Abstract
Background:
Conventional treatments after complicated injuries of the distal radioulnar joint (DRUJ) such as Darrach and Kapandji-Sauvé procedures have many drawbacks, which may eventually lead to a painful unstable distal ulna. The development of DRUJ prosthesis has significantly evolved over the past years. In this study, we assessed the outcome results of patients after DRUJ implant arthroplasty using the Aptis (Scheker) prosthesis.
Methods:
We identified 13 patients with 14 prosthesis during the past 10 years. Patients underwent DRUJ arthroplasty due to persistent symptoms of instability, chronic pain, and stiffness. Records and follow-up visits were reviewed to find the final post-operative symptoms, pain, range of motion, and grip strength with a mean follow-up of 12 months (range: 2-25 months). Also, patients were contacted prospectively by phone in order to administer the disabilities of the arm shoulder and hand (DASH), patient rated wrist evaluation (PRWE), and visual analogue scale (VAS), and to interview regarding satisfaction and progress in daily activities. Eleven patients out of 13 could be reached with a median follow-up time of 60 months (range: 2 to 102 months).
Results:
No patient required removal of the prosthesis. Only two patients underwent secondary surgeries in which both required debridement of the screw tip over the radius. The median DASH score, PRWE score, VAS, and satisfaction were 1.3, 2.5, 0, and 10, respectively. The mean range of flexion, extension, supination, and pronation was 62, 54, 51, and 64, respectively.
Conclusions:
Distal radioulnar joint injuries are disabling and patients usually undergo one or more salvage surgeries prior to receiving an arthroplasty. The Scheker prosthesis has shown satisfactory results with 100% survival rate in all reports. The constrained design of this prosthesis gives enough stability to prevent painful subluxation.
Key words: Aptis, Arthroplasty, Distal radioulnar joint, Scheker
Introduction
Normal distal radioulnar joint (DRUJ) anatomy is mandatory to have full motion, strength, and stability. The inherent stability of the DRUJ is ligamentous, which is prone to injuries (1,2). Conventional treatments after complicated injuries of the distal radioulnar joint have many drawbacks. Darrach and Kapandji-Sauvé procedures are the most commonly performed salvage procedures after DRUJ injuries, which may eventually lead to a painful unstable distal ulna (1, 3, 4).
To enhance stability and create a painless functional joint, mechanical stability using a prosthesis has been proposed. Kapandji was the first to report his outcomes using a DRUJ prosthesis, one after failed Kapandji-Sauvé and one after a Darrach procedure (5). The development of DRUJ prosthesis has significantly evolved over the past years with many reports on both success and failure of different prosthesis designs (6, 7). Scheker introduced a semi constrained ball-and-socket prosthesis designed by himself and reported promising results in his patients (7). Since then, other reports of DRUJ prosthesis after failed salvage procedures have shown good results in terms of motion, stability, grip strength and lifting capability (8-11).
In the current study, we assessed the outcome results of patients after DRUJ implant arthroplasty by the senior author of this article using the Aptis prosthesis.
Materials and Methods
In this institutional review board approved study, we used the database of one large academic medical center from December 2005 to June 2014 to retrospectively identify patients after distal radioulnar joint (DRUJ) implant arthroplasty with Aptis prosthesis (Aptis Medical, Louisville, KY) by the senior author. In total, we identified 13 patients with 14 prosthesis. A woman with Ehlers Danlos syndrome underwent non-simultaneous bilateral DRUJ implant arthroplasty within a three-year interval. All patients experienced at least one previous surgery around the wrist relevant to the existing problem ranging from 1 to 6 previous surgeries. Patients underwent DRUJ arthroplasty due to persistent symptoms of instability, chronic pain, and stiffness.
Incisions were carried out using curved dorsal incision over the wrist, DRUJ and ulna. In patients with previous dorso-ulnar incision, the DRUJ was approached through extending the existing scar and the previous plate, if any, was removed. The retinaculum over the DRUJ was preserved and the ulnar head was resected. Following this, the soft tissue was elevated off of the interosseous membrane keeping the neurovascular structures intact and the membrane was dissected off of the radius. The true components were inserted after having trialed the prosthesis under fluoroscopy. The exact length of ulnar excision was determined based on the fitting of the trial. All surgeries were performed under regional block (Figure 1).
