Abstract
The psychological construct of self-efficacy plays a key role in both general, as well as addiction specific, models of health behavior change and is well supported empirically. As a predictor of treatment outcome it has proven useful; however, in order to further clarify the nature and role of self-efficacy in predicting the complexities of addiction recovery, it would seem crucial also to consider an individuals’ motivation to carry out that future behavior, because the degree to which a measure of self-efficacy predicts behavior may be contingent upon whether that individual is also motivated to enact it. To this end, we tested an interaction model of self-efficacy and motivation on treatment outcome. Young adults (N=302; M age 20; 74% male) undergoing residential SUD treatment were assessed at treatment intake, discharge, and 3, 6, and 12 months post-discharge on self-efficacy (SE), motivation for sobriety (MS), and percent days abstinent (PDA). Hierarchical Linear Modeling (HLM) results revealed main effects for abstinence SE and MS across time but a significant interaction was detected, indicating that the influence of SE on PDA depended on MS. Further analysis revealed that for patients high in SE the level of MS made a small, but significant, difference on PDA, while for those low in SE, high MS made a substantial difference, such that their outcome was not different than patients with high SE. Findings highlight conceptual nuances in self-efficacy theory; and, clinically, convey optimism that, even if a patient reports low confidence in their ability to remain abstinent, it does not necessarily follow that they will have poor outcome, especially if they have a strong recovery motivation.
Keywords: self-efficacy, motivation, commitment to sobriety, treatment, relapse, theory, young adults, addiction
1. Introduction
It has been argued that among the types of thoughts that affect human behavior none is more significant or pervasive than people’s judgments of their capabilities to cope effectively with different realities (Bandura, 1986). Consistent with this assertion, this psychological construct of “self-efficacy” plays a key role in both general, as well as addiction specific, models of health behavior change. Its pivotal value is stressed, for example, in Social Cognitive learning Theory (Bandura, 1986), the Theory of Planned Behavior (Ajzen & Madden, 1986), the Health Beliefs Model (Rosenstock, Strecher, & Becker, 1988) the Transtheoretical Model (TTM) (Prochaska & DiClemente, 1983) as well as in the influential cognitive-behavioral Relapse Prevention Model (Marlatt & Gordon, 1985; Witkiewitz & Marlatt, 2004). The construct is also well supported empirically. Self-efficacy is among the most consistent predictors of abstinence and substance use relapse (Randall et al., 2003), and has support as a common process variable that has been shown to mediate the beneficial effects of myriad theoretically distinct interventions (Forcehimes & Tonigan, 2008; Kadden & Litt, 2011; Kelly, Magill, & Stout, 2009). Consequently, it has clear clinical and practical relevance to substance use disorder (SUD) treatment and research.
In the SUD treatment arena, the accepted theoretical importance of self-efficacy has led to the development and validation of different self-efficacy measures that help predict outcomes among treated populations (DiClemente, Carbonari, Montgomery, & Hughes, 1994; Hoeppner, Kelly, Urbanoski, & Slaymaker, 2011; Randall et al., 2003). As a predictor of SUD treatment outcome it has proven useful, often explaining small, but significant, proportions of outcome variance. In further developing explanatory models that underscore the importance of individuals’ self-efficacy in predicting and explaining the complex task of addiction recovery, however, it would seem critical also to consider an individuals’ motivation or commitment to carry out that future behavior, because the degree to which a measure of self-efficacy predicts future behavior may be contingent upon whether that individual is also motivated to enact the behavior. Concretely, an individual may feel complete confidence in their ability to perform a future task (e.g., stopping substance use), but may have little desire or motivation to do so (i.e., “I’m confident I can stop, but I’m not sure I want to”). Conversely, someone may have low confidence in their ability to perform a future task, but may be highly motivated to perform it (“I really want to stop, but I’m not sure I can”). Our understanding of the nature and role of self-efficacy, therefore, might be enhanced by consideration of an individual’s motivation or commitment to perform the behavior. Because the construct of motivation appears so crucial to understanding the potential of self-efficacy to predict and explain future behavior, it seems imperative to include this key element of how motivationally committed an individual is to enacting the behavior. This construct, however, seldom has been studied in this light (Bandura, 1997)..
