Abstract
The most widely used illicit drug in the United States (US) continues to be marijuana, and its use among emerging adults continues to rise. Marijuana use can result in a range of negative consequences and has been associated with other drug use in adolescents and emerging adults. This study examined the relationship between marijuana use frequency and use of six other drug classes (opiates, cocaine, stimulants, hallucinogens, inhalants, and sleep medications) among emerging adults. The design was a cross-sectional interview with a community sample of 1,075 emerging adults in the northeastern US. Using logistic regression analysis controlling for age, ethnicity, gender, and frequency of binge alcohol, daily marijuana use was associated with a significant increase in the expected odds of opiate, cocaine, stimulant, hallucinogen, inhalant, and tobacco use. The findings identify a subgroup of emerging adult marijuana users – those who use daily –that may be vulnerable to additional negative consequences associated with polysubstance use.
Keywords: Marijuana, cannabis, emerging adults, illicit drug use
Introduction
Marijuana continues to be the most widely used illicit drug in the United States (US), with approximately 32% of non-college, and 35% of college-attending, 18–25 year-olds reporting past year use, and 19% of emerging adults (18–29 years old) reporting past month marijuana use1,2. Treatment-seeking rates for marijuana use increased by 162% from 1992–2002, with one-third among 18–25 year olds, with this group at higher risk for negative consequences associated with use, including a range of impairments, accidents, and injuries3.
Previous work has found that marijuana use is associated with the use of other substances. Concurrent polysubstance use is defined as the use of two or more substances within a given time period (e.g., over the last month, or year) and can lead to dramatic health consequences due to the additive or interactive effects of combining substances4–7. Higher rates of concurrent polysubstance use in emerging adults8,9 may be due to accessibility and availability of drugs10, personality traits11,12, the role of marijuana use in decreasing negative affect, anxiety and mood symptoms13–15, and the age of onset of marijuana use16. The “gateway theory” proposes that marijuana use is associated with later illicit drug use (a drug other than marijuana), and further, that there exists a temporal ordering of substance use such that a lower order substance (i.e., marijuana) precedes the use of a higher order substance (e.g., cocaine) 17, 18. While it remains equivocal if this association is causal, several studies indicate that marijuana use typically precedes the use of “harder” drugs of abuse, even when controlling for important covariates and confounders19–21.
In the current study, we examined frequency of marijuana use and its association with other drug use in a community sample of emerging adults (18–25 years old). We hypothesized that a relationship would emerge such that the frequency of marijuana use would be associated with the increased concurrent use of other drugs. To our knowledge, this is the first study to estimate the probabilities of illicit drug use (opiates, stimulants, hallucinogens, inhalants, sleep medication) across discrete categories of marijuana use frequencies among a large sample of emerging adults in the US.
Materials and method
Sample
Study participants were recruited between January 2012 and July 2013. The study protocol was approved by the Butler Hospital Institutional Review Board. Recruitment was completed using several outlets, including targeting the Rhode Island/southeastern Massachusetts geographical area online through Providence Craig’s List and Facebook, and through advertisements placed in local college newspapers, on public transportation, and on commercial radio. The study advertisement read, “Men and Woman between 18 and 25: Have you recently used marijuana or alcohol? You may be eligible to participate in a research study about the health behaviors of emerging adults.”
Interested persons were instructed to call the study phone number or to send an email to the study address to receive a return call to be screened. Screening was anonymous with verbal informed consent. If eligible for the longitudinal parent study concerning Sexually Transmitted Infections (STI) and substance use, individuals were invited for an in-person interview at the research site and offered compensation ($40) and free STI testing. This analysis uses only data derived from the screening interview.
Measures
The ten-minute phone screen included questions related to demographics and living situations, substance use, prescribed medications, sexual activity, mental health and general health. Use of substances (opiates, cocaine, stimulants, hallucinogens, and inhalants) was measured with the following item: “In the last 30 days, how often have you used (substance)?” Sleep medication use was assessed by the following item: “In the past month, how often have you used medication prescribed or over the counter (your own or someone else’s), to help you sleep?” Tobacco use was measured with the following: “In the last 30 days, how often did you smoke cigarettes?” and binge alcohol use with the following question: “In the last 30 days, how often did you have (4 or 5) or more drinks in a row, that is, in a couple hours?” We defined binge alcohol use as 4 or more drinks for women, 5 or more for men, in a two hour period. Frequency of marijuana use was measured with the following item: “In the last 30 days, how often did you use marijuana?” Response options ranged from “Never” to “Monthly” to “More than Monthly” to “Weekly” to “Daily.”