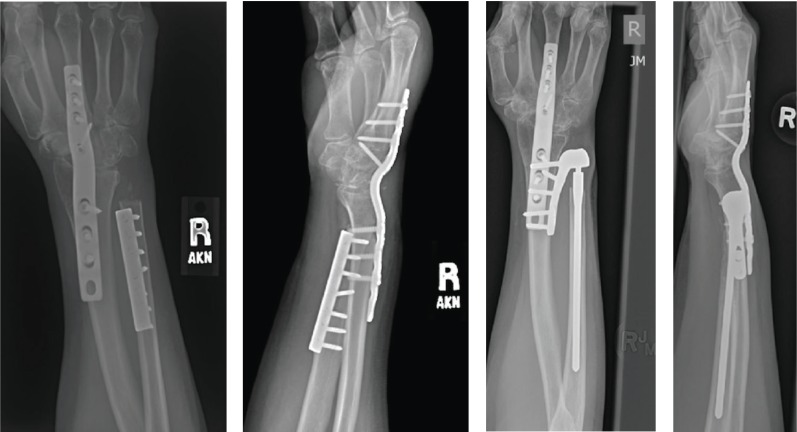
Figure 1.
a & b Pre- and c & d post-operative radiographs of a 44-year old woman with Ehlers-Danlos syndrome underwent distal radio-ulnar joint arthroplasty with Aptis prosthesis due to chronic instability after multiple previous surgeries.
The arm was kept in splint for the first two weeks post-operatively and physical therapy was started thereafter, focusing on return of strength and mobility. In terms of forearm rotation, improvement in pronation was remarkable during the first 2 month, in comparison to supination which took twice as long to regain. All of the wounds healed well without any patients experiencing infection. Only one patient presented 4 days post-operatively with concern for a tight splint and an area of redness about the elbow, which controlled with oral and IV antibiotics.
Records and follow-up visits were reviewed to find the final post-operative symptoms, pain, range of motion, and grip strength with a mean follow-up of 12 months (range: 2-25 months). Also, patients were contacted prospectively by phone in order to administer the disabilities of the arm shoulder and hand (DASH), patient rated wrist evaluation (PRWE), and visual analogue scale (VAS), and to interview regarding satisfaction and progress in daily activities. Eleven patients out of 13 could be reached with a median follow-up time of 60 months (range: 2 to 102 months).
Results
Thirteen patients with 14 wrists were identified with a mean age and standard deviation of 44 (5.8) (Table 1). After mean follow-up of 60 months, no patient required removal of the prosthesis. Only two patients underwent secondary surgeries in which both required debridement of the screw tip over the radius. Nine out of 14 wrists rated their pain 0 and the highest rated was 6 out of 10. The highest pain scores were correlated with the most recent surgeries in the past one year. Ten out of 14 wrists rated 10 to their satisfaction level with the lowest score being 7 on a scale of 1-10. All of the patients reported that they would recommend this surgery to other patients, and if the same injury happens, they would get the same prosthesis in their other wrist. Also the entire patient group responded ‘yes’ to whether they feel better than before getting this prosthesis. The DASH and PRWE scores were low showing no or little disability and functional disturbance after DRUJ implant arthroplasty (Table 2). Based on physical examination at the last follow-up appointment, wrist motion was regained up to the functional level in almost all patients (Table 3). All patients were satisfied with their wrist motion and ability to perform activities of daily living.
Table 1.