To investigate this empirically, the current study sought to examine the predictive utility of both abstinence self-efficacy and motivation for sobriety, but most importantly, their interaction, on substance use outcome in a large clinical sample. Examination of this interaction should help clarify further the nature of the relationship between abstinence self-efficacy and future sobriety. We predicted the effect of self-efficacy on abstinence would hinge on motivation, such that patients high in self-efficacy and high in motivation would have the best outcomes, but individuals high in self-efficacy and low in motivation would have significantly worse outcomes. We also predicted that patients low in self-efficacy and low in motivation would have the worst outcomes, and that patients low in self-efficacy but high in motivation would have marginally better outcomes.
2. Method
2.1 Participants
Participants were 302 young adults (18-24 years old) undergoing residential treatment and enrolled in a naturalistic study of treatment process and outcome. At admission, participants were 20.4 years old on average (SD = 1.6). Most were Caucasian (94.7%); 1.7% identified as American Indian, 1.3% identified as African American, and 1.0% as Asian (1.3% reported “other” or missing). Participants were predominantly male (73.8%), and all were single. At admission, 11.9% were employed full-time and 41.1% were enrolled in school (high school or college). Most had completed high school: 43.4% had a high school diploma and 39.8% had some college education (Table 1). The most commonly reported “drug of choice” was alcohol (28.1%) and marijuana (28.1%), followed by heroin or other opiates (22.2%), cocaine or crack (12.3%), and amphetamines (6.0%). Small proportions reported benzodiazepines (2.0%), hallucinogens (1.0%), or ecstasy (1.0%) as their drug of choice.1
Table 1.
Characteristics of the sample at treatment intake (n=302)
| Variable | Mean ± SD N (%) |
|---|---|
| Demographic Variables | |
| Age (years) | 20.35 ± 1.58 |
| Gender: Male | 223 (73.8) |
| Marital Status: Single | 301 (100) |
| Race: Caucasian | 286 (94.7) |
| Employment: Full-time | 36 (11.9) |
| Education: Some college or greater | 120 (39.8) |
| Student status: Enrolled | 122 (41.1) |
| Clinical Variables | |
| Percent Days Abstinent | 23.98 ± 28.15 |
| Self-Efficacy | 6.96 ± 2.59 |
| Motivation for Sobriety | 24.00 ± 5.23 |
| Psychiatric Diagnoses | |
| Mood Disorder | 186 (61.6) |
| Anxiety Disorder | 126 (41.7) |
| Eating Disorder | 26 (8.6) |
| Substance Use Disorders† | |
| Alcohol | 227 (75.7) |
| Sedatives | 46 (15.3) |
| Cannabis | 216 (72.2) |
| Stimulants | 67 (22.3) |
| Opiates | 102 (34.0) |
| Cocaine | 139 (46.3) |
| Hallucinogens | 46 (15.3) |
| Polydrug | 38 (12.7) |
| Other | 12 (4.0) |
Abuse or dependence
Participants in this private treatment sample were more likely to be Caucasian than young adults (18-24 years old) in public sector residential treatment (76%) (Substance Abuse and Mental Health Services Administration, 2009), or adults (18+ years old) in the broader private treatment sector (71%) (Roman & Johnson, 2004). They were, however, comparable in terms of gender, marital status, and employment status, suggesting that results are broadly generalizable to youth treated for substance-related disorders in the US.
2.2 Treatment
Treatment was comprehensive and multi-faceted, based in a 12-step philosophy of recovery. In addition to the 12-step orientation, motivational enhancement and cognitive-behavioral therapeutic approaches, as well as family therapy, were used to facilitate problem recognition and treatment engagement, and to support recovery. Programming included clinical assessment, individual and group therapy, and a host of specialty groups tailored to meet the needs of individual clients, such as relapse prevention, anger management, eating issues, dual disorders, gender issues, assertiveness training, and trauma. Integrated mental health care was available, including clinical assessment, therapy, and medication management. Participants’ average length of stay at the residential treatment center was 25.5 days (SD = 5.7, ranging from 4 to 35 days). The majority (83.8%) were discharged with staff approval, indicating a high rate of treatment completion. Of the remainder, 9.3% left against staff advice and 7.0% left at the request of staff.
