Summary
Poor adherence to continuous positive airway pressure (CPAP) treatment is associated with substantial health care costs, morbidity and mortality, and has been a leading obstacle in the effective management of obstructive sleep apnea (OSA). Successful interventions to improve CPAP adherence may ultimately include a variety of components. For patients living with spouses (refers to all domestic partners), the spouse will likely be an integral component to any successful intervention. Developing understanding of the role of spouses in adherence to CPAP has been identified to be a critical research need. This review expands the investigation of CPAP adherence to a broader context, from an exclusive focus on individual patients to a dyadic perspective encompassing both patients and their spouses. A conceptual framework based on social support and social control theories is proposed to understand spousal involvement in CPAP adherence. Methodologies for future investigations are discussed, along with implications for developing interventions that engage both patients and their spouses to improve CPAP use.
Keywords: obstructive sleep apnea, continuous positive airway pressure, treatment adherence, spousal involvement, lung
Introduction
Obstructive sleep apnea (OSA) is a serious condition for which there is a highly efficacious treatment (continuous positive airway pressure [CPAP]).1–3 However, treatment success depends on CPAP adherence, which is highly variable.1, 4, 5 Successful interventions to improve CPAP adherence may ultimately include a variety of components. For patients living with “spouses” (refers to all domestic partners in this review), the spouse will likely be an integral component to any successful intervention. Because of the dyadic (pairing two individuals) nature of sleep for many adults,6 the impact of OSA and its treatment extends beyond merely the context of the individual patient. Although engaging the patient’s spouse has been suggested to improve CPAP adherence, little work has been conducted to date.7 The purpose of this review is to more fully understand CPAP adherence by broadening the focus, to consider not only individual patients but a dyadic perspective of both patients and their spouses.
A. Poor adherence to CPAP remains the major impediment to effective treatment for OSA
The current prevalence estimates of moderate to severe OSA (apnea-hypopnea index ≥15 events per hour of sleep) are 10–17% among middle-aged men and 3–9% among middle-aged women.8 These rates substantially increased over the last two decades due to the increasing prevalence of some of the major risk factors for OSA (e.g., obesity and aging).8 Untreated OSA adds at least $3.4 billion to annual medical costs in the U.S.9 and has negative health consequences, such as excessive daytime sleepiness,10 mood disturbances,11 impaired cognition and performance,12 diminished quality of life,13 and increased all-cause mortality.14 The role of OSA as an independent risk factor for hypertension,15 cardiovascular diseases,16 ischemic stroke,17 and insulin resistance18 has been reported and has become one of the most vibrant areas of inquiry. Its high prevalence and negative consequences have led OSA to be viewed as a serious public health threat, on par with cigarette smoking according to some in the health care community.19 Effective treatment for OSA can be achieved through the use of CPAP, which is the primary and most effective treatment option for OSA.1–3 The benefits of CPAP have been well documented, including significant improvement in daytime sleepiness, mood disturbance, functional status, and neuropsychological performance.2, 20, 21 Recent studies also demonstrate that CPAP significantly decreases blood pressure22 and possibly mortality rate, primarily due to a reduction in cardiovascular disease.23
Despite its efficacy, patients’ use of CPAP is often less than optimal. To be effective therapeutically, CPAP should be consistently applied throughout sleep every night; however, less than 50% of the patients actually follow this prescription.5, 24 In a cohort of 149 consecutive patients who were referred to the sleep laboratory and prescribed CPAP therapy, 18% of them rejected CPAP immediately after CPAP titration, and 16% dropped out after 2 weeks of therapy.25 When defining adequate nightly use as at least 4 hours per night, 29–83% of patients could be classified as nonadherent.1, 4 Even when patients do not completely abandon CPAP, their adherence to recommended nightly use may be poor. Although the optimal “dose” is not consistently defined, it is agreed that greater CPAP use optimizes clinical benefits. Weaver and colleagues26 examined CPAP dose response and identified the optimal duration of nightly use to be at least 4 hours to normalize subjective sleepiness, 6 hours to normalize objective sleepiness, and 7 hours to normalize functional status. Failure to use CPAP, even for one night, permits the return of sleep-disordered breathing and associated excessive daytime sleepiness,24 impaired neurobehavioral functioning,27 increased sympathetic activity,28 and marked driving impairment.29 With increasingly robust evidence for the benefits of CPAP and a scarcity of effective treatment alternatives, poor adherence to CPAP remains a major obstacle in the management of OSA.30