Demographics and operative characteristics of 13 patients (14 wrists) after distal radio-ulnar joint implant arthroplasty
| Age, mean (SD) | 44 (5.8) |
| Sex, no (%) | |
| Female | 10 (71) |
| Male | 4 (29) |
| Side, no (%) | |
| Left | 5 (36) |
| Right | 9 (64) |
| Pre-op Diagnosis, no (%) | |
| Chronic instability | 8 (58) |
| Post-traumatic Arthrosis | 2 (14) |
| Stiff DRUJ | 1 (7) |
| DRUJ deformity | 1 (7) |
| Ehlers Danlos Syndrome | 2 (14) |
| Number of previous failed surgeries, mean (SD) | 2.8 (1.8) |
| Previous Surgeries, no (%) | |
| Wrist arthroscopy | 9 (64) |
| Darach or hemiresection | 7 (50) |
| Distal ulnar tenodesis after failed Darach | 3 (21) |
| Proximal row carpectomy | 2 (14) |
| Wrist arthrodesis | 3 (21) |
| DRUJ release | 2 (14) |
| TFCC repair | 2 (14) |
| Other (infection, osteotomy, neurolysis) | 5 (36) |
| Anesthesia, no (%) | |
| Block | 14 (100) |
| Implant type, no (%) | |
| APTIS | 14 (100) |
| Operation duration (min.), mean (SD) | 73 (16) |
| Secondary unplanned surgery | |
| Debridement of Prominent screw tip on radial styloid | 2 (14) |
DRUJ=Distal radio-ulnar joint, TFCC=Triangular fibrocartilage complex, SD=Standard deviation
Table 2.
Patients’ follow-up after distal radio-ulnar joint implant arthroplasty
| Median | Range (Min-Max) | |
|---|---|---|
| Follow up, month | 60 | 2-102 |
| VAS 0-10 | 0 | 0-6 |
| Satisfaction 0-10 | 10 | 7-10 |
| DASH score 0-100 | 1.3 | 0-72 |
| PRWE score 0-100 | 2.5 | 0-61 |
| Pain score 0-50 | 2.0 | 0-30 |
| Function score 0-50 | 0.0 | 0-31 |
| Lifting capacity, 0-20 lbs. | ||
| Involved | 20 | 5-20 |
| Uninvolved | 20 | 10-20 |
DASH=Disabilities of the arm shoulder and hand, PRWE=Patient rated wrist evaluation, VAS=Visual analogue scale
Table 3.
In clinic folloaw-up examination results after distal radio-ulnar joint implant arthroplasty
| Mean (SD) | Range (Min-Max) | |
|---|---|---|
| Follow-up time to examination, month | 12 (10) | 2-25 |
| Flexion | 62 (16) | 50-90 |
| Extension | 54 (8.9) | 40-60 |
| Supination | 51 (30) | 5-80 |
| Pronation | 64 (26) | 20-90 |
| Radial deviation | 13 (6.5) | 5-20 |
| Ulnar deviation | 28 (13) | 10-40 |
| Grip strength | ||
| Involved | 47 (15) | 32-70 |
| Non-involved | 68 (23) | 40-90 |
Discussion
In this study, we assessed the experience of the senior author in managing painful instability of the distal ulna using the Aptis prosthesis. We aimed to assess the objective parameters of range of motion and grip strength, as well as subjective findings by administering the DASH and PRWE questionnaires.
One limitation of our study was inviting patients to come to the clinic for examination. Thus, we retrieved the examination data from the final visit notes retrospectively. However, we were able to reach over two thirds of the patients to complete the disability questionnaires with a 5 year mean follow-up.
We found no patients requiring prosthesis removal after mean follow-up of 5 years, showing promising results in the survival rate of this prosthesis type. The only subsequent operations were due to screw tip debridement, which indicates the necessity of accurate screw length in the radial plate. High satisfaction rate, consensus on recommending this surgery to others, and choosing the same surgery for the contralateral wrist, confirms the substantial improvement that patients experienced after this type of surgery. All patients reported that they have improved in their activities of daily living, motion, strength and lifting capacity as compared to pre-operatively. Also, objective wrist motion at the final clinic visit showed all patients regaining their functional range of motion. A woman with Ehlers-Danlos underwent non-simultaneous bilateral implant arthroplasty and she was pleased with her outcome.
DRUJ, as a link between radius and ulna, enables pronation and supination of the distal radius around ulnar head. Moreover, loads during lifting and gripping are transmitted through this area (2). In a deranged joint, the common complaints are usually pain and instability which may limit the ability to perform daily activities. Historical treatments are still commonly performed as a salvage procedure, however, with the invention and development of new systems to overcome previous complications, trends are growing toward enhancing near normal anatomy.