2.3 Procedure
Participants were enrolled in the study shortly after admission. A total of 607 young adults were admitted to treatment during the recruitment period (October 2006 to March 2008). All of those aged 21-24 years old were approached for study enrollment, as well as every second individual aged 18-20. This was done to ensure sufficient representation of the older age group, given the predominance of those aged 18-20 at the treatment center. A small number of potential participants left treatment before recruitment could take place (n = 6) or were not approached by staff for recruitment (n = 14). Of those approached (n = 384), 64 declined or withdrew participation. Reasons for non-participation included not wanting to participate in the follow-up interviews (44%), not being interested in the study (31%), wanting to focus on treatment (14%), and legal issues (2%). Following enrollment, an additional 17 participants withdrew prior to the baseline assessment and the consent for one participant was misplaced. The final sample of 302 represents 78.6% of those approached for participation.
Research staff conducted assessments at baseline, end of treatment, and 3, 6, and 12 months post-discharge. Each assessment included an interview portion, completed either in person or by telephone, and self-administered surveys, which were returned by mail. Only end of treatment, 3-, 6- and 12-month assessment data were used for these analyses because the assessment battery at these time points contained the variables of interest. Participants were reimbursed $30 for the end of treatment assessment and $30, $40, and $50 for the post-treatment assessments at 3-, 6- and 12-months, respectively. Assessment completion rates were 87.1% (n=263) at end of treatment, 81.8% (n=248) at 3-month follow-up, 74.3% (n = 225) at 6-month follow-up, and 71.3% (n = 216) at 12-month follow-up.
At each time point, those who did not complete the assessment were compared to those who were retained in terms of gender, age, race, education, employment status, and baseline psychological symptoms (BSI), dependence severity (LDQ) and percent days of abstinent (from all substances except nicotine) in the 90 days prior to treatment (α=.05). Relative to those with post-secondary education, those with a high school education or less were more likely to be missed at all time points, both in-treatment and post-treatment. The study was conducted in accordance with the Institutional Review Board at Schulmann Associates IRB, an independent review board, and all participants signed informed consent documents.
2.4 Measures
Demographics
Background sociodemographic information, including age, gender, marital status, race and ethnicity, employment status, educational attainment, and student status, was obtained, with full permission, from the medical record.
Alcohol and other drug use
The Form-90 (Miller & Del Boca, 1994; Project MATCH Research Group, 1993;. Project MATCH Research Group, 1993) is an interview-based measure capturing substance use, use of psychiatric medications, criminal justice system and treatment involvement, and consequences related to work or school. The recall period for the baseline interviews was 90 days. However, a sub-sample (n = 35) completed an interview subsequent to missing a prior one and, thus, reported over a longer than average period of time assessment window (e.g., they missed the 6 month assessment and reported on behavior between 3-month and 12-month follow-up interviews). Primary outcome measures derived from this instrument included percentage of days abstinent (PDA) from all substances (except nicotine). The Form-90 has been tested with adult and adolescent samples and has demonstrated test-retest reliability and validity (Slesnick & Tonigan, 2004; Tonigan, Miller, & Brown, 1997).
Abstinence Self-Efficacy
A single-item assessment of self-efficacy was administered as part of the assessment battery at intake, end of treatment, and 3-, 6- and 12-months post-treatment. The item asked participants to rate the following item on a 10-point scale ranging from not confident (1) to very confident (10): “How confident are you that you will be able to stay clean and sober in the next 90 days, or 3 months?” The endpoints and midpoint were anchored, but most values did not have a verbal description. This single-item measure of self-efficacy has been validated and found to be a strong predictor of relapse, superior to other longer gold standard measures (Hoeppner et al., 2011).
