Abstract
Background:
There is still controversy regarding the best technique for ankle arthrodesis to acheive stable rigid fixation along with reconstructing a functional plantigrade foot. Moreover, existing techniques have complictions related to stability, soft tissue covering, fusion rate, and exposure.
Methods:
With the anterior approach exactly on the tibialis anterior sheath, the joint was exposed and previous hardware, if any, was removed and with the safe direct approach, the ankle, hindfoot, and indirectly the subtalar joints were accessed. Then fresh cancellous bone was obtained and complete denudation was preformed. Lastly, a narrow 4.5 millimeter plate was carefully placed on what was determined to be the best final position.In this prospective study, 12 patients with severe ankle pain and arthritis enrolled from February 2010 to January 2012. Eight of them had posttraumatic arthritis and deformity with hardware, two had rheumatoid arthritis, one had poliomyelitis with severe deformity of the foot and knee, and another had chronic ulcerative synovitis of the ankle joint. The patients were assessed clinically and radiographically for an average of two years (range: 13 months to 4 years) for functional recovery, range of motion, stability of the ankle, and imaging evidence of union.
Results:
Ankle deformities and pain in all 12 cases were corrected. With a short healing time and rapid recovery period, after six weeks all of the patients could walk independently. Also, scores of the Manchester-Oxford Foot Questionnaire (MOXFQ) improved significantly from 69 preoperatively to 33 postoperatively).
Conclusions:
Anterior ankle arthrodesis with molded plating can be an easy and safe way to manage deformities and it has excellent fusion rate and sufficient rigid fixation.
Key words: Ankle, Arthrodesis, Plating
Introduction
The end stage of any diseased condition in a joint is cartilage degeneration or severe dysfunction which affects 15% of the adult population (1). There are several conditions that lead to joint destruction including; infection, tumors, and rheumatoid arthritis, but the most frequent is posttraumatic arthritis. If the problem is only a malfunction, it can be treated with braces or reduced motion and load on the joint, but usually pain remains an important issue. In this situation large joints are treated with joint arthroplasty and small joints with resection arthroplasty that reduces pain while preserving some motion. However, the ankle, which is also a large joint, is different from other large joints as weight bearing adjacent to several small joints, without sufficient soft tissue, and with very complicated kinematics. These unique characteristics have led to ankle arthrodesis as the first choice for long term management because it preserves limb function better; however, in recent years, arthroplasty with accepted criteria and careful patient selection is being increasingly performed (2, 3).
There are several approaches and techniques for ankle arthrodesis according to the patient’s primary disease and severity of dysfunction, as well as the surgeon’s preference and experience. Nowadays, the best fusion technique is considered internal fixation (4). The distal tibia and fibula with the talus form a functional unit. The anterior border of this unit is wider than the posterior, making it suitable for anterior arthrodesis (5). Many surgeons prefer the cross screw technique; however, initial rigidity and early weight bearing is not excellent (6, 7). Under certain conditions, especially nonunions, infected cases and pantalar arthrodesis, retrograde nailing is preferred, although the technique is demanding and correction of severe deformities is difficult. Contrary, a very convenient and rigid way for ankle arthrodesis is plating. There are several techniques that consist of posterior, lateral and anterior plating.
The best position of arthrodesis is 10 degree external rotation without any flexion and varus or 5-10 degree valgus with slight posterior displacement of the talus (8, 9). However, all of the techniques require insertion of fresh cancellous bone on the site of the arthrodesis with the most rigid fixation possible and preservation of the plantigrade foot for walking.
The aim of this study was to introduce the method and results of special type of anterior ankle arthrodesis that we have done in recent years. With a well-done arthrodesis using a suitable plate, a very rigid fused ankle with the possibility of early ambulation can be achieved.
