Introduction
The urgent and emergency care services in England’s National Health Service (NHS) are currently the subject of a national review. The existing system, which is experiencing increases in demand, has been described as unaffordable, unsustainable and fragmented.1 In August 2013, the Prime Minister’s Office and Department of Health announced that an additional £500 million would be made available to relieve pressures on accident and emergency (A&E) departments.2 Since then, the National Audit Office and Public Accounts Committee have both published reports on emergency admissions to hospital, focusing on the management of demand and the value gained from public expenditure.3,4 In this article, we briefly review the current roles of A&E departments in England and then describe how the proportion of emergency hospital admissions that occurred via A&E departments increased from 2001–2002 to 2010–2011. We present a conceptual framework for helping to explain this trend and discuss the potential implications for national policy.
The current roles of A&E departments in England
A&E departments collectively perform three main roles in England: they are an alternative to primary care services for first point of contact care; they are acute diagnostic and treatment centres for patients who need immediate treatment; and they are also portals for emergency admission to hospital.
Type 1, or ‘major’, A&E departments provide consultant-led 24-h services with full resuscitation facilities for a wide range of conditions.5 Type 2 A&E departments provide consultant-led services within a single specialty, such as ophthalmology.5 Services conducting other A&E/minor injury activity, either doctor or nurse-led, are classified as type 3 A&E departments, including urgent care centres (UCCs), minor injuries units and walk-in centres.5
Nationally in 2012–2013, patients were recorded as receiving no treatment or advice only in approximately 47% of attendances at A&E departments and no investigation in 41% of attendances.6 A general practitioner (GP) review of a random sample of 629 case notes for patients attending a major A&E department in Oxford, England, concluded that 38–47% of patients could have been managed by a GP.7 To prevent patients with minor injuries and illnesses from contributing to the workload of major A&E departments, some of these services are co-located with a type 3 A&E department. The College of Emergency Medicine has recommended the use of UCCs led by GPs for this function,8 and in some instances commissioners have closed walk-in centres located in the community and opened UCCs co-located with major A&E departments.9 The initial policy intention of introducing walk-in centres into the NHS over a decade ago was to ensure that patients could access urgent care for minor injuries and illnesses at times and locations convenient for them.10 However, the role of type 3 A&E departments in managing demand for major A&E departments now appears to be more pertinent.
Patients were admitted to hospital as an outcome of approximately 21% of A&E attendances in England in 2012–2013,6 accounting for 71% of all emergency admissions in this year.3 The role of A&E departments, particularly major A&E departments, as portals for emergency admission has received much attention, due, in part, to the increased annual number of these admissions and the associated financial cost, estimated to be £12.5 billion in 2012–2013.3
Emergency hospital admissions via A&E departments
The annual age-sex standardised number of emergency admissions per 100,000 population in England increased from 7675 in 2002–2003 to 8988 in 2011–2012 (a 17% increase).11 A proportion of these admissions are for ‘primary care sensitive’ conditions (PCSCs) – conditions for which it has been hypothesised that the risk of emergency admission can be reduced by high-quality primary care. Rates of emergency admissions for PCSCs are commonly used as a measure of health system performance, including in the NHS Outcomes Framework.12 Between 2001–2002 and 2012–2013, the age-standardised rate of emergency admissions for a subset of these conditions also increased, by 26%, from 1278 to 1614 per 100,000 population.13
In the United States, the proportion of emergency admissions in which patients were admitted via an emergency department increased from 0.61 to 0.69 between 2003 and 2009.14 We use the term ‘A&E proportion’ henceforth to denote the proportion of emergency admissions in which patients are admitted via an A&E department. This trend was driven by a 20% increase in the annual number of emergency admissions via an emergency department (15.3 million to 18.4 million) and a 24% decrease in those from a physician’s office or other primary care setting (8.0 million to 6.1 million).14 These results suggest a growing role for emergency departments in acting as portals for emergency admission to hospital. Although there are large differences in the healthcare systems of the United States and England, the trend described is very similar to that observed in England.
