms supportive of HIV/STI-preventive behaviors, providing peer modeling and an opportunity to practice prevention skills, and enhance peer social support to initiate and maintain preventive behaviors. Furthermore, new media technologies, such as smart phone applications, and established technology, such as SMS (texting) and mobile phone contacts, can be used to enhance contact between program staff and girls, reinforcing prevention messages, addressing newly emerging health threats, and providing a readily accessible and caring adult to provide guidance. Similar to having comprehensive intervention content, it is important to consider concurrently incorporating multiple intervention modalities. Whatever combination of interventions or implementation modalities selected, interventions strategies can benefit from being designed to be gender and culturally congruent and developmentally appropriate.
Finally, while intervening in juvenile detention facilities is desirable, it is not sufficient. Upon release, girls return to their communities, socio-sexual networks and male sex partners, all of which may confer HIV/STI risk. Thus, while intervening in detention facilities has value, interventions need to provide continuity of prevention services for girls upon returning to their communities, optimizing intervention impact and bridging a potentially dangerous transition from the detention facility and to their community.
Strengths and Limitations
Study strengths included using a randomized controlled trial design, a usual care control condition, use of ACASI technology, and use of laboratory-confirmed STIs to provide an objective measure of the efficacy of the intervention. Finally, while the sample is often difficult to retain in trials, retention rates were high for both, the 3- and 6-month assessments.
The present study was not without limitations. The study sample size limited the statistical power to detect intervention effects and the relatively short follow-up period post-intervention may not have been sufficient to capture intervention effects on longer-term behavior change. However, given small effect sizes for the sexual behavior outcomes, lack of power does not likely account for the non-significant findings. Further, the findings may not be applicable to African American adolescent girls with different sociodemographic characteristics or risk profiles, adolescent girls from other ethnic/racial groups or to adolescent males. Finally, it was not possible to blind study personnel administering follow-up assessments of condition assignment. The use of ACASI limited measurement error; however, the objective condom skill assessment could have been subject to observer bias despite specific protocols and training assessment personnel to collect this measure.
Conclusion
Society may have underestimated the impact of the HIV/STI “national health crisis” for African Americans (Southern AIDS Coalition 2012). Adolescent African American girls in juvenile detention are one important population to reach with effective prevention services. In the absence of vaccines for many STIs, including Chlamydia, gonorrhea and HIV, the urgency for additional prevention research with this vulnerable population is clear and compelling. A comprehensive research agenda can support the development of innovative HIV/STI prevention approaches that more precisely target the range of social determinants associated with HIV/STI risk behaviors.
Acknowledgements
This study was supported by a grant from the Centers for Disease Control and Prevention, Cooperative Agreement number 5 UR6 PS000679. The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Teaniese L. Davis and Jennifer L. Brown were supported by National Institute of General Medical Sciences grant number K12 GM000680. Andrea Swartzendruber was supported by National Institute on Alcohol Abuse and Alcoholism grant number F32 AA022058. Jessica M. Sales was supported by the National Institute of Mental Health grant number K01 MH085506.
REFERENCES
- Beck JS. Cognitive therapy: Basics and beyond, Cognitive therapy: Basics and beyond. Guilford Press; New York, NY US: 1995. [Google Scholar]
- Belenko Steven, Dembo Richard, Weiland Doris, Rollie Matthew, Salvatore Christopher, Hanlon Alexandra, Childs Kristina. Recently arrested adolescents are at high risk for sexually transmitted diseases. Sexually Transmitted Diseases. 2008;no. 35(8):758–763. doi: 10.1097/OLQ.0b013e31816d1f94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody Gene H., Chen Yi-fu, Kogan Steven M., Yu Tianyi, Molgaard Virginia K., DiClemente Ralph J., Wingood Gina M. Family-centered Program Deters Substance Use, Conduct Problems, and Depressive Symptoms in Black Adolescents. Pediatrics. 2012;no. 129(1):108–115. doi: 10.1542/peds.2011-0623. doi: 10.1542/peds.2011-0623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Weinhardt LS. Assessing sexual risk behaviour with the Timeline Followback (TLFB) approach: continued development and psychometric evaluation with psychiatric outpatients. International Journal of STD & AIDS. 2001;no. 12(6):365–375. doi: 10.1258/0956462011923309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cauffman E, Feldman S, Steiner H, Waterman J. Posttraumatic Stress Disorder Among Female Juvenile Offenders. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;no. 37(11):1209–1216. [PubMed] [Google Scholar]
- CDC Expedited partner therapy in the management of sexually transmitted diseases. US Department of Health and Human Services. 2006 Available from http://www.cdc.gov/std/treatment/EPTFinalReport2006.pdf.