B. The need for a dyadic perspective to examine CPAP adherence
B. 1. Dyadic nature of sleep
According to the 2005 National Sleep Foundation poll, 61% of adults sleep with a partner, and one-quarter to one-third of married or cohabitating couples report that their intimate relationships are adversely affected by their own or their spouse’s excessive sleepiness or sleep problems.6 Because the majority of adults sleep with a spouse or partner, conceptualizing sleep and sleep disorders from a dyadic perspective is likely to benefit both the patient and the spouse. Despite changes in objective sleep, couples generally reported greater sleep quality when sleeping together as compared with sleeping apart.31 This benefit of co-sleeping on subjective sleep quality suggests a psychological need for closeness and security, and is likely to be moderated by the couple’s relationship quality.31 Sleep is not only a biological need but a necessity embedded in a social context for humans. Shifting from the traditional view of sleep as an individual phenomenon, examining sleep in the social context has revealed sleep to be a novel pathway linking close relationships and health.31, 32 In the heuristic framework proposed by Troxel,31 sleep and relationship functioning are reciprocally related via shared behavioral, chronobiological, psychological, and neurobiological mechanisms. This mutual interaction of sleep and relationship functioning, in turn, is hypothesized to have its effect on physiological pathways that are directly related to physical and mental health.31 This conceptual model has laid the foundation for future investigation of the dyadic nature of sleep and its implications for health.
B. 2. Collateral burden of OSA to spouses
The impact of OSA extends beyond the individual patient.33, 34 Patients with OSA are likely to view their disorder as a burden for their spouses, and often report sleeping apart from them.35 Spouses frequently report disturbed sleep, which can be related to patients’ snoring, gasping, and sleep interruptions, as well as their own concerns with patients’ breathing abnormalities. Referral to a sleep clinic to rule out suspected OSA is typically triggered by a complaint from the partner.36 There is an association between a supportive partner and a patient’s recognition that OSA is a dangerous syndrome.37 In a study of 36 snoring men, half of the bed partners complained of disturbed sleep almost every night and 40% of them had to leave the bedroom weekly.38 Even if the patient sleeps out of the bedroom for one night, no relief is obtained in the sleep of the partner, suggesting that previous night exposure still impairs sleep.39 Women living with snorers are three times as likely to report symptoms of insomnia compared to women living with non-snorers, suggesting that a sleep disorder in one spouse may increase risk for a sleep disorder in the other.39 Adverse associations between OSA and marital satisfaction have been clearly demonstrated.38, 40, 41 A study also reported that wives of OSA patients exhibited an increase in musculoskeletal pain, distress, and impaired sleep in comparison to controls, independent of age and menopausal status.42
B. 3. Positive effects of CPAP for both patients and their spouses
Following CPAP treatment, decreased subjective sleepiness; improved social, emotional, and relationship functioning; and improved quality of life have been demonstrated in both patients with OSA and their spouses.34, 43, 44 Objective improvement in spousal sleep quality has been demonstrated after patients have began using CPAP.45 Baron and colleagues46 also reported a decrease in marital conflict between patients with OSA and their spouses after the first 3 months of CPAP use. In previous reports, we observed that both male and female patients demonstrated improved intimacy and sexual relationships following 3 months of CPAP therapy.47, 48 Such improvements in marital harmony are also likely to have benefits for children and other co-habitants. It has been demonstrated that long-term CPAP treatment can improve sexual function for example by reducing erectile dysfunction in men with OSA.49 However, it is rare for these positive health benefits of using CPAP, such as improved marital relationships and reduced erectile dysfunction, to be discussed or explored in sleep clinics.