Motivation for Recovery
The commitment to sobriety (CSS) scale was used to capture the construct of recovery motivation. The CSS is a 5-item measure of motivation, designed to assess the level of patients’ commitment to sobriety from alcohol and other drug use. Items rate the level of agreement with statements concerning abstinence (e.g., “Staying sober is the most important thing in my life” and “I am totally committed to staying off alcohol/drugs”). Each is rated on a 6-point Likert scale from strongly disagree (1) to strongly agree (6) (Kelly & Greene, Under review). In terms of predicting future abstinence, this measure has been shown to outperform traditional measures of motivation commonly used in the substance field (e.g. the SOCRATES) and shows good internal consistency, as well as convergent, and discriminant validity (Kelly & Greene, Under review).
2.5 Biological Assay
To verify self-reported abstinence from alcohol and other drugs, saliva tests (Cone et al., 2002) were administered on a subsample of subjects that lived within 50 miles of the treatment facility and could attend follow-up interviews in-person (ranging from 2.8% of the sample at 12 months to 21.8% of the sample at 1 month). Abstinence was confirmed in 94.5% to 100% of subjects who self-reported abstinence from all substances during the assessment period prior to each follow-up. Positive tests results were obtained for 1 subject who reported abstinence prior to the 3-month follow-up and this person was removed from the analysis.
2.6 Analysis Plan
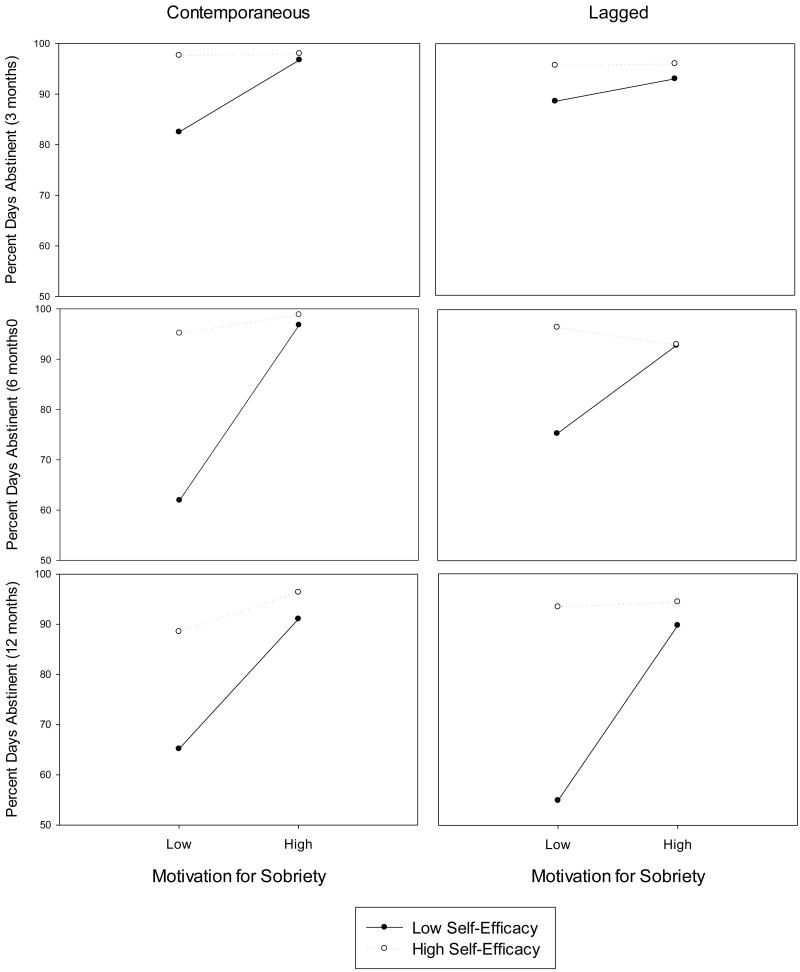
We first computed descriptive demographic and clinical summary data from the sample at treatment intake followed by spearman rank order correlations among commitment to sobriety (CSS), self-efficacy, and PDA at each assessment period. Using this information, we created an indicator variable denoting high versus low self-efficacy and high versus low motivational commitment using median splits at each time point. We then examined measures of central tendency and dispersion of the substance use outcome variable, percent days abstinent (PDA). PDA was considerably skewed and required a negative log transformation such that it would adhere to the statistical assumptions required for further analyses. To examine the association between both motivation and self-efficacy on PDA we ran contemporaneous as well as lagged models. This was done to enhance causal inference (i.e., temporal precedence of motivation and commitment relative to PDA). We created lagged variables such that CSS and self-efficacy could be regressed on PDA reported at the subsequent assessment period. We constructed parallel longitudinal models for both the lagged and contemporaneous designs using hierarchical linear models (HLM). These models yield estimates of the average effects of the relationships among these variables over time. Independent variables included the dichotomized indicator variables for motivation and self-efficacy, upon which we added the interaction between motivation and self-efficacy. To further understand the nature of this interaction, we used slicing as a post-hoc analysis to test for simple effects that were stratified by level of the indicator variables (Schabenberger, Gregoire, Weyerhaeuser, & Kong, 2000). Lastly, we graphed both the contemporaneous and lagged interactions between CSS, self-efficacy and PDA at each assessment.
