Abstract
Introduction:
A growing body of literature indicates that insomnia is related to suicidality. However, the mechanism through which insomnia correlates with suicide risk is unclear. The goal of the present research was to determine whether hopelessness, a robust predictor of suicidality, mediates the relation between insomnia and suicidal ideation (SI).
Methods:
The present study used archival data from community-dwelling adults. Participants (n = 766) completed a Health Survey, two weeks of daily sleep diaries, and five measures of daytime functioning, including the Beck Depression Inventory (BDI). BDI item 2 was used to assess hopelessness, and BDI item 9 was used to assess SI. Criteria from the DSM-5 as well as quantitative criteria were used to identify participants with insomnia (n = 135).
Results:
The analyses revealed that hopelessness is a significant mediator of the relation between insomnia and SI. After adding depression as an additional mediator, hopelessness remained a significant predictor of SI.
Conclusion:
The present research suggests the need for clinicians to routinely screen clients who have insomnia for hopelessness and SI, and to treat hopelessness when it is present. Further research should address the limitations in this sample and should also consider other potential mediators of the insomnia-SI link.
Citation:
Woosley JA, Lichstein KL, Taylor DJ, Riedel BW, Bush AJ. Hopelessness mediates the relation between insomnia and suicidal ideation. J Clin Sleep Med 2014;10(11):1223-1230.
Keywords: insomnia, suicidal ideation, hopelessness, mediation
Suicide rates in the U.S. have been rising steadily in recent years.1 From 2000 to 2009, mortality rates for suicide increased by 15%, with suicide emerging as the leading cause of injury-related death in 2009.2 Among all causes of mortality, suicide was the 10th leading cause of death annually from 2008 to 2010, with approximately 105 deaths by suicide occurring per day in 2010.1,3 Additionally, in 2009 an estimated 1 million adults (aged 18 and older) made suicide attempts.4 Clearly, suicide is a growing problem in the U.S., and research is needed to improve the identification of individuals at risk for suicidal behavior.
In an effort to improve identification of such individuals, many researchers have focused on identifying risk factors for suicide. Demographic characteristics such as disrupted marital status and male gender have been associated with death by suicide,5 and female gender has been associated with suicide attempts.6 A personal history of suicide attempts, a family history of suicide, impulsive or aggressive tendencies, social isolation, and physical illness are also predictive of suicide.7
Suicidal ideation (SI) has been defined as thoughts about engaging in suicide-related behavior.8 The term “suicidal ideation” encompasses a wide range of thoughts, including passive wishes to be dead, thoughts about committing suicide, intent to commit suicide, and specific plans about how to commit suicide.9,10 Longitudinal research indicates that SI is a particularly important risk factor for future suicide attempts and suicide deaths.11,12 Research from a nationally representative survey suggests that approximately 90% of unplanned first suicide attempts and 60% of planned first suicide attempts occur within one year of the onset of SI.6 Additionally, it is generally presumed that SI is a prerequisite for suicide attempts, with the exception being those atypical instances of impulsive suicidal behavior wherein the first instance of SI is contiguous with suicidal behavior. Consequently, assessment of risk among individuals endorsing SI is considered an important step in suicide prevention.13
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although there is much evidence to support the notion that insomnia predicts suicidality, little is known about the mechanisms by which insomnia may lead to increased suicidality. The present study sought to address this gap in the literature by determining whether hopelessness could serve as a mediator of the insomnia-suicidal ideation link.
Study Impact: The results of this research imply that it may be helpful for clinicians who treat individuals with insomnia to screen for and treat hopelessness, as clients with insomnia and elevated levels of hopelessness may be at elevated risk for suicidal ideation. In light of the present findings with cross-sectional data, more research is needed to determine whether this mediation model can be supported longitudinally.
In addition to the aforementioned risk factors, there is evidence that hopelessness contributes to suicidality. Hopelessness has been defined by Beck as pessimism or “a system of negative expectancies” concerning oneself and one's future life.14 Cross-sectional and longitudinal research suggest that hopelessness out-performs depression as a predictor of SI.15,16 Longitudinal research also indicates that hopelessness is predictive of suicide attempts after controlling for a history of attempts.17 Additionally, hopelessness, along with rumination, predicts the duration of SI, suggesting that hopelessness plays a role in maintaining SI.18 Hopelessness has also been shown to mediate the relation between other suicide risk factors (e.g., rumination, past childhood maltreatment, stress, depression) and suicidality.18–20 Thus, it is clear that hopelessness is an important predictor of suicidality.
A growing body of research indicates that insomnia is also associated with heightened suicide risk. Prior cross-sectional research indicates that the presence, severity, and chronicity of insomnia symptoms are associated with increased suicidality.21–28 Further, recent longitudinal research linking insomnia at baseline with suicidality at a later time point suggests that insomnia may contribute to suicidality.29–31 In many of these studies, the relation between symptoms of insomnia and suicidality has remained significant after controlling for other robust predictors of suicidality, such as chronic health problems, depression, and hopelessness.26,27,29,30
One recent study investigated the influence of seven sessions of group cognitive-behavioral therapy for insomnia (CBT-I) on SI.32 In this research, 45% of participants who endorsed SI at baseline (using item 9 from the Beck Depression Inventory–II [BDI-II]) no longer endorsed it following treatment. Further, among the 65 participants who endorsed SI at baseline, the mean score on BDI-II item 9 at baseline was 1.10 at baseline and 0.45 at post-treatment. Thus, CBT-I produced a decrease in SI with a large effect size (d = 1.83). This finding lends further support to the notion that insomnia contributes to SI.
