Abstract
Objective
The current study provides the first measure of pain-related fear for pediatric headache patients.
Methods
From a large pediatric headache clinic a cross-sectional cohort of 206 children and adolescents completed measures of pain-related fear, anxiety sensitivity, catastrophizing, pain acceptance, functional disability, and school functioning.
Results
The two-factor solution of the FOPQ was confirmed from the originally derived structure with pediatric headache patients. Simultaneously regressing FOPQ subscales Fear of Pain and Activity Avoidance on theorized construct validity measures demonstrated that Fear of Pain was more closely linked with anxiety sensitivity and pain catastrophizing while Activity Avoidance had a strong negative association with pain acceptance (activity engagement and pain willingness). Pain-related fear was not significantly associated with pain level. After controlling for demographic factors and pain, Fear of Pain and Activity Avoidance accounted for an additional 26% of the variance in functional disability and school functioning outcomes, with Activity Avoidance accounting for much of this relationship.
Conclusions
Although typically considered an influential construct among musculoskeletal patients, pain-related fear is also an important factor influencing functioning among pediatric headache patients, with the dimension of activity avoidance particularly salient.
Keywords: headache, pain-related fear, children, adolescents, assessment, pain acceptance, anxiety sensitivity, pain-related disability
Introduction
Median prevalence rates of children and adolescents who suffer from headache pain range from 8% for migraine with and without aura to 25% for tension-type headache (1). Although several studies have identified heightened negative affectivity among pediatric headache sufferers (2) and higher levels of disability and poorer quality of life among pediatric headache patients with psychiatric comorbidities (3), pain-specific distress variables have yet to be explored. For example, pain-related fear occurs when stimuli related to pain are perceived as threatening wherein individuals develop fear of pain, reinjury, and/or physical activity and as a result engage in escape/avoidance behaviors that exacerbate pain and promote pain-related disability (4, 5). Pain-related fear is an important psychological factor associated with poor outcomes in children suffering from chronic pain (6, 7). Although it has typically been considered an influential construct among musculoskeletal patients, converging evidence supports the importance of pain-related fear among headache sufferers. Early work identified pain-related fear as not only associated with psychological outcomes such as general anxiety and depression, but also on disruption of life activities among adult headache patients (8). More recent work has identified a high prevalence of maladaptive fear learning in tension type headaches (9). Evidence for an intensified level of avoidance behavior is also accumulating, with high levels of kinesiophobia linked to migraine patients (10). Both Norton (11) and Asmundson (12) have examined adult recurrent headache populations, finding positive associations with fear of pain and anxiety sensitivity (ie., the distress related to the potential sensations and consequences associated with anxiety (13)), suggesting potential application of the Fear Avoidance Model (5) among headache patients.
Despite findings that support heightened fear avoidance and fear learning among adults with headaches, pain-related fear has not been examined in pediatric headache nor do we know if our existing measure of fear avoidance in children with chronic pain applies for headache. A recent study among German children with headache pain did examine pain catastrophizing, a construct considered to predispose individuals to elevated pain-related fear. Investigators not only found significant links between catastrophizing and disability and pain, but after controlling for psychological factors known to be associated with pain outcomes (internalizing symptoms, anxiety sensitivity) catastrophizing continued to be a significant predictor of disability outcomes (14). These initial findings coupled with evidence among adults with persistent headache pain suggest that further work in this area is needed.
The objective of the current study was to validate the Fear of Pain Questionnaire (FOPQ) (15) in a pediatric headache sample. In addition to measures that have been previously examined with the FOPQ, the current study examined convergent validity with anxiety sensitivity and divergent validity with pain acceptance. Lastly, we will examine criterion-related validity with FOPQ scores predicting functional disability and school functioning. We hypothesized that 1) the original two-factor structure derived would be confirmed, with equivalent levels of Activity Avoidance and Fear of Pain as compared to children with primarily neuropathic and musculoskeletal pain, 2) FOPQ scores would be positively associated with anxiety sensitivity and catastrophizing and negatively associated with pain acceptance, and 3) pain-related fear would be a significant predictor of functional disability and school functioning after controlling for potentially influential demographic and pain-related variables.
Method
Participants
English speaking patients 8-17 years of age who underwent a multidisciplinary headache evaluation at a tertiary care pediatric headache clinic in a larger, urban northeast US pediatric hospital were eligible for this cross-sectional cohort study. Of 238 eligible patients, 209 consented patients, and 206 patients had sufficient data for analysis. Primary reason for declining was lack of time or interest. Children in the study were predominantly Caucasian (89.8%) and female (72.8%). Mean child age was 13.6 years. Physician-assigned headache diagnoses for patients included: 26.2 % tension and migraine, 24.8% migraine, 23.3% tension-type headache, 12.1% other primary headache disorders (largely new daily persistent headache), 7.8% attributed to trauma or injury to the head/neck, and 5.8% other (e.g., painful cranial neuropathies). Length of time since onset of pain ranged from 1 to 194 months, with median duration of 19 months. Parents of participating children were generally married (78.6%). Family socioeconomic status (SES) based on the four-factor index of social status ranged from 12 (laborer) to 66 (business owner; professional), with a mean of 46.3 (SD = 12.8), thus on average, families were upper middle class.