- — — — . PS07-004: Adopting and demonstrating the adaptation of prevention techniques for persons at highest risk of acquiring or transmitting human immunodeficiency Virus (ADAPT2) - (UR6) CDC; Atlanta, GA: 2007. [Google Scholar]
- — — — [cited June 25 2013];Compendium of evidence-based HIV behavioral interventions: Risk reduction chapter 2011. 2013 Available from http://www.cdc.gov/hiv/topics/research/prs/rr_chapter.htm.
- — — — . HIV Surveillance Report, 2010. Vol. 22. U.S. Health and Human Services, Centers for Disease Control and Prevention; Atlanta: 2012a. [Google Scholar]
- — — — Sexually transmitted disease surveillance. 2012b. 2011.
- Chesney-Lind M, Sheldon RG. Girls, Delinquency, and Juvenile Justice. Brooks/Cole; Grove, CA: 1998. [Google Scholar]
- Cohen, Spear Deborah, Scribner Suzanne, Kissinger Richard, Mason Patty, John Karen Wildgen. ‘Broken Windows’ and the Risk of Gonorrhea. American Journal of Public Health. 2000;no. 90(2):230–236. doi: 10.2105/ajph.90.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosby R, Salazar LF, DiClemente RJ. Lack of recent condom use among detained adolescent males: a multilevel investigation. Sexually Transmitted Infections. 2004;no. 80(6):425–429. doi: 10.1136/sti.2004.009639. doi: 10.1136/sti.2004.009639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente RJ, Crosby RA, Wingood GM. Enhancing STD/HIV prevention among adolescents: the importance of parenteral monitoring. Minerva Pediatrica. 2002;no. 54(3):171–177. [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Harrington KF, Lang DL, Davies SL, Hook EW, III, Oh MK, Crosby RA, Hertzberg VS, Gordon AB, Hardin JW, Parker S, Robillard A. Efficacy of an HIV prevention intervention for African American adolescent girls: a randomized controlled trial. JAMA: Journal of the American Medical Association. 2004;no. 292(2):171–179. doi: 10.1001/jama.292.2.171. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Wingood GM, Rose ES, Sales JM, Lang DL, Caliendo AM, Hardin JW, Crosby RA. Efficacy of sexually transmitted disease/human immunodeficiency virus sexual risk-reduction intervention for African American adolescent females seeking sexual health services: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2009;no. 163(12):1112–1121. doi: 10.1001/archpediatrics.2009.205. doi: 10.1001/archpediatrics.2009.205. [DOI] [PubMed] [Google Scholar]
- Estes Larissa J., Lloyd Linda E., Teti Michelle, Raja Sheela, Bowleg Lisa, Allgood Kristi L., Glick Nancy. Perceptions of Audio Computer-Assisted Self- Interviewing (ACASI) among Women in an HIV-Positive Prevention Program. Plos One. 2010;no. 5(2):1–8. doi: 10.1371/journal.pone.0009149. doi: 10.1371/journal.pone.0009149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hubbard, Jones Dana, Pratt Travis C. A Meta-Analysis of the Predictors of Delinquency Among Girls. Journal of Offender Rehabilitation. 2002;no. 34(3):1. [Google Scholar]
- Latham Teaniese P., Sales Jessica M., Boyce Lorin S., Renfro Tiffaney L., Wingood Gina M., DiClemente Ralph J., Rose Eve. Application of ADAPT-ITT: adapting an evidence-based HIV prevention intervention for incarcerated African American adolescent females. Health Promotion Practice no. 2010;11(3 Suppl):53S–60S. doi: 10.1177/1524839910361433. doi: 10.1177/1524839910361433. [DOI] [PubMed] [Google Scholar]
- Latham Teaniese P., Sales Jessica M., Renfro Tiffaney L., Boyce Lorin S., Rose Eve, Murray Colleen C., Wingood Gina M., DiClemente Ralph J. Employing a teen advisory board to adapt an evidence-based HIV/STD intervention for incarcerated African-American adolescent women. Health Education Research. 2012;no. 27(5):895–903. doi: 10.1093/her/cyr003. [DOI] [PubMed] [Google Scholar]
