Abstract
Developmental dysplasia of the hip (DDH) or congenital hip dysplasia (CDH) is the most prevalent developmental childhood hip disorder. It includes a wide spectrum of hip abnormalities ranging from dysplasia to subluxation and complete dislocation of the hip joint. The natural history of neglected DDH in adults is highly variable. The mean age of onset of symptoms is 34.5 years for dysplastic DDH, 32.5 years for low dislocation, 31.2 years for high dislocation with a false acetabulum, and 46.4 years for high dislocation without a false acetabulum. Thorough understanding of the bony and soft tissue deformities induced by dysplasia is crucial for the success of total hip arthroplasty. It is important to evaluate the existing acetabular deformity three-dimensionally, and customize the correction in accordance with the quantity and location of ace tabular deficiencies. Acetabular reconstruction in patients with DDH is challenging. Interpretation of published data is difficult and should be done with caution because most series include patients with different types of hip disease. In general, the complication rate associated with THA is higher in patients with hip dysplasia than it is in patients with osteoarthritis. Overall, clinical and functional outcomes following THA in patients hip dysplasia (DDH) differ from those treated for primary hip osteoarthritis, possibly due to the lower age and level of activity. Although function scores decline with age, the scores for pain and range of motion presented with a statistically significant improvement in the long-term.
Key words: Acetabulum, Arthroplasty, Congenital, Developmental, Hip
Introduction
Developmental dysplasia of the hip (DDH) is the most common childhood hip disorder. DDH is characterized by a wide range of clinical and radiographic entities that range from a mild form of hip dysplasia to a high dislocation of the femoral head.
Hip instability during infancy usually resolves within the first few weeks after birth without treatment. The reported incidence of DDH is 1-2 per 1000 newborns; the rate of true hip instability ranges from 15 to 20 per 1000 cases.The development of secondary osteoarthritis (OA) to DDH is well established. Twenty-six percent of hip replacements performed in patients over 40years of age had secondary OAovera period of 20 years, which was attributed to hip dysplasia (1).
The natural course of an untreated DDH is non-predictable. Hartofilakidis et altried to correlate the onset of symptoms to the type and severity of DDH; the authors found that the mean age of pain onset was 34.5 for dysplastic DDH, 32.5 years when related to low dislocation of the hip, 46.4 years when related to high dislocation without a false acetabulum and 31.2 years when related to high hip dislocation with the presence of a false acetabulum (2).
Initial attempts for surgical repair have not been successful. In 1948 Smith Petersen presented 12 cases of DDH that were managed operatively with interpositionarthroplasty. The method was implemented by several authors (Sticnchfield and Carroll and later by Merle D’Aubigne) showing improved results (3). D’Aubignesincluded a series of 28 strictly selected cases that suffered from DDH with hip dislocation and severe functional deficit (inability to walk one hour without severe pain). It was shown that reposition of the hip to its anatomical position during a hiparthroplasty in young patients was possible. The study suffered only from possible false positive election of candidates due to young girls that were eager to rid of the trendelerburg gait thus sometimes perhaps overstating their disability and functional deficit (3).
Morphology of the acetabulum in patients with DDH
The acetabulum in DDH, as studied with CT images, is characterized by anatomic abnormalities. Theseconsist of shallow articular cavity, increased anteversion, insufficient acetabular coverage of the femoral head and a deficient anterior wall (2,4).
The abnormal joint anatomy is related to a redistribution of stresses onto the femoral head surface and articular cartilage of the acetabulum. Early secondary osteoarthritis (OA) of adults has been associated with residual hip dysplasia at childhood (4). The accuracy of the Severin classification in predicting the severity of degenerative hip arthritis is high; 46% of Severin III/IV hip are associated with severe degenerative changes, compared with only 3% of hips categorized as Severin I/II (5).
Hartofilakis et al. described the variant deformities of the acetabulum in patients with DDH: dysplasia consists of a shallow acetabulum with a superior segmental defect; the femoral head is covered by the hypoplastic acetabulum (1, 2). Low hip dislocation,is characterized by the presence of a false acetabulum that partially covers the true acetabulum; the femoral head is usually contained in thefalse acetabulum. Anterior segmental defect or a posterior wall deficiency, and increased anteversionare usually present (3). In high hip dislocation, the femoral head is migratedpostero-superiorlyin relation to the true acetabulum, which is narrow, shallow, and triangular in shape; the iliac wing is alsoanteverted and the entire rim of the acetabulum may be found defective (6).