It seems plausible that hopelessness about one's sleep could also contribute to suicidality. For instance, hopelessness may have contributed to the aforementioned finding that people with persistent insomnia were more likely to report SI than people having less chronic insomnia and people without insomnia.28 People with insomnia may presumably become more hopeless about improving their sleep the longer their insomnia persists. However, despite recent interest in the relation between insomnia and suicidality, the association between insomnia and hopelessness has yet to be explored in great depth.
One recent study that examined the relation between insomnia and suicidality reported a significant cross-sectional correlation (r = 0.55, p < 0.001) between insomnia (measured by the sum of scores on two items from the Beck Depression Inventory and one item from the Suicide Probability Scale) and hopelessness (measured by the Beck Hopelessness Scale).29 Cross-sectional and longitudinal multiple regression analyses were conducted to determine whether insomnia, controlling for other potential predictors of SI (including hopelessness), predicted SI. Although insomnia was found to be a significant predictor in both models, there are a few reasons why these findings do not necessarily rule out the possibility that hopelessness may mediate the insomnia-SI relation. First, the researchers (who were not seeking to identify mediators of the insomnia-SI relation) did not run analyses to determine whether hopelessness was acting as a partial mediator. Further, although the longitudinal regression model failed to show that baseline hopelessness predicted SI at one-month follow-up, hopelessness was not measured at the second time point. Therefore, it is unknown whether a change in hopelessness between time points mediated the relation between insomnia and SI.
The only study that has considered hopelessness as a potential mediator of the insomnia-SI relation found that hopelessness (measured by the Beck Hopelessness Scale) was significantly related to SI, but not to Insomnia Severity Index score (r = 0.19).33 However, this research did find that dysfunctional beliefs about sleep, some of which have a sense of hopelessness about them, did significantly mediate the insomnia-SI relation. Notably, this research was conducted using psychiatric patients with depressive disorders, which may have limited variability in BHS and ISI scores. Further, the participants were taking a variety of psychotropic medications (e.g., antidepressants, antipsychotics, mood stabilizers, hypnotics) that may have influenced their sleep, and thereby influenced the relation between BHS and ISI scores. In light of these considerations, further research is warranted.
Prior research with a subset of the sample used in this study used backward stepwise logistic regression to identify variables that predict SI. Of a large group of candidate variables (including presence of various medical conditions, sleep diary measures, age, BMI, and daytime impairment) insomnia was one of three variables that predicted SI.34 The present research sought to expand on that finding by testing the hypothesis that hopelessness mediates the relation between insomnia and SI. The present study has a number of methodological differences from the aforementioned study by McCall and colleagues,33 which the investigators felt could influence the outcome.
METHODS
The present study used archival data gathered from a community-dwelling sample of participants in an epidemiological study of sleep.35 The purposes of that study were to establish sleep norms; elucidate age, gender, and ethnic differences in sleep; obtain detailed data on insomnia; and to ascertain daytime correlates of sleep.
Participants
Participants were recruited via random-digit dialing in the Memphis area. The list of phone numbers included all valid 3-digit prefixes in use in the Memphis area paired with randomly generated 4-digit numbers. This list included business, home, cellular, and unissued numbers. Recruiters called each random number until they had made a “successful” call or called a particular number 5 times unsuccessfully. A successful phone call was defined as one having one of the following outcomes: non-working numbers, business numbers, individuals who agreed to participate, individuals who did not agree to participate, and individuals who did not meet study criteria. Phone calls were made only during the following hours: 10 a.m. to 11:30 a.m., 1:30 p.m. to 4:30 p.m., and 6:30 p.m. to 8 p.m. These particular time periods were used in order to avoid calling potential participants at inconvenient times (i.e., the early morning, lunchtime, and the late evening hours).
To be eligible for the study, participants had to be ≥ 20 years old and able to speak and read English at a seventh-grade level. In situations in which cohabiting partners expressed an interest in the study, only one of the partners was allowed to participate due to the concern that there would be constrained variability in bed partners' sleep habits. However, other members of the same household were allowed to participate. There were no screening criteria related to sleep schedules, health status, or presence/absence of a sleep complaint. The goal was to recruit 50 men and 50 women in each of the following age groups: 20-29, 30-39, 40-49, 50-59, 60-69, 70-79, and 80+. After an age group was filled, potential participants in that age group were excluded.
Of the 19,893 households contacted, 1,769 participants were recruited. Eight hundred fifty-eight of these recruits returned their packets. Because 87 of these participants had a large amount of missing or ambiguous data, the number of participants was reduced to 771. These individuals participated in an epidemiological study conducted by Lichstein and colleagues.35 Five of the aforementioned 771 participants were excluded from the present study due to missing responses on item 2 of the BDI. Three of the excluded participants were also missing responses to item 9 of the BDI.
Measures
Health Survey
The health survey35 included 13 items regarding demographic information (height, weight, and race); sleep disorder symptoms (e.g., endorsement of a sleep problem, type of sleep problem endorsed, snoring, sleep attacks); physical health (current illnesses, medications, and vitamins); mental health (e.g., self-reported mental health problems, diagnoses); consumption of alcohol, caffeine, and nicotine; and household education level. One additional question asked participants to list any illnesses they had, or medications they used, that affected their sleep.
Sleep Diary
Sleep diaries35 included the following measures: bedtime (the time the individual entered bed with the intent of going to sleep), SOL (the interval between bedtime and sleep onset), NWAK (the number of awakenings that occurred between sleep onset and the final awakening), WASO (the total time spent awake after sleep onset and before the final awakening), time of final wake-up (the time at which the individual awoke for the last time), rising time (the time at which the individual got out of the bed), bedtime medication/alcohol (any sleep medication or alcohol taken near bedtime with the amount taken and the time at which it was taken), and nap (total time spent napping the previous day). From this information, the researchers calculated time in bed (TIB), terminal wake time (TWAK; the interval between time of final wake-up and rising time), total sleep time (TST), and sleep efficiency percentage (SE). TIB was determined by the interval between bedtime and rising time. The investigators calculated the total amount of wake time during the sleep period by adding SOL, WASO, and TWAK, and then subtracting the total wake time from TIB to yield TST (TIB = TST + total wake time). Finally, SE was calculated by dividing TST by TIB and multiplying by 100.