Materials and Methods
This case series is comprised of eight males and four females. The age of the patients was 26 to 65 years old at the time of surgery. In our institute these accepted guidelines were followed for indications of ankle arthrodesis:
Severe and painful ankle joint degeneration preferably with painless subtalar and hindfoot joints caused especially after trauma and pilon fracture, followed by infection, poliomyelitis, rheumatoid arthritis, and hemophilic arthritis
Severe deformity of the ankle and hindfoot
Severe instability and flail foot
Salvage for failed total ankle arthroplasty
All of the patients had severe ankle pain and arthritis. Posttraumatic arthritis of the ankle with previous hardware existed in eight cases and there was also one case of poliomyelitis with severe deformity of the foot and knee. Causes of arthrodesis in two cases were rheumatoid arthritis and in one case the problem was chronic monoarticular ulcerative synovitis. The patients were assessed clinically and radiographically for an average of two years (range: 13 month to four years). When a patient was considered a suitable candidate for ankle arthrodesis, their ankle was clinically and radiographically assessed.
Physical examination
Every patient was examined for ankle and subtalar range of motion, extremity alignment, ankle and foot stability, and soft tissue envelope. Two patients had compensatory malalignments as a result of poliomyelitis and rheumatoid arthritis which had to be taken into account.
Imaging
Anteroposterior and lateral views of the ankle and foot in weight bearing is necessary to confirm the end stage of arthrosis and assess alignment and bone quality. Usually MRI is not required except for suspicious cases of talar avascular necrosis and in this study there were no such cases.
Technique
Patients were placed in the supine position on a radiolucent table with a cushion under the ipsilateral buttock.
The anterior approach was carried out using a 15 centimeter anterior longitudinal incision centred on the tibialis anterior tendon 10 centimeters above the joint line to the talonavicular joint. The branches of superficial peroneal nerve were preserved and an extensor retinaculum split at the lateral border of the tibialis anterior tendon was performed. Then anterior arthrotomy was done and if a plate was present it was removed. Subcutaneous tissue in this region was not undermined except directly on the extensor retinaculum. We stepcut the retinaculum since it facilitates closure of the retinaculum after plate fixation, thus soft tissue coverage is better enhanced and tension on the suture line is lessened.
The majority of patients had arthrosis of the ankle with a history of pilon fracture, so first the previous plate and all the hardware was remove and then remaining cartilage with a shell of subchondral bone down to fresh bleeding cancellous bone was removed and denuded carefully with a high speed burr. If the cysts were large, autogenous cancellous bone was packed.
The position of the arthrodesis was at 10-degree external rotation of the foot with slight posterior displacement of the talus and without any flexion and varus. A narrow 4.5 mm compression plate was molded and compression at the site of arthrodesis was exerted by this mean. If in preoperative assessment it was decided to do pantalar arthrodesis with long cancellous screws using a plate, as in the case of the patient with poliomyelitis, it was possible to proceed. On average, two screws in the talus and three screws in the distal tibia were inserted.
There was one patient with poliomyelitis and flail knee and ankle. The patient had severe calcaneus deformit. Pantalar arthrodesis using this technique was done to reconstruct the plantigrade foot. Fusion site healed after three month (Figure 1A, 1B). There was a 10 centemeter shortening that had to be corrected by Elizarov technique (Figure 2). There was one patient with chronic hypertrophic ulcerative synovitis with incomplete ankylosis of the ankle and severe pain with a long history of prednisolon consumption that underwent pantalar arthrodesis (Figure 3) Complete pain relief was achieved within one month. In one case of previous pilon fracture fixation, there were signs of infection with elevated ESR up to 35 and a positive bone scan (Figure 4). Ankle arthrodesis with anterior plating was done with rapid recovery and complete fusion after two month was acheived. This patient was followed for 15 months after operation (Figures 5A, B). There was a case of ankle degeneration in a 60-year-old man who had a history of ankle fracture during childhood and longstanding malalignment of the ankle in weight bearing. Severe pain was superimposed since a previous year (Figure 6). In this patient, anterior ankle arthrodesis with deformity correction and anterior plating with two additional cross screws was done (Figure 7).