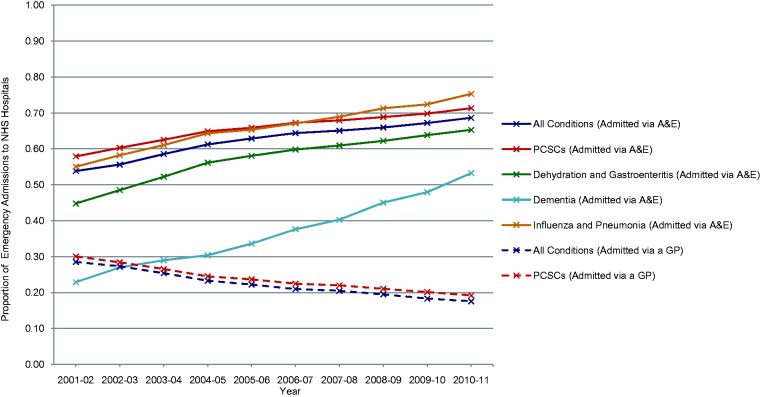
Across all NHS-funded hospitals in England, the A&E proportion increased by 0.15 (0.54 to 0.69; p < 0.001) from 2001–2002 to 2010–2011 (Figure 1). A similar increase, of 0.13 (0.58 to 0.71; p < 0.001), occurred for admissions with a subset of PCSCs12,15 recorded as the primary diagnoses. Particularly large year-on-year increases in the A&E proportion were observed for the PCSCs ‘dehydration and gastroenteritis’ (0.45 to 0.65; p < 0.001), ‘influenza and pneumonia’ (0.55 to 0.75; p < 0.001) and ‘dementia’ (0.23 to 0.53; p < 0.001). The A&E proportion increased, in the range 0.08 to 0.21, for each of the other 18 PCSCs analysed. In contrast, the proportion of emergency admissions in which patients were admitted via a GP decreased by 0.11 for all conditions (0.29 to 0.18; p < 0.001) and for PCSCs (0.30 to 0.19; p < 0.001) from 2001–2002 to 2010–2011. The overall trend is driven by a 72% increase in the annual number of emergency admissions via A&E departments (2.1 million to 3.6 million) and a 17% decrease in those via general practices (1.12 million to 0.93 million).
Figure 1.
Proportion of Emergency Admissions in which Patients were Admitted via A&E, or via a GP, in England, 2001–02 to 2010–11.
Data are from Hospital Episode Statistics (HES), a national administrative database containing details of all admissions to NHS hospitals in England. The primary care sensitive conditions (PCSCs) analysed were: angina; asthma; cellulitis; congestive heart failure; convulsions and epilepsy; chronic obstructive pulmonary disease; dehydration and gastroenteritis; dental conditions; diabetes complications; ear, nose and throat infections; gangrene; hypertension; influenza and pneumonia; iron-deficiency anaemia; nutritional deficiency; other vaccine-preventable diseases; pelvic inflammatory disease; perforated/bleeding ulcer; and pyelonephritis, as defined by Purdy,15 in addition to dementia and atrial fibrillation as defined in the NHS Outcomes Framework.12
These results suggest that the role of A&E departments as portals for emergency admission is growing in England, particularly for several selected PCSCs. Furthermore, the frequency with which GPs directly admit patients appears to be declining.
A conceptual framework for the A&E proportion
The explanation for the increase in the A&E proportion in England is plausibly composed of several interacting components that have contributed to the consistent increase in the number of emergency admissions via A&E departments, the consistent decrease in the number of admissions via general practice, or both (Figure 2).
Figure 2.
A Possible Conceptual Framework for Explaining the Growing Role of A&E Departments as Portals for Emergency Admission.
The arrows represent the movement of patients through time, from one quadrant to another, in a possible conceptual framework to explain the increased proportion of emergency admissions to NHS hospitals via A&E (top left). (A) The clinical need for hospital admission via A&E is increasing due to demographic changes; (B) Patients who would previously have been managed in A&E without admission to hospital are now admitted; (C) Increased failure of management in primary care and outpatient settings that is unexplained by changes in population demographics; (D) Patients who would previously have been admitted via a GP or consultant outpatient clinic are now (recorded as being) admitted via A&E.