The biomechanics of the hip joint are also severely changed:hip flexors, adductors and extensors are shortened due to persistent dislocation of the hip joint, and the center of hip rotation is migrated laterally and superiorly and abundant soft tissue, consisting of the joint capsule and the elongated ligamentumteres, covers the true acetabulum. Patients are usually limping and have a characteristic Trendelemburg gait due to the loss of the fulcrum effect of the abductors muscles (7,8).
Thus in any attempt to surgically correct a patients’ hip with DDH deformity, one must take into account both skeletal and soft tissue deformities. Three-dimensional assessment of the bony anatomy is of paramount importance before proceeding to any kind of surgical intervention (2). The importance of CT imaging in the preoperative planning and templating is evident due to its increased accuracy in comparison to plain x-ray especially in measuring the supero-inferior dimension of the acetabulum.
Classification systems
Several classification have been presented in the current literature. Crowe et al., described a simple method aimed in quantifying the amount of dislocation of the hip (9). Three landmarks identified in an AP x-ray. The radiographic teardrops when joined at their inferior margins consist a reference line. The distance from the medial head-neck junction to this reference line is measured. The amount of dislocation is the ratio between this distance and the vertical height of the pelvis.In this classification four types of femoral head dislocations are described: type 1, 50% dislocation; Type 2, 50-75% dislocation; Type 3, 75-100% dislocation. In types 2 and above the head/neck junction is situated above the reference line by at least 10% in relation to the height of the pelvis.Weaknesses of this classification are related to its inherent inability to explain the underlying pathology, inability to accurately locate the head-neck junction on the pelvic x-ray (1,2).
The Hartofilakidis classification focuses on the acetabular anatomical variations related to DDH. Three main types are mentioned: hip dysplasia, low dislocation, and high dislocation (1). In hip dysplasia the hip is subluxed but still contained in the true acetabulum (2). In low dislocation the femoral head is partially covered by the true acetabulum and articulates with a false acetabulum (3). In high dislocation the femoral head is truly dislocated in a superoposterior position (6). Later modifications of this classification included two subtypes for both low and high dislocations. In low dislocation subtype B1 is related to extended coverage of the true acetabulum by the false acetabulum whereas in type B2 there is little coverage.In high dislocation subtype C1 relates to an iliac wing positioned acetabulum and in subtype C2 the femoral head lies in the abductor muscles.Hartofilakidis et al, demonstrated that type C2 dysplastic hips are associated with higher revision rates compared to type C1 hips (P=0.001) (10).
Eftekharpresented another classification system for hip dysplasia based on the grade of dislocation of the femoral head. According to this system, the severity of dysplasia is classified into four stages, ranging from dysplasia to complete dislocation.In type A, the acetabulum is slightly elongated in its superoinferior dimension and the femoral head has a characteristic mushroom shape and is flattened. Types B and C are described intermediate and high dislocations, respectively. The true acetabulum is poorly developed. The lower border of the false acetabulum covers the roof of the original acetabulum. Following removal of fibrofatty tissue from the anatomic area of the true acetabulum we can identify thefloor of the true acetabulum, which is usually thick. In type D dysplastic hips, the femoral head is totally dislocated. The original acetabulum can be hardly recognized representing a narrow “isthmus” over the fusedtriradiate cartilage (11,12).
All of the above-mentioned classifications (Crowe, Hartofilakidis, Eftekhar), have been characterized as reproducible and repeatable and useful in evaluating and treating DDH (11,13-17).
Preoperative Planning & Radiographic Parameters
X-ray evaluation typically includes an anteroposterior (AP) view of the pelvis and AP and lateral views of the affected hip. Computed tomography (CT) imagesare more accurate in evaluating the bony deficiencies of the acetabulum in patients with DDH.
Radiographic parameters such as Wiberg’s lateral center-edge angle (LCE) and Lequesne’s acetabular index (AI) are used for diagnosis and treatment planning, allowing the preoperative evaluation of possible loss of primary stability in dysplastic hips (18,19). The pathological cut-off values for LCE angle and AI are below 20° and above 12° for the LCE and AI, respectively (19).