Procedure
All participant families who presented for a headache clinic appointment within a large children's hospital from September 2011- June 2013 were invited to participate in this study. The study was approved by the hospital's Institutional Review Board. Patients and their parents were approached by a research assistant during their evaluation and asked to consent/assent to completing the research measures as well as give permission for their responses to clinic measures to be used for research purposes. All measures were completed separately.
Measures
Basic demographic (e.g, age, gender) and medical information (e.g., diagnosis assigned by the evaluating neurologist) were collected from patient charts.
Pain
During the pain evaluation, children were asked to provide their average pain rating on a standard 11-point numeric rating scale (16) from 0 (no pain) to 10 (most pain possible)(17).
Pain-related fear
The Fear of Pain Questionnaire (FOPQ-C) (15)assesses child pain-related fears. The FOPQ-C consists of 24 items with strong internal consistency among patients with neuropathic and musculoskeletal pain (α = .92). This measure has two subscales: Fear of Pain (α = .89) and Avoidance of Activities (α = .86). Specific items include: “I try to avoid activities that cause my pain” (avoidance) and “Feelings of pain are scary to me” (fear). It is rated on a 5-point scale from 0= strongly disagree to 4= strongly agree. Items are summed to derive a total score. Higher scores indicate high levels of pain-related fear.
Construct validity
Anxiety Sensitivity
The Children's Anxiety Sensitivity Index (CASI) (18) is an 18-item self-report scale that measures the level of anxiety sensitivity in children and adolescents. Patients rate how negatively they view anxiety symptoms (i.e. “It scares me when my heart beats fast”, “Unusual feelings in my body scare me”) on a scale of 1 (“none”) to 3 (“a lot”). There are three domains included in the CASI that encompass physical, psychological and social concerns. Total CASI score results from the summation of all items where higher scores are indicative of higher levels of anxiety sensitivity. The CASI has demonstrated strong internal consistency (α=.87).
Pain catastrophizing
The Pain Catastrophizing Scale (PCS-P) (19) assesses negative thinking associated with pain. It is comprised of 13 items rated on a 5-point scale. Items are summed with higher scores indicated higher levels of catastrophic thinking. The PCS-C has strong internal consistency (α=.87) and demonstrated validity (19).
Acceptance
The Chronic Pain Acceptance Questionnaire, adolescent report (CPAQ-A)(20) is a 20-item measure consisting of two subscales: activity engagement (11 items) and pain willingness (9 items). Activity engagement reflects the degree of participation in regular daily activities in the presence of pain (e.g., “My life is going well, even though I have chronic pain”). Pain willingness reflects the absence of attempts to avoid or control pain (e.g., “I avoid putting myself in situations where my pain might increase” – reverse keyed). Previous research supports the internal consistency (α=.87), factor structure, and validity of the CPAQ-A (21).
Criterion-related validity
Functional disability
The Functional Disability Inventory (FDI)(22) is a scale that assesses difficulty in physical and psychosocial functioning due to physical health. The instrument consists of 15 items concerning perceptions of activity limitations during the past two weeks; total scores are computed by summing the items. Higher scores indicate greater disability. The FDI has strong internal consistency (males α=.86; females α=.91), reliability, and validity (23) .
School functioning
The Pediatric Quality of Life Inventory (24) is a scale that assesses several domains of life function. The 5-item parent-report School Functioning subscale was used for these analyses. Internal consistency for this subscale is .76 with validity data supporting the use of this measure among medically ill and healthy children (24) and children with pain (25).
Statistical Analyses
Data were entered into SPSS version 21.0. Descriptive statistics examining item skew and kurtosis were conducted to examine underlying assumptions of normality for all variables of interest. Item-total correlations were calculated for the FOPQ-C. Confirmatory factor analysis (CFA) was then conducted to test the fit of the derived model for the FOPQ-C. Factor analytic rule-of-thumb generally suggests 5-10 subjects per item (26), with others suggesting that a sample size of 200 is sufficient for analyses of less than 40 items (27). With 24 items, we have approximately 8 subjects per item for our analyses. The CFA was conducted with AMOS for SPSS version 21. CFA is a type of structural equation modeling (SEM) that examines the fit between a predetermined factor structure, derived from EFA or prior research, and the sample data. A model was specified that included the items and corresponding factors based on the initial validation study (15). Questionnaire items were treated as continuous variables in the CFA, consistent with the Likert-type format of the response options. Full information maximum likelihood estimation (FIML) was employed. Based on recommendations by Bentler and Bonett (28) and Ullman(29) the following statistics were used to evaluate model fit:χ2, χ2/df (<2 acceptable), Comparative Fit Index (CFI; >.90 acceptable, >.95 excellent), and Root Mean Square Error of Approximation (RMSEA; <.08 acceptable, <.05 excellent). In order to examine potential modification indices individuals with missing data on any items were dropped from analyses, thus n=189 were submitted for the CFA.
