Abstract
Background:
We aimed to report outcomes of total hip arthroplasty (THA) in very young patients under the year of 30.
Methods:
Thirty patients (45 hips) with various indications for THA were retrospectively reviewed radiologically and clinically and analyzed regarding survival, reasons of failure, factors associated with outcomes and postoperative complications.
Results:
Within a mean follow-up time of 116 months the 10-year survival rate was 90.3%. All hips were revised due to aseptic loosening. No association was found among the tested parameters with increased revision rates. Three complications associated with the THA were recorded and managed conservatively. All patients had statistically significant improved clinical scores compared to the pre-operative period, despite the underlying disorder that compromised the condition in the majority of the patients.
Conclusions:
Our study showed excellent long term outcomes of THA in patients younger than 30 years of age, comparable with those in older patients.
Key words: Aseptic loosening, Congenital hip disease, Juvenile rheumatoid arthritis, Total hip arthroplasty, Young patients
Introduction
Total hip arthroplasty (THA) is the main treatment option for restoring function and mobility for various end-stage degenerative conditions of the hip cartilage. Despite the fact that THA was initially designed to be performed in elderly low-demanding patients, the benefit of the procedure in younger populations has also been well documented (1-3). However, the number of young patients undergoing THA is gradually decreasing due to the early diagnosis and the effective treatment of the underlying disease. The reported outcomes of THA in young patients are poorer compared to older patients, with a 10-year survival rate ranging from 49% to 95% in the published literature (4-6). Higher revision rates are reported in juvenile arthritis series (7,8), while aseptic loosening is the main reason for revision (9). The poor survivorship of the prostheses in the young population has been attributed mainly to the underlying condition (most commonly rheumatoid arthritis and congenital hip disease), that is usually associated with markedly musculoskeletal deficiencies and deformations which influence the stability of the surgical implants thus leading to early loosening. Other factors associated with poor survival of THA in young patients are the higher activity, the use of cemented components in the early years and the common use of screws in acetabular designs (10,11).
The purpose of the present study is to report outcomes of THA in patients under the year of 30 regarding survival rates, reasons of failure, clinical outcomes and factors associated with poor survival. The study represents the 22-year experience of a single institution.
Materials and Methods
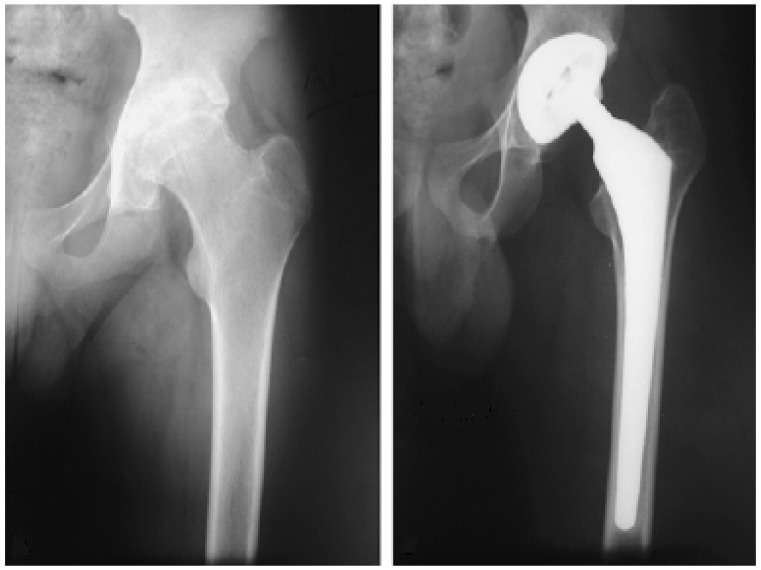
We retrospectively reviewed all patients younger than 30 years of age that had primary THA at the Department of Orthopaedic Surgery of University of Ioannina between January 1988 and December 2010 by the senior author (T.X) and at least 2-year follow-up period. No patients had previous surgeries at the hip. Thirty-eight patients were initially considered eligible to be included in the study. Eight patients were eventually excluded from the study due to no follow up data, leaving 30 patients (45 hips) available for analysis. The main indication for THA was juvenile rheumatoid arthritis (19 hips, 42.2%), followed by osteonecrosis of the femoral head (11 hips, 24.4%) (Figure 1) and congenital hip disease (5 hips, 11.1%) (Table 1). Twenty seven THA were performed in female patients. The mean age at the operation was 23.3 years (range 13-29). Twenty –two THAs were right sided.