Placement of the acetabular component in patients with DDH is very challenging because anatomic landmarks are very difficult to identify and bony anatomy severely compromised. Stans et al. showed that 25,7% of acetabular implants are placed outside the true acetabulum in a series a series of Crowe type III dysplastic hips, compared to a 12% in Crowe type II hips (20).
In an effort to overcome the difficulty in recognizing the true acetabulum, Crowe et al, showed that that the center of hip rotation may be accurately identified by placing it atthe center of a triangle that is formed by the anterior inferior iliac spine, ischial tuberosity and the obturator foramen (9). Cup should be ideally placed close to the teardrop in order to better restore the acetabular offset and therefore the biomechanics of the hip joint. The distance from the acetabular fossa to the quadrilateral plate should be also estimated carefully because this is associated with the placement of acetabular screws. Therefore, meticulous preoperative templating, which identifies patients’ individual anatomy and available bone stock is essential for preventing suboptimal placement of the acetabular component and accidental penetration into the medial wall of the acetabulum.
Surgical technique
Hip dysplasia / Crowe types I-II
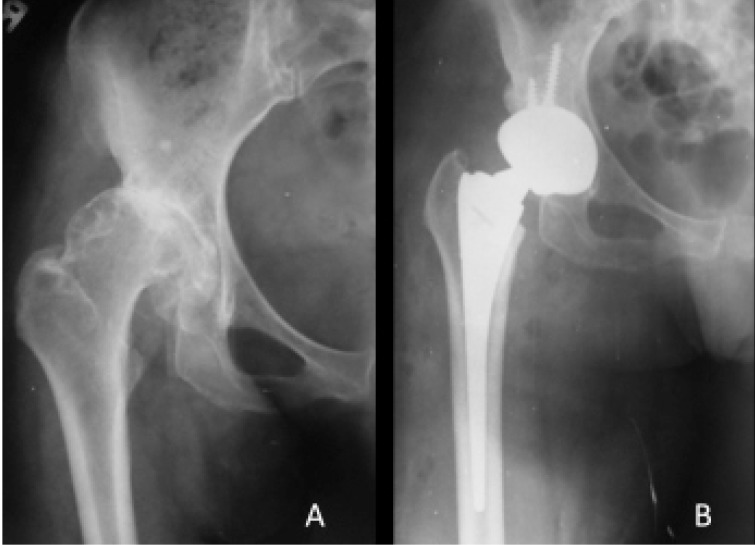
Medialization of the acetabular implant, placed within the true acetabulum usually is possible. Preservation of the bone stock of the anterior wall, which is usually thin, is necessary during reaming. Cementless press fit implants are favored (Figure 1).
Figure 1.
Preoperative (A) and postoperative (B) anteroposterior radiograph of the right hip demonstrating the reconstruction of a Hartofilakidis type A DDH using a hemispherical cementless pressfit modular cup augmented with two transacetabular screws.
Low hip dislocation / Crowe type III
In low hip dislocations / Crowe type III the femoral head is found subluxed and migrated towards a cephalic and lateral direction. The anterior and superior walls are dysplastic creating an oval shape of the acetabulum. Intraoperative recognition of the inferior rim of the acetabulum and identification of the acetabular notch is of paramount importance. These two anatomic landmarks useful to identify the true acetabulum, which is usually covered by the a false acetabulum.
Soft tissue release of the inferior acetabulum is necessary in order to provide adequate exposure. Reaming aims in providing adequate bone coverage. There is not a consensus over the minimum cup exposure (i.e. the amount of acetabular component that is found uncovered from acetabular bone in an anteroposterior radiograph of the pelvis) for a construct to be considered stable. Chanley and Fuegin suggested avoiding THA if the cup exposure exceeds 5mm (21). Garvin et al, suggests that approximately 20% of the superolateral aspect of the cup could be left uncovered by bone, without compromising postoperative implant stability (22). It is suggested that 50-60% coverage of the acetabular implant is sufficient when ultra-porous implants are used. Stability is further enhanced with the use of screws, the benefit of early weight bearing.