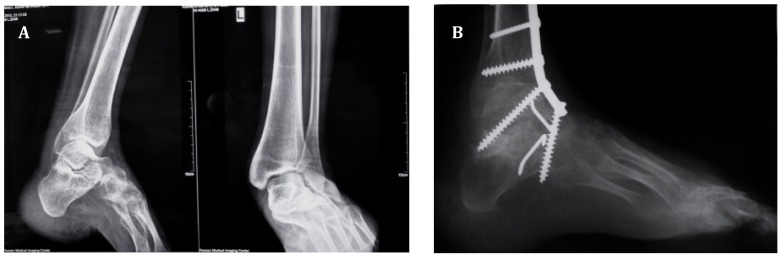
Figure 1.
A) Preoperative radiograph of the severely deformed foot and ankle in a patient with poliomyelitis. B) The last post-operative follow-up AP and lateral view radiographs after two years.
Figure 2.
Ten centimeter discrepancy between both limbs is shown.
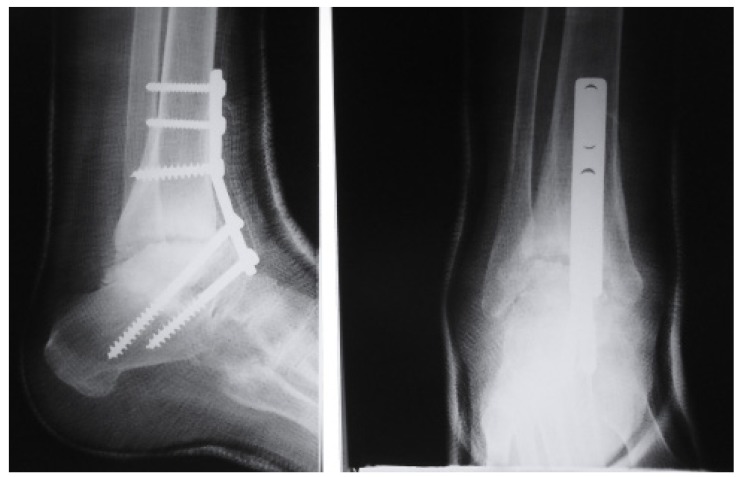
Figure 3.
Post operative lateral (left) anteroposterior (right) radiograph of the pantalar arthrodesis six weeks after surgery.
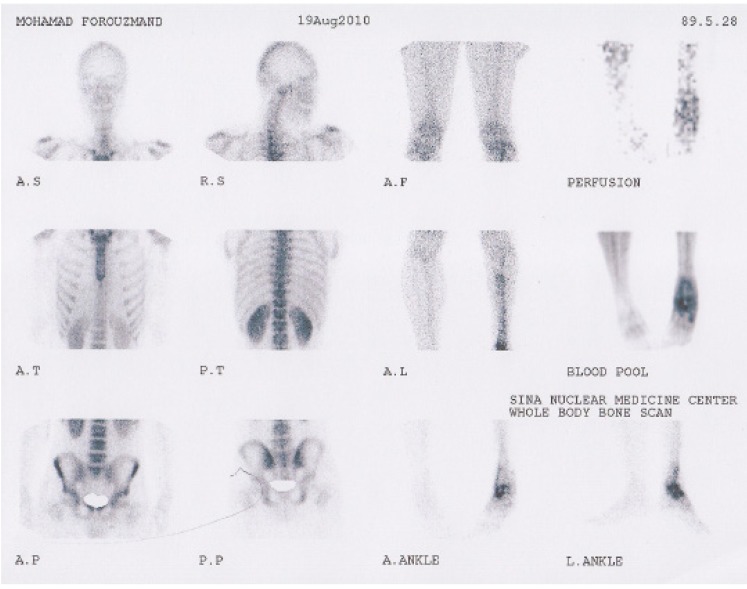
Figure 4.
Preoperative whole body scan of a previous pilon fracture with signs of infection.
Figure 5.