The number of emergency admissions via A&E departments is equal to the product of the number of A&E attendances and the percentage of attendances that result in admission. Emergency admissions via major A&E departments accounted for 99% of emergency admissions via A&E departments in 2013–2014 (and 98% in 2004–2005).5 The increase in the percentage of attendances at major A&E departments that resulted in admission, from 21% to 27%,5 between 2004–2005 and 2013–2014 accounted, by itself, for 76% of the increase in admissions via this portal over this period. The number of attendances at major A&E departments increased by 7% (13.3 million to 14.2 million) over the same time frame. There are three main hypotheses that may only explain the increase in the number of emergency admissions via A&E departments.
First, demographic changes in the English population may have resulted in a greater clinical need for emergency admission via A&E departments (A; Figure 2); the age and sex distribution explain 40% of the increase in emergency admission rates between 2004–2005 and 2008–0916 and almost all of the increase in emergency admissions is attributable to those via major A&E departments.3 Second, A&E departments’ thresholds for admitting patients could have lowered, such that patients who would previously have been managed in A&E without admission are now admitted to hospital (B; Figure 2). Its causes could include the practice of more ‘defensive’ medicine, consistent with the observed large increase in short-stay admissions (1.8 million to 2.7 million from 2004–2005 to 2012–13),3 possibly to acute medical units which are variably coded in hospital data. The high burden of service delivery placed on junior A&E doctors8 and overcrowding in A&E departments could also contribute to lowered admission thresholds. Of note, the introduction of ‘Payment by Results,’ the activity-based system used to pay NHS hospitals, for emergency care and the initial 4-h waiting time target did not appear to influence admission from A&E departments at a national level.16,17 Third, a greater clinical need for emergency admission via A&E departments may have occurred due to an increased failure of management in primary care and outpatient settings that is unexplained by changes in population demographics (C; Figure 2).
Neither of the three hypotheses outlined above can plausibly explain the consistent decrease in the annual number of emergency admissions via general practices between 2001–2002 and 2010–2011. This trend is observed despite an estimated 35% increase in the annual number of general practice consultations (225.3 million to 303.9 million) between 2000–2001 and 2008–2009, which exceeds the growth in the English population size.18 If we assume that the percentage of general practice consultations that resulted in the patient being referred to hospital remained the same between 2001–2002 and 2008–2009 (0.5%), an additional 0.5 million admissions via a GP are expected than are observed in 2008–2009. Hence, some patients who would previously have been admitted directly via a general practice are now being, or recorded as being, admitted via A&E instead (D; Figure 2). This may be related, in part, to the growth of acute medicine as a specialty over the study period, accompanied by the establishment of acute medical units within many hospitals to which GPs can directly refer patients. Some hospitals code the activity of acute medical units as hospital admissions, while others do not.3 For the latter group, inpatient admissions from these units may be coded as admissions via an A&E department by some hospitals, and, in addition, acute medical units may prevent a patient’s stay from being recorded as an admission at all in some instances. The number of acute/general medicine consultants increased by approximately 63% from 2002 to 2007, and 92% of hospitals in the United Kingdom admitted acutely unwell patients to acute medical units by 2008.19 In the United States, primary care physicians may have increasingly referred or directed patients to emergency departments rather than arranging a direct hospital referral,14 which could also apply in England. Alternatively, patients could have increasingly self-referred to A&E departments, rather than their general practice, for conditions they perceived as possibly requiring treatment in hospital. This may reflect increased health awareness, increased consumerism and difficulties accessing general practice services in a timely manner.
Each of the hypotheses given above could help to explain the consistent increase in the A&E proportion, across all conditions and specific to PCSCs, throughout the study period. Changes in population demographics, primary care and outpatient management, admission thresholds in emergency departments, pathways to admission after contact with primary care services, and patients’ healthcare-seeking behaviour may be common to both England and the United States and contribute to the similar trends observed.