B. 4. Previous investigations in CPAP use indicate the need for a dyadic perspective
Although collateral damage of OSA to the spouse and the benefit of CPAP treatment for both the patient and the spouse have been well documented, the dyadic nature of CPAP treatment has not been emphasized. Previous investigations of CPAP adherence have primarily focused on individual patients, which may have missed important and modifiable environmental factors such as spousal interaction. Few reliable determinants have been consistently identified to influence CPAP use. There is some evidence to support the role of OSA severity,50 demographic characteristics (e.g., race,51, 52 social economic status,51, 53 gender,54, 55 age,56), psychological factors particularly self-efficacy,57–60 daytime sleepiness,50 improvement in functional status,61 and CPAP side effects such as claustrophobia.62 Sawyer and colleagues63 conducted a thorough review of CPAP adherence across age groups and summarized the factors that influence CPAP adherence as falling into four categories: disease and patient characteristics; treatment titration procedures; technological device factors and side effects; and psychological and social factors.
Overall, there is a paucity of tested effective interventions to improve adherence to CPAP. To date, only a few randomized controlled studies have reported positive findings.63–68 For example, Hoy and colleagues64 examined the effect of intensive support to improve CPAP use. Their intervention—which included intensive CPAP setup with home education, 3 nights of CPAP titration, and home visits by nurses at 7, 14, 28, and 120 days—improved daily CPAP use by 1.5 hours compared to standard clinical care.64 In contrast, another study using intensive supportive care did not demonstrate improvement in CPAP use.65 The inconsistent findings have called into question the beneficial effect of this intervention. The applicability of intensive support care to clinical practice is limited, as it is labor-intensive, costly, and time-intensive. The positive effects may be difficult to sustain when intensive support stops. Motivational enhancement therapy66–68 and cognitive behavioral therapy69 are promising interventions based on either self-management of disease or motivational enhancement, and have been reported to improve CPAP adherence. Self-efficacy and social support are important elements in these successful interventions.69 Spousal influence has been identified as one major factor in patient self-efficacy of CPAP use,70 and a spouse remains the primary and foremost resource of social support.71 Thus, the investigation of the dyad of patient and spouse is essential; interventions engaging spouses of CPAP users have a strong potential to improve adherence to CPAP therapy.
The latest Cochrane Review by Wozniak and colleagues assessed the effectiveness of strategies that are educational, supportive or behavioral to improve the usage of CPAP in adults with OSA.72 Low- to moderate-quality evidence showed that all three types of interventions had a positive impact on increasing average CPAP use over a limited time. Among the thirty studies included in this review,72 only two studies64, 69 intended to include spouses of OSA patients, although neither considered spouses as their study participants. Future studies involving spouses should be helpful in understanding the role they may play in improving the long-term use of CPAP, and whether the engagement of spouses can strengthen the effectiveness of those educational, supportive or behavioral interventions.
C. What do we know about spousal involvement in CPAP adherence?
In a recent prospective study examining pre-treatment and immediate early treatment factors predicting CPAP use during the first week of therapy, difficulty being intimate with partners was the only side effect of CPAP treatment significantly correlated with CPAP adherence.52 Having difficulty being intimate, along with African American race and higher residual apnea-hypopnea index, were identified as independent predictors of reduced CPAP use during the first week.52 These results suggest the need to assess the aspects of CPAP treatment that interfere with sexual relations. However, patients’ concerns about the impact of CPAP on their intimate relationships cannot be addressed without an understanding of their partners’ perspective.