Results
Analytical Methods
Descriptive statistics are presented to summarize the demographic characteristics and self-reported substance use behaviors of participants. Logistic regression was used to estimate the adjusted association of marijuana use frequency with each of 6 substance classes. All models adjusted for age, gender, race/ethnicity, and frequency of binge alcohol use, which was entered into the model as a linear predictor. For all substance use outcomes we used a difference in likelihood ratio chi-square test to compare the fit of a model defining frequency of marijuana use as a linear predictor to a model defining frequency of marijuana use as a 5-category unordered predictor with no marijuana use defined as the reference category; the latter fit the observed data better for stimulants and daily cigarette smoking (p < .05).
In addition, based on the best fitting model, we present a figure plotting the estimated adjusted probability of using each substance class across categories of marijuana use frequency. Because the models are neither linear nor additive with respect to predicted probabilities, all other covariates must be fixed to specific values prior to estimating probabilities. Here, we set age and frequency of binge drinking to their respective means and defined probabilities for non-Hispanic White males. Further, because possession of an ounce or less of marijuana became decriminalized on April 1, 2013, we compared frequency of marijuana use before, and after that date. Finally, we performed auxiliary analysis to determine if the relationship between marijuana use frequency and other substances is conditional on age; for these analyses, age was dichotomized to contrast persons 21 years of age or older to persons under 21.
Results
Participants’ (n = 1,075) mean age was 21.4 (2.2) years; 577 (53.7%) were male, 634 (59.0%) were non-Hispanic White, 156 (14.5%) were African-American, 164 (15.3%) were Hispanic, and 121 (11.3%) were of other racial or ethnic origins. Regarding frequency of marijuana use, 187 (17.4%) reported no use of marijuana, 59 (5.5%) said they used once a month or less, 79 (7.3%) said 2–3 times a month, 315 (43.9%) used weekly or more often, and 437 (40.6%) said they were daily marijuana users. Regarding frequency of binge drinking, 201 (18.7%) reported no binge drinking, 167 (15.5%) reported binging about once a month, 215 (20.0%) said they binged 2–3 times a month, 473 (43.9%) reported binge drinking weekly, and 21 (2.0%) were daily binge drinkers. Sixty-eight (6.3%) reported using opioids, 71 (6.6%) reported using cocaine, 154 (14.3%) reported using stimulants, 75 (7.0%) reported using inhalants or hallucinogens, 200 (18.6%) reported use of sleep medications, and 382 (35.5%) said they were daily smokers.
Table 1 shows the results of logistic regression models predicting use of 6 classes of substances. For each outcome we compared the fit of a model defining frequency of marijuana use as a linear predictor to a model treating it as an unordered categorical predictor; the latter fit the observed data better for stimulants (LR2 = 7.84, df = 3, p = .049) and daily cigarette smoking (LR2 = 8.41, df = 3, p = .038). After controlling for age, ethnicity, gender, and frequency of binge drinking, a 1-category increase in marijuana use frequency was associated with a significant increase in the expected odds of opioid use (OR = 1.42, 95% CI 1.13; 1.77, p = .005), the expected odds of cocaine use (OR = 1.82, 95% CI 1.36; 2.45, p < .001), and the expected odds of hallucinogen/inhalant use (OR = 1.48, 95% CI 1.17; 1.86, p = .001). Relative to no marijuana use, the expected odds of stimulant use were 3.18 (95% CI 1.59; 6.34, p = .001) and 3.10 (95% CI 1.57; 6.11, p = .001) times higher among those who used marijuana weekly or daily, respectively. The expected likelihood of daily cigarette smoking was also much higher among weekly (OR = 3.37, 95% CI 2.02; 5.62, p < .001) and especially among daily (OR = 8.50, 95% CI 5.19; 13.92, p < .001) marijuana users. The odds of sleep medication use was not associated significantly with frequency of marijuana use (OR = 1.10, 95% CI 0.98; 1.23, p = .103).