Gatekeeping in A&E departments
The role of A&E departments as portals for emergency admission is growing, regardless of its explanation. This is despite efforts to reduce A&E attendance rates and national recommendations to support direct admission to acute medical care.20 Consequently, A&E staff now have increasing responsibility as gatekeepers for inpatient care and as care coordinators, which is not reflected in how A&E departments’ activity is measured or reimbursed.
The ‘clinical quality indicators’ currently used to assess A&E departments’ performance include the unplanned re-attendance rate and the percentage of A&E attendances for cellulitis and deep vein thrombosis that result in admission.21 Unplanned re-attendance rates are proposed to reflect the quality of care provided, while cellulitis and deep vein thrombosis are considered largely manageable without hospital admission.21 However, these indicators are not being used consistently by A&E services throughout England,8 and cellulitis and deep vein thrombosis account for only a small proportion of A&E attendances. Furthermore, the majority of A&E departments in England are paid according to a national, activity-based ‘Payment by Results’ tariff8 which is also used to reimburse admitted patient care. Yet the tariff payments for inpatient admissions are significantly greater than those for A&E attendances, and therefore, hospitals stand to financially gain from admitting more patients. In 2012–2013, the Department of Health introduced the ‘Same Day Emergency Care’ tariff which, for a range of clinical scenarios, reimburses hospitals a greater amount for same-day discharges than for inpatient admissions lasting one or more days.22 The College of Emergency Medicine has recommended the extension of this tariff to certain groups of patients in A&E departments to disincentivise ‘inappropriate’ admissions.8
The challenge for A&E departments is also compounded by medical staffing issues, such as low recruitment into higher specialty training and unfilled consultant posts.23 Consequently, junior A&E doctors may lack supervision and training that would otherwise further the skills necessary to perform a gatekeeping function effectively.
Changes to the performance measurement, reimbursement and medical staffing of A&E departments may be insufficient to address their growing role as portals for emergency admission. If so, redesign of the delivery of urgent and emergency care services across patient pathways is an alternative intervention. The most notable example of such redesign has been planned for northwest London.24
A&E service reconfiguration in northwest London
The major A&E departments at four hospitals in northwest London (Charing Cross, Central Middlesex, Hammersmith and Ealing) were to be closed under initial plans, with GP-led UCCs assuming full responsibility for providing urgent care at these sites instead (Box 1).24 The major services at Charing Cross and Ealing Hospitals may now be reconfigured rather than closed. Five other hospitals in the region (Chelsea and Westminster, Hillingdon, Northwick Park, St. Mary’s and West Middlesex) are intended to have co-located UCCs and major A&E departments to which patients can be referred from other sites.24
Box 1.
Reconfiguration of Health Services in Northwest London.
| The Shaping a Healthier Future programme, led by a Joint Committee of Primary Care Trusts, was established in 2011 to determine the most appropriate configuration of health services in northwest London.24 The status quo was not acceptable to the Committee. |
| Inequalities in the quality of care exist, prevention of ill health is inadequate, the local health system is too dependent on hospital services, and hospital trusts could move into financial deficit.24 Consequently, the Committee recommended concentrating A&E resources by having major A&E departments at fewer hospital sites, whilst placing GP-led urgent care centres (UCCs) at each 'local' and 'major' hospital. The UCCs are intended to be accessible 24 hours a day, 7 days a week and have access to X-ray and other diagnostic services. |
| The reconfiguration is expected to increase the financial sustainability of services and improve patient outcomes in A&E. Clinical Commissioning Groups (CCGs) are also anticipated to make significant investments in out-of-hospital services across northwest London. |
UCCs staffed by GPs and emergency nurse practitioners have been operational at Charing Cross and Hammersmith Hospitals since 2009; self-referred patients are unable to access the co-located major A&E departments without first being seen by a GP or nurse in the UCCs. Approximately 13% of self-referred patients visiting these UCCs since October 2009 have been initially redirected to the major A&E departments. In this case, the majority of patients can be dealt with by the GPs and emergency nurse practitioners working in the UCCs. Future research will examine the resulting effect on the number of emergency admissions to hospital.25
The existing evidence on the effect of GPs working directly within major A&E departments, from studies that have used non-randomised or uncontrolled designs to investigate individual departments,26 is inconclusive and inconsistent. The still-unanswered question as to whether GPs are less likely to admit patients than A&E doctors, given the same case-mix, could be addressed through well powered, adjusted comparisons between areas with and without GPs as providers of hospital-based urgent care. Alternatively, patients could be randomised to different entry portals – major A&E or GP-led UCC – in a trial.