Acetabular bone deficiency can be substituted by any of the following methods:
Acetabular reconstruction of the anatomic hip center using bone graft and/or augments
Autogenous impaction grafting
Medialization of the anatomic hip joint- Cotyloplasty
Acetabular reconstruction at a high hip center.
High hip dislocation / Crowe type IV
In this type of DDH there is no need for bone graft augmentation. The acetabulum tends to be shallow and the soft tissue contracted due to chronic dislocation. Therefore extensive capsulotomy, iliopsoas tendon release and placement of a small cementlessacetabular shell (average outside diameter 38-44 mm) in the anatomic center, which can be localized using as reference marks the cross section of the ischium and pubic ramus.
Implant selection
Small, monoblock implants or ceramic on ceramic bearing surfaces are preferred (23-26). Cementess reconstruction of the acetabulum is related to lower rates of revision. Cemented reconstruction has been reported to have revision rates of up to 37% (27,28).
Among several implants designs aiming in solving several technical issues that arise in acetabular fitting, Holzapfel et al, presented an oval- shaped cementless press-fit cup to be used with bulk femoral autografts (29). In comparison to hemispherical cups it was found that the oval cups were less successful in re-establishing the hip center ofrotation, thus being less favored in use by surgeons.
The Artek cup, which was especially designed for use in dysplastic hips, presented as a good alternative reconstructive option. However the metal on metal articulation raises concerns regarding the increased metal ions release and potential development of allergic reactions and early aseptic loosinening and, therefore, it should be used with caution (30).
The 15-face changing cup is designed to position the bearing surface in a less than 45 degrees angle of inclination. This cup was introduced for use in patients withHartofilakidis types A or B deformities (31). Up to now, no available clinical data exist to support the broad use of this component in patients with DDH.
The Muller acetabular roof-reinforcement ring, provides adequate surface for fixation of the cup with cement (32). A variation of this implant including a hook was designed in order to deal with bone stock deficiencies (33).
The Centroid Hilock cup consistsa middle solution combining most of the above-mentioned innovations. It combines the properties of a cup and a ring. Koulouvaris et al presented good clinical outcomes in patients with severe DDH after 5 years of follow-up (34).
Component anteversion
The anatomy of the hip joint in patients with DDH is severely altered concerning theacetabular version, the femoral version and the femoral torsion (35). For these cases it is questionable if acetabular and femoral implants should be orientated in such a way to reconstruct individual anatomy or fit within a safe zone. Choosing a correct combined orientation of both components, the acetabular cup and femoral stem, will yield a maximized, stable range of motion (ROM) and will reduce the risk for dislocation. Widmer et al. have shown that final component orientation must consider cup containment, implant impingement with bone and soft tissue, and preoperative skeletal contractures or deformities to achieve the optimal compromise for each patient (36). The technique of combined cup and stem anteversion in THA based on femoral anteversion has been suggested as a method to compensate for abnormal femoral anteversion. The “Ranawat test” for combined anteversion between the cup and stem is a visual judgment when the femoral neck and head are aligned coplanar to the acetabular cup periphery (37). The degree of internal rotation required to reproduce a coplanar head-cup orientation consists the combined anteversion. There is a wide safe zone of 25° to 50° for combined anteversion for THA. Dorr et al.demonstarted that if anatomic stem anteversion is better to compensated with altering cup anteversion than changing stem anteversionto avoid postoperative rotational deformities of the leg and foot (38).
Use of trans-acetabular screws
The posterosuperior quadrant which was initially considered a safe zone for screw placement, is not considered to be safe in hips with high dislocation (39). Use of the posterosuperior quadrant has been related to frequent injury of the obturator vessels (40). Safe zones are defined using volumetric CT information with 3D mapping of bone and vascular structures.
Postoperative care
Physiotherapy is aimed in restoring pelvic balance and is individualized according to patients’ status and operative procedure performed. Flexion of the ipsilateral knee prevents sciatic nerve tension. Patients that have undergone trochanteric osteotomy should be warned of an apparent leg lengthening that usually lasts for a period of 4-6 months. Routine pain management and anticoagulation protocols are implementeded. Single-dose perioperative antibiotics are usually administered according to local epidemiological data.
Outcomes
DDH surgery is related to increased mortality rates, with a higher than expected 6-month mortality rate as observed in a series presented byBoyle et al. Patients suffering from other pathologies such as primary osteoarthritis or rheumatoid arthritis have worse long term outcomes (41-43). Young age is related to higher percentage of postoperative implant failures (44).
