Abstract
Recent research has documented the unusually high rates of incarcerated women’s serious mental illness (SMI) and substance use disorders (SUD). Complicating these high rates is the high comorbidity of SMI with SUD and trauma histories. Yet, incarcerated women have significantly less access to treatment and health services while incarcerated than men. We used data from a multi-site, multi-method project funded by the Bureau of Justice Assistance (2011–2012) to determine the risk profile of women in jail (n=491) with a current co-occurring SMI (i.e., major depressive disorder, bipolar disorder, schizophrenia spectrum disorder)and SUD (i.e., abuse, dependence). The study spanned multiple geographic regions, and structured diagnostic interviews were used to understand better the women that comprised this vulnerable population. One-in-five of the women had a current co-occurring disorder (CCOD). The findings revealed that significantly more women with a CCOD had been exposed to violence and were exposed to drugs at a younger age. Further, about one-third of women with a CCOD had received no treatment from a health care professional in the past year, demonstrating a substantial unmet need. We conclude that investing in mental and behavioral health care in jails is critical to the health and safety of women as well as the communities to which they return.
Keywords: serious mental illness, substance use disorders, co-occurring disorders, women in jail
The criminalization of mental illness and the mass incarceration resulting from the War on Drugs have converged, with incarcerated populations having significantly higher prevalence of serious mental illness (SMI) and substance use disorders (SUD) than the general population. Some argue that these factors have created a “revolving-door” phenomenon such that many mentally ill people move continuously between homelessness and the criminal legal system (Baillargeon, Binswanger, Penn, Williams, & Murray, 2009). A 2006 Bureau of Justice Statistics report shows that half of inmates have at least one mental health problem(Glaze & James, 2006). Recent research has documented the unusually high rates of incarcerated women’s SMI(Binswanger et al., 2010; DeHart, Lynch, Belknap, Dass-Brailsford, & Green, 2013; Lynch et al., in press; Steadman, Osher, Clark Robbins, Case, & Samuels, 2009) and SUD(Abram, Teplin, & McClelland, 2003; Daniel, Robins, Reid, & Wilfley, 1988; Proctor, 2012). Complicating these high rates is the high comorbidity of SMI with SUD and trauma histories (Abram, et al., 2003; Butler, India, Allnutt, & Mamoon, 2011; Lynch, Fritch, & Heath, 2012). In fact, incarcerated women have worse health than incarcerated men across a broad range of health outcomes (Arriola, Braithwaite, & Newkirk, 2006; Marcus-Medoza, 2010). Yet, incarcerated women have significantly less access to treatment and health services while incarcerated (Eliason, Taylor, & Williams, 2004). Women represent the fastest growing offender segment of the U.S. criminal legal system (PEW Center, 2008), increasing 757% between 1977 and 2004, nearly twice rate of men for this same time period (Frost, Greene, & Pranis, 2006). Thus, correctional facilities house an unprecedented number of women with specific and complex mental health treatment needs.
Given the number of people cycled through US jails every year – 11.8 million in 2011 (Minton, 2012)– jails can be seen as a setting to identify mental health problems among persons who are likely underserved in their community. Providing a diagnosis and coordinating for transitions in care upon release from jail can be extremely beneficial for community public health (Binswanger, Redmond, Steiner, & Hicks, 2011) and in reducing recidivism (Baillargeon, et al., 2009). This is especially important given the high risk of drug-related death, suicide, and homicide during the two weeks after release from jail (Lim et al., 2012).
The current study sought to determine the risk profile of women in jail with current co-occurring SMI and SUD, designated as CCOD (current co-occurring disorders). The participants were from multiple geographic regions, and data were obtained using structured diagnostic interviews to understand better the women that comprised this vulnerable population. Specifically, we assessed differences in demographic and background characteristics, incarceration history, victimization, and family risk exposure. Additionally, we investigated the patterns of treatment and service utilization for these women to document unmet needs that could be addressed within jail settings and, more importantly, in community settings upon release from jail. This study is significant because research using structured diagnostic interviews for incarcerated women has been limited to facilities in one geographic area, predominantly the Northeast (Green, Miranda, Daroowalla, & Siddique, 2005; Steadman, et al., 2009; Trestman, Ford, Zhang, & Wiesbrock, 2007).