Clinical commissioning groups (CCGs) may choose, albeit with a lack of evidence, to commission models of urgent and emergency care services featuring GP-led UCCs, integrated with out-of-hours services, as planned for northwest London. However, the role of GPs in providing urgent care in general practice should also be reviewed, due to the need to implement locally applicable ‘demand management’ strategies that limit the use of hospital services.
Urgent care in general practice
National, cross-sectional associations between access to general practice and emergency admissions for cancer, chronic obstructive pulmonary disease, diabetes complications, heart failure and stroke have previously been reported in England.27–31 In addition, a similar association with rates of self-referred A&E attendances that resulted in the patient being discharged has also been found.32 Assuming that these results are not due to residual confounding, the findings could represent a true effect of access to general practice on demand for hospital-based urgent and emergency care.
The UK Government has recently created a £50 million ‘GP Access Fund’ to support approximately 14% of general practices in opening from 8:00 to 20:00, seven days a week,33 and some practices already receive additional payments for offering appointments outside their core contracted hours of 8:00 to 18:30, Monday to Friday.34 The ‘GP Access Fund’ should be rigorously evaluated to produce evidence capable of informing future policy on access to general practice. If the intervention brings desired results, including those relating to A&E attendances and emergency admissions, it may be appropriate for NHS England to review the funding of primary care and increase the capacity of general practice to deal with patients presenting with acute problems.
Conclusion
The proportion of emergency hospital admissions in which patients were admitted via an A&E department increased markedly in England between 2001–2002 and 2010–2011. The explanation for this trend must account for the consistent increase in the number of admissions via major A&E departments, the consistent decrease in the number via general practices and the similarity between the trends for all conditions and a subset of primary care sensitive conditions. The findings are similar to those in the United States. Policy should address gatekeeping in A&E departments and the provision of urgent care in general practice in response to this challenge. New models of urgent care services that employ GPs in A&E departments as the gatekeepers to specialist urgent care must be evaluated before they are scaled up to avoid further ad hoc service developments.
Declarations
Competing interests
None declared
Funding
This report is independent research supported by the National Institute for Health Research (NIHR) (Doctoral Research Fellowship, Thomas Cowling, DRF-2013-06-142). The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The Department of Primary Care and Public Health at Imperial College London is grateful for support from the Northwest London NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC), the Imperial NIHR Biomedical Research Centre (BRC) and the Imperial Centre for Patient Safety and Service Quality (CPSSQ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethical approval
Not required
Guarantor
TEC
Contributorship
TEC conceived the idea for the article, designed and conducted the analysis and drafted the first version of the manuscript. MAS, DB and AM made substantial contributions to the interpretation of the results and revision of the manuscript for important intellectual content. All authors approved the final version to be published.
Acknowledgements
None
Provenance
Not commissioned; peer-reviewed by Eric Heymann
References
- 1.NHS England. The Evidence Base from the Urgent and Emergency Care Review. 2013. See http://www.england.nhs.uk/wp-content/uploads/2013/06/urg-emerg-care-ev-bse.pdf (last checked 28 August 2014).
- 2.UK Government. Prime Minister Announces £500 Million to Relieve Pressures on A&E. See https://www.gov.uk/government/news/prime-minister-announces-500-million-to-relieve-pressures-on-ae (last checked 28 August 2014).
