Abstract
Background:
Clavicle fractures are common and usually heal without complications. In this study, we evaluated the outcomes of non-operative versus operative management of displaced fractures.
Methods:
In a prospective clinical trial study, sixty-five patients with displaced clavicle mid-shaft fractures were non-randomly divided in two treatment groups. The first group underwent non-operative treatment with figure of 8 bandage (30 patients), and the other underwent operative treatment with plate fixation (35 patients). Figure of 8 bandage and 3.5 millimeter DCP plate with at least six cortical screws were used in non-operative and operative groups respectively. We followed up all patients at weeks 2, 6 and 12, and at month sixth. In addition to clinical examination and x-ray evaluation, we assessed satisfaction, DASH and Constant Shoulder Score for each individual.
Results:
The average durations of union were 19.3 and 24.4 weeks in operative and non-operative groups respectively (P=0.006). Satisfaction with operative treatment was 74.3% and with non-operative treatment was 66.7%, showing no significant difference (P=0.500). The non-union rate was 5.7% in the operative group and 13.3% in the non-operative group (P=0.518). A significant difference between the two groups in terms of DASH and Constant Shoulder Scores after the six-month follow-up was not found (P=0.352).
Conclusions:
According to our results, we recommend operative treatment in mid-shaft clavicle fractures only when there is a definitive indication.
Key words: Clavicle, Constant Shoulder Score, DASH score, Internal fixation, Non-operative management
Introduction
Clavicle fractures, accounting for about 2% of total body fractures and 34-45% of shoulder girdle injuries in adults, are one of the most common bone injuries in body. This fracture is more common in men (68%) (1).
Most clavicle fractures (69-81%) are in the middle one-third of the clavicle, which is the thinnest part and entails the least soft tissue, 17% in the lateral one-third and 2% in the medial one-third (2).
The most common mechanism of injury to the clavicle is direct trauma to the shoulder, causing a fracture in the middle part of the shoulder. Two-thirds of the injuries result in a diaphysis fracture of the clavicle in adults and has more displacements in comparison to the other fractures located in the medial and lateral one-third (3).
Traditionally, fractures of the middle clavicle are treated non-surgically by a hanging hand splint or a figure-eight bandage; a surgical intervention is rarely required. Previous studies indicate that even if a clavicle fracture is accompanied by a displacement, it is considered benign damage, and that if the fracture is treated non-surgically, it has a reasonable prognosis (4). Recent evidence, however, reveals that the final result of middle one-third clavicle fractures that were treated non-surgically, particularly those with quite large displacements or shortening, are not like that which was previously thought. Thus, recently there is a growing tendency toward surgical treatment (5).
Recent studies showed that the rate of non-union in fractures with a displacement of the middle clavicle that were treated by a non-surgical treatment is more than 15%, compared to 2.2% in surgical treatment (6).
Several studies have demonstrated the effectiveness of surgical fixation of the displaced clavicle fractures with a plate that resulted in a higher rate of union with less adverse effects (7).
This study aims to compare non-operative management of displaced mid-clavicle fractures with a figure-eight bandage and operative management with plate and screws in terms of union, final outcome and complications.
Materials and Methods
In a prospective clinical trial study, 70 patients with displaced mid-shaft fractures of the clavicle were referred to the Hospital of the Ahvaz University of Medical Sciences and enrolled in our study from 2011 to 2013. These patients were deliberately placed into two treatment groups: non-surgical (with figure-eight bandage) and surgical (with plate fixation).
Our inclusion criteria was as follows: between 18-60 years of age with closed isolated acute, displaced or angulated (fracture type was based on Robinson 2A2, 2B1, 2B2), fractures of the middle third of the clavicle.
Exclusion criteria included: open fractures, neurological compromise, fracture of the medial or lateral third of the clavicle, pathologic fractures, severe injury of soft tissue, multiple trauma, injury of the same side upper organ and medical disease.
Clavicle fracture patients who met the inclusion criteria were invited to participate in the study. The ethical committee of the university approved the study and all patients signed an informed constant form.
We missed five patients during follow-up due to travel, migration, and dissatisfaction, all of them belonging to the group with non-surgical treatment. Thus, 35 patients with a mean age of 31 years (SD=9.5) and 30 patients with a mean age of 30 years (SD=13.0) were left in the surgical and non-surgical groups, respectively. There were 10 females (28.6%) and 25 males (71.4%) in the surgical group and 7 females (23.3%) and 23 males (76.7%) in the non-surgical group.
After the explanation of the advantages and disadvantages of both therapeutic methods, the patients were placed in either the operative or non-operative group on their own volition.