Methods
Study Design
The data for this study were collected from 2011 to 2012 as part of a multi-site, multi-method project funded by the Bureau of Justice Assistance. This project was designed to examine the prevalence of serious mental illness in women in jail as well as pathways to jail for women. Incarcerated women were randomly selected for participation (n = 491) from nine local county jails in four regions: Idaho (n = 110), Colorado (n = 203), South Carolina (n = 84), and Maryland/Virginia (n = 93). These regions were chosen because they represented varied rural and urban settings across the United States. Approximately 43 percent of the women were housed in jails in rural or low population areas. Institutional review board approval was obtained for the study protocol from a university in each region, and written and signed informed consent was obtained from all study participants. Women were randomly selected for participation from rosters provided by corrections staff. The rosters were constantly updated, and women who declined to participate were removed from the roster. A total of 142 out of 633 women (22%) declined to participate. All currently incarcerated women across regions were eligible to participate unless they were experiencing acute stress. Ten women were excluded from the study due to violent threats and acute distress at the time of the invitation to interview. Eligibility criteria were further constrained in one of the four regions due to IRB restrictions prohibiting interviews with pre-sentence offenders charged with homicide, first degree assault, or felony sex charges. This resulted in the exclusion of five additional potential participants. The overall response rate for the study was 76 percent.
Once informed consent was obtained, a structured diagnostic interview was administered in a private room at the jail. The structured interview lasted on average two hours and collected socio-demographic information as well as histories of incarceration, mental health, substance use, and treatment utilization. Women’s compensation varied by jail. Depending on local jail policies, participants were compensated with $10 deposited to their commissary account, were provided with snacks, or the jail’s general fund was provided with incentive funds (e.g., to purchase self-help books for the women).
Measures
Information was collected on women’s socio-demographic background. Standard measures included age (continuous), marital status (0 not married, 1 married), level of education (0 = less than high school, 1 = at least high school), and employment prior to incarceration (0 = unemployed/part-time/occasional, 1 = full-time). We also assessed whether the participant had a minor child (0 no, 1 yes), whether she was raised in foster care or by someone else because her parents could no longer care for her (0 no, 1 yes), and whether she had ever received public assistance (0 no, 1 yes).
Incarceration history was assessed by examining the total number of self-report past convictions (continuous) and the type of offense for which she was currently incarcerated. These offenses were dummy coded and included violent offense, drug offense, property offense, prostitution offense, and “other” offense. Other offense was comprised mostly of probation violations or parole revocations.
Because of our focus on traumatic experiences and pathways of women offenders, we expanded the assessment of trauma exposure by including items from the Life Stressor Checklist- Revised (Wolfe & Kimerling, 1997) and the Turner and colleagues’ measure of non-victimization adversity (Turner, Finkelhor, & Ormrod, 2006). Violent victimization as assessed in this study was derived from items from the Life Stressor Checklist-Revised (LSC-R)(Wolfe & Kimerling, 1997). Dummy variables for violent victimization across three domains were included. Specifically, physical abuse by a family member was characterized by whether the participant was ever “abused or physically attacked (not sexually) by a family member (for example, a parent, step-parent, or other relative, hit, slapped, choked, burned, or beat you up)?” or the participant ever saw “violence between family members (for example, hitting, kicking, slapping, punching)?” Intimate partner violence was assessed as ever being “abused or physically attacked (not sexually) by a person you were dating or in a relationship with (for example, a partner, boyfriend, or husband, hit, slapped, choked, burned, or beat you up).” Finally, rape/sexual assault was also assessed for any time in the life course, including child sexual abuse and rape/sexual assault as an adult using adapted LSC-R items (Wolfe & Kimerling, 1997). Specifically, women were asked whether they were ever “touched or made to touch someone else in a sexual way because he/she forced you in some way, drugged you, or threatened to harm you if you didn’t,” and whether she ever had “sex (oral, anal, genital) when you didn’t want to because someone forced you in some way, drugged you, or threatened to hurt you if you didn’t.”
Family risk exposure was represented by four dummy variables: family member used drugs, family member had been incarcerated, parent or guardian gave her drugs before the age of 16, and parent or guardian gave her alcohol before the age of 16 years. These items were adapted from Turner and colleagues’ (2006) measure of non-victimization adversity. Specifically, women were asked “Has there been a time that a family member drank or used drugs so often that it caused problems?”, “Was a close family member ever sent to jail?”, “Before the age of 16, was there ever a time that your parent or caregiver gave you alcohol?”, and “Before the age of 16, was there ever a time that your parent or caregiver gave you illegal drugs to use?”
The WHO CIDI was used to assess whether the women in this study met the DSM-IV diagnostic criteria for having a current (past year) SMI and or SUD. The WHO CIDI is a comprehensive structured interview designed for use by trained lay interviewers for the assessment of mental disorders as defined by and meeting the criteria of the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th Edition). SMIs included major depressive disorder, bipolar disorder, and or schizophrenia spectrum disorder (schizophrenia, schizoaffective disorder, delusional disorder, or brief psychotic disorder). SUDs included alcohol abuse, alcohol dependence, drug abuse, and or drug dependence. Women had a current co-occurring disorder (CCOD) if they met the criteria for any SMI and any SUD (0 no, 1 yes) in the past year.