Epworth Sleepiness Scale (ESS)
The ESS measures daytime sleepiness in various quiescent situations. Respondents are instructed to rate their likeliness of falling asleep in a variety of everyday circumstances (e.g., sitting and reading, sitting inactive in a public place). In terms of validity, the ESS has been found to correlate significantly with the multiple sleep latency test. Furthermore, research indicates that the ESS has strong test-retest reliability (r = 0.82) and high internal consistency (Cronbach's α = 0.88).36
Fatigue Severity Scale (FSS)
The FSS is a brief questionnaire that measures subjective severity of fatigue.37 Respondents read 9 short statements (e.g., “fatigue interferes with carrying out certain duties and responsibilities”) and to rate their agreement with each one. In a study comparing patients having multiple sclerosis or systemic lupus erythematosus to healthy controls, the FSS was able to distinguish between the healthy controls and patients. Furthermore, the FSS exhibited good internal consistency (Cronbach's α = 0.88).37
Insomnia Impact Scale (IIS)
The IIS is a measure of daytime functioning for people with insomnia. It instructs respondents to rate their agreement with 40 statements about the impact of poor sleep (e.g., “Poor sleep prevents career advancement”). It has been found to discriminate between people seeking treatment for insomnia and normal sleepers.38
Beck Depression Inventory (BDI)
The BDI is a measure of depression severity, with 21 items, each of which addresses a different symptom of depression, such as lack of satisfaction, suicidal wishes, and crying.39 Respondents choose one of four responses that best reflects how they feel, with the lower-numbered responses corresponding to low symptom severity and the higher-numbered responses corresponding to greater symptom severity. A meta-analysis of psychometric research on the BDI determined that its mean coefficient alphas for internal consistency among psychiatric patients and non-psychiatric participants were 0.86 and 0.81, respectively.40 The BDI also has good concurrent validity with other established measures of depression (e.g., Hamilton Rating Scale for Depression, Minnesota Multiphasic Personality Inventory – Depression Scale).40
Item 2 on the BDI was used to measure hopelessness. Respondents choose one of the four following statements on Item 2 that best described how they feel: “I am not particularly discouraged about the future,” “I feel discouraged about the future,” “I feel I have nothing to look forward to,” “I feel the future is hopeless and that things cannot improve.” These items are scored on a scale of 0 to 3 to indicate severity. Item 2 has been found to correlate significantly with scores on the Beck Hopelessness Scale (r = 0.67, p < 0.001) and has been shown to predict death by suicide.41,42 Additionally, clinicians are sometimes advised to pay particular attention to this item as an indicator of suicide risk.43
Item 9 on the BDI will be used as a measure of SI. Respondents choose one of the following statements on Item 9 that best describes how they feel: “I don't have any thoughts of killing myself,” “I have thoughts of killing myself, but I would not carry them out,” “I would like to kill myself,” “I would kill myself if I had the chance.” These items are scored on a scale of 0 to 3 to indicate severity. There is evidence to suggest that Item 9 can provide a valid measure of SI; item 9 has shown a significant correlation with the first five items of Beck's Scale for Suicidal Ideation, which screen for attitudes about living and dying (only individuals who indicate a desire to make a suicide attempt in their responses to the first five items of the Scale for Suicidal Ideation complete the remainder of the measure).44 Further, an extensive review of the psychometric properties of suicide assessment measures concluded that there is evidence that BDI item 9 has good concurrent and predictive validity.45 This item has also been used as a measure of SI in previous research.32,46
State-Trait Anxiety Inventory, Trait Scale, Form Y (STAI)
The trait scale of the STAI is a 20-item measure used to assess trait anxiety.47 Respondents rate each statement with regard to how often that statement is true, with higher scores indicating greater levels of anxiety.
Procedure
After agreeing to participate in the study on the phone, participants were mailed a packet containing sleep diaries for 14 days, the health survey, daytime functioning questionnaires (ESS, FSS, IIS, BDI, STAI), a cover sheet with instructions, and two informed consent forms (one to sign and return and one to keep). The packet also contained a compensation form and a preaddressed, stamped envelope for return of the packet. Participants completed sleep diaries each morning for two weeks. They also completed each of the daytime impairment measures on the last day (14th day) of completing sleep diaries. Participants were instructed to complete these measures with regard to their functioning over the previous two weeks (i.e., the same period of time as they were completing sleep diaries). After returning the completed measures, participants received financial compensation.
All questionnaires were scored twice independently by research assistants. The scored questionnaires were reviewed by a supervisor, who resolved any discrepancies. Research assistants entered data, and these entries were checked by a second research assistant, who made note of any discrepancies. Discrepancies were then resolved by a supervisor. Subsequently, the data were checked for outliers and implausible values. Dubious values were checked against the raw data and corrected as needed.
Statistical Analyses
In order to determine whether hopelessness mediates the relation between insomnia and SI, mediation analyses48,49 were conducted. Baron and Kenny recommended using the following steps to assess mediation: (1) regress the outcome on the predictor (path c in Figure 1), (2) regress the mediator on the predictor (path a in Figure 1), (3) regress the outcome on the mediator (path b in Figure 1), and (4) regress the outcome on the predictor after controlling for the mediator on Step 1 (path c' in Figure 1).48 According to Baron and Kenny, if the variance explained by the predictor decreases after controlling for the mediator, there is evidence of mediation.