Although inclusion of spouse or bed partner has been recommended as one strategy to promote CPAP adherence,63 there has been surprisingly little investigation of the impact of spousal involvement on CPAP adherence. Spouses have seldom been a formal part of scientific inquiry in CPAP adherence literature. Results from recent studies examining co-sleeping,73, 74 relationship quality,46 and facilitators of and barriers to CPAP use75 have suggested the important role spouses play in CPAP adherence. For example, one study reported that during the first week of treatment, patients living alone used CPAP an average of 3.2 hours per night, whereas patients who lived with a partner used CPAP for 4.5 hours.73 In a small study examining male patients with OSA and their wives, CPAP use in the first 2 weeks was positively related to the number of nights the couple slept together.74 These findings suggest that CPAP adherence may not be due solely to the patient’s effort to utilize this therapy. In a study assessing patient self-efficacy in sleep apnea, half of the participants stated that they would not use CPAP if it disturbed their spouse’s sleep.70 This concern was rated as one of the greatest deterrents to CPAP use, exceeding other commonly perceived barriers such as nasal stuffiness and feelings of claustrophobia.70 In fact, patients have described a sense of engagement on the part of the spouse as an important facilitator, while they cite insufficient spousal support as a major barrier to their using CPAP.75 However, none of the above studies has directly examined the role of spousal involvement in CPAP adherence.
Social support, including spousal support, has been positively associated with patient adherence to medical treatment.76 The nature of spousal involvement may be complicated and cannot be simply represented by marital status or living arrangement. For example, patients who reported seeking treatment at their spouses’ urging, rather than on their own initiative, demonstrated lower CPAP adherence over the first 3 months of therapy.64 Thus, while spouses can provide a strong incentive to maintain treatment, spouses can also negatively influence patient’s CPAP use, as spousal initiation of evaluation may be a marker of reduced patient motivation.64, 77 This concept is supported by the work conducted by Barron and colleagues,77, 78 who first directly examined diverse types of spouse involvement in CPAP adherence. They found that in male OSA patients, the pressure from the wife to use CPAP predicted poorer adherence at 3 months,77 while perceptions of collaborative spousal involvement were associated with a greater use of CPAP.78 This bidirectional relationship between spousal involvement and patients’ adherence to CPAP needs to be examined further.
D. Recommendations for future investigations of spousal involvement in CPAP adherence
D. 1. Conceptual framework
Based on social support and social control theories, and a review of pertinent literature, we have proposed a conceptual framework to guide future investigations of spousal involvement in CPAP adherence (Figure 1). Two basic aspects of spousal involvement have been investigated in the literature: positive (positive reinforcement and cooperative approach) and negative (nagging, threatening, and criticizing the spouse).79, 80 We hypothesize that a spouse’s more frequent use of positive approaches may be associated with the patient’s greater engagement in the desired behavior; whereas a spouse’s negative interactions may be associated with the patient’s greater tendency to ignore the spouse’s demands, do the opposite, or hide unhealthy behaviors.79, 80 Both positive (support and collaboration) and negative (pressure, coercion) spousal influence on patient’s adherence to CPAP therapy should be evaluated, with the goal to define modifiable factors which can be used for intervention to promote CPAP use.
Figure 1. Spousal Involvement and CPAP Adherence.