- 3.National Audit Office. Emergency Admissions to Hospital: Managing the Demand. 2013. See http://www.nao.org.uk/wp-content/uploads/2013/10/10288-001-Emergency-admissions.pdf (last checked 28 August 2014).
- 4.Committee of Public Accounts. Forty-Sixth Report: Emergency Admissions to Hospital. See http://www.publications.parliament.uk/pa/cm201314/cmselect/cmpubacc/885/88502.htm (last checked 28 August 2014).
- 5.NHS England. Weekly A&E SitReps 2013–14. See http://www.england.nhs.uk/statistics/ae-waiting-times-and-activity/weekly-ae-sitreps-2013-14/ (last checked 28 August 2014).
- 6.Health and Social Care Information Centre. Accident and Emergency Attendances in England—2012–13. See http://www.hscic.gov.uk/searchcatalogue?productid=14120&q=Accident+and+Emergency+Attendances+in+England+&sort=Relevance&size=100&page=1#top (last checked 28 August 2014).
- 7.Thompson MIW, Lasserson D, McCann L, Thompson M, Heneghan C. Suitability of emergency department attenders to be assessed in primary care: survey of general practitioner agreement in a random sample of triage records analysed in a service evaluation project. BMJ Open 2013; 3: e003612–e003612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The College of Emergency Medicine. The Drive for Quality—How to Achieve Safe, Sustainable Care in Our Emergency Departments. 2013. See http://secure.collemergencymed.ac.uk/Shop-Floor/Professional%20Standards/Quality%20in%20the%20Emergency%20Department/ (last checked 28 August 2014).
- 9.Monitor. Walk-in Centre Review: Final Report and Recommendations. 2014. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/283778/WalkInCentreFinalReportFeb14.pdf (last checked 2 September 2014).
- 10.Salisbury C, Chalder M, Scott TM, Pope C, Moore L. What is the role of walk-in centres in the NHS? BMJ 2002; 324: 399–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHS Information Centre for Health and Social Care. Dataset: Emergency Hospital Admissions: All Conditions: Indirectly Standardised Rate, All Ages, Annual Trend. See https://indicators.ic.nhs.uk/webview/ (last checked 28 August 2014).
- 12.Department of Health. The NHS Outcomes Framework 2013/14: Technical Appendix. 2012. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/214902/PbR-Guidance-2013-14.pdf (last checked 2 September 2014).
- 13.Blunt I. Trends in Emergency Admissions for Ambulatory Care Sensitive Conditions, 2001 to 2013. London: Nuffield Trust, 2013. See http://www.nuffieldtrust.org.uk/sites/files/nuffield/publication/131010_qualitywatch_focus_preventable_admissions_0.pdf (last checked 28 August 2014).
- 14.Morganti KG, Bauhoff S, Blanchard JC, Abir M, Iyer N, Smith AC, et al. The Evolving Role of Emergency Departments in the United States. 2013. See http://www.rand.org/content/dam/rand/pubs/research_reports/RR200/RR280/RAND_RR280.pdf (last checked 28 August 2014). [PMC free article] [PubMed]
- 15.Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health 2009; 123: 169–173. [DOI] [PubMed] [Google Scholar]
- 16.Blunt I, Bardsley M and Dixon J. Trends in Emergency Admissions in England 2004–09. London: The Nuffield Trust, 2010. See http://www.nuffieldtrust.org.uk/sites/files/nuffield/Trends_in_emergency_admissions_REPORT.pdf (last checked 28 August 2014).
- 17.Weber EJ, Mason S, Freeman JV, Coster J. Implications of England's four-hour target for quality of care and resource use in the emergency department. Ann Emerg Med 2012; 60: 699–706. [DOI] [PubMed] [Google Scholar]
- 18.Health and Social Care Information Centre. Trends in Consultation Rates in General Practice—1995–2009. See http://www.hscic.gov.uk/searchcatalogue?productid=729&q=consultation+gp&topics=1%2fPrimary+care+services%2fGeneral+practice&sort=Most+recent&size=10&page=1 (last checked 28 August 2014).