Figure 1. Model with hopelessness mediating the relation between insomnia and suicidal ideation.
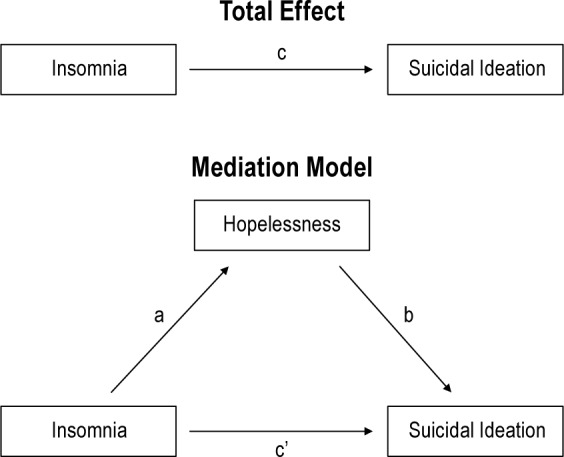
Hypothesized mediation model. Path a represents the relation between the predictor (insomnia) and the mediator (hopelessness), path b represents the relation between the mediator (hopelessness) and the outcome (suicidal ideation), path c represents the relation between the predictor (insomnia) and the outcome (suicidal ideation), and path c' represents the relation between the predictor and the outcome after controlling for the mediator.
Baron and Kenny also discussed using the Sobel test to determine whether the indirect effect (the influence of the predictor on the outcome through the mediator) is significant.48 However, one of the assumptions of the Sobel test is a normal distribution of the indirect effect, but such distributions are frequently skewed.49 Therefore, in the present study, the Preacher and Hayes method was used instead. Hayes' PROCESS macro,50 which uses a nonparametric bootstrapping procedure to determine whether the coefficient of the indirect path is significant, was used for the mediation analyses in the present study. The bootstrapping procedure treats the sample data as a population and draws multiple samples with replacement (called bootstrap samples) from this “population.” For each bootstrap sample, the indirect effect and standard deviation are calculated. The indirect effect is calculated using the product of the coefficients of paths a and b (i.e., the relations between the predictor and the mediator and between the mediator and the outcome). The final estimate of the indirect effect is represented by the mean indirect effect computed over 1,000 bootstrap samples, and the estimated standard error is the standard deviation of the 1,000 indirect effect estimates. The 95% confidence interval (CI) is determined by ordering the 1,000 estimates of the indirect effect from low to high. The lower limit of the CI is the 25th score in the distribution, and the upper limit is the 976th score in the distribution.49
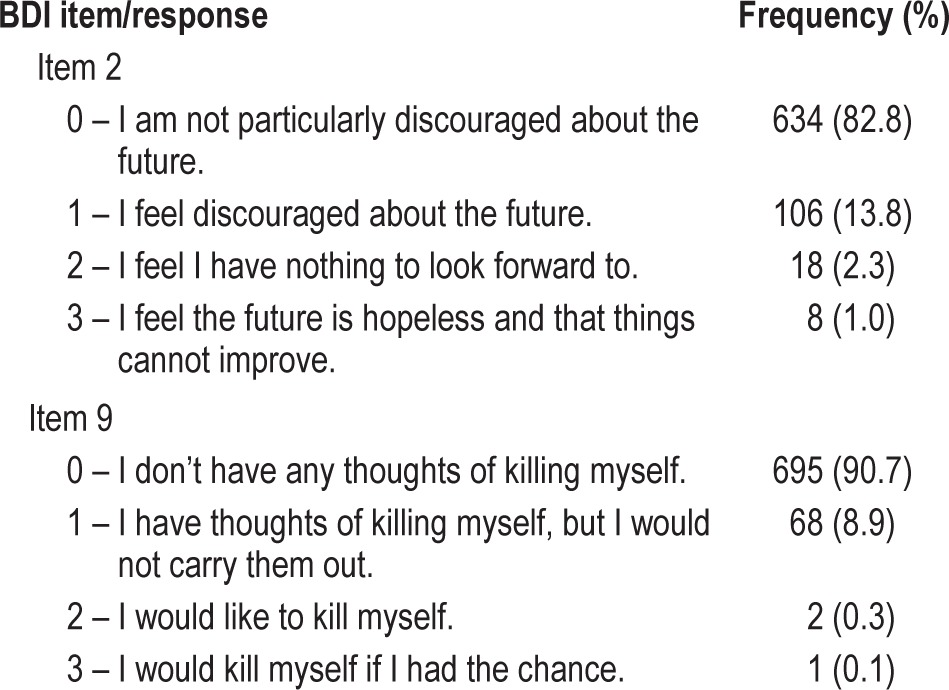
For all analyses, responses to BDI item 9 were dichotomized into absence/presence of SI due to the low frequency of scores > 1 on this item (see Table 1 for frequencies). Recent research identified a score of 1 as the optimal cutoff to predict suicide deaths,51 and this threshold has been used in prior research to distinguish individuals experiencing SI from those not experiencing SI.32,52 Thus, there were 695 participants for whom SI was absent (i.e., score of 0 on item 9) and 71 participants for whom it was present (i.e., score > 0 on item 9). Additionally, because of the low frequency of scores of 3 on BDI item 2 (see Table 1), participants scoring 2 or 3 on this item were combined. As such, there were 634 participants who obtained a score of 0 on this item, 106 participants who obtained a score of 1, and 26 participants who obtained a score of 2 or 3.
Table 1.
Responses to BDI items 2 and 9.