Figure 1.
Cementless THA in a male patient with osteonecrosis of the femoral head 12 years postoperatively.
Table 1.
Indication for total hip arthroplasty in patients included in the study
| Indication | Hips (n) |
|---|---|
| Juvenile Rheumatoid Arthritis | 19 |
| Osteonecrosis of femoral head | 11 |
| Congenital hip disease | 5 |
| Post-traumatic osteoarthritis | 4 |
| Angylosing Spondylitis | 1 |
| Septic Arthritis | 1 |
| Systemic Lupus Erythematosus | 1 |
| Osteochondritis | 1 |
| Slipped capital femoral epiphysis | 1 |
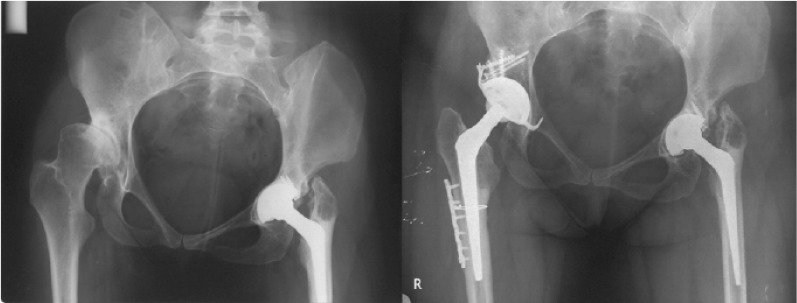
All operations were performed at the Department of Orthopaedic Surgery of the University of Ioannina under general anesthesia. A posterolateral approach was used in all patients. The median duration of the operation was 90 minutes (range 60-210 minutes). In 6 arthroplasties autologous bone graft was used, consisted of acetabular impaction grafting with morselized bone from the femoral head in 4 hips and a bone block with screw fixation in 2 hips. In 22 hips a ceramic on polyethylene design was used, in 19 hips a metal on polyethylene design, 2 hips a ceramic on ceramic and in 2 a metal on metal (Figure 2). Several types of acetabular components were used (Table 2). Fourteen THAs (31%) required screw fixation of the acetabular component. In 24 hips a ceramic femoral head was used, while in 21 hips the head was metallic. The sizes of the femoral heads were 22 in 19 hips (all metallic), 28 in 20 hips (all but 1 ceramic), 32 in 4 hips 46 in 1 hip and 52 in 1 hip. In the vast majority of the patients, cementless femoral components were used (32 hips, 71%). In five hips additional operations were performed. Two hips had shortening osteotomies due to leg-length discrepancy using LC-DCP Synthes plates (1 supracondylar osteotomy with correction of the varous knee deformity and 1 z-type subtrochanteric osteotomy (Figure 3). One hip had a supracondylar osteotomy with an L-plate by Osteo due to varous knee deformity. Finally, two hips had trochanteric osteotomies with wire fixation, due to excessive trochander deformity for the restoration of the hip anatomy and biomechanics.
Figure 2.
23-year old patient with secondary osteonecrosis of the femoral head due to hypophysis tumor and a metal on metal THA.
Table 2.
Types of acetabular implant
| Acetabular implant | Hips (%) |
|---|---|
| Zimmer Hedrocel® | 16 (35.5%) |
| Stryker OmniFit® EON® | 12 (26.7%) |
| Stryker Secur-Fit® | 4 (8.9%) |
| CST | 4 (8.9%) |
| Symbios Centroid Hilock® | 3 (6.7%) |
| Zimmer Durom® | 2 (4.4%) |
| Other | 4 (8.9%) |
Figure 3.
Female patient with congenital hip disease. The patient had a THA with autologous bone graft consisted of a bone block of the femoral head with screw fixation and a z-type subtrochanteric osteotomy.