3.0 Results
3.1 Clinical characteristics of the sample
At treatment intake, this sample of young adults reported, on average, approximately 24 percent days abstinent. The majority of the sample met criteria for alcohol (75.7%) or cannabis (72.2%) abuse or dependence. The prevalence of abuse or dependence was less than 50% for any other substance respectively (Table 1). The majority of the sample met criteria for a mood disorder (61.6%), while less than half met criteria for an anxiety disorder (41.7%) or eating disorder (8.6%).
Upon examining the variables of interest at each assessment period, we found the distribution of CSS and self-efficacy to be negatively skewed. Scores on the motivation scale range from the lowest possible value, five, to the highest possible value, thirty. Average motivation scores ranged from 23.96 at 12-months to 25.64 at 3-months post-treatment. The median score for motivation was 28 at 3-months and 27 at the end of treatment, 6-, and 12-months. Scores on the single-item self-efficacy measure ranged from the lowest possible score, one, to the highest possible score, ten. The mean score ranged from 7.38 at 6-months to 8.38 at end of treatment. The median score for self-efficacy was 8 at 6-months and 9 at end of treatment, 3-, and 12-months. Pearson correlations revealed moderate to strong positive bivariate associations between self-efficacy, motivation, and PDA, most of which were significant (p<0.01) (Table 2).
Table 2.
Pearson correlations among high vs. low commitment to sobriety, high vs. low abstinence self-efficacy, and percent days abstinent (negative log transformed) across time
| N(%)/ Mean ± SD | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | (11) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Motivation End of Treatment | 130 (50.2) | -- | 0.36** | 0.41** | 0.35** | 0.32** | 0.13 | 0.19* | 0.30** | 0.18* | 0.25** | 0.21* |
| 2. Motivation 3 Months | 129 (52.7) | -- | 0.49** | 0.39** | 0.11 | 0.30** | 0.22* | 0.22** | 0.38** | 0.26** | 0.23* | |
| 3. Motivation 6 Months | 112 (50.9) | -- | 0.56** | 0.28** | 0.33** | 0.53** | 0.43** | 0.34** | 0.56** | 0.49** | ||
| 4. Motivation 12 Months | 105 (51.7) | -- | 0.31** | 0.27** | 0.42** | 0.59** | 0.37** | 0.45** | 0.57** | |||
| 5. Self-Efficacy End of Treatment | 146 (56.4) | -- | 0.26** | 0.32** | 0.31** | 0.29** | 0.31** | 0.30** | ||||
| 6. Self-Efficacy 3 Months | 128 (52.2) | -- | 0.35** | 0.31** | 0.39** | 0.38** | 0.27** | |||||
| 7. Self-Efficacy 6 Months | 144 (65.8) | -- | 0.48** | 0.38** | 0.71** | 0.59** | ||||||
| 8. Self-Efficacy 12 Months | 107 (52.7) | -- | 0.36** | 0.43** | 0.55** | |||||||
| 9. PDA 3 Months | 3.74 ± 1.33 | -- | 0.58** | 0.45** | ||||||||
| 10. PDA 6 Months | 3.43 ± 1.58 | -- | 0.63** | |||||||||
| 11. PDA 12 Months | 3.02 ± 1.68 | -- |
p<.01
p<.001
3.2 Interaction between motivation and self-efficacy
Preliminary observation of the interaction between motivation and self-efficacy was conducted by calculating average PDA stratified by level of motivation and self-efficacy (high vs. low). Motivation and self-efficacy were dichotomized using a median split. Upon examination, it appears that PDA is greatest when both motivation and self-efficacy are high and conversely, PDA is lowest when both motivation and self-efficacy are low (Table 3). To further investigate the significance of this pattern and possible interaction, we constructed inferential hierarchical linear models of both contemporaneous and lagged design.