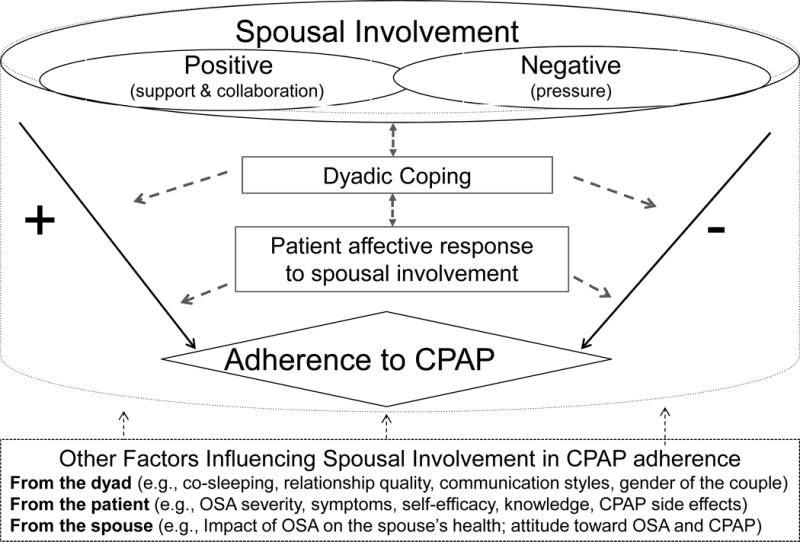
OSA – obstructive sleep apnea; CPAP – continuous positive airway pressure
Two factors that are important in the dyad, dyadic coping and affective response, are hypothesized to influence the impact of spousal involvement on CPAP adherence. A widely accepted definition of dyadic coping is an interpersonal process in which a stressful event affects both partners either directly or indirectly and triggers the coping efforts of both partners.81 The stress may be experienced primarily by one partner (e.g. workplace stress or an illness) but affects both partners when one’s stress is communicated to the other. Some couples communicate clearly about their stress and can mobilize positive and supportive coping strategies for managing the stress. Yet other couples may not be able to respond to each other’s stress, and choose to avoid or cope with the stress independently. Therefore, dyadic coping is a concept that describes various ways that couples interact (e.g., avoid, support, communicate, collaborate, overprotect), as they deal with stressors. Studies have examined the phenomenon of dyadic coping as it relates to patients receiving treatment for other illnesses such as cancer, arthritis, myocardial infarction, and depression.82 Adherence to treatment is not the major focus of these studies but managing physical symptoms, emotional distress, and practical concerns related to the illness are often the sources of stress. In the case of OSA, the accumulating effects of stresses from the disease (e.g., non-restorative sleep, insomnia, marital dissatisfaction) on the couple’s relationship, and inadequate management of the stress, may persist as the patient begins using CPAP. A growing body of research suggests that adjustment to an illness is enhanced when patients and spouses view challenges as “our” problem and are mutually responsive to each other’s stress.82, 83 Similarly, we believe that a patient’s adherence to CPAP may be enhanced when both patient and spouse approach the disease and/or treatment regimen as a stressor that affects both of them. Dyadic coping has been emphasized in couple-based interventions,83, 84 and may also be an important target for interventions to promote CPAP use. Affective response has been emphasized in social control literature when examining spouses’ strategies in attempting to modify each other’s health behaviors.80 Patients may have a positive or a negative affective response to spousal involvement; this various affective response can, in turn, influence the patient’s health behavior.80 A similar moderating effect of affective response may exist, influencing the impact of spousal involvement in CPAP use, and may need to be examined to facilitate our understanding of how spousal involvement may have an impact on patients’ CPAP use. Although dyadic coping and affective response can have significant impacts on health outcomes and health behavior, they have not been examined in the context of CPAP therapy. Future studies using validated tools for these variables, such as Dyadic Coping Inventory85 and Positive and Negative Affect Scale,86 can help to test our hypotheses and to discover the “ideal” dyadic coping or interaction styles that will promote CPAP adherence.
Other potentially important variables need to be considered when examining spousal involvement in CPAP adherence. Examples of these factors include co-sleeping, relationship quality, marital satisfaction, communication styles, and psychological factors such as self-efficacy and knowledge. The impact of OSA on the spouse’s health, and the spouse’s attitude toward CPAP therapy, also need to be examined in order to understand spousal involvement in CPAP adherence.