Complications
Factors such as prolonged operative time, extensive soft tissue releases, use of bone grafts, and extensive surgical wound are related to higher rates of infection, compared to THA for OA (42,43). Sciatic nerve palsy is related to limb lengthening, with increased risk of nerve palsy at >4cm of leg lengthening and 2 cm being considered a safe limit (45,46). Operative techniques and choice of surgical approach influence the rate of postoperative dislocations. Southern approach when performed without repair of external rotators or capsule repair on completion is related to increase rates of dislocations. The useof cementless cups is favored; these cups have a documented 10-year implant survival rate of 94%, in patients with femoral allograft augmentation (24,34,47,48). Higher rates of incorporation of bone grafts with morcelized bone particles from autogenous femoral heads in relation to bulk allografts is noted, a phenomenon attributed to better osseointegrationof small bone particles (Figure 2) (49). In cotyloplasty, overzealous medialization leads to increased fixation failures (Figure 3) (50). Changes in the center of rotation are related to altered mechanics of the hip. Bicanic et al. found that for every millimeter of lateral displacement of the cup from its anatomical position the hip load may be increased by 0,7% (51).
Figure 2.
Postoperative AP radiograph of the left hip showing resorption of the structural allograft 5 yrs postoperatively. The cup was not relying on the graft and remained stable.
Figure 3.
Postoperative AP radiograph of the left hip showing a case with excessive medial displacement of the cup.
Conclusions
Developmental dysplasia of the hip (DDH) includes a wide spectrum of hip abnormalities ranging from dysplasia to subluxation and complete dislocation of the hip joint. The natural history of neglected DDH in adults is highly variable. Thorough understanding of the bony and soft tissue deformities induced by dysplasia is crucial for the success of total hip arthroplasty. It is important to evaluate the existing acetabular deformity in three dimensions, and customize the correction in accordance with the quantity and location of acetabular bony deficiencies.
Acetabular reconstruction in patients with DDH is challenging. Excesive acetabular anteversion, defficient anterior wall of the acetabulum, shallow and oblong shape of the acetabulum consist the most common anatomic alterations of the bony anatomy an patients with DDH. Several methods of reconstructions have been proposed depending on the type of dislocation and severity of bony deficiency.
Interpretation of published data is difficult and should be done with caution because most series include patients with different types of hip disease. In general, the complication rate associated with THA is higher in patients with hip dysplasia than it is in patients with osteoarthritis. Overall, clinical and functional outcomes following THA in patients hip dysplasia (DDH) differ from those treated for primary hip osteoarthritis, possibly due to the lower age and higher level of activity.
References
- 1.Engesaeter IO, Lehmann T, Laborie LB, Lie SA, Rosendahl K, Engesaeter LB. Total hip replacement in young adults with hip dysplasia: age at diagnosis, previous treatment, quality of life, and validation of diagnoses reported to the Norwegian Arthroplasty Register between 1987 and 2007. Acta Orthop. 2011;82(2):149–54. doi: 10.3109/17453674.2011.566146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karachalios T, Hartofilakidis G. Congenital hip disease in adults: terminology, classification, pre-operative planning and management. J Bone Joint Surg Br. 2010;92(7):914–21. doi: 10.1302/0301-620X.92B7.24114. [DOI] [PubMed] [Google Scholar]
- 3.Merle D’Aubigne RM. Reposition with arthroplasty for congenital dislocation of the hip in adults. J Bone Joint Surg Br. 1952;34(1):22–9. doi: 10.1302/0301-620X.34B1.22. [DOI] [PubMed] [Google Scholar]