Standardized questions about treatment access were embedded into the CIDI. If women met the criteria for having a SMI or SUD, they were asked about their treatment history. For the current study, we assessed whether women with a CCOD have received counseling by a professional for SMI within the past 12 months, have received prescription medication for SMI within the past 12 months, have received any individual treatment (e.g., counseling) by a professional for SUD within the past 12 months, and or have received any treatment from a self-help group (e.g., AA, NA) for SUD in the past 12 months. It is important to note that we did not differentiate between treatment received while incarcerated or prior to her current incarceration.
Analysis
Descriptive statistics were calculated for all study measures. The chi-square and t-test were used to test the differences among women with and without co-occurring disorders. A multivariate logistic regression model examined the association among having a CCOD (current co-occurring SMI and SUD) and incarceration history, victimization history, and family risk exposure controlling for background characteristics. In other words, the study was designed to determine which factors were most related to having a current CCOD among women in jail. Potential confounding among covariates was examined using Pearson’s correlation. However, all study variables were retained in the multivariate analysis due to the theoretical significance in their association with CCODs or because they were important demographic controls (e.g., age and race/ethnicity). Patterns of missing data were observed, and multiple imputation was used to estimate missing values and generate 20 datasets (StataCorp, 2009) for use in running regression models. Robust standard errors were calculated to account for the clustered nature of the data and model fit was assessed using a model F test. Additional descriptive statistics characterized the treatment needs for women with co-occurring disorders.
Findings
Twenty percent of women met the criteria for having a CCOD. Overall, 32 percent of women had a current SMI, and 53 percent of women had a current SUD (not shown in table). Specifically, the frequency for women meeting the criteria for different SUD was 17 percent for alcohol dependence, 9 percent for alcohol abuse, 33 percent for drug dependence, and 5 percent for drug abuse. The frequency for women meeting the criteria for different SMI was 22 percent for major depressive disorder, 8 percent for bipolar disorder, and 4 percent for schizophrenia spectrum disorder.
The average age of participants was 35 years, and this did not differ by having a CCOD (Table 1). Thirty-seven percent identified as non-Hispanic white, 37 percent as non-Hispanic black, 15 percent as Hispanic, and 10 percent as other. No differences were observed in racial/ethnic distributions by CCOD status. Overall, 17 percent of the women were currently married, 70 percent had at least a high school education including a GED, and 33 percent were employed full-time prior to being incarcerated. Women with CODD were significantly more likely to have a high school education (89.1% vs. 67.1%, p<0.001). About half of the women had a child under the age of 18 years. Thirty-six percent were raised in foster care, and 55 percent had received public assistance (e.g., welfare, food stamps) at some point in their lives.
Table 1.
Characteristics of Women in Jail with and without Co-occurring SMI and SUD
| Total (n=490) | Co-occurring Disorder (n=104) | No Co-occurring Disorder (n=386) | p | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Demographic & Background Characteristics | |||||||
| Agea | 34.8 (10.6) | 35.6 (10.8) | 34.5 (10.6) | ||||
| Non-Hispanic White | 183 | 37.4% | 43 | 41.4% | 140 | 36.3% | |
| Non-Hispanic Black | 183 | 37.4% | 34 | 32.7% | 149 | 38.6% | |
| Hispanic | 74 | 15.1% | 13 | 12.5% | 61 | 15.8% | |
| Other Race | 50 | 10.2% | 14 | 13.5% | 36 | 9.3% | |
| Married | 82 | 17.0% | 23 | 22.6% | 59 | 15.5% | |
| High School Education | 343 | 70.0% | 84 | 80.8% | 259 | 67.1% | ** |
| Full-time Employment | 162 | 33.1% | 30 | 28.9% | 132 | 34.2% | |
| Child Under 18 | 270 | 55.3% | 56 | 54.4% | 214 | 55.6% | |
| Raised in Foster Care | 172 | 35.8% | 39 | 38.2% | 133 | 35.2% | |
| Received Public Assistance | 257 | 54.6% | 60 | 59.4% | 197 | 53.2% | |
| Incarceration History | |||||||
| Number of Convictionsa | 2.84 (3.08) | 4.08 (3.16) | 2.51 (2.97) | *** | |||
| Incarcerated for Violent Offense | 77 | 15.7% | 25 | 24.0% | 52 | 13.5% | ** |
| Incarcarated for Drug Offense | 100 | 20.4% | 22 | 21.2% | 78 | 20.2% | |
| Incarcerated for Property Offense | 63 | 12.9% | 8 | 7.7% | 55 | 14.3% | |
| Incarcerated for Prostitution Offense | 18 | 6.7% | 5 | 4.8% | 13 | 3.4% | |
| Incarcerated for Other Offense | 228 | 46.5% | 44 | 42.3% | 184 | 47.7% | |
| Victimization | |||||||
| Physical Abuse by Family Member | 359 | 75.4% | 90 | 87.4% | 269 | 72.1% | *** |
| Intimate Partner Violence | 336 | 69.6% | 80 | 77.7% | 256 | 67.4% | * |
| Sexual Assault/Rape | 292 | 61.9% | 83 | 81.4% | 209 | 56.5% | *** |
| Family Exposure | |||||||
| Family Member Used Drugs | 299 | 62.2% | 75 | 72.1% | 224 | 59.4% | * |
| Family Member Incarcerated | 347 | 72.3% | 75 | 73.5% | 272 | 72.0% | |
| Parent Gave Drugs Before 16 | 65 | 13.5% | 22 | 21.2% | 43 | 11.4% | ** |
| Parent Gave Alcohol Before 16 | 149 | 30.9% | 39 | 37.5% | 110 | 29.0% | |
p<0.05;
p<0.01;
p<0.001
chi-square test;
t-test
Women were most likely to be incarcerated for an “other” offense (46.5%) followed by a drug offense (20.4%), violent offense (15.7%), property offense (12.9%), and prostitution offense (6.7%). Women with a CCOD (current co-occurring SMI and substance use disorder) differed from women without a CCOD with regard to incarceration history. Women with a CCOD reported a significantly higher number of previous convictions (4.08 vs. 2.51, p<0.001) and were also more likely to be currently incarcerated for violent offense (24.0% vs. 13.5%, p<.001). Women did not differ with respect to being currently incarcerated for a drug offense, prostitution offense, or other offense.