Table 1.
Logistic Regression Models Estimating the Adjusted Effect of Marijuana Use Frequency on the Odds of Substance Use (n = 1,075)
| Opioids | Cocaine | Stimulants | Inhalants | Sleep Medsa | Smoking | |
|---|---|---|---|---|---|---|
| Model Comparison | LR2 = 0.97 | LR2 = 0.51 | LR2 = 7.84 | LR2 = 2.26 | LR2 = 3.17 | LR2 = 8.41 |
| Linear v. Categoricalb | (p = .802) | (p = .916) | (p = .049) | (p = .592) | (p = .366) | (p = .038) |
|
Estimated Effect on Odds of Use
|
||||||
| Age | 1.14* | 0.97 | 0.92* | 0.95 | 0.97 | 1.13** |
| Ethnicity | ||||||
| African-American | 0.75 | 0.26** | 0.29** | 0.41* | 0.83 | 0.89 |
| Hispanic | 0.73 | 0.32** | 0.46** | 0.78 | 1.29 | 0.78 |
| Other | 0.47 | 0.29** | 0.46* | 0.95 | 1.26 | 1.51 |
| White [REF] | [1.00] | [1.00] | [1.00] | [1.00] | [1.00] | [1.00] |
| Gender (Male) | 1.15 | 1.85* | 0.86 | 1.44 | 0.59** | 1.56** |
| Binge Frequency | 1.35** | 1.97** | 1.39** | 1.34** | 1.24** | 1.21** |
| MJ Freq. (Linear) | 1.42** | 1.83** | NA | 1.48** | 1.10 | NA |
| MJ Freq. (Categorical) | ||||||
| Monthly or Less | 0.25 | 1.57 | ||||
| Monthly Plus | NA | NA | 2.05 | NA | NA | 1.62 |
| Weekly | 3.18** | 3.37** | ||||
| Daily | 3.10** | 8.50** | ||||
| None [REF] | [1.00] | [1.00] | ||||
p < .05,
p < .01
Due to item specific missing data the effective n for the model predicting sleep medication use was 1,073
Likelihood-ratio difference test comparing a model with marijuana use frequency defined as a linear effect to a model with marijuana use frequency defined as an unordered categorical variable. A p-value > .05 indicates the more complex model defining use frequency as an unordered categorical indicator does not fit the observed data significantly better than the more parsimonious linear model. Here, the likelihood ratio test has 3 degrees of freedom. Only the effect on the odds for the best fitting model is presented.
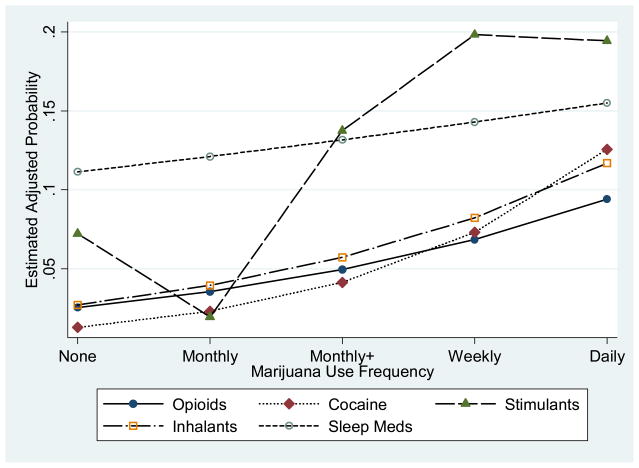
Figure 1 displays the expected probability of substance use across categories of marijuana use frequency implied by the logistic regression models summarized in Table 1 (daily cigarette smoking not presented). The specific probabilities reported were estimated for non-Hispanic white males of average age and with mean levels of binge drinking. For persons with no reported marijuana use, the expected probabilities of opioid, cocaine, and inhalant use were .025, .013, and .027, respectively. For these three outcomes the linear effect of marijuana use frequency fit the observed data adequately. For daily marijuana users the expected probabilities of opioid, cocaine, and inhalant use had increased to .094, .126, and .117, respectively. The effect of marijuana use frequency on sleep medication use was not significant; in this cohort the expected probability of sleep medication use increased from .111 among those reporting no marijuana use to .155 among daily marijuana users. The association between marijuana use frequency and stimulant use was not linear; the estimated probability of stimulant use was lowest (.019) among those using marijuana monthly or less often, increased to .137 among those using marijuana 2–3 times a month and was .198 and .194 among those using marijuana weekly or daily, respectively.
