A 47-year-old male with excessive daytime sleepiness was diagnosed with mild obstructive sleep apnea (apnea-hypopnea index 8) and presented to our sleep disorders clinic for routine follow-up after initiation of therapy. He had been initiated on CPAP at a pressure of 6 centimeters of water, heated humidification, pressure relief of 2, ramp time of 15 minutes, and a full face mask interface based on his preference during the PAP titration trial. He reported no problems with his machine or interface. His symptoms of daytime fatigue had dramatically improved. Review of data downloaded from his CPAP tracking systems revealed an apnea-hypopnea index of 4.0, use > 4 h on 77% of nights for all nights, and an average time in large leak of 4 h 48 min per day.
QUESTION:
Based on the compliance download
(Figure 1), what recommendation should you give the patient?
Perform mask refitting due to significant leak.
Refrain from drinking alcohol on the weekend as it appears he is turning his machine on but he is either not getting a good seal or forgetting to put his mask.
No changes indicated, continue with current therapy.
He has failed CPAP therapy and should be considered for an oral appliance.
ANSWER:
C. No changes indicated, continue with current therapy.
DISCUSSION
The patient practices Orthodox Judaism. In accordance with rabbinical law, electrical appliances should not be turned on or off during the Sabbath (Friday evening through Saturday evening). His data download (Figure 1) revealed an interesting pattern of large leak appearing only on the weekends (example of typical weekend see Figure 2). To refrain from violating the rabbinical law, the patient would leave his CPAP machine running throughout the day on the Sabbath so he would not have to turn it on in the evening. No use on a couple of days was noted and evidenced by large spaces between bars in Figure 1.
Figure 1. Compliance information graphic.
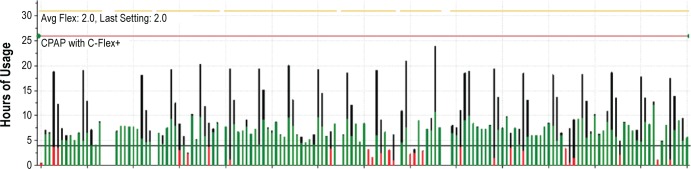
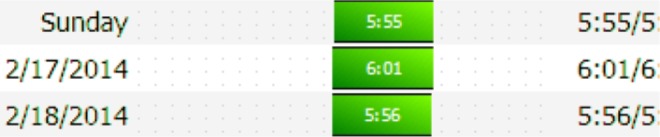
Figure 2. Typical weekday pattern of use obtained from download of CPAP compliance system.
Outcome measures such as mortality, quality of life, and daytime sleepiness are improved with increased CPAP adherence.1,2 Despite minimal data showing CPAP tracking systems improve OSA outcomes or improve CPAP adherence, review of data downloaded from CPAP tracking systems has become integral to the longitudinal care of patients with obstructive sleep apnea. The ATS statement on CPAP adherence tracking systems indicates CPAP adherence can be reliably determined, but residual events (apnea/hypopnea) and leak data from these systems are not easy to interpret. Further, the definitions of these parameters differ among manufacturers.3
Figure 2 reflects a normal usage pattern during the week and Figure 3 illustrates a typical weekend usage pattern for this patient obtained from the CPAP tracking system. He would turn his machine on Friday evening (start of the Sabbath). He would then permit his machine to run until the end of the Sabbath (Saturday evening). After this he would resume a normal pattern of having the machine on during times of usage. Black lines on the compliance information graphic and the patterns of use graphic correspond to either large leak or the machine being on but not attached to the patient. Green bars indicate usage of the device with the sum total for that day being a usage ≥ 4 h. Red bars indicate usage for that day being < 4 h of use. The number next to the bar for the pattern of usage indicates the number of hours and minutes CPAP was used with next number indicating the number of hours the CPAP machine was on (for instance, Figure 3: the machine was on for 18 hours and the patient used it a total of 7 h 9 min).
Figure 3. Typical weekend pattern of use obtained from download of CPAP compliance system.

Figure 4 is another weekend taken from the pattern of use data and the corresponding leak graphic for the Saturday of use. Minimal usage on Friday (i.e., < 4 h) is illustrated by the red bar. Color coding for the leak graphic includes black for leak with breathing not detected; light green for large leak; dark green for normal mask fit; and a blue line indicates the leak corresponding to y-axis in liters per minute. Again, leak data can be difficult to interpret. For instance, the second part of the leak graph shows a normal mask fit with a relatively large leak as indicated by the blue line. However, just after this leak, a light green area indicating large leak is associated with a relative small leak in terms of LPM. Making interpretation even more complex is that the black line may represent CPAP being on but not attached to the patient, or extremely large leak leading to the machine being unable to detect a patient's breathing.