A) Post operative lateral (left) anteroposterior (right) ankle arthrodesis radiographs after two and eight months, retrospectively. B) Post operative lateral (left) anteroposterior (right) ankle arthrodesis radiographs after 15 months.
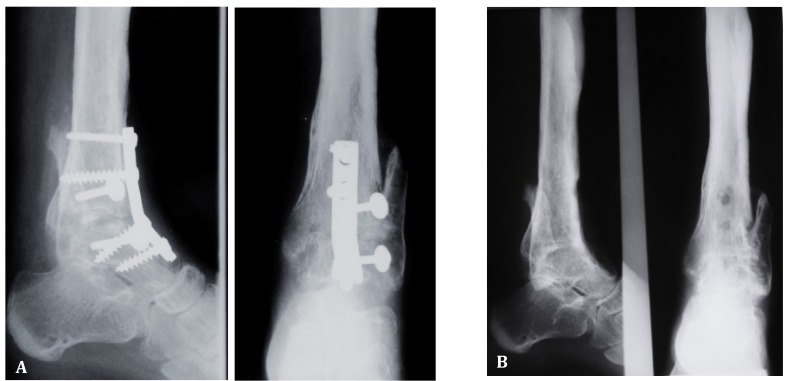
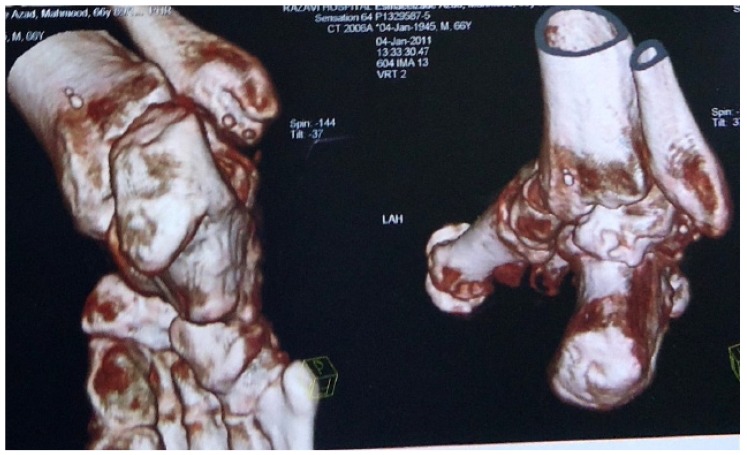
Figure 6.
Preoperative coronal and three dimensional x-ray scans of the degenerated malaligned ankle.
Figure 7.
Post operative lateral (right) anteroposterior (left) radiograph five months after index operation.
Postoperative care
After the operation, all of the patients wore a short leg non-weight bearing cast for three weeks. After that, walking with high-top leather shoes with a 3-centimeter heel was prescribed. Hardware was removed after one year, which is routine, because of its subcutaneous position.
Data related to the three domains (pain, walking/standing and social interaction) taken from the Manchester–Oxford Foot Questionnaire (MOXFQ) were analyzed before the operation and afterwards in the follow up period. MOXFQ is a 16-item questionnaire that was translated into Persian and recently validated and is being currently published. Its scores ranges between 16 and 80.
Results
In this study, 12 cases of ankle arthrodesis with anterior plating up to an average of two years (13 month to four years) were followed. mean age of patients was 52.8 years old. The time for complete recovery and weight bearing was eight weeks in all of the patients (6-12 weeks) and all of the deformities were corrected and complete plantigrade foot was achieved. The patients did not have any problem with their hardware; however, they were removed after one year because of their subcutaneous position. Mean MOXFQ score was 69 preoperatively with a 3.7 standard deviation. Mean (SD) scores decreased to 38+_8.4.