RESULTS
Participant Characteristics
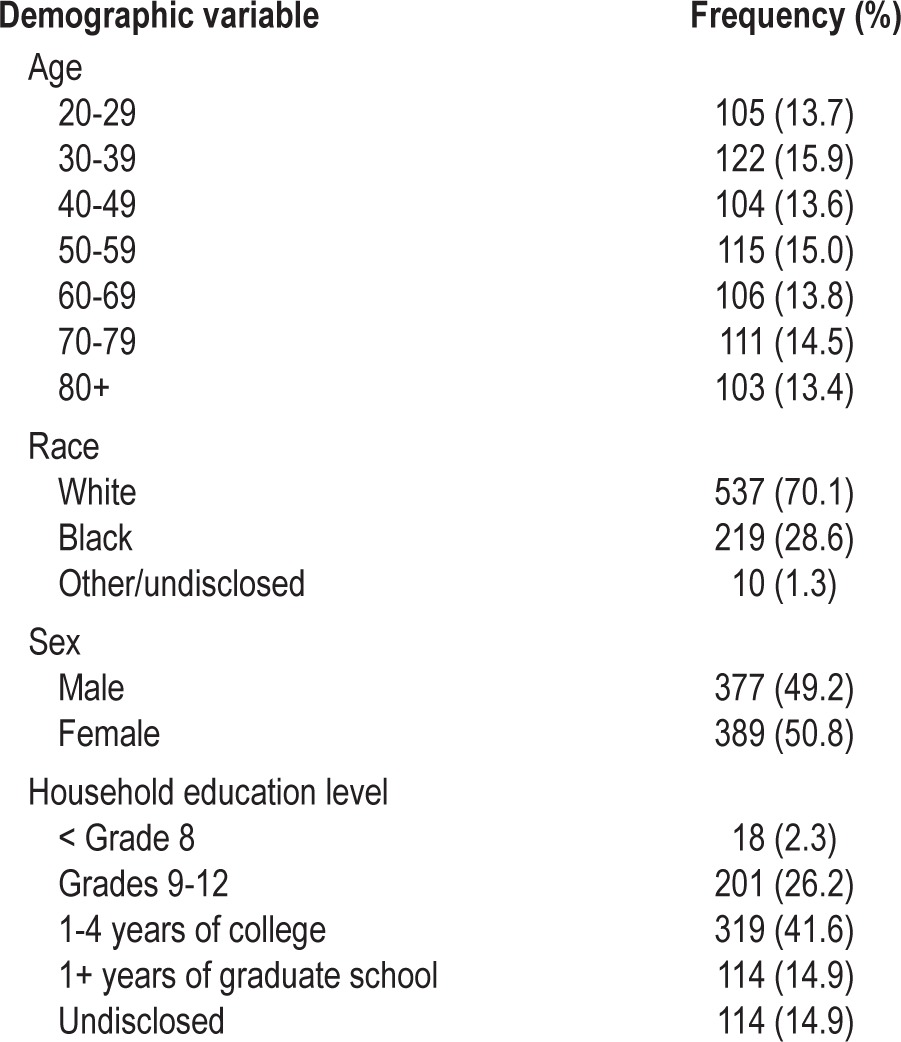
These analyses included 766 participants ranging in age from 20 to 98 (mean = 53.78, SD = 19.85). Participants' demographic characteristics are presented in Table 2. Forty-nine percent of the participants identified as male and 51% as female. Approximately 70% of participants were White and 29% were Black. The remaining 1% of participants were of other races (1 Hispanic, 7 Asian) or chose not to disclose their race. Scores on BDI item 2 ranged from 0 to 3 (mean = 0.22, SD = 0.53), and scores on BDI item 9 ranged from 0 to 3 (mean = 0.10, SD = 0.32).
Table 2.
Participant demographic characteristics.
Of the 766 participants included in this study, 135 were determined to have insomnia using DSM-5 diagnostic criteria as well as quantitative criteria.53 The DSM-5 criteria for Insomnia Disorder include the following: (a) a complaint of difficulty initiating or maintaining sleep and (b) clinically significant distress or impaired daytime functioning resulting from the sleep disturbance.9 The quantitative criteria included: (a) a subjective complaint of insomnia with a duration ≥ 6 months, (b) impaired daytime functioning (score ≥ 7.4 on the Epworth Sleepiness Scale, ≥ 5.5 on the Fatigue Severity Scale, ≥ 125 on the Insomnia Impact Scale, ≥ 10 on the Beck Depression Inventory, or ≥ 37 on the State-Trait Anxiety Inventory), and (c) sleep onset latency (SOL) > 30 min or wake time after sleep onset (WASO) totaling > 30 min ≥ 3 nights per week as assessed by sleep diary.
Hopelessness as a Mediator
The relation between insomnia and SI (path c in Figure 1) was significant (likelihood ratio χ2[1] = 5.35, p = 0.021, McFadden's R 2 = 0.011; step 1 of Baron and Kenny's method). Additionally, the relations between insomnia and hopelessness (likelihood ratio χ2[2] = 30.42, p < 0.001, McFadden's R2 = 0.036; step 2 of Baron and Kenny's method) and between hopelessness and SI (likelihood ratio χ2[2] = 75.15, p < 0.001, McFadden's R 2 = 0.159; step 3 of Baron and Kenny's method) were both significant (paths a and b in Figure 1, respectively). As expected, after controlling for hopelessness, insomnia no longer predicted SI (likelihood ratio χ2[1] = 0.001, p = 0.974; path c' in Figure 1; step 4 of Baron and Kenny's method). Additionally, the CIs for the bootstrapped estimate of the indirect effect did not include zero (95% CI [0.24, 0.71]), indicating that hopelessness is a significant mediator of the relation between insomnia and SI.