- 4.Argenson JN, Flecher X, Parratte S, Aubaniac JM. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007;465:40–5. doi: 10.1097/BLO.0b013e3181576052. [DOI] [PubMed] [Google Scholar]
- 5.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br. 2004;86(6):876–86. doi: 10.1302/0301-620x.86b6.14441. [DOI] [PubMed] [Google Scholar]
- 6.Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1996;78(5):683–92. doi: 10.2106/00004623-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Lai KA, Lin CJ, Jou IM, Su FC. Gait analysis after total hip arthroplasty with leg-length equalization in women with unilateral congenital complete dislocation of the hip--comparison with untreated patients. J Orthop Res. 2001;19(6):1147–52. doi: 10.1016/S0736-0266(01)00032-8. [DOI] [PubMed] [Google Scholar]
- 8.Radin EL, Paul IL. The biomechanics of congenital dislocated hips and their treatment. Clin Orthop Relat Res. 1974. pp. 32–8. [DOI] [PubMed]
- 9.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23. [PubMed] [Google Scholar]
- 10.Hartofilakidis G, Babis GC, Lampropoulou-Adamidou K, Vlamis J. Results of Total Hip Arthroplasty Differ in Subtypes of High Dislocation. Clin Orthop Relat Res. 2013;471(9):2972–9. doi: 10.1007/s11999-013-2983-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brunner A, Ulmar B, Reichel H, Decking R. The Eftekhar and Kerboul classifications in assessment of developmental dysplasia of the hip in adult patients. Measurement of inter- and intraobserver reliability. HSS J. 2008;4(1):25–31. doi: 10.1007/s11420-007-9066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson MJ, Harris WH. Total hip arthroplasty with insertion of the acetabular component without cement in hips with total congenital dislocation or marked congenital dysplasia. J Bone Joint Surg Am. 1999;81(3):347–54. doi: 10.2106/00004623-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Decking R, Brunner A, Decking J, Puhl W, Gunther KP. Reliability of the Crowe und Hartofilakidis classifications used in the assessment of the adult dysplastic hip. Skeletal Radiol. 2006;35(5):282–7. doi: 10.1007/s00256-005-0061-5. [DOI] [PubMed] [Google Scholar]
- 14.Kose O, Celiktas M, Guler F, Baz AB, Togrul E, Akalin S. Inter- and intraobserver reliability of the Crowe and Hartofilakidis classifications in the assessment of developmental dysplasia of the hip in adult patients. Arch Orthop Trauma Surg. 2012;132(11):1625–30. doi: 10.1007/s00402-012-1600-x. [DOI] [PubMed] [Google Scholar]
- 15.Gaston MS, Gaston P, Donaldson P, Howie CR. A new classification system for the adult dysplastic hip requiring total hip arthroplasty: a reliability study. Hip Int. 2009;19(2):96–101. doi: 10.1177/112070000901900203. [DOI] [PubMed] [Google Scholar]
- 16.Yiannakopoulos CK, Chougle A, Eskelinen A, Hodgkinson JP, Hartofilakidis G. Inter- and intra-observer variability of the Crowe and Hartofilakidis classification systems for congenital hip disease in adults. J Bone Joint Surg Br. 2008;90(5):579–83. doi: 10.1302/0301-620X.90B5.19724. [DOI] [PubMed] [Google Scholar]
- 17.Yiannakopoulos CK, Xenakis T, Karachalios T, Babis GC, Hartofilakidis G. Reliability and validity of the Hartofilakidis classification system of congenital hip disease in adults. Int Orthop. 2009;33(2):353–8. doi: 10.1007/s00264-007-0472-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Werner CM, Copeland CE, Ruckstuhl T, Stromberg J, Turen CH, Bouaicha S. Relationship between Wiberg’s lateral center edge angle, Lequesne’s acetabular index, and medial acetabular bone stock. Skeletal Radiol. 2011;40(11):1435–9. doi: 10.1007/s00256-011-1141-3. [DOI] [PubMed] [Google Scholar]
- 19.Werner CM, Ramseier LE, Ruckstuhl T, Stromberg J, Copeland CE, Turen CH, et al. Normal values of Wiberg’s lateral center-edge angle and Lequesne’s acetabular index--a coxometric update. Skeletal Radiol. 2012;41(10):1273–8. doi: 10.1007/s00256-012-1420-7. [DOI] [PubMed] [Google Scholar]