A standard closed-suction was used that was removed on the second postoperative day. Postoperatively all patients received anticoangulation therapy for 5 weeks with low molecular weight heparins in doses according to the body mass index and a 3-day scheme of antibiotic therapy consisted of second generation cephalosporin that began the night before surgery . All patients followed the same rehabilitation program. They were mobilized at the second postoperative day with use of 2 crunches and partial weight-bearing. Full weight bearing was allowed 2 to 3 months postroperatively, individualized according to the case. No patient underwent intensive physiotherapy.
All patients were assessed clinically and radiologically preoperatively and postoperatively. The clinical assessment was performed using the Merle d’Aubigne score the day before the operation and at 1 year from the operation (12). The Merle d’ Aubigne score evaluates pain, gait and mobility, on a scale of 1 to 6 for each item. Eighteen points indicate an excellent result, fifteen to seventeen indicate a good result and twelve to fourteen a fair result. Scores less than twelve points represent poor results. The radiological assessment of the patients was performed preoperatively and postoperatively immediately after the operation, at 6 weeks, 3 months, 6 months, 1 year and annually thereafter.
Two independent investigators reviewed the clinical records and the serial x-rays and reached consensus on all patients. All complications were recorded (intraoperative, immediate postoperative and late). Patients were evaluated for the development of heterotopic ossification at 6 months from the operation, using the Brooker scoring system (13).
The Kaplan Meier method was used to evaluate the survivorship of the whole group (14). Primary end-point was the revision of any the two components for any reason. Secondary end-points were clinical improvement of the patients as expressed by the Merle-D’Aubigne score and any type of complication during the postoperative period. A t-test for independent samples was performed to evaluate differences between the pre-operative and postoperative scores. A logistic regression analysis was used to evaluate parameters associated with increased risk for revision surgery, such as age, sex, indication for arthroplasty, gender, type of prosthesis (cemented or cementless), type of femoral head (ceramic or metal), use of screws and use of bone graft. P-values <0.5 were considered statistically significant: all P-values were two-tailed. All statistical analyses were performed using the Statistical Package of Social Sciences (SPSS 21.0, Chicago, IL, USA).
Results
Thirty patients (45 hips) were available for the analysis. The mean patient follow up was 116 months (range 24-255 months). One patient had a small non displayed fracture (fissure fracture) of the central part of the lesser trochanter intraoperatively, that was managed with wire fixation. No other intra-operative complications were recorded. No patient developed any immediate postoperative complication during the hospitalization. One patient had traumatic hip dislocation at 1 month after the operation that was managed with close reduction. Two patients developed heterotopic ossification of Brooker 2 and 3 at 6 months from the operation. One patient with osteonecrosis due to combined sickle cell disease and b-thalassemia developed septic arthritis of the ipsilateral knee at 1 year from the operation that was managed with arthroscopic lavage and antibiotic therapy. Finally, 1 patient with juvenile rheumatoid arthritis had an ipsilateral Pilon’s fracture, managed with internal fixation. Two patients with combined sickle cell disease and b-thalassemia died during the follow-up period; a male patient died from disease at 3 years from the operation and a female patient with bilateral THAs died from pulmonary infection at 16 years from the operation. Both patients had no indication of aseptic loosening in the last clinical and radiological evaluation.
Eleven THAs were revised during the follow up period (24.4%, 95% CI 12.9%-39.5%). All hips were revised due to aseptic loosening. Eight patients had aseptic loosening of the acetabular component, 2 hips had polyethylene wear and 1 hip had aseptic loosening of the femoral component. Among the 8 patients with loosening of the acetabular component, in 3 patients this was combined with polyethylene wear. The mean time to revision surgery was 139 months (range 96-255 months). The 10-year survival rate was 90.3% (95% CI 73.5%- 97.9%) (Figure 1).
No parameter was found to be associated with increased risk for revision surgery including age (P=0.13), sex (P=0.80), use of graft (P=0.44), use of cement (P=0.59), use of screws (P=0.39), head size (P=0.85) and head type (P=0.84).