Figure 1.
Estimated Adjusted Probability of Substance Use by Frequency of Marijuana Use
The relationship between marijuana use frequency and likelihood of using other substances was not conditional on age. Tests of the first-order age by marijuana use frequency were not statistically significant for opiates (Wald χ2 = 1.02, df = 1, p = .313), cocaine (Wald 2 = 2142.02, df = 1, p = .120), stimulants (Wald χ2 = 1.23, df = 4, p = .873), inhalants (Wald χ2 = 0.69, df = 1, p = .405), sleep medications (Wald χ2 = 0.78, df = 1, p = .378), or daily smoking (Wald χ2 = 0.82, df = 1, p = .365). Frequency of marijuana use did not differ significantly before and after possession of an ounce or less was decriminalized (t = 0.58, p = .565).
Probabilities of daily cigarette smoking were not included in Figure 1 because the base rate of use was considerably higher than for other substances, which would necessitate use of a different Y-scale range for interpretability. The expected probability of daily smoking was .58 among daily marijuana users and .357 among weekly marijuana users; rates were .142 among those reporting no marijuana use and were just over .2 among those who used marijuana 2–3 times a month or less frequently.
Frequency of binge drinking was also associated with significantly higher likelihoods of using all six classes of substances (Table 1). The product moment (r = .102, p < .001) and rank-order (rs = .094, p < .001) correlations between frequency of marijuana use and frequency of binge drinking were statistically significant but substantively weak.
Discussion
Our findings demonstrate a significant relationship between marijuana use frequency and the use of other substances, including cocaine, stimulants, opiates, and hallucinogens/inhalants, as well as tobacco use, in this community sample of emerging adults (18–25 years old). These results comport with prior research that found a significant association between marijuana use and other illicit drugs in adolescents and emerging adults19–21. The current findings extend our understanding of this association by showing that daily marijuana use predicts a wide range of other types of drug use, including tobacco and binge alcohol use, which are both highly prevalent and co-occurring substances in emerging adults1. To our knowledge, this study is the first to estimate the probabilities of illicit drug use across discrete categories of marijuana use frequencies among a large sample of emerging adults in the US.
Although these data support the association between increased marijuana use and the use of other drugs, we are not able to draw causal conclusions. However, we can speculate as to potential explanations for this association. First, the availability and accessibility of other substances may increase as emerging adults use more marijuana10. Second, emerging adults who use increasing amounts of marijuana may represent a subset of users who are using to self-medicate or mitigate distressing symptoms, including anxiety and depressive symptoms and polysubstance use may augment this perceived self-medication. Third, personality traits, such as impulsivity, may link increased marijuana use to greater use of other substances11, 12, 22. Neuroimaging studies suggest that shared neurological pathways that may increase the risk for later and wider substance misuse 23–25.
These study findings identify a subgroup of marijuana users – daily users – that may be vulnerable not only to risks directly associated with chronic marijuana use, including cognitive impairment (e.g., compromised ability to learn and remember information, sustain and shift attention), and health consequences (e.g., respiratory problems and increased risk of accidents), but also with the additional risks associated with the concurrent use of other drugs. This is an important concern especially during this sensitive time period, given the susceptibility for harm that exists during the late adolescent/early adult years, when brain development of the prefrontal cortex, in particular, continues24, 26. Daily use of drugs of abuse can alter and interfere with the function of neurotransmitters and can lead to compromises in decision-making, placing these emerging adults at further risk for negative consequences.
There are important strengths in the current study. First, our sample was large (n = 1,075) and diverse with regard to gender and race/ethnicity, and identifies a vulnerable age group that has become an important target for intervention. Second, we controlled for important covariates in our analyses, including alcohol binge use, in order to assess the independent effect of marijuana use on other drug use. Third, our analytic approach determined marijuana use frequency using discrete categories, including daily use, which have not been included in previous studies27.