These women reported high levels of victimization. Specifically, 75 percent reported experiencing physical abuse by a family member, 70 percent reported experiencing intimate partner violence, and 62 percent reported experiencing sexual assault/rape. Women with a CCOD were significantly more likely to report experiencing all three types of victimization: physical abuse by a family member (87.4% vs. 72.1%, p<0.001), intimate partner violence (77.7% vs. 76.4%, p<0.05), and sexual assault/rape (81.4% vs. 56.5%, p<0.001). Thus, nine in ten women with a CCOD had experienced physical abuse by a family member, and eight in ten women with a CCOD had experienced intimate partner violence and sexual assault/rape. Women without a CCOD reported rates of seven in ten for physical abuse by a family member and intimate partner violence and six in ten for sexual assault/rape.
Women also reported a high level of exposure to family risks. Specifically, 62 percent had a family member use drugs while growing up, 72 percent had a family member incarcerated, 14 percent had a parent give them drugs while growing up, and 31 percent had a parent give them alcohol while growing up. Women with a CCOD are significantly more likely to have had a family member use drugs while growing up (72.1% vs. 59.4%, p<0.001) and have a parent give them drugs (21.2% vs. 11.4%, p<0.01) or alcohol (37.5% vs. 29.0%, P<0.10) before the age of 16.
In the fully adjusted multiple logistic regression model, the background characteristics that remained significant were high school education and full-time employment (Table 2). Specifically, women with a CCOD were more than twice as likely to have at least a high school education (Odds Ratio[OR] = 2.18; 95% Confidence Interval[CI] = 1.71, 2.77; p<0.001) and had 20 percent reduced odds of working full-time prior to incarceration (OR = 0.79; 95% CI = 0.62, 0.99; p<0.01). Full-time employment was not statistically significant in the bivariate analysis indicating a suppression effect which may have been due to the strong association of education with having a CCOD and the strong correlation between employment and education. All of the incarceration history variables were statistically significant. The odds that a woman with a CCOD reported a greater number of previous convictions was significant with OR = 1.14 (95% CI = 1.01, 1.28; p<0.05). Compared to violent offenses, women with a CCOD had reduced significantly odds of being incarcerated for a drug offense (OR = 0.56; 95% CI = 0.32, 0.98, p<0.05), property offense (OR = 0.34; 95% CI = 0.15, 0.75; p<0.01), prostitution offense (OR = 0.61; 95% CI = 0.47, 0.80; p<0.001), and other offense (OR = 0.43; 95% CI = 0.26, 0.70; p<0.01). In other words, women with a CCOD had significantly higher odds of being incarcerated for a violent offense than for any other offense. Women with a CCOD were more than 2.5 times as likely to report having been sexually assaulted or raped in their lifetime compared to those women without a CCOD. Finally, none of the family risk exposure variables remained significant in the multivariable model.
Table 2.