Table 3.
Average PDA stratified by motivation for sobriety and self-efficacy
| Contemporaneous |
Lagged |
||||
|---|---|---|---|---|---|
| Motivation for Sobriety | Motivation for Sobriety | ||||
|
| |||||
| 3 Month PDA | Low | High | Low | High | |
|
| |||||
| Self-Efficacy | Low | 82.50 | 96.75 | 88.56 | 93.02 |
| High | 97.63 | 98.00 | 95.71 | 96.04 | |
|
| |||||
| 6 Month PDA | |||||
|
| |||||
| Self-Efficacy | Low | 61.94 | 96.77 | 75.33 | 92.92 |
| High | 95.17 | 98.84 | 96.52 | 93.07 | |
|
| |||||
| 12 Month PDA | |||||
|
| |||||
| Self-Efficacy | Low | 65.16 | 91.05 | 54.93 | 89.72 |
| High | 88.53 | 96.37 | 93.41 | 94.42 | |
Results from the HLM analyses revealed that there was a main effect of both motivation (p<0.001) and self-efficacy (p<0.001) such that having high levels of either construct was associated with higher PDA contemporaneously and prospectively. However, a significant interaction between CSS and self-efficacy (p<0.001) was observed, indicating that the predictive relationship between these two variables is differentially associated with PDA depending on the level of motivation and self-efficacy (Table 4).
Table 4.
Contemporaneous and lagged HLMs assessing the relationship between motivation for sobriety, self-efficacy and percent days abstinent
| Contemporaneous |
Lagged |
|||||||
|---|---|---|---|---|---|---|---|---|
| β | SE | F | p-value | β | SE | F | p-value | |
|
| ||||||||
| Model 1: Main Effects | ||||||||
| Motivation for Sobriety | 0.962 | 0.108 | 79.36 | 0.000 | 0.412 | 0.121 | 11.52 | 0.001 |
| Self-Efficacy | 0.896 | 0.104 | 74.14 | 0.000 | 0.657 | 0.119 | 30.29 | 0.000 |
| Model 2: Interaction | ||||||||
| Motivation for Sobriety | 1.602 | 0.157 | 97.35 | 0.000 | 0.935 | 0.183 | 17.85 | 0.000 |
| Self-Efficacy | 1.431 | 0.139 | 75.02 | 0.000 | 1.087 | 0.160 | 31.66 | 0.000 |
| Motivation for Sobriety x Self- Efficacy Interaction |
−1.093 | 0.200 | 30.00 | 0.000 | −0.840 | 0.231 | 13.21 | 0.000 |
The post-hoc slicing analyses revealed that in the contemporaneous models, the relationship between motivation and PDA remained significant at both high and low levels of self-efficacy (p<0.05). Similarly, self-efficacy maintained a significant association with PDA at high and low levels of motivation independently (p<0.05). Conversely, post-hoc slicing analysis of the lagged models suggest that when motivation for sobriety is high, there is not a main effect of self-efficacy (p=0.150), however when motivation for sobriety is low, there is a significant main effect of self-efficacy such that higher levels of self-efficacy are associated with greater PDA (p<0.05). In accordance with this finding, when self-efficacy is high, there is no significant main effect of commitment to sobriety (p=0.529); however, when self-efficacy is low, commitment to sobriety is a significant predictor of PDA (p<0.05). These findings are supported by the illustrations of the interaction at each assessment point for both the lagged and contemporaneous models (Figure 1).
Figure 1.