Figure 4. Pattern of use data and the corresponding leak graphic for the Saturday of use downloaded from the patient's CPAP compliance system.

The numbers on right side of the patient download show the number of hours the patient used the machine followed by the number of hours the machine was turned on. Unfortunately our data download had a portion of the total amount of time the machine was on cut off. A typical download illustrating patient usage (left number) and total machine on time (right number) is shown in Figure 5. Figure 4 illustrates the fact that the black line is not associated with computation of the leak because the device believes it is not attached to the patient. Thus, a patient may use therapy and have a very large leak that may not be reported. In this case the total on time would be greater than the actual usage time. One could argue this fact may have—at least to a degree—been present in our case, and the decision to refit our patient's mask could also be considered appropriate. Importantly, time in large leak reported in the final summary of a data download corresponds to time with leak greater than twice the expected leak for the given pressure, and will not necessarily include the extremely large leak manifested as a black line and discussed above.
Figure 5. Illustration of a typical download including numbers on the right side of the download that correspond to time used by patient and total number of hours the machine is in use.
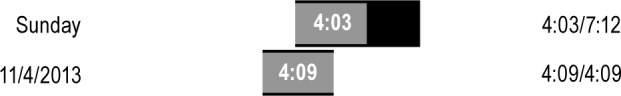
In this example on Sunday the patient used the machine for a total of 4 h 3 min, but the machine was either on and not attached to the patient, or extremely large leak was present during a portion of Sunday. Total on time for the machine was 7 h 12 min. The following day the patient used the machine a total of 4 h 9 min, and the machine was on a total of 4 h 9 min.
Despite a limited literature supporting the use of CPAP tracking systems, use of such systems intuitively makes sense. Physicians using this technology should be familiar with the benefits and current limitations of data management software when utilizing it to make clinical decisions. Our patient with mild sleep apnea presented with an overall improvement in daytime symptoms. Given his mild apnea, we were treating for symptom improvement. Further decreasing his already normalized AHI is not necessary. His average large leak of 4 h 48 min per day needs to be interpreted in the clinical context with the knowledge that leak data is not an exact science. Although the patient did have short bouts of large leak (as indicated by black lines) on non-weekend days, he did not complain of leak affecting compliance and AHI was normalized. Therefore it was felt no further intervention was needed. Given his clinical improvement and no concerns or complaints with CPAP usage including leak, no changes were made and current therapy was continued.
SLEEP MEDICINE PEARLS
CPAP adherence can be reliably determined, but residual events (apnea/hypopnea) and leak data from CPAP tracking systems are not easy to interpret, and the definitions of these parameters differ among manufactures.
Large leak found on data reviewed from CPAP tracking systems should be reviewed within the clinical context prior to suggesting interventions. In this example, the black bars represent either the machine running but not attached to the patient or a leak so high that the machine believes it is not being used.
Clinicians following OSA patients longitudinally should be familiar with the benefits and current limitations in using CPAP tracking systems to make clinical decisions.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Strollo has received grant support from ResMed, Philips Respironics, and Inspire Medical Systems and also serves as a consultant for Emmi Solutions, PinMed Inc., and the National Football League. Dr. Stansbury has indicated no financial conflicts of interest. All work was performed at the University of Pittsburgh Medical Center, Pittsburgh, PA. This manuscript does not report on off-label or investigational use of medical therapy.
CITATION
Stansbury RC, Strollo PJ. An unorthodox CPAP usage pattern. J Clin Sleep Med 2014;10(11):1241-1243.
REFERENCES
- 1.Campos-Rodriguez F, Peña-Griñan N, Reyes-Nuñez N, et al. Mortality in obstructive sleep apnea-hypopnea patients treated with positive airway pressure. Chest. 2005;128:624–33. doi: 10.1378/chest.128.2.624. [DOI] [PubMed] [Google Scholar]
- 2.Antic NA, Catcheside P, Buchan C, Asdfasd, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34:111–9. doi: 10.1093/sleep/34.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwab RJ, Badr SM, Epstein LJ, et al. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188:613–20. doi: 10.1164/rccm.201307-1282ST. [DOI] [PMC free article] [PubMed] [Google Scholar]