Treatment for the operative group included undergoing open reduction and internal fixation (ORIF) using the anterosuperior approach.
All patients of the surgical group underwent ORIF under general anesthesia using a 3.5 millimeter plate with at least six cortical screws. One prophylaxis dosage of antibiotic (Cefazolin) was administered for all of the patients in the surgical group half an hour before surgery. The prophylaxis antibiotic was continued for 24 hours after surgical operation.
At the end of the second week, patients were visited, wounds were observed, control graphs were taken and shoulder pendulum motions were started. Both groups of patients were followed up at weeks 2, 6, 12 and after 6 months. Clinical examination and fracture radiography were done, and DASH and Constant Shoulder Scores were evaluated and recorded for all patients at the end of the treatment (Figure 1). Standard anteroposterior radiography was obtained at each visit to assess the healing process and any complications. Heeled fracture was defined as bony callus formation across the fracture fragments. DASH is a self–reported questionnaire designed to measure physical function and symptoms in patients with any of several musculoskeletal disorders of the upper limb. Shoulder function is measured by the Constant Shoulder Score, which includes the pain score, functional assessment, range of motion and strength measures. Patient satisfaction according to strength, shoulder function and pain was also assessed (7).
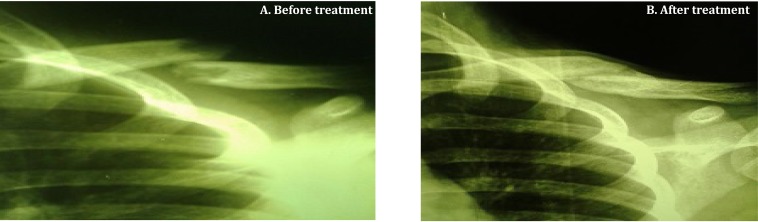
Figure 1.
Left clavicle fracture of a 18 years old man who was treated by non-surgical technique.
All statistical analyses were conducted by SPSS. Independent t-tests were used to compare quantitative data such as treatment duration, and Chi-square was employed to evaluate the relationship between type of treatment and qualitative data such as side effects.
A P-value of less than 0.05 was considered a significant difference.
In both groups, most of the patients were men, and traffic accidents with motorcycle or car were the most common mechanism of injury. The right extremity and dominant hand were more commonly affected in both groups. More details are available in Table 1.
Table1.
General information regarding patients in both groups, managed operatively and non-operatively
| Basic Information | Operative Group | Non-operative |
|---|---|---|
| Total number | 35 | 30 |
| Male | 25(71.4%) | 23(76.7%) |
| Female | 10(28.6%) | 7(23.3%) |
| Mean age | 31.0 | 31.8 |
| Right hand | 20(57.1%) | 18(60%) |
| Left hand | 15(42.9%) | 12(40%) |
| Dominant hand | 21(60%) | 18(60%) |
| Non-dominant hand | 14 (40%) | 12(40%) |
| Fracture type 2A2 | 8(22.9%) | 7(23.3%) |
| Fracture type 2B1 | 18(51.4%) | 15(50%) |
| Fracture type 2B2 | 9 (25.7%) | 8(26.7%) |
| Injury from traffic accidents | 24(68.6%) | 22(73.3%) |
| Injury from direct trauma | 2(5.7%) | 2(6.7%) |
| Injury from falling down | 9(25.7%) | 6(20%) |
Results
Both groups were compared on the basis of patient satisfaction according to treatment. In the surgical group, 26 patients (73.3%) were satisfied with treatment and 9 patients (25.7%) were dissatisfied with the result of treatment. In the non-surgical group, 20 patients (66.7%) were satisfied with treatment and 10 people (33.3%) were dissatisfied (P=0.50). Most dissatisfaction resulted from clavicle appearance (13.8%), pain (21.5%), motion restrictions during performing heavy work with more reduced ability than the opposite side (16.9%). Patients’ overall satisfaction was defined with a separate questionnaire evaluating functional and anesthetic outcomes.
Five patients (14.3%) in the operative group had surgical site infections, while there were no cases of infection in the non-surgical group (P=0.03). Except for one case, which was treated with irrigation and debridement and intravenous antibiotics, other cases were treated by oral antibiotic.
Six patients (17.1%) in the surgical group and 6 patients (20%) in the non-surgical group complained of pain at the fracture site after complete union (P=0.7). The average radiologic union time was 19.3 weeks (SD=5.4) in the surgical group and 24.4 weeks (SD=3.8) in the non-surgical group (P=0.006).