Twenty-eight patients (42 hips) had available preoperative and postoperative clinical evaluation with the Merle d’Aubigne score. In 2 patients the clinical evaluation was impossible due to the multifocal localization of the underlying disease. The mean pre-operative score was 7. 24 (SD 2.61) and the mean post-operative score at 1-year from the operation was 16.67 (SD 1.76). The mean difference was highly statistically significant (P<0.001).
Discussion
The present study represents a 22-year of experience of a single institution regarding THAs performed in very young patients under the year of 30. The hips included in this study showed high survival rates with a 10-year survival of 90%, the highest among similar studies in the published literature. Aseptic loosening was the only reason for revision. Despite the fact that the study included several patients with abnormal hip anatomy (poor bone stock and musculoskeletal deformities), as well as a variety of serious multifocal medical problems from the underlying disease that seriously compromised the restoration of the hip biomechanics and the normal mobilization of the patients, the survival rates were comparable to those reported on older less demanding patients with fewer technical requirements (15-19). Moreover, a few serious complications directly related to the arthroplasty were recorded (3 hips, 6.7%). No association was found among the tested parameters with increased revision rates. All patients had statistically significant improved clinical scores compared to the pre-operative period, although the mean postoperative clinical score was not excellent rendered by the multiple joint involvement due to the underlying disorder.
The indications of THA in very young patients differ from those in older patients and involve several end stage degenerative hip diseases as a result of an underlying systematic condition in the majority of the cases. Juvenile rheumatoid arthritis is the most common disorder for THA in the young population, in the published literature (20-24). However, the introduction of modern disease modifying drugs for the treatment of rheumatoid arthritis during the last years, such as tumor necrosis factor-alpha inhibitors has lead to a significant decrease of very young patients that undergo THAs that reach nearly 50% in reported series (9, 25). Other indications for THA include the osteonecrosis of the femoral head (5,6,9), the congenital hip disease (5,6,9), the posttraumatic osteoarthritis (5,6,9), the slipped capital femoral epiphysis (9,26), inflammatory conditions such as angylosing spondylitis, systemic lupus erythematosus, psoriatic arthritis and Crohn’s disease and others (5,9). A recent systematic review of the literature showed that THAs performed after 1988 were less likely to be performed for juvenile rheumatoid arthritis than earlier procedures (9). Before 1988 juvenile rheumatoid arthritis was the commonest indication for THA in the young population (49.5%), while after 1988 the predominant indication was avascular necrosis (34.8%) (9). The same study also showed a trend towards cementless fixation in the recent years, as well as a significant decrease in revision rates.
A few studies have reported on outcomes of THAs performed in young populations under the year of 30. The reported survival rates in the published literature range from 49% to 95% (4-6, 27). In all studies aseptic loosening was the main reason for revision. Unfortunately, the vast majority of the published studies are small case series that report on short-term outcomes of THAs (3,28,29). A large multicenter study by Girard et al with 896 patients evaluated factors influencing the revision rate of THAs performed in patients younger than 30 years (30). Four factors independently influenced the rate of revision; the use of hard-on-soft bearings (Odds Ratio 3.42), younger ages at the time of primary THA (Odds Ratio 1.14), more than two previous surgeries (Odds Ratio 5.41) and at least one dislocation after the primary THA (Odds ratio 3.98).
The present study is limited by several factors. First of all it is a retrospective evaluation with limited sample size that influence reliable survivorship analyses and preclude evidence-based subgroup analyses for the identification of risk factors for implant survival. However, this was inevitable taking into account the fact that THAs in populations under 30 are not common and have a decreasing trend over the years. Moreover, the heterogeneity of included patients regarding the indication for THA and the type of THA was remarkable as in the majority of the published studies. Both of them could influence the short and long- term outcomes. Our study had one the longest follow up periods among the published literature (approximately 10 year mean follow up), however some patients were not followed in the long-term that is necessary to assess implant longevity in this patient population. Finally, the present study did not perform any radiological analysis that could identify early signs of prosthesis loosening (radiolucent lines and prosthesis migration), due to the lack of radiological data in some patients after the first postoperative year.