Relations with demographic, pain-related variables and FOPQ-C were examined with bivariate correlations and one-way ANOVAs. A multiple regression model was tested in structural equation modeling in which child anxiety sensitivity, pain catastrophizing, activity engagement, and pain willingness were simultaneously regressed on the 2 FOPQ factors (Fear of Pain and Activity Avoidance) in a single model to assess the construct validity of the FOPQ. We decided to test these associations in structural equation modeling rather than in a regression analysis as given the ability of structural equation modeling to test for multiple associations simultaneously and to identify the unique relations between our subscales and construct validity variables. We examined criterion-related validity of the FOPQ using regression analyses. In the first step of the regression analyses, we entered all relevant demographic and pain variables that were significant at the bivariate level. In the second step we entered Fear of Pain and in the third step we entered Activity Avoidance. This was driven by the theoretical position that Fear of Pain leads to Avoidance of Activities in the Fear Avoidance Model.
Results
Scale internal consistency
Each of the 24 items was examined to determine their contribution to the scale. No items violated assumptions of normality (skew and/or kurtosis >2.0) Next, item-total correlations were conducted with corrected item-total correlations ranging from .53 to .73.
Confirmatory factor analysis
The two-factor model was tested with structural equation modeling in order to verify the factor structure among pediatric headache patients and examine overall model fit. The model provided modest fit to the data [χ2(251) = 646.3, p<.01; χ2/df = 2.5; CFI = .84, RMSEA = .087 (90% CI =0.079-.096)]. Modification indices were examined to determine whether any changes could be made to the model to improve fit. The modification indices suggested that adding error covariances for pairs of items would improve model fit. Two pairs that were consistent with the two subscales were selected (item 10 “I cannot go back to school until my pain is treated” with item 21 “I do not go to school because it makes my pain worse” and item 4 “When I feel pain, I am afraid something terrible will happen” with “Feelings of pain are scary for me”). With these modifications, model fit improved [χ2(249) = 537.7, p<.01; χ2/df = 2.2; CFI = .88, RMSEA = .079 (90% CI =0.069-.088)]. All factor loadings were significant. See Figure 1 for the CFA model, including factor loadings and error covariances.
Figure 1.
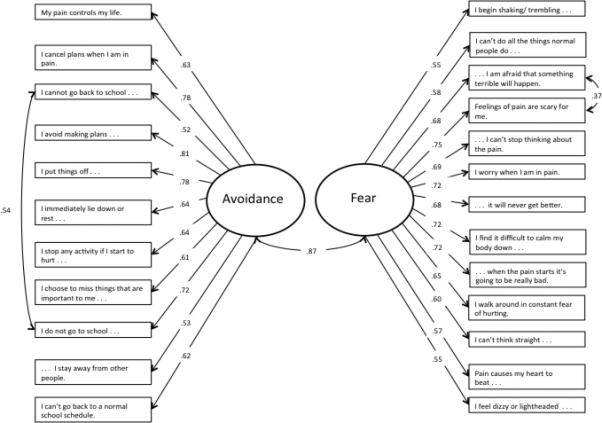
Factor loadings of the FOPQ=C with headach patients.
In order to further assess the appropriateness of the current model, the proposed two-factor solution was compared to an alternative model in which all items loaded on a single factor. The single-factor model resulted in a significant deterioration in model fit when compared to the two-factor model (Δχ2(1) = 177.23, p < .001), indicating that the two-factor solution provided significantly better fit to the data.
The total FOPQ scale had a Cronbach's alpha of .94. Sample mean for the scale was 37.4 (SD =18.9). FOPQ total scores were normally distributed across the sample. Fear of Pain consisted of 13 items (α = .90) and Activity Avoidance consisted of 11 items (α = .90). The two subscales were strongly intercorrelated, r = .78, p < .01. Scores on the Activity Avoidance subscale (M=18.3, SD=9.5) were commensurate with results in the chronic pain FOPQ validation sample (M=18.9, SD=9.0)(15). Scores on the Fear of Pain subscale (M=19.1, SD=10.6) were significantly lower compared to the musculoskeletal and neuropathic chronic pain validation sample (M=23.9, 10.7)(15), t(500)=5.03, p<.01.