Two patients (5.7%) of the surgical group and four patients of the non-surgical group (13.3%) suffered from nonunion. There was no significant difference between the two groups (P=0.518).
Eighteen patients (60%) in the surgical group and seven (20%) inthe nonsurgical group had delayed union (P=0.001). Delayed union was more common in the non-surgical treatment group.
The average time of return to work among the surgical patients was estimated 8.5 weeks (SD=1.9) after treatment and 8.8 weeks (SD=1.9) after treatment in the nonsurgical group, indicating no significant difference between two groups (P=0.32).
The average DASH score was 24.6 (range 0-88) for the surgical group and 22.7 (range 0-87) for the nonsurgical group, yielding no significant difference between the two groups (P=0.352).
The average Constant Shoulder Score was 20.97 (SD=5.7) for the surgical group and 20.53 for the non- surgical group (SD=7.04) (P=0.787) indicating no significant difference between the groups. Each group of patients was followed-up for 6 months.
Four patients of the nonsurgical group who suffered from nonunion had fracture type 2B2 according to Robinson’s division were treated with autogenous bone grafts and surgery operations with fracture fixation plates and achieved union.
Discussion
This study is a clinical trial in which patients were compared and matched in terms of age, sex, injury mechanism, injury site, dominant or non-dominant hand, and type of fracture according to Robinson’s division in two groups: surgical and nonsurgical.
Analysis revealed that there was a significant difference between two surgical and nonsurgical groups in terms of satisfaction level. Our result is compatible with Till et al.’s findings on 52 mid-third fractures of clavicle with complete displacement that was reported from 4.4% to 31% (6).
The observed infection rate after surgical treatment was 14%, meaning there was a significant difference between the two groups. Sahal et al. treated 132 patients in two surgical and nonsurgical groups and compared them. The degree of post-operation infection was reported at about 6% in their study(8).
Zlowodzki et al. reported a post-operational infection rate in patients treated surgically with plate fixation near 1%. Thus, the rate of post-operation infection in our study was greater than that of previous studies (9).
There was no significant difference in the functional results of the Constant Shoulder Scores and DASH scores for the two groups; however, this result differs that of Saha et al., in which the Constant Shoulder Score and DASH score were better in the surgical group (8).
In another study by Kaisa et al., 28 patients were surgically treated and 32 were non-surgically treated by figure-eight bandage and followed-up for one year. Similar to our study, the two groups did not have a significant difference in terms of DASH score and Constant Shoulder Score (10). In the study by Sahal et al. (8), the average radiographic union time was 28.4 weeks in the nonsurgical group and 16.4 weeks in the surgical group. This study shows an average radiographic union time of 1924.37 26 weeks in the nonsurgical group and 19.26 weeks in the surgical group. Our findings are compatible with Sahal et al.’s study.
In Sahal et al.’s study, there were two and seven cases of nonunion in the surgical and nonsurgical groups, respectively. In our study these amounts were two and four cases in the surgical and nonsurgical groups, respectively. The rate of nonunion in the nonsurgical group was more than that of the surgical group in Sahal et al.’s study, and such results are confirmed by this study (8).
In Sahal et al.’s study, nine cases of delayed union were observed in the nonsurgical group while there were no cases in the surgical group. However, 18 cases of symptomatic delayed union were observed in the non-surgical group and 7 cases in the surgical group. When compared to our study, delay in union was higher in the nonsurgical group (8).
Moreover, Ilija Ban et al. examined delayed union rates among 365 patients and observed that the rate was less in patients treated surgically compared to those treated nonsurgically (11). Our results are confirmed by the above result; that is, delayed union is more commonly observed in nonsurgical treatment than in surgical treatment.
Robinson et al. reported a 21% nonunion rate for displaced and cracked mid-shaft clavicle fractures by nonsurgical treatment (12). In another study, Brinker et al. mentioned a degree of nonunion between 20 to 33% of cracked or displaced fractures in young males (13).
In a meta-analysis evaluating 214 mid-shaft clavicle fractures, rates of 15.1% nonunion for non-surgical treatment and 2.2% for surgical group were reported (9).
Our results are comparable to those of these three studies. In our study, the rate of non-union (13.3%) in nonsurgical treatment was higher than that of surgical treatment (5.7%).
Dhoju et al. treated 20 patients suffering from clavicle fractures (Edinborge type 2) via surgery operation and fixation with reconstruction plate (14). All of the patients achieved anatomic union within 16 weeks or less, and only 2 people suffered from side effects such as infection that required follow up treatment. In our study, patients who were surgically treated by plate had a smaller average clinic radiographic union time (19.26 weeks) than did those in the nonsurgical group (24.37 weeks).