Exploration of Alternative Mediation Models
To determine whether alternative models might better fit the data, other mediation models were tested. One such model investigated whether SI acts as a mediator between hopelessness and insomnia. The relation between hopelessness and insomnia (likelihood ratio χ2[2] = 30.42, p < 0.001, McFadden's R2 = 0.036) remained significant after controlling for SI (likelihood ratio χ2[1] = 24.15, p < 0.001), and the confidence intervals for the bootstrapped estimate of the indirect effect included zero (95% CI [-0.14, 0.15]). This indicates that SI does not significantly mediate the relation between hopelessness and insomnia.
Another mediation model was tested wherein insomnia was entered as the mediator between hopelessness and SI. The relation between hopelessness and SI (likelihood ratio χ2[2] = 75.15, p < 0.001, McFadden's R2 = 0.159) remained significant after controlling for insomnia (likelihood ratio χ2[1] = 68.56, p < 0.001), and the CIs for the bootstrapped estimate of the indirect effect estimate included zero (95% CI [-0.13, 0.11]). These findings indicate that insomnia does not mediate the relation between hopelessness and SI.
Due to concern that BDI item 2 may have functioned as a proxy measure of depression, two serial multiple mediator models were tested in an effort to distinguish BDI item 2 from depression. In light of the shortcomings of the BDI that precipitated its revision (e.g., lack of concordance with diagnostic criteria for depression), as well as the potential overlap between certain items on the BDI and symptoms of insomnia (e.g., worry about health, fatigue, irritability), a subscale of items was created for use as a measure of depression (Cron-bach's α = 0.77). The items included and their corresponding DSM-5 symptoms are as follows: mean of items 1 and 10 (depressed mood), item 4 (loss of interest/pleasure), item 18 (change in appetite), mean of items 5 and 8 (feelings of worthlessness or guilt), and item 13 (concentration impairment or indecisiveness).
In both serial multiple mediator models, the indirect effect was significant (95% CI [0.55, 1.25]). Both depression and hopelessness independently predicted SI in step 4 of the Baron and Kenny method, whereas insomnia was no longer a significant predictor. In the first model, depression was entered as the first mediator and hopelessness was entered as the second mediator of the relation between insomnia and SI. The specific indirect effect through depression and hopelessness in serial was significant (95% CI [0.05, 0.28]). In the second model, the order of the mediators was reversed—hopelessness was entered as the first mediator and depression as the second. The specific indirect effect through hopelessness and depression was also significant (95% CI [0.15, 0.49]).
DISCUSSION
The results of this study are consistent with the hypothesis that hopelessness mediates the relation between insomnia and SI. Additionally, examination of alternative models considering SI as a mediator of the relation between hopelessness and insomnia or insomnia as a mediator of the relation between hopelessness and SI did not provide evidence of mediation. This lends support to the proposed mediation model and to the notion that insomnia may contribute to SI through its influence on hopelessness. Additionally, there was evidence that hopelessness and depression function as independent mediators of the insomnia-SI relation.
To the best of the authors' knowledge, this study is only the second to have explored mediators of the insomnia-SI relation. The fact that hopelessness was significantly associated with insomnia and that it mediated the insomnia-SI relation suggests that it may be worthwhile for clinicians who treat individuals having insomnia to assess their clients' degree of hopelessness. Based on the present findings, as well as previous research that has established hopelessness as a robust predictor of suicidality,17 clients who endorse high levels of hopelessness are likely to be at greater risk for SI, and ultimately, suicidal behavior. Such clients may require routine risk assessment, particularly if their insomnia persists. Further, they may benefit from treatments that directly target their hopelessness (e.g., cognitive restructuring to reduce negative thinking about the future). As previous research identified dysfunctional beliefs about sleep (many of which could be considered to have a sense of hopelessness to them) as a mediator of the insomnia-SI relation,33 it may be particularly worthwhile for clinicians to address hopeless cognitions about clients' sleep.
One possible interpretation of the results from the serial mediation models is that hopelessness and depression may function in different ways in mediating the insomnia-SI link. In some instances, insomnia may first lead to symptoms of depression other than hopelessness, such as anhedonia or indecisiveness. As the depression worsens, hopelessness may set in, and subsequently, SI. In other cases, insomnia may lead to hopelessness about poor sleep, which could then lead to other symptoms of depression and then SI. The latter interpretation is consistent with the finding that dysfunctional beliefs about sleep mediate the insomnia-SI relation.33
One limitation in this study is that the direction of the relation between insomnia, hopelessness, and SI cannot be determined due to the cross-sectional design. Based on the mediation model in this study, it seems likely that insomnia contributes to hopelessness, which then contributes to SI. Although it is possible that the reverse of this could be true, it seems unlikely given past research that indicates that hopelessness prospectively predicts SI.18,54
Another limitation in this research pertained to the measures that were used. Because single items were used to measure hopelessness and SI, it is likely that there were aspects of these constructs that were not reflected in these measures. Additionally, single items cannot capture as much variability in a construct as can multiple-item questionnaires, and they are likely to be less valid and reliable than multiple-item measures.
A final limitation in this study is the positive skew of scores on BDI items 2 and 9. Because this research used a community sample, it was uncommon for participants to endorse high levels of SI and hopelessness. As a result, groups of participants were combined for analyses (e.g., participants scoring 2 or 3 on BDI item 2). This reduced the variability in the outcome measures and reduced the amount of information the analyses could provide about participants experiencing more severe SI or hopelessness.
Because the finding that hopelessness mediates the relation between insomnia and SI is a relatively novel one, and given the inconsistency between the present results and those from the one previous study testing a similar mediation model,33 additional research testing this model would be worthwhile. The discrepancy in results may be due to methodological differences (e.g., use of a sample of community-dwelling adults vs. a sample of psychiatric patients, use of BDI item 2 vs. Beck Hopelessness Scale to measure hopelessness). Thus, research testing this model using various approaches (e.g., samples drawn from other populations) would be particularly helpful in determining the generalizability of these findings.