FOPQ and demographic factors
One-way ANOVAs were conducted to examine differences in FOPQ subscale scores across categorical demographic factors, pain duration, and pain diagnosis. Older age was associated with greater Activity Avoidance (r=.20, p<.01). Females reported more Activity Avoidance (M=19.1, SD=9.7) compared to their male counterparts (M=16.1, SD=8.3), f(1,204)=4.54, p <.05. Lastly, children of divorced, separated, or single parents reported significantly higher Activity Avoidance (M=21.7, SD=9.0) compared to children of married parents (M=17.4, SD=9.4), p=.01. No differences or relations emerged for Fear of Pain and age (r=.11, ns), gender (p=.13), and parent marital status (p=.18). FOPQ subscale scores were not associated with duration of pain (p >.23) and did not significantly differ across headache diagnostic groups (p >.83). Pain levels were modestly correlated with Activity Avoidance (average pain r=.21, p<.01; current pain r=.20, p=.01; lowest pain r=.06, ns; highest pain r=.25, p<.01) and Fear of Pain (average pain r=.24, p<.01; current pain r=.18, p=.01; lowest pain r=.11, ns; highest pain r=.26, p<.01).
FOPQ construct validity
Means and standard deviations of all study variables are provided in Table 1. A multiple regression model was tested in structural equation modeling in which pain level (using average pain), child anxiety sensitivity, pain catastrophizing, activity engagement, and pain willingness were simultaneously regressed on the two FOPQ factors, Fear of Pain and Activity Avoidance. Regression coefficients are provided in Table 2. For convergent validity, the cognitive constructs of anxiety sensitivity and pain catastrophizing were more strongly associated with high levels of Fear of Pain. For discriminant validity, lower levels of activity engagement and less pain willingness were more strongly associated with Activity Avoidance. Fear of Pain was also significantly associated with Pain Willingness, but minimally related to Activity Engagement. Pain ratings were not strongly associated with either subscale. This further underscores the two related, yet distinct dimensions measured by the Fear of Pain Questionnaire that are not dependent on pain levels.
Table 1.
Descriptive statistics of all study variables
| Variable | Mean | SD | n |
|---|---|---|---|
| FOPQ Fear of pain | 23.9 | 10.7 | 206 |
| FOPQ Activity Avoidance | 18.3 | 9.02 | 206 |
| Anxiety sensitivity | 20.4 | 4.93 | 202 |
| Pain willingness | 28.5 | 5.37 | 204 |
| Activity engagement | 26.6 | 7.76 | 206 |
| Pain catastrophizing | 22.4 | 10.8 | 205 |
| Functional disability | 17.7 | 11.1 | 201 |
| School functioning | 52.1 | 22.7 | 196 |
Table 2.
Construct validity of the Fear of Pain Questionnaire
| Fear of Pain Questionnaire | ||
|---|---|---|
| Variables | Fear of Pain | Activity Avoidance |
| Anxiety sensitivity | .37** | .22** |
| Pain catastrophizing | .45** | .23** |
| Pain | .06 | .03 |
| Activity engagement | −.02 | −.34** |
| Pain willingness | −.33** | −49** |
Note.
*p < 0.05
p < 0.01, Listed above are standardized regression coefficients from structural equation modeling where all variables were simultaneous regressed on the two FOPQ subscales.
To examine criterion-related validity of the FOPQ, we conducted two separate linear regression analyses predicting functional disability and school functioning detailed in Table 3. Given the strong relationship between the two FOPQ dimensions, we tested for multicollinearity for Fear of Pain (Tolerance=.39; VIF=2.56) and Activity Avoidance (Tolerance=.38; VIF=2.67), with both in the acceptable range. For both models, we included in the first step demographic and pain variables that were significant at the bivariate level; thus in Step 1 for both models age, gender, parent marital status, and pain were entered. Only pain emerged as a significant predictor of functional disability. In Step 2, Fear of Pain was entered with both pain and Fear of Pain emerging as significant predictors. Lastly, we entered Activity Avoidance. With all variables in the model, only pain and Activity Avoidance emerged as significant predictors of functional disability. An additional 26% of the variance in functional disability was explained with the addition of Fear of Pain and Activity Avoidance in the model. In predicting school functioning, age, gender, parent marital status, and pain were entered in Step 1, . Only older age emerged as a significant predictor of school impairment. In Step 2, Fear of Pain was entered with both age and Fear of Pain emerging as significant predictors. Lastly, we entered Activity Avoidance. With all variables in the model, only age and Activity Avoidance emerged as significant predictors of school functioning. An additional 26% of the variance in school functioning was explained with Fear of Pain and Activity Avoidance included in the model.
Table 3.