Overall, on the 0 to 10-point grading scale, patient satisfaction increased five points (range 3–8 points) at the last follow up. Four patients had limitation in recreational activities, but not in daily activities. None of the patients had ankle-hindfoot instability. Clinically, ankle-hindfoot alignment was good, with pre-planned foot position in all patients (slight equinus or plantigrade). Fusion was determined clinically and radiographically. All arthrodeses fused radiographicaly in the correct position within about 12 weeks (range: 8-15 weeks) and after three weeks rigidity was sufficient for walking and weight bearing. The position of the foot was satisfactory in all patients.
Discussion
The 12 patients of anterior ankle arthrodesis showed significant improvement in the MOXFQ subjective criteria. Based on the MOXFQ scoring the most satisfaction was seen in previous pilon cases and the least was in the patient with poliomyelitis and 10 centimeter limb shortening. Hence, our results show that anterior ankle plating is a convenient and effective way of ankle arthrodesis with low complication rates. However, accuracy in performing the technique and attention to arthrodesis alignment, joint denoding, and compression are mandatory in order to acheive excellent results.
There are several articles in favor of retrograde nailing for ankle arthrodesis (9-12). In this technique calcaneotalotibial arthrodesis can only be performed. Michael Geobel et al. in a short-term prospective study on a heterogenous group of cases, who required calcaneotalotibial, arthrodesis used retrograde intramedullary nails. Mean age of the patients was 53 years and most of their patients had post traumatic ankle and subtalar arthritis. They introduced this thechnique as a minimally invasive technique with a high union rate. At least two incisions, one lateral for transfibular arthrodesis and one plantar incision for the nail entry site, were made and in the presence of previous hardware, additional incisions became mandatory. The mean follow up period was 25 months and the complication rate was 21%. At the final follow up period they had 7% deep infections,10% nonunions, 7.2% revisions for nonunion and heel pain was observed in 14% (11). Patients in our study were compatible with this study because most of them had post traumatic injuries with a mean age of 52.8 years. However, we did not have a case of heel pain and infection or any limitation in accessing the joints needed for arthrodesis and only one incision was made. Also intramedullary nailing is not feasible with a lack of talus bone stock and we did not have this limitation during the plating technique (13). Special complications related to retrograde nailing in diabetic and nondiabetic patients were mentioned as heel pain and fibrosis, and lateral plantar nerve neuritis these complications are not seen in plating technique (12, 14).
Recently several articles have recommended the arthroscopic method for joint preparation; however, more than two thirds of arthritic patients are traumatic with previous incisions and hardware that require removal. In our study, reported complications and recovery time was better than the arthroscopic method (10, 11, 15).
Hans Zwipp et al. in a retrospective study on 92 ankle arthritis cases without subtalar or midtarsal problems used the four-screw method with the anterior approach medial to the tibialis anterior tendon. Patients that were not ideal candidates for screw fixation such as those with infection or severe deformity were excluded. Their patients’ mean age was 53 years. The reason for ankle arthritis varied, but 90% were posttraumatic. Their approach and joint preperation was similar to our study. Their fixation method was with four screws from the tibia to the talus. Their union rate was 99% and minor complications were 12% with one case of loss of correction. In midterm follow up they reported that 35% developed secondary or progressed subtalar arthritis (16).
In comparison, using the cross screw, which most surgeons prefer, we had lower complication rates with better stability (17). Usually post operative casting is done for three months, consisting of six weeks of non-weight bearing and another six weeks of a weight bearing cast, but we required our patients to undergo three to four weeks of casting followed by wearing high-top leather shoes. Midtarsal and subtalar joint motion is better preserved if shorter periods of immobilization (about six weeks) after ankle arthrodesis are used instead of longer immobilization times of 12 to 15 weeks (18). In this regard, we believe rigid fixation with a plate eliminates the need for long-time external support.
When fusion is established, functional outcome is related to the position of arthrodesis, foot alignment, and the amount of joints that are involved (16, 19).
Usually iliac bone grafting is used in bone defects like avascular necrosis of the talus or severe malalignment. We did not use iliac bone grafting, except in one case with previous pilon fracture and severe deformity. All of the patients had enough union without pain, although accepted high risk patients for nonunion such as infection and previous nonunion were included in this study (20).