In the future, researchers should also address the limitations in the present study. It would be ideal if subsequent studies incorporated multiple time points of data collection. Such a design would allow researchers to examine the directionality of the relation between insomnia, hopelessness, and SI, and this information could impact the evaluation and treatment of individuals with insomnia.
Further, recruiting from a clinical setting, or a combination of settings including inpatient and outpatient facilities and the community, may increase variability in scores on hopelessness and SI. Future studies could also use multiple-item measures of hopelessness and suicidality to provide further support for the present results. For instance, researchers could use the Beck Hopelessness Scale or the Helplessness/Hopelessness Scale of the MMPI-2-RF to measure hopelessness. The worry/helplessness subscale of the Dysfunctional Beliefs and Attitudes about Sleep scale could also be used to measure cognitions about sleep that have a sense of hopelessness to them. Measures of suicidality that could be used in future research could include the Beck Scale for Suicidal Ideation, the Adult Suicidal Ideation Questionnaire, or the Suicide Intent Scale. It is probable that the use of such multiple-item questionnaires would allow for more variability in responses, which could lead to more robust results.
Besides addressing the limitations in the present research, future research should more closely evaluate the relation between insomnia and hopelessness. Because not all people with insomnia are hopeless, and not all people who feel hopeless have insomnia, there must be factors mediating this relation. If mediating factors could be identified, these factors could be directly targeted in treatment.
Finally, future research should consider other potential mediators of the insomnia-SI relation. Given the complexity of human behavior, cognition, and physiology, it is likely that there are multiple variables influencing the insomnia-SI link. Factors such as impaired problem-solving abilities, abnormal functioning in serotonergic pathways, hyperarousal, and eveningness chronotype could reasonably play a mediating role in this relation.55 Identification of additional mediators would be beneficial in guiding the treatment of individuals experiencing insomnia and SI.
In conclusion, this research indicates that a relation exists between insomnia and hopelessness. Due to the important clinical implications of this finding, additional research in this area is warranted. It is the investigators' hope that this line of research will lead to improvements in the identification and treatment of individuals who are at risk for suicide.
DISCLOSURE STATEMENT
This was not an industry supported study. Research was supported by National Institute on Aging grants AG12136 and AG14738. Data were collected at the University of Memphis and analyzed at The University of Alabama. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Centers for Disease Control and Prevention. Fatal Injury Data. Atlanta, GA: National Center for Injury Prevention and Control; 2012. Web-based Injury Statistics Query and Reporting System (WISQARS) Retrieved January 19, 2013, from http://www.cdc.gov/injury/wisqars/index.html. [Google Scholar]
- 2.Rockett IRH, Regier MD, Kapusta ND, et al. Leading causes of unintentional and intentional injury mortality: United States, 2000–2009. Am J Public Health. 2012;102:e84–e92. doi: 10.2105/AJPH.2012.300960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kochanek KD, Xu J, Murphy SL, Miniño AM, Kung HC. Deaths: final data for 2009. Natl Vital Stat Rep. 2011;60:1–116. [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Health Services Administration. Rockville, MD: 2010. Results from the 2009 National Survey on Drug Use and Health: Mental Health Findings (Office of Applied Studies, NSDUH Series H-39, HHS Publication No. SMA 10-4609) [Google Scholar]
- 5.Moscicki EK. Epidemiology of suicide. Int Psychogeriatr. 1995;7:137–48. [PubMed] [Google Scholar]
- 6.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–25. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Injury Center: Violence Prevention. Atlanta, GA: National Center for Injury Prevention and Control, Division of Violence Prevention; 2012. Suicide: Risk and Protective Factors. Retrieved February 9, 2013, from http://www.cdc.gov/violenceprevention/suicide/riskprotectivefactors.html. [Google Scholar]
- 8.Department of Health and Human Services. National Strategy for Suicide Prevention: Goals and Objectives for Action. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2001. Glossary of suicide prevention terms. [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.McAuliffe CM. Suicidal ideation as an articulation of intent: a focus for suicide prevention? Arch Suicide Res. 2000;6:325–38. [Google Scholar]
- 11.Britton PC, Conner KR. Suicide attempts within 12 months of treatment for substance use disorders. Suicide Life Threat Behav. 2010;40:14–21. doi: 10.1521/suli.2010.40.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Darke S, Ross J, Williamson A, Mills KL, Havard A, Teesson M. Patterns and correlates of attempted suicide by heroin users over a 3-year period: findings from the Australian treatment outcome study. Drug Alcohol Depend. 2007;87:146–52. doi: 10.1016/j.drugalcdep.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 14.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974;42:861–5. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 15.Wetzel RD, Margulies T, Davis R, Karam E. Hopelessness, depression, and suicide intent. J Consult Clin Psychol. 1980;41:159–60. [PubMed] [Google Scholar]
- 16.Beck AT, Steer RA, Beck JS, Newman CF. Hopelessness, depression, suicidal ideation, and clinical diagnosis of depression. Suicide Life Threat Behav. 1993;23:132–45. [PubMed] [Google Scholar]
- 17.Klonsky ED, Kotov R, Bakst S, Rabinowitz J, Bromet E. Hopelessness as a predictor of attempted suicide among first admission patients with psychosis: a 10-year cohort study. Suicide Life Threat Behav. 2012;42:1–10. doi: 10.1111/j.1943-278X.2011.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith JM, Alloy LB, Abramson LY. Cognitive vulnerability to depression, rumination, hopelessness, and suicidal ideation: multiple pathways to self-injurious thinking. Suicide Life Threat Behav. 2006;36:443–54. doi: 10.1521/suli.2006.36.4.443. [DOI] [PubMed] [Google Scholar]