Odds ratios from regressing co-occurring disorder on background characteristics, incarceration history, victimization, and family exposure (n=491)
| OR | 95% CI | p | |
|---|---|---|---|
| Background Characteristics | |||
| Age | 1.00 | 0.97, 1.03 | |
| Race (compared to White) | |||
| Non-Hispanic Black | 0.93 | 0.44, 1.98 | |
| Hispanic | 0.75 | 0.48, 1.16 | |
| Other Race | 1.13 | 0.92, 1.39 | |
| Married | 1.30 | 0.88, 1.93 | |
| High School Education | 2.18 | 1.71, 2.77 | *** |
| Full-time Employment | 0.79 | 0.62, 0.99 | * |
| Child Under 18 | 0.88 | 0.61, 1.28 | |
| Raised in Foster Care | 0.67 | 0.39, 1.16 | |
| Received Public Assistance | 1.27 | 0.81, 1.98 | |
| Incarceration History | |||
| Number of Convictions | 1.14 | 1.01, 1.28 | * |
| Offense (compared to Violent) | |||
| Incarcarated for Drug Offense | 0.56 | 0.32, 0.98 | * |
| Incarcerated for Property Offense | 0.34 | 0.15, 0.75 | ** |
| Incarcerated for Prostitution Offense | 0.61 | 0.47, 0.80 | *** |
| Incarcerated for Other Offense | 0.43 | 0.26, 0.70 | ** |
| Victimization | |||
| Physical Abuse by Family Member | 1.89 | 0.58, 6.08 | |
| Intimate Partner Violence | 1.00 | 0.75, 1.32 | |
| Sexual Assault/Rape | 2.63 | 1.44, 4.83 | ** |
| Family Exposure | |||
| Family Member Used Drugs | 1.24 | 0.61, 2.51 | |
| Family Member Incarcerated | 0.69 | 0.44, 1.08 | |
| Parent Gave Drugs Before 16 | 1.44 | 0.86, 2.41 | |
| Parent Gave Alcohol Before 16 | 0.93 | 0.64, 1.34 | |
p<0.10;
p<0.05;
p<0.01;
p<0.001
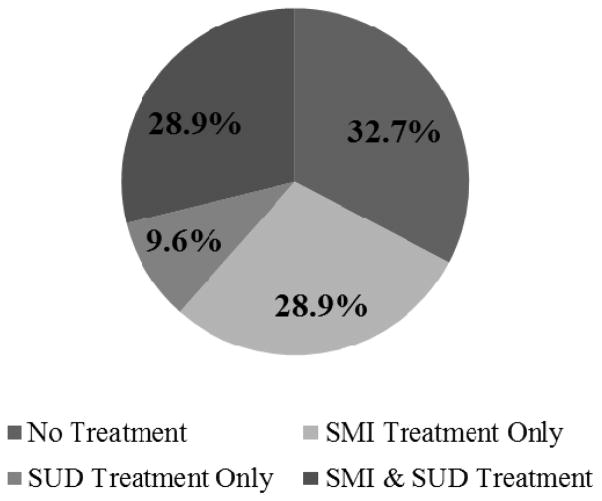
About one-third of women with a CCOD (current co-occurring SMI and substance use disorders) during the past year received no treatment for either their SMI or SUD (Figure 1). Twenty-nine percent of women received treatment for SMI only, and 29 percent received treatment for both SMI and SUD. Finally, only 10 percent of women received treatment for SUD only. A total of 58 percent of women reported received counseling for SMI from a professional; 57 percent of women were prescribed a medication for SMI; 39 percent of women received counseling for SUD from a professional, and 56 percent of women attended a self-help group (Table 3).
Figure 1.
Treatment Utilization among Women in Jail with Co-occurring SMI & SUD n=104
Table 3.
Types of Treatment Services Used by Women in Jail with Co-occurring SMI & SUD (n=104)
| n | % | |
|---|---|---|
| SMI Counseling | 60 | 57.7% |
| SMI Medication | 59 | 56.7% |
| SUD Counseling | 40 | 38.5% |
| SUD Group | 58 | 55.8% |
Women who reported experiencing violent victimization represented the most vulnerable subgroup of women in jail. A total of 104 women met the diagnostic criteria for a CCOD. Of those 104 women, 90 experienced physical abuse by a family member (86.5%), 80 experienced intimate partner violence (76.9%), and 83 experienced sexual assault/rape (79.8%). An overwhelming 6 out of 10 women with a CCOD experienced all three types of victimization and thus are likely to have complex treatment needs (n=62). However, rates of receiving both SMI and SUD treatment were low. Less than one-third of women with a CCOD that experienced victimization received dual treatment in the past year for SMI and SUD, and about two-thirds of women with a CCOD that experienced victimization received any form of treatment in the past year (Table 4).
Table 4.
Types of Victimization and Treatment among Women in Jail with Co-occurring SMI & SUD (n=104)
| n | % Receiving Both SMI & SUD Treatment | % Receiving Any SMI & SUD Treatment | |
|---|---|---|---|
| Types of Victimization | |||
| Physical Abuse by Family Member | 90 | 28.9% | 65.6% |
| Intimate Partner Violence | 80 | 31.3% | 66.3% |
| Sexual Assault/Rape | 83 | 30.1% | 71.1% |
| Experienced All 3 Victimizations | 62 | 29.0% | 66.1% |
Discussion
The risk factors for crime are the same for persons with serious mental illness and for those without (Andrews & Bonta, 2006; Epperson et al., 2011)including antisocial behaviors; attitudes and personality patterns; poor school and work performance; estrangement from family members; substance use disorders; and a lack of prosocial recreational pursuits. In other words, for persons with SMI, “multiple morbidities are the expectation, not the exception” (Lurigio, 2012:7). Nonetheless, the current study identified aspecific risk profile for women in jail with CCOD as well as a clear need for treatment services that target co-occurring substance use and serious mental illness. Although almost a third (29%) of women with a CCOD had received treatment for both SMI and SUD, it is critical to note that another one-third had received no treatment from a doctor or health care professional in the past year. Similarly, among women with a CCOD that reported having experienced severe victimization including physical abuse by a family member, intimate partner violence, and sexual assault/trauma (62 women, 13% of the total sample), 29 percent reported receiving treatment for both SMI and SUD.