Fear of Pain predicting functional disability and school functioning
| Variables | Beta | T | R2 change |
|---|---|---|---|
| Functional Disability | |||
| Step 1 | .10** | ||
| Age | .06 | .79 | |
| Gender | .12 | 1.76 | |
| Parent marital status | .13 | 1.87 | |
| Average pain | 24** | 3.47** | |
| Step 2 | .18** | ||
| Age | .03 | .51 | |
| Gender | .09 | 1.42 | |
| Parent marital status | .09 | 1.51 | |
| Average pain | .15* | 2.29* | |
| Fear of Pain | .43** | 6.84** | |
| Step 3 | .06** | ||
| Age | −.01 | −.21 | |
| Gender | .06 | 1.02 | |
| Parent marital status | .05 | .77 | |
| Average pain | .14* | 2.26* | |
| Fear of Pain | .14 | 1.48 | |
| Activity Avoidance | .39** | 3.97** | |
| School Functioning | |||
| Step 1 | .08** | ||
| Age | −.23** | −3.15** | |
| Gender | −.03 | −.40 | |
| Parent marital status | −.06 | −.81 | |
| Average pain | −.13 | −1.80 | |
| Step 2 | .07** | ||
| Age | −.21** | −3.05** | |
| Gender | −.01 | −.14 | |
| Parent marital status | −.04 | −.59 | |
| Average pain | −.07 | −.93 | |
| Fear of Pain | −27** | −3.91** | |
| Step 3 | .14** | ||
| Age | −.14 | −2.19* | |
| Gender | .03 | .41 | |
| Parent marital status | .03 | .50 | |
| Average pain | −.06 | −.98 | |
| Fear of Pain | .19* | 1.91* | |
| Activity Avoidance | −.62** | −6.14** |
p =< 0.05
p < 0.01. All standardized Beta and t-values are from the final model with all variables included; R2 change is derived from each step of the model.
Discussion
The aim of the current study was to validate the Fear of Pain Questionnaire (FOPQ) in a pediatric headache sample. While evidence exists supporting the relevance of the fear-avoidance model in adult tension headache and migraine patients (9, 11, 12), this is the first study to our knowledge to examine pain-related fear in children and adolescents with headache.
Results revealed that the 24-item, 2-factor structure of the FOPQ derived in a diverse pediatric chronic pain sample was upheld among pediatric headache patients. Internal consistency of the two subscales, Fear of Pain and Activity Avoidance, were strong and significantly correlated; however, a one-factor structure led to deterioration of model fit and was rejected. Thus, while these two constructs are related, they are still distinct. Skewness and kurtosis of all items were within normal range, supporting the relevance of all FOPQ items with headache patients.
Consistent with findings in adult headache (8), pediatric headache patients reported high levels of fear of pain and activity avoidance. Interestingly, patients with headache reported similar levels of activity avoidance as children and adolescents with musculoskeletal and neuropathic pain, but endorsed lower levels of fear compared to their musculoskeletal and neuropathic counterparts. Some of the items from the Fear of Pain subscale (eg. “I can't do all the things normal people do because it's so easy to hurt my body”) are movement based and may be less endorsed by headache patients who are more concerned about other dimensions of pain-related fear associated with the cognitive demands and stresses on the Fear of Pain subscale (eg. “I can't think straight when I’m in pain”).
Although fear of pain did not differ across demographic and medical variables, patients who were older, female, or from non-intact (divorced/separated/or single) parent homes had higher levels of activity avoidance; thus identifying potential risk factors for this dimension of pain-related fear. The relationship between older age and greater activity avoidance observed in this sample is consistent with previous findings in a pediatric musculoskeletal and neuropathic pain population (15). This may reflect the potential chronicity of headache pain that can evolve in adolescence (30) or perhaps suggests the development of avoidant response patterns at the onset or anticipation of headache symptoms maintained through fear learning (31) among older children. Higher levels of avoidance among females may represent cultural norms of higher expectations for boys to function in the presence of pain or may perhaps reflect gender differences in underlying neural circuits (e.g. greater use of emotional circuitry compared to sensory processing in women) that may contribute to more impairment in females (32). With regards to non-intact families, it is possible that inconsistent parent responses to headache episodes may contribute to higher levels of activity avoidance, as protective parenting is consistently associated with poor outcomes (e.g., (33)). Although there were no significant differences across headache subtypes, this may be due to the small size of each group in the contrast. Patients who experienced headaches attributed to trauma or injury to the head/neck (post-concussive headache) did report relatively higher levels of Fear of Pain, but with only 16 patients in the group, the variance within the group precluded finding any significant differences between groups. Given the often inconsistent nature of demographic factors and pain-related outcomes, it is important to replicate these results in future studies among pediatric headache patients in order to solidify a relationship between FOPQ scores and demographic factors.