- 20.Stans AA, Pagnano MW, Shaughnessy WJ, Hanssen AD. Results of total hip arthroplasty for Crowe Type III developmental hip dysplasia. Clin Orthop Relat Res. 1998;348:149–57. [PubMed] [Google Scholar]
- 21.Charnley J, Feagin JA. Low-friction arthroplasty in congenital subluxation of the hip. Clin Orthop Relat Res. 1973. pp. 98–113. [DOI] [PubMed]
- 22.Garvin KL, Bowen MK, Salvati EA, Ranawat CS. Long-term results of total hip arthroplasty in congenital dislocation and dysplasia of the hip. A follow-up note. J Bone Joint Surg Am. 1991;73(9):1348–54. [PubMed] [Google Scholar]
- 23.Macheras GA, Kateros K, Koutsostathis SD, Tsakotos G, Galanakos S, Papadakis SA. The Trabecular Metal Monoblock acetabular component in patients with high congenital hip dislocation: a prospective study. J Bone Joint Surg Br. 2010;92(5):624–8. doi: 10.1302/0301-620X.92B5.23256. [DOI] [PubMed] [Google Scholar]
- 24.Takigami I, Ito Y, Matsumoto K, Ogawa H, Terabayashi N, Shimizu K. Primary total hip arthroplasty with a spongy metal surface acetabular component for hip dysplasia. J Arthroplasty. 2013;28(1):172–7. doi: 10.1016/j.arth.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Kim YH, Park JW, Kim JS. Cementless metaphyseal fitting anatomic total hip arthroplasty with a ceramic-on-ceramic bearing in patients thirty years of age or younger. J Bone Joint Surg Am. 2012;94(17):1570–5. doi: 10.2106/JBJS.K.00697. [DOI] [PubMed] [Google Scholar]
- 26.Pignatti G, Stagni C, Fravisini M, Giunti A. Ceramic-ceramic coupling. Total hip arthroplasty in young patients. Chir Organi Mov. 2003;88(4):369–75. [PubMed] [Google Scholar]
- 27.Numair J, Joshi AB, Murphy JC, Porter ML, Hardinge K. Total hip arthroplasty for congenital dysplasia or dislocation of the hip. Survivorship analysis and long-term results. J Bone Joint Surg Am. 1997;79(9):1352–60. doi: 10.2106/00004623-199709000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Sochart DH, Porter ML. Long-term results of cemented Charnley low-friction arthroplasty in patients aged less than 30 years. J Arthroplasty. 1998;13(2):123–31. doi: 10.1016/s0883-5403(98)90089-4. [DOI] [PubMed] [Google Scholar]
- 29.Holzapfel BM, Greimel F, Prodinger PM, Pilge H, Noth U, Gollwitzer H, et al. Total hip replacement in developmental dysplasia using an oval-shaped cementless press-fit cup. Int Orthop. 2012;36(7):1355–61. doi: 10.1007/s00264-012-1510-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schollner C, Decking J, Eckardt A. The Artek cup for total hip replacement of dysplastic hip joints. Arch Orthop Trauma Surg. 2003;123(6):299–304. doi: 10.1007/s00402-003-0523-y. [DOI] [PubMed] [Google Scholar]
- 31.Zahos K, Mehendale S, Ward AJ, Smith EJ, Nichols M. The 15 degrees face-changing acetabular component for treatment of osteoarthritis secondary to developmental dysplasia of the hip. J Bone Joint Surg Br. 2012;94(2):163–6. doi: 10.1302/0301-620X.94B2.27348. [DOI] [PubMed] [Google Scholar]
- 32.Gill TJ, Sledge JB, Muller ME. Total hip arthroplasty with use of an acetabular reinforcement ring in patients who have congenital dysplasia of the hip. Results at five to fifteen years. J Bone Joint Surg Am. 1998;80(7):969–79. doi: 10.2106/00004623-199807000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Siebenrock KA, Tannast M, Kim S, Morgenstern W, Ganz R. Acetabular reconstruction using a roof reinforcement ring with hook for total hip arthroplasty in developmental dysplasia of the hip-osteoarthritis minimum 10-year follow-up results. J Arthroplasty. 2005;20(4):492–8. doi: 10.1016/j.arth.2004.09.045. [DOI] [PubMed] [Google Scholar]
- 34.Koulouvaris P, Stafylas K, Xenakis T. Cementless modular centroid reconstruction cup in young adults with congenital dysplasia of the hip. J Arthroplasty. 2008;23(1):79–85. doi: 10.1016/j.arth.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Merle C, Grammatopoulos G, Waldstein W, Pegg E, Pandit H, Aldinger PR, et al. Comparison of native anatomy with recommended safe component orientation in total hip arthroplasty for primary osteoarthritis. J Bone Joint Surg Am. 2013;95(22):172. doi: 10.2106/JBJS.L.01014. [DOI] [PubMed] [Google Scholar]