We had one case of infection; however, with successful results. These patients are generally treated with elizarov or intramedullary nailing and a nonunion rate as high as 40% has been reported (4). The reason for excellent union was complete exposure of the ankle joint with good debridement and corticotomy from the anterior (21).
O’Neill et al. in a cadaver study compared locking plate to intramedullary nailing and showed that locking plate offered superior rigidity (22). This approach is easy with a low risk of neurovascular and soft tissue damage. In our study, more complete denude of the joint was possible and most importantly so was the use of strong hardware with perfect handling of arthrodesis positioning. Also, previous hardware removal was possible using one approach at the same time. We did not have any nonunion, hardware breakage, infection, or malalignment after surgery and early complete weight bearing was achieved in four weeks.
In a study done in 2005 to 2010, Slater et al. used anterior ankle arthrodesis with a customized synthesis plate and found that the anterior plate allows calcaneus to be incorporated into the arthrodesis. Anterior plating is successful even in cases of failed total ankle replacements. Also, this technique provides a variety of screw entry points and enough immediate rigidity with a high rate of fusion and few complications (5).
Our research showed that anterior ankle arthrodesis is a safe, easy and cost effective technique for patients with refractory ankle arthrosis that is associated with satisfactory early clinical outcomes.
This study had several limitations including the number of patients, short follow-up period, using MOXFQ for the functional outcome measure which is not as common as more popular measures such as SF36 and AOFAS, and non-homogenous patient cohort. There was a short-term follow up of the patients and this was because we wanted to show our technique and the short-term results related to this technique. On the other hand, long-term outcomes are related to limb alignment and number of involved joints; hence, we believe long term results should be compared with arthroplasty results.
References
- 1.Abidi NA, Gruen GS, Conti SF. Ankle arthrodesis: indications and techniques. J Am Acad Orthop Surg. 2000;8:200–9. doi: 10.5435/00124635-200005000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Buck P, Morrey B, Chao E. The optimum position of arthrodesis of the ankle. A gait study of the knee and ankle. J Bone Joint Surg Am. 1987;69:1052–62. [PubMed] [Google Scholar]
- 3.Demetracopoulos CA, Halloran JP, Maloof P, Adams SB, Jr, Parekh SG. Total ankle arthroplasty in end-stage ankle arthritis. Curr Rev Musculoskelet Med. 2013;6:279–84. doi: 10.1007/s12178-013-9179-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zuo Q, Wei X, Su J. Recent progress of fixation techniques of ankle arthrodesis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012;26:449–52. [PubMed] [Google Scholar]
- 5.Slater GL, Sayres SC, O’Malley MJ. Anterior ankle arthrodesis. World J Orthop. 2014;5:1–5. doi: 10.5312/wjo.v5.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Betz MM, Benninger EE, Favre PP, Wieser KK, Vich MM, Espinosa N. Primary stability and stiffness in ankle arthrodes—Crossed screws versus anterior plating. Foot Ankle Surg. 2013;19:168–72. doi: 10.1016/j.fas.2013.04.006. [DOI] [PubMed] [Google Scholar]
- 7.Kakarala G, Rajan DT. Comparative study of ankle arthrodesis using cross screw fixation versus anterior contoured plate plus cross screw fixation. Acta Orthop Belg. 2006;72:716–21. [PubMed] [Google Scholar]