In examining the multiple regression model of FOPQ construct validity relationships were consistent with our hypotheses. The cognitive constructs of anxiety sensitivity and pain catastrophizing were more strongly associated with Fear of Pain than Activity Avoidance. We also found that Activity Avoidance was more strongly related to lower levels of pain acceptance as assessed by activity engagement and pain willingness. Notably, both FOPQ subscales were not associated with pain ratings when accounting for other variables in the model, revealing that fear of pain and activity avoidance are pertinent dimensions of the pediatric headache experience independent of pain severity.
We found that pain-related fear predicted a quarter of the variance in both functional disability and school impairment, after accounting for pertinent demographic variables and pain level. Of particular salience among pediatric headache patients was avoidance of activities. Once avoidance of activities was included in the model, the fear of pain subscale was no longer a significant predictor of outcome. This is consistent with the pediatric application of the Fear Avoidance Model of Chronic Pain (6) where avoidance of activities is a more proximal link to functional outcomes, but fear of pain is an essential precursor to avoidance with the two constructs highly correlated, yet distinct. While much of the initial FAM work involved low back pain patients(4), it has since successfully expanded to both adult headache sufferers (12) and IBS patients(34),with evidence that that similar mechanisms are at play for children(6). These findings support application of the Fear Avoidance Model (FAM) in children and adolescents with headache, yet what continues to be remiss and needs to be expanded upon is the role of parent catastrophizing and fear in the development and maintenance of pain-related fear in children (35, 36).
With regards to study limitations, all measures were collected at one time-point, thus we were unable to examine test-retest reliability or treatment sensitivity, both important next steps for this measure among headache patients. While the sample is primarily comprised of female and Caucasian patients, this is generally reflective of the demographic characteristics of pediatric headache patients (1). In assessing the chronicity of headache pain, we did not include frequency of headaches and this is potentially important given the episodic nature of headache pain for many patients. Additionally, there may also be other questions that include fears and worries unique to headache patients (e.g. exposure to bright light or attending a movie with loud noise), which are not included in the original FOPQ. It may be worthwhile to create a headache-specific module that assesses these additional concerns and may increase sensitivity to detecting fear avoidant beliefs or behaviors among headache patients. Although there may be items that are less relevant for pediatric headache patients, only one item had a mean difference of greater than 1.0 (“I can't do all things that normal people do because it's so easy to hurt my body”) compared to the general chronic pain validation sample (14). Additionally, the item-total correlations for all items of the FOPQ in this sample were above .53, suggestive of strong construct consistency.
Overall the FOPQ is a psychometrically sound measure for children and adolescents with headache. It captures the multidimensional nature of fear avoidance and provides a brief tool for clinicians and researchers to utilize in the assessment and treatment of pediatric patients suffering from persistent headache pain and associated disability. Future studies should explore the application of exposure-based treatments that target pain-related fear (37) for pediatric headache patients. This treatment approach as been applied to neck injury patients (38), but to our knowledge has not been used for headache patients. Given the individually-tailored nature of graded invivo exposure, this treatment approach could be easily adapted for this population. The findings of this study supplement the state of the fear-avoidance literature by verifying the existence and importance of pain-related fear and fear avoidance behaviors among pediatric headache sufferers. The role of psychosocial factors, including pain-related fear and activity avoidance, in the maintenance and exacerbation of migraine and tension headache in children and adolescents should not be overlooked.
Clinical Implications.
Pain-related fear is a robust predictor of functional disability and school impairment among children and adolescents suffering from headache pain.
The Fear of Pain Questionnaire (FOPQ) is a brief and valid tool for assessing levels of pain-related fear in children with headache.
Screening for pain-related fear can lead to the implementation of targeted treatment that focuses directly on exposing headache patients to feared and avoided activities.
Delivering targeted treatments that extinguish maladaptive fear learning patterns can potentially lead to improved coping in the face of subsequent headache episodes and reduce pain-related disability in children and adolescents with headache.
Acknowledgements
The authors wish to thank Sharon Segal, MA for her assistance on this study. This investigation was supported by NIH grant K23HD067202 (LS), the Sara Page Mayo Endowment for Pediatric Pain Research and Treatment, and the Department of Anesthesiology, Perioperative and Pain Medicine at Children's Hospital Boston.
Footnotes
There are no conflicts of interest to report.