- Lederman Cindy S., Dakof Gayle A., Larrea Maria A., Li Hua. Characteristics of adolescent females in juvenile detention. International Journal Of Law And Psychiatry. 2004;no. 27(4):321–337. doi: 10.1016/j.ijlp.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Locke Edwin A., Latham Gary P. Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. American Psychologist. 2002;no. 57(9):705–717. doi: 10.1037//0003-066x.57.9.705. doi: 10.1037/0003-066x.57.9.705. [DOI] [PubMed] [Google Scholar]
- Maruschak LM, Beavers R. Bureau of Justice Statistics Bulletin: HIV in Prisons, 2007-08. Bureau of Justice Statistics. 2009 [Google Scholar]
- McFarlane Mary, St. Lawrence Janet S. Adolescents’ recall of sexual behavior: Consistency of self-report and effect of variations in recall duration. Journal of Adolescent Health. 1999;no. 25(3):199–206. doi: 10.1016/s1054-139x(98)00156-6. doi: 10.1016/s1054-139x(98)00156-6. [DOI] [PubMed] [Google Scholar]
- Morris R, DiClemente RJ. High-Risk and Out-of-Control Behavior. In: Neinstein L, editor. Adolescent Healthcare. 5th Edition Lippincott Williams & Wilkins; New York: 2007. [Google Scholar]
- Morris RE, Baker CJ, Huscroft S. Incarcerated youth at risk for HIV infection. In: DiClemente RJ, editor. Adolescents and AIDS: A generation in jeopardy. Sage Publications; Thousand Oaks, CA: 1992. pp. 52–70. [Google Scholar]
- Nappi CM, Thakral C, Kapungu C, Donenberg GR, DiClemente R, Brown L. Parental monitoring as a moderator of the effect of family sexual communication on sexual risk behavior among adolescents in psychiatric care. AIDS & Behavior. 2009;no. 13(5):1012–1020. doi: 10.1007/s10461-008-9495-9. doi: 10.1007/s10461-008-9495-9. [DOI] [PubMed] [Google Scholar]
- Nunn A, Dickman S, Cornwall A, Kwakwa H, Mayer KH, Rana A, Rosengard C. Concurrent sexual partnerships among African American women in Philadelphia: results from a qualitative study. Sexual Health. 2012;no. 9(3):288–296. doi: 10.1071/SH11099. doi: 10.1071/sh11099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OJJDP Juvenile Offenders and Victims: National Report Series Bulletin: Juvenile Arrests 2009. 2011a Available from http://www.ojjdp.gov/pubs/236477.pdf.
- — — — [cited January 31 2013];Statistical Briefing Book. 2011b 2013. Available from http://www.ojjdp.gov/ojstatbb/corrections/qa08211.asp?qaDate=2010.
- Piantadosi S. Clinical Trials: A Methodologic Perspective. John Wiley & Sons, Inc.; New York, NY: 2005. [Google Scholar]
- Robertson Angela R., St. Lawrence Janet, Morse David T., Thomas Connie Baird, Liew Hui, Gresham Kathleen. The “Healthy Teen Girls Project": Comparison of Health Education and STD Risk Reduction Intervention for Incarcerated Adolescent Females. Health Education & Behavior. 2011;no. 38(3):241–250. doi: 10.1177/1090198110372332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar Laura F., Crosby Richard A., Diclemente Ralph J. Exploring the mediating mechanism between gender-based violence and biologically confirmed Chlamydia among detained adolescent girls. Violence Against Women. 2009;no. 15(3):258–275. doi: 10.1177/1077801208330100. doi: 10.1177/1077801208330100. [DOI] [PubMed] [Google Scholar]
- Sales JM, Milhausen RR, DiClemente RJ. A decade in review: building on the experiences of past adolescent STI/HIV interventions to optimise future prevention efforts. Sexually Transmitted Infections. 2006;no. 82(6):431–436. doi: 10.1136/sti.2005.018002. doi: 10.1136/sti.2005.018002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz KF, Grimes DA. Blinding in randomised trials: hiding who got what. Lancet. 2002;no. 359(9307):696. doi: 10.1016/S0140-6736(02)07816-9. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Kochman A, Tarakeshwar N, Neufeld S, Meade CS, Fox AM. Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: reductions in traumatic stress. AIDS & Behavior. 2007;no. 11(1):49–60. doi: 10.1007/s10461-006-9149-8. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Kelly JA, Winett RA, Solomon LJ, Cargill VA, Roffman RA, McAuliffe TL, Heckman TG, Anderson EA, Wagstaff DA, Norman AD, Perry MJ, Crumble DA, Mercer MB. Outcomes of a randomized community-level HIV prevention intervention for women living in 18 low-income housing developments. American Journal of Public Health. 2000;no. 90(1):57–63. doi: 10.2105/ajph.90.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder HN, Sickmund M. Juvenile Offenders and Victims: 2006 National Report. Office of Juvenile Justice and Delinquency Prevention; Pittsburgh P. A.: 2006. [Google Scholar]