Our study also has limitations worth noting. First, our sample was recruited for a study that specifically targeted emerging adults in the community who used alcohol or marijuana; results may not be generalizable to all emerging adults. Second, we used single items to assess drug use and frequency, and all assessment was based on self-report in this convenience sample. Third, our assessment of stimulant use could not distinguish between medical and non-medical use of prescription stimulants. Fourth, because the study was cross-sectional, we were not able to determine temporal ordering of drug use and whether marijuana use preceded other drug use as the “gateway theory” proposes and thus limited in not directly addressing the issue of marijuana as a gateway drug. Fifth, the study was performed in a state where the possession of less than one ounce of marijuana was decriminalized in April, 2013, and findings may differ in other locations.
Despite the hazards, there is a growing shift in the attitude towards marijuana use, including the misconceptions that emerging adults may have about risks of use (e.g., that its use offers short-term benefits without harmful health effects), perhaps exacerbated by emerging policy changes for medical marijuana use and its legalization for recreational use in some states28. The current findings suggesting a strong relationship between increasing marijuana use and polysubstance use have important clinical implications. Concurrent use of psychoactive substances may increase the risk of negative health consequences. Education in community and medical settings for marijuana users about polysubstance use and its increased risks can be an important form of intervention during the adolescent and emerging adult years for the great majority of users who never seek substance abuse or mental health treatment.
Acknowledgments
This study was supported by NIAAA grant R01AA020509. Dr. Stein is a recipient of NIDA Award K24 DA000512.
References
- 1.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. NSDUH Series H-46, HHS Publication No. 13-4795. [Google Scholar]
- 2.Johnson LD, O'Malley PM, Bachman JG, Schulenberg JE. College students and adults ages. Vol. 2. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2013. Monitoring the Future national survey results on drug use, 1975–2012; pp. 19–50. [Google Scholar]
- 3.Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD. Smoking, drinking, and drug use in young adulthood: The impacts of new freedoms and new responsibilities. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1997. [Google Scholar]
- 4.Pape H, Rossow I, Storvoll E. Under double influence: Assessment of simultaneous alcohol and cannabis use in general youth populations. Drug Alcohol Depen. 2009;101:69–73. doi: 10.1016/j.drugalcdep.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Midanik LT, Tam TW, Weisner C. Concurrent and simultaneous drug and alcohol use: Results of the 2000 National Alcohol Survey. Drug Alcohol Depen. 2007;90:72–80. doi: 10.1016/j.drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boys A, Marsden J, Strang J. Understanding reasons for drug use among young people: a functional perspective. Health Ed Res. 2001;16:457–469. doi: 10.1093/her/16.4.457. [DOI] [PubMed] [Google Scholar]
- 7.Grant BF, Harford TC. Concurrent and simultaneous use of alcohol with sedatives and tranquilizers: Results of a nation survey. J Sub Abuse. 1990;2(1):14. doi: 10.1016/s0899-3289(05)80042-2. [DOI] [PubMed] [Google Scholar]
- 8.McCabe SE, Cranford JA, Morales M, Young A. Simultaneous and concurrent polydrug use of alcohol and prescription drugs: prevalence, correlates, and consequences. J Stud Alcohol. 2006;67(4):529–537. doi: 10.15288/jsa.2006.67.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins RL, Ellickson PL, Bell RM. Simultaneous polydrug use among teens: Prevalence and predictors. J Sub Abuse. 1998;10:233–253. doi: 10.1016/s0899-3289(99)00007-3. [DOI] [PubMed] [Google Scholar]