- 8.Frigg A, Nigg B, Davis E, Pederson B, Valderrabano V. Does alignment in the hindfoot radiograph influence dynamic foot-floor pressures in ankle and tibiotalocalcaneal fusion? Clin Orthop Relat Res. 2010;468:3362–70. doi: 10.1007/s11999-010-1449-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haaker R, Kohja E, Wojciechowski M, Gruber G. Tibio-talo-calcaneal arthrodesis by a retrograde intramedullary nail. Ortop Traumatol Rehabil. 2010;12:245–9. [PubMed] [Google Scholar]
- 10.Caixeta TB, Júnior MOC, de Castro RV, Martins JS, Costa EN, Albieri AD, et al. Tibiotalocalcaneal arthrodesis with retrograde intramedullary nailing: 29 patients’ clinical and functional evaluation. Revista Brasileira de Ortopedia (English Edition) 2014;49:56–61. doi: 10.1016/j.rboe.2013.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goebel M, Gerdesmeyer L, Mückley T, Schmitt-Sody M, Diehl P, Stienstra J, et al. Retrograde Intramedullary Nailing in Tibiotalocalcaneal Arthrodesis: A Short-Term, Prospective Study. J Foot Ankle Surg. 2006;45:98–106. doi: 10.1053/j.jfas.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 12.Mendicino RW, Catanzariti AR, Saltrick KR, Dombek MF, Tullis BL, Statler TK, et al. Retrograde Intramedullary Nailing in Tibiotalocalcaneal Arthrodesis: A Short-Term, Prospective Study. J Foot Ankle Surg. 2006;45:98–106. doi: 10.1053/j.jfas.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Plaass C, Knupp M, Barg A, Hintermann B. Anterior double plating for rigid fixation of isolated tibiotalar arthrodesis. Foot Ankle Int. 2009;30:630–9. doi: 10.3113/FAI.2009.0631. [DOI] [PubMed] [Google Scholar]
- 14.Pochatko DJ, Smith JW, Phillips RA, Prince BD, Hedrick MR. Anatomic structures at risk: combined subtalar and ankle arthrodesis with a retrograde intramedullary rod. Foot Ankle Int. 1995;16:542–7. doi: 10.1177/107110079501600905. [DOI] [PubMed] [Google Scholar]
- 15.Cottino U, Collo G, Morino L, Cosentino A, Gallina V, Deregibus M, et al. Arthroscopic ankle arthrodesis: a review. Curr Rev Musculoskelet Med. 2012;5:151–5. doi: 10.1007/s12178-012-9119-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zwipp H, Rammelt S, Endres T, Heineck J. High union rates and function scores at midterm followup with ankle arthrodesis using a four screw technique. Clin Orthop Relat Res. 2010;468:958–68. doi: 10.1007/s11999-009-1074-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Valderrabano V, Hintermann B, Nigg BM, Stefanyshyn D, Stergiou P. Kinematic changes after fusion and total replacement of the ankle part 2: Movement transfer. Foot Ankle Int. 2003;24:888–96. doi: 10.1177/107110070302401203. [DOI] [PubMed] [Google Scholar]
- 18.Takakura Y, Tanaka Y, Sugimoto K, Akiyama K, Tamai S. Long term results of arthrodesis for osteoarthritis of the ankle. Clin Orthop Relat Res. 1999;361:178–85. doi: 10.1097/00003086-199904000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Buchner M, Sabo D. Ankle fusion attributable to posttraumatic arthrosis: a long-term followup of 48 patients. Clin Orthop Relat Res. 2003;406:155–64. doi: 10.1097/01.blo.0000038046.63743.c3. [DOI] [PubMed] [Google Scholar]
- 20.Baumhauer JF, Pinzur MS, Daniels TR, Lin SS, Beasley W, Donahue RM, et al. Survey on the Need for Bone Graft in Foot and Ankle Fusion Surgery. Foot Ankle Int. 2013;34:1629–33. doi: 10.1177/1071100713503815. [DOI] [PubMed] [Google Scholar]
- 21.Tan BY, Ng SY, Chong KW, Rikhraj IS. Tibiotalocalcaneal arthrodesis in a Singaporean hospital. J Orthop Surg (Hong Kong) 2013;21:51–4. doi: 10.1177/230949901302100114. [DOI] [PubMed] [Google Scholar]
- 22.O’Neill PJ, Logel KJ, Parks BG, Schon LC. Rigidity comparison of locking plate and intramedullary fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2008;29:581–6. doi: 10.3113/FAI.2008.0581. [DOI] [PubMed] [Google Scholar]