Interaction between commitment to sobriety and self-efficacy across assessment periods
4.0 Discussion
The current study investigated the interplay between self-efficacy and motivation for sobriety and how these relate to treatment outcomes in the year following residential SUD treatment using hierarchical linear modeling. In keeping with prior research, findings suggest that each variable alone is an independent statistically significant and moderately strong predictor of substance use, but that there is an important interplay among these variables as they interact significantly, such that the effect of one is dependent on the other. Findings highlight the significance of motivation in understanding how self-efficacy relates to behavioral change.
The nature of the relationships among motivation, self-efficacy, and substance use following treatment, generally followed the pattern we hypothesized. In keeping with predictions, in the contemporaneous model, it was found that for patients high in self-efficacy the level of an individual’s motivation made a statistically significant, but not large, difference to their outcome over time, with lower motivation pulling down PDA despite the high confidence. Conversely, for patients low in self-efficacy, the level of motivation made a much bigger difference than we anticipated, with high motivation making a large positive impact that appeared to completely compensate for their perceived lower confidence. In the lagged model, the latter finding was also true for those low in self-efficacy; for those high in self-efficacy, however, the level of motivation did not make a significant difference to PDA. As illustrated in figure 1 and documented in table 3, the magnitude of these differences are large and clinically meaningful, boosting PDA for those low in self-efficacy but high in motivation at the 6-month time point, for example, from 61.94% up to 96.77%. Overall, the moderating effects of motivation, particularly on low self-efficacy, appear to support the maxim, “Where there’s a will there’s a way”: highly motivated patients may be able to maintain high levels of abstinence, despite the potential handicap conferred by low confidence in their ability to do so. From a theoretical standpoint, although it has been argued that individuals may be unlikely to engage in a course of action unless they believe themselves capable of achieving it (e.g., Bandura, 1997), findings here suggest that despite low confidence in one’s ability to achieve an outcome (e.g., future abstinence from alcohol and other drugs), it may nevertheless still be attempted and achieved, via mobilizing strong intrinsic motivational drives.
The observation that patients low in self-efficacy but high in motivation can still have very good outcomes is intriguing, but how this is achieved is unclear. It may be that there is a certain sub-group of individuals with a strong desire for recovery but whose lack of confidence in their ability to stay sober may actually lead to greater help-seeking in the same way that Alcoholics Anonymous (AA) members’ recognition of their “powerlessness” over alcohol and inability to abstain from it without help (i.e., low abstinence self-efficacy), mobilizes members to obtain an AA sponsor and to become active in the AA program in order to recover (Alcoholics Anonymous, 1953). Extending this logic, it would also follow that patients high in self-efficacy, who appear to maintain high levels of abstinence, may not need this type of ongoing outside support as much. Future research should examine this.
4.1. Limitations
Generalizations from the current study should be made with caution in light of certain limitations. The sample is derived from a single private residential facility treating young adults and, despite being similar in certain characteristics to other programs in the United States, may differ across other important variables that were not measured or available for comparison. The sample was also predominantly Caucasian and male. Consequently, generalizations to other age groups, outpatients, and minorities, need to be made cautiously and clarified in future research. Also, biological assays were only collected on subsample of patients (15%) and it may be that self-reported estimates of abstinence are to some degree inaccurate. The follow up rates, although quite high early post discharge from treatment, diminished to just above 71% at the 12-month follow-up. Confidence in the findings is bolstered, however, by the consistency in the pattern of relationships among variables across time, but future replications are needed to determine the robustness of our findings.
4.2. Conclusions
Self-efficacy is a psychological construct of central importance in understanding human behavior that is well supported empirically. Its merit in theories of relapse is supported here as a significant and moderately strong predictor of treatment outcome. In addition, the significance of its predictive ability may be moderated by an individual’s motivation to enact the behavior. Findings herein, highlight important conceptual nuances in self-efficacy theory; and, clinically, convey optimism that, even if a patient reports low confidence in their ability to remain abstinent, it does not necessarily follow that they will have poor outcome, especially if they have a strong desire to remain abstinent.