Several limitations should be considered when interpreting the study findings. First, recall bias may have been an issue for women when recounting childhood events. However, previous research has documented good discriminant validity and predictive efficiency in adult reporting of childhood trauma, although, underreporting is an issue (Widom & Morris, 1997; Widom & Shepard, 1996). Second, this study was limited in its examination of treatment for women with CCOD because of the small sample size of this subgroup (n=104). The overall small sample size (n=491) may also have resulted in inadequate statistical power to detect some associations of meaningful magnitude as statistically significant. A larger sample was needed to evaluate the factors associated with using treatment. Relatedly, the sample may not have been representative of all women in jail because of the study’s restrictions to just four regions. Third, we did not identify where treatment was received. This is an important limitation of the study because it has consequences for jail treatment programs. Nonetheless, we were still able to identify unmet needs among women in jail with CCOD who reported experiencing high levels of violent victimization. Finally, a previous study with these data identified some significant differences in the prevalence of serious mental illness across regions (Lynch, DeHart, Belknap, & Green, Dass-Brailsford, Johnson, & Whalley, in press), consistent with regional differences in national rates of mental illness (Substance Abuse and Mental Health Services Administration, 2011). To address this issue, robust standard errors were estimated to adjust for the clustered nature of the data.
Despite these limitations, it was clear that substantial numbers of incarcerated women in our sample had co-occurring serious mental illness and substance use problems. One in five women in jail in this multi-site study (20%) met the DSM-IV criteria for having both a current serious mental illness and a current substance use disorder. Women in jail in our sample who had a CCOD had been exposed to significantly higher levels of violence than incarcerated women without CCOD in our sample. Eighty-seven percent of these women reported having experienced physical abuse by a family member, while 81 percent reported having experienced sexual assault, and 78 percent reported having experienced intimate partner violence compared to 72 percent, 57 percent, and 67 percent, respectively, for women without a CCOD. Moreover, women in jail with a CCOD in our sample were more likely to be incarcerated for a violent offense than any other offense. These women were also exposed to drugs at a young age:21 percent of women in jail with a CCOD were given drugs by their parent prior to their 16th birthday compared to 11 percent of non-CCOD women, and 72 percent had a family member that had used drugs compared to 59 percent of non-CCOD women. Given the extent of these traumatic and adverse events among a racially/ethnically and regionally diverse sample of women in jail, the findings of this study strongly suggest an unmet need for women with a CCOD.
Inmates with CCOD can be difficult to supervise because they are more vulnerable to stressors and can be impulsive or unpredictable; the coordination of services can be difficult and costly; and not all jurisdictions offer services (Matz, 2012). Many who work in the criminal legal system are not equipped to deal with mental illness. Therefore, it is not surprising that the criminal legal system tends to exacerbate mental illness (Slate, 2003). Research has shown that integrated care is most effective in reducing SMI and SUD rather than treating only one condition (Drake, Mueser, Brunette, & McHugo, 2004). Research has also documented the need for trauma-informed care for women with SUD (Elliot, Bjelajac, Fallot, Markoff, & Grover Reed, 2005). Unfortunately, the treatment offered in correctional settings may be inconsistent and challenging (Chandler, Peters, Field, & Juliano-Bult, 2004; Teplin, Abram, & McClelland, 1997). Treatment providers may be especially hesitant to begin treatment for those inmates who are serving short sentences or have yet to be convicted. One alternative may be jail diversion programs in which those committing low-level offenses and who have SMI or SUD are diverted from the criminal legal system into treatment. Research evaluating these programs suggests that jail diversion reduces time spent in jail without increasing the public safety risk, while linking participants to community-based services (Steadman & Naples, 2005). Nonetheless, identifying the risk profile and treatment needs for women in jail is imperative since these women will most likely be released back into their communities.
The female midyear population in local jails on June 30, 2011 was 93,300 or 12.6 percent of the jailed population (Minton 2012). In total, local jails admitted almost 11.8 million persons during the 12 months ending midyear 2011. Given that incarcerated persons are guaranteed the right to health care, jails comprise an important space for identification of disorders and for providing treatment and other services for some of the most vulnerable segments of the U.S. population. We echo Lurigio (2012) in saying that proving mental health treatment to criminally involved persons with CCOD is a moral, ethical, and legal obligation, and the right and humane thing to do. However, it is important that treatment services extend into the community context through jail diversion programs and case management that coordinates the transition of care to community service providers. Additionally, treatment interventions must consider the trauma and family histories of women with co-occurring disorders. Investing in mental and behavioral health care in jails is critical for the health and safety of women as well as the communities to which they return.