- 19.Gibb BE, Alloy LB, Abramson LY, Rose DT, Whitehouse WG, Hogan ME. Childhood maltreatment and college students' current suicidal ideation: a test of the hopelessness theory. Suicide Life Threat Behav. 2001;31:405–15. doi: 10.1521/suli.31.4.405.22042. [DOI] [PubMed] [Google Scholar]
- 20.Dieserud G, Røysamb E, Ekeberg Ø, Kraft P. Toward an integrative model of suicide attempt: a cognitive psychological approach. Suicide Life Threat Behav. 2001;31:153–68. doi: 10.1521/suli.31.2.153.21511. [DOI] [PubMed] [Google Scholar]
- 21.Bernert RA, Joiner TE, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005:1135–41. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 22.Krakow B, Ribeiro JD, Ulibarri VA, Krakow J, Joiner TE. Sleep disturbances and suicidal ideation in sleep medical center patients. J Affect Disord. 2011;131:422–7. doi: 10.1016/j.jad.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 23.McCall WV, Blocker JN, D'Agostino R, Kimball J, Boggs N, Lasater B. Insomnia severity is an indicator of suicidal ideation during depression. Sleep Med. 2010;11:822–7. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–8. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carli V, Roy A, Bevilacqua L, Maggi S, Cesaro C, Sarchiapone M. Insomnia and suicidal behaviour in prisoners. Psychiatry Res. 2011;185:141–4. doi: 10.1016/j.psychres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43:526–31. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nadorff R, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43:139–49. doi: 10.1111/sltb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suh S, Kim H, Yang HC, Cho ER, Lee SK, Shin C. Longitudinal course of depression scores with and without insomnia in non-depressed individuals: a 6-year follow-up longitudinal study in a Korean cohort. Sleep. 2013;36:369–76. doi: 10.5665/sleep.2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136:743–50. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 30.Wong MM, Brower KJ. The prospective relationship between sleep problems and suicidal behavior in the National Longitudinal Study of Adolescent Health. J Psychiatr Res. 2012;46:953–9. doi: 10.1016/j.jpsychires.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li SX, Lam SP, Yu MW, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71:1440–6. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 32.Manber R, Bernert RA, Sooyeon S, Nowakowski S, Siebern AT, Ong JC. CBT for insomnia in patients with high and low depressive symptom severity: adherence and clinical outcomes. J Clin Sleep Med. 2011;7:645–52. doi: 10.5664/jcsm.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCall WV, Batson N, Webster M, et al. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. J Clin Sleep Med. 2013;9:135–40. doi: 10.5664/jcsm.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pigeon WR, Woosley JA, Lichstein KL. Insomnia and hypnotic medications are associated with suicidal ideation in a community population. Arch Suicide Res. 2014;18:170–80. doi: 10.1080/13811118.2013.824837. [DOI] [PubMed] [Google Scholar]
- 35.Lichstein KL, Durrence HH, Riedel BW, Taylor DJ, Bush AJ. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. Epidemiology of Sleep: Age, Gender, and Ethnicity. [Google Scholar]
- 36.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 37.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–3. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 38.Hoelscher TJ, Ware JC, Bond T. Initial validation of the Insomnia Impact Scale. Sleep Res. 1993;22:149. [Google Scholar]
- 39.Beck AT, Steer RA. Orlando, FL: Psychological Corporation; 1987. Beck Depression Inventory. [Google Scholar]
- 40.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 41.Steer RA, Rissmiller DJ, Ranieri WF, Beck AT. Use of the computer-administered Beck Depression Inventory and Hopelessness Scale with psychiatric inpatients. Comp Hum Behav. 1994;10:223–9. [Google Scholar]
- 42.Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;142:559–63. doi: 10.1176/ajp.142.5.559. [DOI] [PubMed] [Google Scholar]
- 43.Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9) Arthritis Care Res. 2011;63:S454–66. doi: 10.1002/acr.20556. [DOI] [PubMed] [Google Scholar]
- 44.Desseilles M, Perroud N, Guillaume S, et al. Is it valid to measure suicidal ideation by depression rating scales? J Affect Disord. 2012;136:398–404. doi: 10.1016/j.jad.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 45.Brown GK. Bethesda, MD: National Institute of Mental Health; 2000. A Review of Suicide Assessment Measures for Intervention Research with Adults and Older Adults. Available at http://www.hawaii.edu/hivandaids/Review of Suicide Assess for Interven Res w Adults and Older Adults.pdf. [Google Scholar]
- 46.Farabaugh A, Bitran S, Nyer M, et al. Depression and suicidal ideation in college students. Psychopathology. 2012;45:228–34. doi: 10.1159/000331598. [DOI] [PubMed] [Google Scholar]
- 47.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Palo Alto, CA: Consulting Psychologists Press; 1983. State-Trait Anxiety Inventory (Form Y) [Google Scholar]
- 48.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research—Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 49.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 50.Hayes AF. New York: Guilford Press; 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. [Google Scholar]
- 51.Green KL, Brown GK, Jager-Hyman S, Cha J, Steer RA, Beck AT. Long and short-term predictive validity of the Beck Depression Inventory suicide item. Poster presented at: 47th Annual Conference of the American Association of Suicidology; 2014 April 9-12; Los Angeles, CA. [Google Scholar]
- 52.Agargun MY, Cartwright R. REM sleep, dream variables and suicidality in depressed patients. Psychiatr Res. 2003;119:33–9. doi: 10.1016/s0165-1781(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 53.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 54.Joiner TE, Rudd MD. Disentangling the interrelations between hopelessness, loneliness, and suicidal ideation. Suicide Life Threat Behav. 1996;26:19–26. [PubMed] [Google Scholar]
- 55.McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Curr Psychiatry Rep. 2013;15:389. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