- Southern AIDS Coalition . In: Southern States Manifesto: Update 2012. Southern AIDS Coalition, editor. Birmingham, AL: 2012. [Google Scholar]
- Staples-Horne M. Sugar and Spice: Understanding the Health of Incarcerated Girls. In: Braithewaite RL, Ariola KJ, Newkirk C, editors. Health Issues among Incarcerated Women. Rutgers University Press; New Brunswich, NJ: 2006. pp. 67–87. [Google Scholar]
- Teplin Linda A., Abram Karen M., McClelland Gary M., Mericle Amy A., Dulcan Mina K., Washburn Jason J. Psychiatric Disorders of Youth in Detention. Juvenile Justice Bulletin. Office of Juvenile Justice and Delinquency Prevention; 2006. Washington D. C. Office of Juvenile Justice Department of Justice, and Prevention Delinquency. [Google Scholar]
- Tolou-Shams, Marina, Stewart Angela, Fasciano John, Brown Larry K. A review of HIV prevention interventions for juvenile offenders. Journal Of Pediatric Psychology. 2010;no. 35(3):250–261. doi: 10.1093/jpepsy/jsp069. doi: 10.1093/jpepsy/jsp069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Pol B, Ferrero DV, Barrington L. Buck, Hook E, 3rd, Lenderman C, Quinn T, Gaydos CA, Lovchik J, Schachter J, Moncada J, Hall G, Tuohy MJ, Jones RB. Multicenter evaluation of the BDProbeTec ET System for detection of Chlamydia trachomatis and Neisseria gonorrhoeae in urine specimens, female endocervical swabs, and male urethral swabs. J Clin Microbiol. 2001;no. 39(3):1008–16. doi: 10.1128/JCM.39.3.1008-1016.2001. doi: 10.1128/jcm.39.3.1008-1016.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voisin DR, King K, Schneider J, DiClemente RJ, Tan K. Sexual Sensation Seeking, Drug Use and Risky Sex among Detained Youth. JOurnal of AIDS & Clinical Research. 2012;no. S1:1–5. doi: 10.4172/2155-6113.S1-017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voisin DR, Neilands TB, Salazar LF, Crosby R, DiClemente RJ. Pathways to drug and sexual risk behaviors among detained adolescents. Social Work Research. 2008;no. 32(3):147–157. doi: 10.1093/swr/32.3.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood G, DiClemente RJ. Partner influences and gender-related factors associated with noncondom use among young adult. American Journal of Community Psychology. 1998;no. 26(1):29. doi: 10.1023/a:1021830023545. [DOI] [PubMed] [Google Scholar]
- — — — . HIV/AIDS in Women. In: Wingood G, DiClemente RJ, editors. Handbook of Women’s Sexual and Reproductive Health. Kluwer/Plenum Publishing Corporation; New York, NY: 2002. pp. 281–301. [Google Scholar]
- Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV Interventions. Journal Of Acquired Immune Deficiency Syndromes. 2008;no. 47(Suppl 1):S40–S46. doi: 10.1097/QAI.0b013e3181605df1. 1999. [DOI] [PubMed] [Google Scholar]
- Wingood Gina M., Rubtsova Anna, DiClemente Ralph J., Metzger David, Blank Michael. A new paradigm for optimizing HIV intervention synergy: the role of interdependence in integrating HIV prevention interventions. Journal Of Acquired Immune Deficiency Syndromes. 2013;no. 63(Suppl 1):S108–S113. doi: 10.1097/QAI.0b013e318291fff4. 1999. doi: 10.1097/QAI.0b013e318291fff4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman RS, Atwood KA, Cupp PK. Improving the validity of self-reports for sensitive behaviors. In: Crosby RA, DiClemente RJ, Salazar LF, editors. Research Methods in Health Promotion. Jossey-Bass, Inc.; San Francisco: 2006. pp. 260–288. [Google Scholar]