- 10.Hawkins DJ, Catalano RF, Miller JY. Risk and protective factors for alcohol and other substance problems in adolescence and early adulthood: Implications for substance abuse prevention. Psych Bull. 1992;112(1):64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- 11.Guy SM, Smith GM, Bentler PM. Consequences of adolescent drug use and personality factors on adult drug use. J Drug Educ. 1994;24:109–132. doi: 10.2190/X4WU-BV3X-Q483-Y5BT. [DOI] [PubMed] [Google Scholar]
- 12.Gruber SA, Yurgelun-Todd DA. Neuroimaging of marijuana smokers during inhibitory processing: a pilot investigation. Cog Brain Res. 2005;23:107–118. doi: 10.1016/j.cogbrainres.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 13.Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. Brit Med J. 2002;325(7374):1195–1198. doi: 10.1136/bmj.325.7374.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harris KM, Edlund MJ. Self-Medication of Mental Health Problems: New Evidence from a National Survey. Health Serv Res. 2005;40(1):117–134. doi: 10.1111/j.1475-6773.2005.00345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johns A. Psychiatric Effects of Cannabis. Brit J Psychol. 2001;178:116–211. doi: 10.1192/bjp.178.2.116. [DOI] [PubMed] [Google Scholar]
- 16.Brook JS, Brook DW, De La Rosa M, Duque LF, Rodriguez E, Montoya ID, Whiteman M. Pathways to marijuana use among adolescents: Cultural/ecological, family, peer, and personality influences. J Am Acad Child Adoles Psychiatry. 1998;37:759–766. [PubMed] [Google Scholar]
- 17.Kandel DB, Yamaguchi K, Chen K. Stages of progression in drug involvement from adolescence to adulthood: further evidence for the gateway theory. J Stud Alcohol. 1992;53:447–457. doi: 10.15288/jsa.1992.53.447. [DOI] [PubMed] [Google Scholar]
- 18.Stenbacka M, Allebeck P, Romelsjo A. Initiation into drug abouse: the pathway from being offered drugs to trying cannabis and progression to intravenous drug abuse. Scan J Soc Med. 1993:31–39. doi: 10.1177/140349489302100106. [DOI] [PubMed] [Google Scholar]
- 19.Lessem JM, Hopfer CJ, Haberstick BC, Timberlake D, Ehringer MA, Smolen A, Hewitt JK. Relationship between adolescent marijuana use and young adult illicit drug use. Beh Gen. 2006;36(4):498–506. doi: 10.1007/s10519-006-9064-9. [DOI] [PubMed] [Google Scholar]
- 20.Fergusson DM, Horwood LJ. Does cannabis use encourage other forms of illicit drug use? Addiction. 2000;95:505–520. doi: 10.1046/j.1360-0443.2000.9545053.x. [DOI] [PubMed] [Google Scholar]
- 21.Yamaguchi K, Kandel DB. Patterns of drug use from adolescence to young adulthood: III. Predictors of progression. Am J Public Health. 1984;74:673–681. doi: 10.2105/ajph.74.7.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lejuez CW, Aklin WM, Zvolensky MJ, Pedulla CM. Evaluation of the Balloon Analogue Risk Task (BART) as a predictor of adolescent real-world risk-taking behaviours. J Adoles. 2003;26:475–479. doi: 10.1016/s0140-1971(03)00036-8. [DOI] [PubMed] [Google Scholar]
- 23.Gruber SA, Silveri MM, Dahlgren MK, Yurgelun-Todd DA. Why so impulsive? White matter alterations are associated with impulsivity in chronic marijuana smokers. Exp Clin Psychopharm. 2011;19(3):231–242. doi: 10.1037/a0023034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Squeglia LM, Jacobus BA, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci. 2009;40(1):31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Silveri MM, Tzilos GK, Yurgelun-Todd DA. Relationship between white matter volume and cognitive performance during adolescence: effects of age, sex and risk for drug use. Addiction. 2008;103(9):1509–1520. doi: 10.1111/j.1360-0443.2008.02272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann NY Acad Sci. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- 27.Fergusson DM, Boden JM, Horwood LJ. Cannabis use and other illicit drug use: testing the cannabis gateway hypothesis. Addiction. 2006;101:556–569. doi: 10.1111/j.1360-0443.2005.01322.x. [DOI] [PubMed] [Google Scholar]
- 28.Office of National Drug Control Policy (ONDCP) Marijuana Myths &Facts. [Accessed electronically on 10/1/13];The Truth Behind 10 Popular Misperceptions. https://www.ncjrs.gov/ondcppubs/publications/pdf/marijuana_myths_facts.pdf.