References
- 1.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152:2729–38. doi: 10.1016/j.pain.2011.07.016. 2011. [DOI] [PubMed] [Google Scholar]
- 2.Kroner-Herwig B. Pediatric headache: associated psychosocial factors and psychological treatment. Current pain and headache reports. 2013;17:338. doi: 10.1007/s11916-013-0338-7. 2013. [DOI] [PubMed] [Google Scholar]
- 3.Slater SK, Kashikar-Zuck SM, Allen JR, LeCates SL, Kabbouche MA, O'Brien HL, et al. Psychiatric comorbidity in pediatric chronic daily headache. Cephalalgia : an international journal of headache. 2012;32:1116–22. doi: 10.1177/0333102412460776. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–32. doi: 10.1016/S0304-3959(99)00242-0. 2000. [DOI] [PubMed] [Google Scholar]
- 5.Vlaeyen JW, Linton SJ. Fear-avoidance model of chronic musculoskeletal pain: 12 years on. Pain. 2012;153:1144–7. doi: 10.1016/j.pain.2011.12.009. 2012. [DOI] [PubMed] [Google Scholar]
- 6.Simons LE, Kaczynski KJ. The fear avoidance model of chronic pain: examination for pediatric application. J Pain. 2012;13:827–35. doi: 10.1016/j.jpain.2012.05.002. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilson AC, Lewandowski AS, Palermo TM. Fear-avoidance beliefs and parental responses to pain in adolescents with chronic pain. Pain research & management : the journal of the Canadian Pain Society = journal de la societe canadienne pour le traitement de la douleur. 2011;16:178–82. doi: 10.1155/2011/296298. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hursey KG, Jacks SD. Fear of pain in recurrent headache sufferers. Headache. 1992;32:283–6. doi: 10.1111/j.1526-4610.1992.hed3206283.x. 1992. [DOI] [PubMed] [Google Scholar]
- 9.Klinger R, Matter N, Kothe R, Dahme B, Hofmann UG, Krug F. Unconditioned and conditioned muscular responses in patients with chronic back pain and chronic tension-type headaches and in healthy controls. Pain. 2010;150:66–74. doi: 10.1016/j.pain.2010.03.036. 2010. [DOI] [PubMed] [Google Scholar]
- 10.Martins IP, Gouveia RG, Parreira E. Kinesiophobia in migraine. J Pain. 2006;7:445–51. doi: 10.1016/j.jpain.2006.01.449. 2006. [DOI] [PubMed] [Google Scholar]
- 11.Norton PJ, Asmundson GJ. Anxiety sensitivity, fear, and avoidance behavior in headache pain. Pain. 2004;111:218–23. doi: 10.1016/j.pain.2004.06.018. 2004. [DOI] [PubMed] [Google Scholar]
- 12.Asmundson GJ, Norton PJ, Veloso F. Anxiety sensitivity and fear of pain in patients with recurring headaches. Behaviour research and therapy. 1999;37:703–13. doi: 10.1016/s0005-7967(98)00172-7. 1999. [DOI] [PubMed] [Google Scholar]
- 13.Asmundson GJ, Taylor S. Role of anxiety sensitivity in pain-related fear and avoidance. Journal of behavioral medicine. 1996;19:577–86. doi: 10.1007/BF01904905. 1996. [DOI] [PubMed] [Google Scholar]
- 14.Kroner-Herwig B, Maas J. The German Pain Catastrophizing Scale for Children (PCS-C) - psychometric analysis and evaluation of the construct. Psycho-social medicine. 2013;10 doi: 10.3205/psm000097. (2013):Doc07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simons LE, Sieberg CB, Carpino E, Logan D, Berde C. The Fear of Pain Questionnaire (FOPQ): assessment of pain-related fear among children and adolescents with chronic pain. J Pain. 2011;12:677–86. doi: 10.1016/j.jpain.2010.12.008. 2011. [DOI] [PubMed] [Google Scholar]
- 16.Varni JW, Thompson KL, Hanson V. The Varni/Thompson Pediatric Pain Questionnaire: I. Chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain. 1987;28:27–38. doi: 10.1016/0304-3959(87)91056-6. 1987. [DOI] [PubMed] [Google Scholar]
- 17.von Baeyer CL, Spagrud LJ, McCormick JC, Choo E, Neville K, Connelly MA. Three new datasets supporting use of the Numerical Rating Scale (NRS-11) for children's self-reports of pain intensity. Pain. 2009;143:223–7. doi: 10.1016/j.pain.2009.03.002. 2009. [DOI] [PubMed] [Google Scholar]
- 18.Silverman WK, Fleisig W, Rabian B, Peterson RA. Child Anxiety Sensitivity Index. Journal of Clinical Child Psychology. 1991;20:162–8. 1991. [Google Scholar]
- 19.Crombez G, Bijttebier P, Eccleston C, Mascagni T, Mertens G, Goubert L, Verstraeten K. The child version of the pain catastrophizing scale (PCS-C): a preliminary validation. Pain. 2003;104:639–46. doi: 10.1016/S0304-3959(03)00121-0. 2003. [DOI] [PubMed] [Google Scholar]