Acknowledgments
This project was supported by Grant 2010-DB-BX-K048 awarded by the Bureau of Justice Assistance, Office of Justice Programs, United States Department of Justice. Points of view in this document are those of the authors and do not necessarily represent the official position or policies of the United States Department of Justice.
Contributor Information
Kathryn M. Nowotny, University of Colorado at Boulder.
Joanne Belknap, University of Colorado at Boulder.
Shannon Lynch, Idaho State University.
Dana DeHart, University of South Carolina.
References
- Abram KM, Teplin LA, McClelland GM. Comorbidity of Severe Psychiatric Disorders and Substance Use Disorders Among Women in Jail. The American Journal of Psychiatry. 2003;160(5):1007–1010. doi: 10.1176/appi.ajp.160.5.1007. [DOI] [PubMed] [Google Scholar]
- Andrews D, Bonta J. The psychology of criminal conduct. 4. Newark, NJ: Anderson Publishing; 2006. [Google Scholar]
- Arriola KJ, Braithwaite RL, Newkirk C. An Overview of Incarcerated Women’s Health. In: Arriola KJ, Braithwaite RL, Newkirk C, editors. Health Issues Among Incarcerated Women. Bewbrunswick, NJ: Rutgers University Press; 2006. pp. 3–17. [Google Scholar]
- Baillargeon J, Binswanger IA, Penn JV, Williams BA, Murray OJ. Psychiatric Disorders and Repeat Incarcerations: The Revolving Prison Door. American Journal of Psychiatry. 2009;166(1):103–109. doi: 10.1176/appi.ajp.2008.08030416. [DOI] [PubMed] [Google Scholar]
- Binswanger IA, Merrill JO, Krueger PM, White MC, Booth RE, Elmore JG. Gender Differences in Chronic Medical, Psychiatric, and Substance-Dependence Disorders Among Jail Inmates. American Journal of Public Health. 2010;100(3):476–482. doi: 10.2105/AJPH.2008.149591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binswanger IA, Redmond N, Steiner JF, Hicks LS. Health Disparities and the Criminal Justice System: An Agenda for Further Research and Action. Jounral of Urban Health. 2011;89(1):98–107. doi: 10.1007/s11524-011-9614-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler T, India D, Allnutt S, Mamoon H. Co-occurring mental illness and substance use disorder among Australian prisoners. Drug and Alcohol Review. 2011;30(2):188–194. doi: 10.1111/j.1465-3362.2010.00216.x. [DOI] [PubMed] [Google Scholar]
- Chandler RK, Peters RH, Field G, Juliano-Bult D. Challenges in implementing evidence-based treatment practices for co-occurring disorders in the criminal justice system. Behavioral Sciences & the Law. 2004;22(4):431–448. doi: 10.1002/bsl.598. [DOI] [PubMed] [Google Scholar]
- Daniel AE, Robins AJ, Reid JC, Wilfley DE. Lifetime and Six-Month Prevalence of Psychiatric Disorders among Sentences Female Offenders. Journal of the American Academy of Psychiatry and the Law Online. 1988;16(4):333–342. [PubMed] [Google Scholar]
- DeHart D, Lynch S, Belknap J, Dass-Brailsford P, Green B. Life-history models of female offending: The role of serious mental illness and trauma in women’s pathwats to jail. Psychology of Women Quarterly 2013 [Google Scholar]
- Drake RE, Mueser KT, Brunette MF, McHugo GJ. A Review of Treatments for People with Severe Mental llnesses and Co-Occurring Substance Use Disorders. Psychiatric Rehabilitation Journal. 2004;27(4):360–374. doi: 10.2975/27.2004.360.374. [DOI] [PubMed] [Google Scholar]
- Eliason MJ, Taylor JY, Williams R. Physical health of women in prison. Journal of Correctional Health. 2004;7:175–203. [Google Scholar]
- Elliot DE, Bjelajac P, Fallot RD, Markoff LS, Grover Reed B. Trauma-informed or trauma-denied: Principles and implementation of trauma-informed services for women. Journal of Community Psychology. 2005;33(4):461–477. [Google Scholar]
- Epperson M, Wolff N, Morgan R, Fisher W, Frueh BC, Huening J. The next generation of behavioral health and criminal justice interventions: improving outcomes by improving interventions. New Brunswick, NJ: Rutgers University; 2011. [Google Scholar]
- Frost NA, Greene J, Pranis K. Hard hit: The growth in the imprisonment of women, 1977–2004. 2006. [Google Scholar]
- Glaze LE, James DJ. Mental Health Problems of Prison and Jail Inmates. Washington DC: Bureau of Justice Statistics; 2006. [Google Scholar]
- Green BL, Miranda J, Daroowalla A, Siddique J. Trauma Exposure, Mental Health Functioning, and Program Needs of Women in Jail. Crime & Delinquency. 2005;51:133–151. [Google Scholar]