Bajuri et al. surgically treated 70 patients suffering from a fracture in the middle one-third of the clavicle (15). They observed an average Constant Shoulder Score of 31.69 that is compatible with our average Constant Score.
There were some limitations to our study, Since the patients themselves selected their treatment, they were not randomly and evenly distributed into two groups. We could not investigate other factors such as range of motion, pain score and shoulder strength influencing the results of treatment. Finally, the six-month follow-up time in this study, was not enough for complete evaluation of the outcome and any chronic complications.
Fractures with displacement and a shortened clavicle (Robinson’s 2B2, 2B1 and 2A2) that are treated by surgical operation have a less delay union times than nonsurgical treatment.
Functional results of two groups, however, did not have a significant difference. Although nonunion and delayed union risks are significant in nonsurgical treatment, in surgical operations, infection and plate removal are significant risks.
Since the results of both surgical and nonsurgical treatment are similar, and with regard to the risk of surgical operation, surgical treatment is recommended with caution.
Acknowledgments
This study was financially supported by the Ahvaz Jundishapour Univesity of Medical Sciences.
References
- 1.Neer CS., II Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 2.Van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2012;21(3):423–9. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 3.Stanley D, Trowbridge EA, Norris SH. The mechanism of clavicular fracture. A clinical and biomechanical analysis. J Bone Joint Surg Br. 1988;70(3):461–4. doi: 10.1302/0301-620X.70B3.3372571. [DOI] [PubMed] [Google Scholar]
- 4.Browner BD, Jupiter JB. Skeletal Trauma. 3rd. Philadelphia: WB Saunders; 2003. [Google Scholar]
- 5.Graves ML, Geissler WB, Freeland AE. Midshaft clavicular fractures: the role of operative treatment. Orthopedics. 2005;28(8):761–4. doi: 10.3928/0147-7447-20050801-12. [DOI] [PubMed] [Google Scholar]
- 6.Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79(4):537–9. doi: 10.1302/0301-620x.79b4.7529. [DOI] [PubMed] [Google Scholar]
- 7.Tabatabaei S, Shalamzari S. Treatment of displaced midshaft clavicular fractures: A comparison between smooth pin and LCDCP and reconstruction plate fixation. Pak J Med Sci. 2011;27(5):1129–34. [Google Scholar]
- 8.Altamimi SA, McKee MD. Canadian Orthopaedic Trauma Society. Nonoperative Treatment Compared With Plate Fixation of Displaced Midshaft Clavicular Fractures. J Bone Joint Surg Am. 2008;90:1–8. doi: 10.2106/JBJS.G.01336. [DOI] [PubMed] [Google Scholar]
- 9.Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Evidence-Based Orthopaedic Trauma Working Group. Treatment of acute midshaft clavicle fractures: systematic review of 214 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19:504–7. doi: 10.1097/01.bot.0000172287.44278.ef. [DOI] [PubMed] [Google Scholar]
- 10.Virtanen KJ, Remes V, Pajarinen J, Savolainen V, Björkenheim JM, Paavola M. Sling Compared With Plate Osteosynthesis For Treatment of Displaced Midshaft Clavicular Fractures. J Bone Joint Surg Am. 2012;94(17):1546–53. doi: 10.2106/JBJS.J.01999. [DOI] [PubMed] [Google Scholar]
- 11.Ban I, Branner U, Holck K, Krasheninnikoff M, Troelsen A. Clavicle fractures may be conservatively treated with acceptable results-asystematic review. Danish Med J. 2012;59:1–7. [PubMed] [Google Scholar]
- 12.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86:1359–65. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Brinker MR, Edwards TB, O’Connor DP. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2005;87(3):676–7. doi: 10.2106/00004623-200503000-00034. [DOI] [PubMed] [Google Scholar]
- 14.Dhoju D, Shrestha D, Parajuli NP, Shrestha R, Sharma V. Operative fixation of displaced middle third clavicle (Edinburg Type 2) fracture with superior reconstruction plate osteosynthesis. Kathmandu Univ Med J (KUMJ) 2011;9(36):286–90. doi: 10.3126/kumj.v9i4.6346. [DOI] [PubMed] [Google Scholar]
- 15.Bajuri MY, Maidin S, Rauf A, Baharuddin M, Harjeet S. Functional Outcomes of Conservatively treated Clavicle fractures. Clinics (Sao Paulo) 2011;66(4):635–9. doi: 10.1590/S1807-59322011000400019. [DOI] [PMC free article] [PubMed] [Google Scholar]