Acknowledgements
This work was funded by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) grant number R21AA01815-01A2 and by an anonymous donation for youth research to the Hazelden Foundation. Dr. Kelly’s participation is supported by NIAAA grant 1R21AA01815-01A2.
Footnotes
A small number of participants (n=5) reported more than one drug of choice, such that these proportions do not sum to 100%.
Conficts: None for either author.
References
- Ajzen I, Madden TJ. Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology. 1986;22:453–474. [Google Scholar]
- Alcoholics Anonymous . Twelve steps and twelve traditions. Alcoholics Anonymous World Services; New York: 1953. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Bandura A. Self-efficacy: The exercise of self-control. Freeman and Company, NY; New York: 1997. [Google Scholar]
- Cone EJ, Presley L, Lehrer M, Seiter W, Smith M, Kardos KW, Niedbala RS. Oral fluid testing for drugs of abuse: positive prevalence rates by Intercept immunoassay screening and GC-MS-MS confirmation and suggested cutoff concentrations. J Anal Toxicol. 2002;26(8):541–546. doi: 10.1093/jat/26.8.541. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RPG, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. Journal of Studies on Alcohol. 1994;55(2):141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- Forcehimes A, Tonigan J. Self-efficacy as a factor in abstinence from alcohol/other drug abuse: A meta-analysis. Alcoholism Treatment Quarterly. 2008;26(4):480–489. [Google Scholar]
- Hoeppner BB, Kelly JF, Urbanoski KA, Slaymaker V. Comparative utility of a single-item versus multiple-item measure of self-efficacy in predicting relapse among young adults. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] J Subst Abuse Treat. 2011;41(3):305–312. doi: 10.1016/j.jsat.2011.04.005. doi: 10.1016/j.jsat.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden RM, Litt MD. The role of self-efficacy in the treatment of substance use disorders. [Research Support, N.I.H., Extramural Review] Addict Behav. 2011;36(12):1120–1126. doi: 10.1016/j.addbeh.2011.07.032. doi: 10.1016/j.addbeh.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Greene MC. Beyond motivation: Initial validation of the Commitment to Sobriety Scale. J Subst Abuse Treat. doi: 10.1016/j.jsat.2013.06.010. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addiction Research & Theory. 2009;17(3):236–259. [Google Scholar]
- Marlatt GA, Gordon JR, editors. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol Suppl. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. [Research Support, U.S. Gov’t, P.H.S.] J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17(6):1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): Rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcoholism: Clinical Experimental Research. 1993;17(6):1130–1145. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Randall CL, Del Boca FK, Mattson ME, Rychtarik R, Cooney NL, Donovan DM, Wirtz PW. Primary treatment outcomes and matching effects: Aftercare arm. In: Babor TF, Del Boca FK, editors. Treatment matching in alcoholism. Cambridge University Press; New York, NY US: 2003. pp. 135–149. [Google Scholar]
- Roman PM, Johnson JA. National Treatment Center Study Summary Report: Private treatment centers. Institute for Behavioral Research, University of Georgia; Athens, GA: 2004. [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Schabenberger O, Gregoire TG, Weyerhaeuser JP, Kong F. Collections of simple effects and their relationship to main effects and interactions in factorials. The American Statistician. 2000;54(3):210–214. [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of Alcohol and Other Drug Use by Runaway Youths: A Test-Retest Study of the Form 90. Alcohol Treat Q. 2004;22(2):21–34. doi: 10.1300/J020v22n02_03. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . National Admissions to Substance Abuse Treatment Services. Rockville, MD: [Accessed 14 December 2010]. 2009. Treatment Episode Data Set (TEDS). Highlights 2007. DASIS Series: S-45, DHHS Publication No (SMA) 09-4360 [ http://oas.samhsa.gov/TEDS2k7highlights/toc.cfm] [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: an instrument for assessing alcohol treatment outcome. J Stud Alcohol. 1997;58(4):358–364. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: that was Zen, this is Tao. Am Psychol. 2004;59(4):224–235. doi: 10.1037/0003-066X.59.4.224. doi: 10.1037/0003-066X.59.4.224 2004-14303-002 [pii] [DOI] [PubMed] [Google Scholar]