THA in the young is a challenging problem. Our study showed excellent long term outcomes of THA in patients younger than 30 years of age. Despite the fact that approximately half of the patients included in our study had juvenile rheumatoid arthritis (known to be associated with decreased survivorship rates), we had 90% 10-year survival in THAs. The establishment of prospective designs with homogenous populations regarding indications and types of arthroplasty should be the future goal. The advances in prosthetic component design render the evaluation of modern uncemented alternative bearing implants such as ceramic on ceramic implants in the long term.
References
- 1.Springer BD, Connelly SE, Odum SM, Fehring TK, Griffin WL, Mason JB, et al. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24(6):2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]
- 2.Torchia ME, Klassen RA, Bianco AJ. Total hip arthroplasty with cement in patients less than twenty years old. Long-term results. J Bone Joint Surg Am. 1996;78(7):995–1003. doi: 10.2106/00004623-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Finkbone PR, Severson EP, Cabanela ME, Trousdale RT. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J Arthroplasty. 2012;27(2):213–9. doi: 10.1016/j.arth.2011.05.022. [DOI] [PubMed] [Google Scholar]
- 4.Wangen H, Lereim P, Holm I, Gunderson R, Reikeras O. Hip arthroplasty in patients younger than 30 years: excellent ten to 16-year follow-up results with a HA-coated stem. Int Orthop. 2008;32(2):203–8. doi: 10.1007/s00264-006-0309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Busch V, Klarenbeek R, Slooff T, Schreurs BW, Gardeniers J. Cemented hip designs are a reasonable option in young patients. Clin Orthop Relat Res. 2010;468(12):3214–20. doi: 10.1007/s11999-010-1355-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Engesæter LB, Engesæter IØ, Fenstad AM, Havelin LI, Kärrholm J, Garellick G, et al. Low revision rate after total hip arthroplasty in patients with pediatric hip diseases. Acta Orthop. 2012;83(5):436–41. doi: 10.3109/17453674.2012.736171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chmell MJ, Scott RD, Thomas WH, Sledge CB. Total hip arthroplasty with cement for juvenile rheumatoid arthritis. Results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg Am. 1997;79(1):44–52. doi: 10.2106/00004623-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Haber D, Goodman SB. Total hip arthroplasty in juvenile chronic arthritis: a consecutive series. J Arthroplasty. 1998;13(3):259–65. doi: 10.1016/s0883-5403(98)90170-x. [DOI] [PubMed] [Google Scholar]
- 9.Adelani MA, Keeney JA, Palisch A, Fowler SA, Clohisy JC. Has total hip arthroplasty in patients 30 years or younger improved? A systematic review. Clin Orthop Relat Res. 2013;471(8):2595–601. doi: 10.1007/s11999-013-2975-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clohisy JC, Oryhon JM, Seyler TM, Wells CW, Liu SS, Callaghan JJ, et al. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clin Orthop Relat Res. 2010;468(12):3207–13. doi: 10.1007/s11999-010-1468-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Learmonth ID, Heywood AW, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1989;71(2):209–12. doi: 10.1302/0301-620X.71B2.2925736. [DOI] [PubMed] [Google Scholar]
- 12.D’ Aubigne RM, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36(3):451–75. [PubMed] [Google Scholar]
- 13.Brooker AF, Bowerman JW, Robinson RA, Riley LH., Jr Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55(8):1629–32. [PubMed] [Google Scholar]
- 14.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53(282):457–81. [Google Scholar]