- 36.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22(4):815–21. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 37.Dorr LD, Jones RE, Padgett DE, Pagnano M, Ranawat AS, Trousdale RT. Robotic guidance in total hip arthroplasty: the shape of things to come. Orthopedics. 2011;34(9):652–5. doi: 10.3928/01477447-20110714-30. [DOI] [PubMed] [Google Scholar]
- 38.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467(1):119–27. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wasielewski RC, Galat DD, Sheridan KC, Rubash HE. Acetabular anatomy and transacetabular screw fixation at the high hip center. Clin Orthop Relat Res. 2005;438:171–6. doi: 10.1097/01.blo.0000165855.76244.53. [DOI] [PubMed] [Google Scholar]
- 40.Liu Q, Zhou YX, Xu HJ, Tang J, Guo SJ, Tang QH. Safe zone for transacetabular screw fixation in prosthetic acetabular reconstruction of high developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91(12):2880–5. doi: 10.2106/JBJS.H.01752. [DOI] [PubMed] [Google Scholar]
- 41.Boyle MJ, Frampton CM, Crawford HA. Early results of total hip arthroplasty in patients with developmental dysplasia of the hip compared with patients with osteoarthritis. J Arthroplasty. 2012;27(3):386–90. doi: 10.1016/j.arth.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 42.Prokopetz JJ, Losina E, Bliss RL, Wright J, Baron JA, Katz JN. Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC Musculoskelet Disord. 2012;13:251. doi: 10.1186/1471-2474-13-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wright EA1, Katz JN, Baron JA, Wright RJ, Malchau H, Mahomed N, et al. Risk factors for revision of primary total hip replacement: results from a national case-control study. Arthritis Care Res (Hoboken) 2012;64(12):1879–85. doi: 10.1002/acr.21760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dudkiewicz I, Salai M, Ganel A, Blankstein A, Chechik A. Total hip arthroplasty in patients younger than 30 years of age following developmental dysplasia of hip (DDH) in infancy. Arch Orthop Trauma Surg. 2002;122(3):139–42. doi: 10.1007/s004020100307. [DOI] [PubMed] [Google Scholar]
- 45.Eggli S, Hankemayer S, Muller ME. Nerve palsy after leg lengthening in total replacement arthroplasty for developmental dysplasia of the hip. J Bone Joint Surg Br. 1999;81(5):843–5. doi: 10.1302/0301-620x.81b5.9610. [DOI] [PubMed] [Google Scholar]
- 46.Farrell CM, Springer BD, Haidukewych GJ, Morrey BF. Motor nerve palsy following primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87(12):2619–25. doi: 10.2106/JBJS.C.01564. [DOI] [PubMed] [Google Scholar]
- 47.Georgiades G, Babis GC, Kourlaba G, Hartofilakidis G. Effect of cementless acetabular component orientation, position, and containment in total hip arthroplasty for congenital hip disease. J Arthroplasty. 2010;25(7):1143–50. doi: 10.1016/j.arth.2009.12.016. [DOI] [PubMed] [Google Scholar]
- 48.Kim M, Kadowaki T. High long-term survival of bulk femoral head autograft for acetabular reconstruction in cementless THA for developmental hip dysplasia. Clin Orthop Relat Res. 2010;468(6):1611–20. doi: 10.1007/s11999-010-1288-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li H, Wang L, Dai K, Zhu Z. Autogenous impaction grafting in total hip arthroplasty with developmental dysplasia of the hip. J Arthroplasty. 2013;28(4):637–43. doi: 10.1016/j.arth.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 50.Symeonides PP, Pournaras J, Petsatodes G, Christoforides J, Hatzokos I, Pantazis E. Total hip arthroplasty in neglected congenital dislocation of the hip. Clin Orthop Relat Res. 1997;341:55–61. [PubMed] [Google Scholar]
- 51.Bicanic G, Delimar D, Delimar M, Pecina M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop. 2009;33(2):397–402. doi: 10.1007/s00264-008-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]