Scheker et al published the first report in 2001 on 23 patients with a mean of 15 months follow-up. In his series, all of the patients achieved full range of motion and relief from pain without any major complication (7). In the subsequent reports, there was 100% survival rate after 5 years and the functional abilities including grip strength and forearm rotation reached close to the normal side (9, 11). Bizimungu and Dodds in a 5 year follow-up report after 10 Aptis arthroplasties achieved flexion, extension, supination, and pronation of 32°, 45°, 73°, and 70°, respectively (8). Also the average grip strength was 55 Ibs with a mean pain score of 3.6 (8). Similarly, Axelsson and Sollerman reported their experience with Aptis prosthesis on eight patients with a mean follow-up of 3.7 years (3). In their series, all of the patients had 1 to 7 previous failed surgeries. The survival rate was 100% with regaining 80/90 supination, 70/75 pronation, and 21/29 kg grip strength in comparison to the contralateral side (3). Besides the advantages of Aptis in traumatic situations, its use in Madelung’s deformity has also showed improved results, with the most prominent change in regaining supination (12).
Distal radioulnar joint injuries are disabling and patients usually undergo one or more salvage surgeries prior to receiving an arthroplasty. The Aptis prosthesis has shown satisfactory results with 100% survival rate in all reports. The constrained design of this prosthesis gives enough stability to prevent painful subluxation. DRUJ implant arthroplasty seems to be an answer to these unresponsive complicated injuries, and possibly can be considered as the first line treatment in reconstructing this joint.
References
- 1.Degreef I, De Smet L. The Scheker distal radioulnar joint arthroplasty to unravel a virtually unsolvable problem. Acta Orthop Belg. 2013;79(2):141–5. [PubMed] [Google Scholar]
- 2.Sauerbier M, Arsalan-Werner A, Enderle E, Vetter M, Vonier D. Ulnar head replacement and related biomechanics. J Wrist Surg. 2013;2(1):27–32. doi: 10.1055/s-0032-1333464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Axelsson P, Sollerman C. Constrained implant arthroplasty as a secondary procedure at the distal radioulnar joint: early outcomes. J Hand Surg Am. 2013;38(6):1111–8. doi: 10.1016/j.jhsa.2013.03.030. [DOI] [PubMed] [Google Scholar]
- 4.Ewald TJ, Skeete K, Moran SL. Preliminary experience with a new total distal radioulnar joint replacement. J Wrist Surg. 2012;1(1):23–30. doi: 10.1055/s-0032-1324407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kapandji AI. Distal radio-ulnar prosthesis. Ann Chir Main Memb Super. 1992;11(4):320–32. doi: 10.1016/s0753-9053(05)80480-6. [DOI] [PubMed] [Google Scholar]
- 6.Schuurman AH, Teunis T. A new total distal radioulnar joint prosthesis: functional outcome. J Hand Surg Am. 2010;35(10):1614–9. doi: 10.1016/j.jhsa.2010.06.026. [DOI] [PubMed] [Google Scholar]
- 7.Scheker LR, Babb BA, Killion PE. Distal ulnar prosthetic replacement. Orthop Clin North Am. 2001;32(2):365–76. doi: 10.1016/s0030-5898(05)70256-x. [DOI] [PubMed] [Google Scholar]
- 8.Bizimungu RS, Dodds SD. Objective outcomes following semi-constrained total distal radioulnar joint arthroplasty. J Wrist Surg. 2013;2(4):319–23. doi: 10.1055/s-0033-1358544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Savvidou C, Murphy E, Mailhot E, Jacob S, Scheker LR. Semiconstrained distal radioulnar joint prosthesis. J Wrist Surg. 2013;2(1):41–8. doi: 10.1055/s-0032-1333466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scheker LR. Implant arthroplasty for the distal radioulnar joint. J Hand Surg Am. 2008;33(9):1639–44. doi: 10.1016/j.jhsa.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 11.Scheker LR, Martineau DW. Distal radioulnar joint constrained arthroplasty. Hand Clin. 2013;29(1):113–21. doi: 10.1016/j.hcl.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Coffey MJ, Scheker LR, Thirkannad SM. Total distal radioulnar joint arthroplasty in adults with symptomatic Madelung’s deformity. Hand (N Y) 2009;4(4):427–31. doi: 10.1007/s11552-009-9182-y. [DOI] [PMC free article] [PubMed] [Google Scholar]