- 20.McCracken LM, Gauntlett-Gilbert J, Eccleston C. Acceptance of pain in adolescents with chronic pain: validation of an adapted assessment instrument and preliminary correlation analyses. European journal of pain. 2010;14:316–20. doi: 10.1016/j.ejpain.2009.05.002. 2010. [DOI] [PubMed] [Google Scholar]
- 21.Wallace DP, Harbeck-Weber C, Whiteside SP, Harrison TE. Adolescent acceptance of pain: confirmatory factor analysis and further validation of the chronic pain acceptance questionnaire, adolescent version. J Pain. 2011;12:591–9. doi: 10.1016/j.jpain.2010.11.004. 2011. [DOI] [PubMed] [Google Scholar]
- 22.Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol. 1991;16:39–58. doi: 10.1093/jpepsy/16.1.39. 1991. [DOI] [PubMed] [Google Scholar]
- 23.Claar RL, Walker LS. Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain. 2006;121:77–84. doi: 10.1016/j.pain.2005.12.002. 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Varni JW, Seid M, Rode CA. The PedsQL: measurement model for the pediatric quality of life inventory. Medical care. 1999;37:126–39. doi: 10.1097/00005650-199902000-00003. 1999. [DOI] [PubMed] [Google Scholar]
- 25.Chann E, Piira T, Betts G. The school functioning of children with chronic and recurrent pain. Pediatric Pain Letter. 2005;7:11–6. 2005. [Google Scholar]
- 26.Tinsley HE, Tinsley DJ. Uses of factor analysis in counseling psychology research. Counseling Psychology Research. 1987;34:414–24. 1987. [Google Scholar]
- 27.Comrey AL. Factor-analytic methods of scale development in personality and clinical psychology. Journal of consulting and clinical psychology. 1988;56:754–61. doi: 10.1037//0022-006x.56.5.754. 1988. [DOI] [PubMed] [Google Scholar]
- 28.Bentler PM, Bonett DG. Significance tests and goodness-of-fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–600. 1980. [Google Scholar]
- 29.Ullman JB. Structural equation modelling. 4th ed. Allyn and Bacon; Boston: 2001. [Google Scholar]
- 30.Lu SR, Fuh JL, Wang SJ, Juang KD, Chen SP, Liao YC, Wang YF. Incidence and risk factors of chronic daily headache in young adolescents: a school cohort study. Pediatrics. 2013;132:e9–e16. doi: 10.1542/peds.2012-1909. 2013. [DOI] [PubMed] [Google Scholar]
- 31.Flor H. New developments in the understanding and management of persistent pain. Current opinion in psychiatry. 2012;25:109–13. doi: 10.1097/YCO.0b013e3283503510. 2012. [DOI] [PubMed] [Google Scholar]
- 32.Maleki N, Linnman C, Brawn J, Burstein R, Becerra L, Borsook D. Her versus his migraine: multiple sex differences in brain function and structure. Brain : a journal of neurology. 2012;135:2546–59. doi: 10.1093/brain/aws175. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kaczynski KJ, Claar RL, Lebel AA. Relations between pain characteristics, child and parent variables, and school functioning in adolescents with chronic headache: a comparison of tension-type headache and migraine. J Pediatr Psychol. 2013;38:351–64. doi: 10.1093/jpepsy/jss120. 2013. [DOI] [PubMed] [Google Scholar]
- 34.Craske MG, Wolitzky-Taylor KB, Labus J, Wu S, Frese M, Mayer EA, Naliboff BD. A cognitive-behavioral treatment for irritable bowel syndrome using interoceptive exposure to visceral sensations. Behaviour research and therapy. 2011;49:413–21. doi: 10.1016/j.brat.2011.04.001. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Asmundson GJ, Noel M, Petter M, Parkerson HA. Pediatric fear-avoidance model of chronic pain: foundation, application and future directions. Pain research & management : the journal of the Canadian Pain Society = journal de la societe canadienne pour le traitement de la douleur. 2012;17:397–405. doi: 10.1155/2012/908061. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goubert L, Simons LE. Cognitive styles and processes in paediatric pain. In: McGrath P, Stevens B, Walker S, Zemsky W, editors. Oxford textbook of paediatric pain. Oxford University Press; Oxford, UK: 2014. pp. 95–101. [Google Scholar]
- 37.Leeuw M, Goossens ME, van Breukelen GJ, de Jong JR, Heuts PH, Smeets RJ, et al. Exposure in vivo versus operant graded activity in chronic low back pain patients: results of a randomized controlled trial. Pain. 2008;138:192–207. doi: 10.1016/j.pain.2007.12.009. 2008. [DOI] [PubMed] [Google Scholar]
- 38.de Jong JR, Vangronsveld K, Peters ML, Goossens ME, Onghena P, Bulte I, Vlaeyen JW. Reduction of pain-related fear and disability in post-traumatic neck pain: a replicated single-case experimental study of exposure in vivo. J Pain. 2008;9:1123–34. doi: 10.1016/j.jpain.2008.06.015. 2008. [DOI] [PubMed] [Google Scholar]