- Lim S, Levanon Seligson A, Parvez FM, Luther CW, Mavinkurve MP, Binswanger IA, et al. Risks of Drug-Related Death, Suicide, and Homicide During the Immediate Post-Release Period Among People Released From New York City Jails, 2001–2005. American Journal of Epidemiology. 2012;175(6):519–526. doi: 10.1093/aje/kwr327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurigio AJ. Responding to the needs of people with mental illness in the criminal justice system: an area ripe for research and community partnerships. Journal of Crime and Justice. 2012;35(1):1–12. [Google Scholar]
- Lynch S, DeHart D, Belknap J, Green B. Pathways Project-Research Factsheet: Mental Health & Trauma among Women in Jails. Pocatello, ID: Idaho State University; 2012. [Google Scholar]
- Lynch S, DeHart D, Belknap J, Green B, Dass-Brailsford P, Johnson KJ, et al. A multi-site study of the prevalence of serious mental illness, PTSD, and substance use disorders in women in jail. Psychiatric Services. doi: 10.1176/appi.ps.201300172. (in press) [DOI] [PubMed] [Google Scholar]
- Lynch SM, Fritch A, Heath NM. Looking Beneath the Surface: The Nature of Incarcerated Women’s Experiences of Interpersonal Violence, Treatment Needs, and Mental Health. Feminist Criminology. 2012;XX:1–20. [Google Scholar]
- Marcus-Medoza S. Feminist Therapy with Incarcerated Women: Practicing Subversion in Prison. Women & Therapy. 2010;34(1–2):77–92. [Google Scholar]
- Matz AK. Community Corrections Procurement Guide with Bid Specification. Lexington, KY: American Probation and Parole Association; 2012. [Google Scholar]
- Minton TD. Jail Inmates at Midyear 2011 - Statistical Tables. Washington DC: Bureau of Justice Statistics; 2012. [Google Scholar]
- PEW Center. One in 100: Behind Bars in America. Washington DC: The Pew Charitable Trusts; 2008. [Google Scholar]
- Proctor SL. Substance use disorder prevalence among female state prison inmates. American Journal of Drug and Alcohol Abuse. 2012;38(4):278–285. doi: 10.3109/00952990.2012.668596. [DOI] [PubMed] [Google Scholar]
- Slate RN. From the jailhouse to Capitol Hill: Impacting mental health court legislation and defining what constitutes a mental health court. Crime & Delinquency. 2003;49:6–29. [Google Scholar]
- StataCorp. Stata 11 Multiple Imputation Reference Manual. College Station, TX: Stata Press; 2009. [Google Scholar]
- Steadman HJ, Naples M. Assessing the effectiveness of jail diversion programs for persons with serious mental illness and co-occurring substance use disorders. Behavioral Sciences & the Law. 2005;23(2):163–170. doi: 10.1002/bsl.640. [DOI] [PubMed] [Google Scholar]
- Steadman HJ, Osher FC, Clark Robbins P, Case B, Samuels S. Prevalence of Serious Mental Illness Among Jail Inmates. Psychiatric Services. 2009;60(6):761–765. doi: 10.1176/ps.2009.60.6.761. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. The NSDUH Report: State Estimates of Adult Mental Illness. Center for Behavioral Health Statistics and Quality; 2011. [Google Scholar]
- Teplin LA, Abram KM, McClelland GM. Mentally disordered women in jail: who receives services? American Journal of Public Health. 1997;87(4):604–609. doi: 10.2105/ajph.87.4.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trestman RL, Ford J, Zhang W, Wiesbrock V. Current and lifetime psychiatric illness among inmates not identified as acutely mentally ill at intake in Connecticut’s jails. Journal of the American Academy of Psychiatry and the Law. 2007;35:490–500. [PubMed] [Google Scholar]
- Turner H, Finkelhor D, Ormrod R. The ffect of lifetime victimization on the mental health of children and adolescents. Social Science & Medicine. 2006;62:13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- Widom CS, Morris S. Accuracy of adult recollections of childhood victimization, Part 2: Childhood sexual abuse. Psychological Assessment. 1997;91(1):34–46. [Google Scholar]
- Widom CS, Shepard RL. Accuracy of adult recollections of childhood victimization, Part 2: Childhood physical abuse. Psychological Assessment. 1996;8(4):412–421. [Google Scholar]
- Wolfe J, Kimerling R. Gender isues in the assessment of Posttraumatic Stress Disorder. In: Wilson J, Keane TM, editors. Assessing psychological trauma and PTSD. New York, NY: Guilford; 1997. [Google Scholar]