- 15.Hwang KT, Kim YH, Kim YS, Choi IY. Total hip arthroplasty using cementless grit-blasted femoral component: a minimum 10-year follow-up study. J Arthroplasty. 2012;27(8):1554–61. doi: 10.1016/j.arth.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Lazarinis S, Kärrholm J, Hailer NP. Effects of hydroxyapatite coating on survival of an uncemented femoral stem. A Swedish Hip Arthroplasty Register study on 4,772 hips. Acta Orthop. 2011;82(4):399–404. doi: 10.3109/17453674.2011.597699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JM, Nam HT. Acetabular revision total hip arthroplasty using an impacted morselized allograft and a cementless cup: minimum 10-year follow-up. J Arthroplasty. 2011;26(7):1057–60. doi: 10.1016/j.arth.2011.03.035. [DOI] [PubMed] [Google Scholar]
- 18.Ali MS, Kumar A. Hydroxyapatite-coated RM cup in primary hip arthroplasty. Int Orthop. 2003;27(2):90–3. doi: 10.1007/s00264-002-0410-0. [DOI] [PubMed] [Google Scholar]
- 19.Müller LA, Wenger N, Schramm M, Hohmann D, Forst R, Carl HD. Seventeen-year survival of the cementless CLS Spotorno stem. Arch Orthop Trauma Surg. 2010;130(2):269–75. doi: 10.1007/s00402-009-0969-7. [DOI] [PubMed] [Google Scholar]
- 20.Scott RD, Sarokhan AJ, Dalziel R. Total hip and total knee arthroplasty in juvenile rheumatoid arthritis. Clin Orthop Relat Res. 1984;182:90–8. [PubMed] [Google Scholar]
- 21.Bilsel N, Gökçe A, Kesmezacar H, Mumcuoğlu E, Ozdoğan H. Long-term results of total hip arthroplasty in patients with juvenile rheumatoid arthritis. Acta Orthop Traumatol Turc. 2008;42(2):119–24. doi: 10.3944/aott.2008.42.2.119. [DOI] [PubMed] [Google Scholar]
- 22.Cruz-Pardos A, García-Rey E, García-Cimbrelo E, Ortega-Chamarro J. Alumina-on-alumina THA in patients with juvenile idiopathic arthritis: a 5-year follow up study. Clin Orthop Relat Res. 2012;470(5):1421–30. doi: 10.1007/s11999-011-2046-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.De Ranieri A, Wagner N, Imrie SN, Hwang KL, Goodman SB. Outcome of primary total hip arthroplasty in Charnley Class C patients with juvenile idiopathic arthritis: a case series. J Arthroplasty. 2011;26(8):1182–8. doi: 10.1016/j.arth.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 24.Kitsoulis PB, Siamopoulou A, Beris AE, Xenakis TA. Total hip and knee arthroplasty for juvenile rheumatoid arthritis. Folia Med (Plovdiv) 2006;48(3-4):42–9. [PubMed] [Google Scholar]
- 25.Hekmat K, Jacobsson L, Nilsson JÅ, Petersson IF, Robertsson O, Garellick G, et al. Decrease in the incidence of total hip arthroplasties in patients with rheumatoid arthritis--results from a well defined population in south Sweden. Arthritis Res Ther. 2011;13(2):67. doi: 10.1186/ar3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schoof B, Citak M, O’Loughlin PF, Kendoff D, Haasper C, Gehrke T, et al. Eleven year results of total hip arthroplasty in patients with secondary osteoarthritis due to slipped capital femoral epiphysis. Open Orthop J. 2013;7:158–62. doi: 10.2174/1874325001307010158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odent T, Journeau P, Prieur AM, Touzet P, Pouliquen JC, Glorion C. Cementless hip arthroplasty in juvenile idiopathic arthritis. J Pediatr Orthop. 2005;25(4):465–70. doi: 10.1097/01.bpo.0000161096.53963.0e. [DOI] [PubMed] [Google Scholar]
- 28.Hyder N, Nevelos AB, Barabas TG. Cementless ceramic hip arthroplasties in patients less than 30 years old. J Arthroplasty. 1996;11(6):679–86. doi: 10.1016/s0883-5403(96)80006-4. [DOI] [PubMed] [Google Scholar]
- 29.Kamath AF, Sheth NP, Hosalkar HH, Babatunde OM, Lee GC, Nelson CL. Modern total hip arthroplasty in patients younger than 21 years. J Arthroplasty. 2012;27(3):402–8. doi: 10.1016/j.arth.2011.04.042. [DOI] [PubMed] [Google Scholar]
- 30.Girard J, Glorion C, Bonnomet F, Fron D, Migaud H. Risk factors for revision of hip arthroplasties in patients younger than 30 years. Clin Orthop Relat Res. 2011;469(4):1141–7. doi: 10.1007/s11999-010-1669-x. [DOI] [PMC free article] [PubMed] [Google Scholar]