- 19.Scott I, Vaughan L, Bell D. Effectiveness of acute medical units in hospitals: a systematic review. Int J Qual Health Care 2009; 21: 397–407. [DOI] [PubMed] [Google Scholar]
- 20.Royal College of Physicians. Acute Medical Care. The Right Person, in the Right Setting—First Time. Report of the Acute Medicine Task Force. 2007. See http://www.rcplondon.ac.uk/sites/default/files/documents/acute_medical_care_final_for_web.pdf (last checked 28 August 2014).
- 21.Department of Health. A&E Clinical Quality Indicators. 2010. See http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digitalasset/dh_122892.pdf (last checked 28 August 2014).
- 22.Department of Health. Payment by Results Guidance for 2013–14. 2013. See https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/214902/PbR-Guidance-2013-14.pdf (last checked 2 September 2014).
- 23.Emergency Medicine Taskforce. Interim Report. 2012. See http://secure.collemergencymed.ac.uk/Development/Policy%20and%20Service%20Development/Workforce/ (last checked 28 August 2014).
- 24.NHS North West London. Shaping a Healthier Future: Decision Making Business Case—Executive Summary. 2013. See http://www.healthiernorthwestlondon.nhs.uk/sites/default/files/documents/SaHF%20DMBC%20Executive%20Summary%20%28extract%20from%20Volume%201%29.pdf (last checked 28 August 2014).
- 25.Gnani S, Ramzan F, Ladbrooke T, Millington H, Islam S, Car J, et al. Evaluation of a general practitioner-led urgent care centre in an urban setting: description of service model and plan of analysis. JRSM Short Rep 2013; 4: 2042533313486263. [DOI] [PMC free article] [PubMed]
- 26.Khangura JK, Flodgren G, Perera R, Rowe Brian H, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev 2012; 11: CD002097–CD002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bottle A, Tsang C, Parsons C, Majeed A, Soljak M, Aylin P. Association between patient and general practice characteristics and unplanned first-time admissions for cancer: observational study. Br J Cancer 2012; 107: 1213–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brettell R, Soljak M, Cecil E, Cowie MR, Tuppin P, Majeed A. Reducing heart failure admission rates in England 2004–2011 are not related to changes in primary care quality: national observational study. Eur J Heart Fail 2013; 15: 1335–1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calderon-Larranaga A, Carney L, Soljak M, Bottle A, Partridge M, Bell D, et al. Association of population and primary healthcare factors with hospital admission rates for chronic obstructive pulmonary disease in England: national cross-sectional study. Thorax 2011; 66: 191–196. [DOI] [PubMed] [Google Scholar]
- 30.Calderon-Larranaga A, Soljak M, Cecil E, Valabhji J, Bell D, Prados Torres A, et al. Does higher quality of primary healthcare reduce hospital admissions for diabetes complications? A national observational study. Diabet Med 2014; 31: 657–665. [DOI] [PubMed] [Google Scholar]
- 31.Soljak M, Calderon-Larranaga A, Sharma P, Cecil E, Bell D, Abi-Aad G, et al. Does higher quality primary health care reduce stroke admissions? A national cross-sectional study. Br J Gen Pract 2011; 61: e801–e807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cowling TE, Cecil EV, Soljak MA, Lee JT, Millett C, Majeed A, et al. Access to primary care and visits to emergency departments in England: a cross-sectional, population-based study. PLoS One 2013; 8: e66699–e66699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Department of Health. Millions to Benefit from Improved GP Care. See https://www.gov.uk/government/news/millions-to-benefit-from-improved-gp-care (last checked 28 August 2014).
- 34.NHS Employers. Extended Hours Access Directed Enhanced Service (DES) 2013/14. 2013. See http://www.nhsemployers.org/Aboutus/Publications/Pages/2013_14_extended_hours_DES_guidance.aspx (last checked 2 September 2014).