This conceptual framework primarily emphasizes the positive and negative aspects of spousal involvement on CPAP adherence, and explores how dyadic coping and affective response may influence the impact of spousal involvement on CPAP adherence. Our goal is to highlight some modifiable aspects in the dyad, which can direct future investigation and lay a foundation for couple-based interventions to improve CPAP use. Reciprocal relationships need to be considered in the dyad. For example, although spousal involvement is hypothesized to be a predictor of adherence to CPAP in patients, day-to-day CPAP use can, in turn, change how spouses are involved in the treatment. In addition, different dyadic coping styles may be related to positive or negative affective response to spousal involvement. Dyadic coping can also change patient’s self-efficacy of CPAP use, which may directly influence the adherence behavior. These potential pathways need to be explored in future studies.
Gender may play a role in spousal involvement of CPAP use. The data regarding how men and women with OSA approach CPAP treatment are sparse. A few studies have reported gender differences in CPAP adherence, but the results are conflicting.54, 55 As demonstrated by the findings from the Swedish Obese Subjects Study, OSA had a greater impact on divorce rate in women than in men.87 It is possible that female partners of men with OSA are more tolerant of loud snoring or daytime sleepiness than vice versa.87 This difference may influence how male and female partners perceive the impact of OSA on their lives and how they would engage in their partners’ CPAP treatment. In addition, gender-specific concerns may exist during treatment, which may directly influence the adherence behavior. As demonstrated in a study examining adherence to antiretroviral therapy in a group of Italian patients, non-adherent women worried excessively about negative feedback from others, while non-adherent males seemed focused less on relational aspects.88 Another largely unknown area is whether the same-sex dyad makes a difference in adherence compared to the opposite-sex dyad. Future studies should investigate this issue by including both heterosexual and same-sex couples.
D. 2. Methodological considerations
In reviewing interventional studies to improve CPAP adherence, we found two studies that intended to involve spouses or partners.64, 69 Hoy et al.64 tested the effect of an intensive education and support program on CPAP adherence, in which spouses were invited to participate in the initial CPAP education and follow-up home visits. Richards and colleagues69 also mentioned their inclusion of participants’ partners in their cognitive behavioral therapy. However, both studies did not recruit spouses as study participants. Neither of the studies specified how many patients had a partner, nor how many partners actually participated in the intensive support or cognitive behavior therapy. It is unknown whether the involvement of spouses or partners indeed contributed to the positive findings. It has been recognized that simple recommendations to involve a spouse may not be sufficient in behavior-modification efforts.80 Due to both the positive and negative impact spouses can have on CPAP adherence, this approach of merely adding spouses to a study may not be adequate.
In the two studies conducted by Baron and colleagues77, 78 which directly examined spousal involvement in CPAP adherence, the researchers relied on the report from OSA patients for all assessments, and the dyadic nature of spousal involvement could not be fully evaluated. Spousal involvement should be more accurately measured by independent evaluation from both partners, as spouses’ supportive interactions sometimes go unrecognized by recipients.89, 90 The exclusive enrollment of male participants may limit the generalizability of the finding. Instead, we recommend recruiting both male and female patients and their partners in future investigations of spousal involvement and CPAP adherence.
Qualitative inquiry can contribute to the understanding of the exact nature of the couple’s experiences with CPAP, how they manage treatment, and the nature of supportive and unsupportive behaviors. In-depth interviews may inform the state of the science related to CPAP adherence by identifying perceived facilitators of and challenges to CPAP use, and the consequences of CPAP treatment for both partners from their own perspective. Based on previous findings of benefit of CPAP for spouses, researchers may hold the assumption that spouses will embrace this therapy. However, spouses could have a negative reaction to the therapy due to its cumbersome nature, which could, in turn, impede patients’ use of this therapy. A qualitative approach may help to eliminate a researcher’s potential bias when investigating spousal involvement in CPAP adherence. A recent study conducted in Sweden used a qualitative descriptive design to explore decisive situations affecting partners’ support for patients with OSA and how the partners manage these situations during the initial phase of CPAP therapy.91 A great variety of situations were identified that could have negative or positive influences on the partners’ support for patients.91 One limitation of this study is that only partners of patients with CPAP-treated OSA were interviewed, thus the bidirectional relationship between patient and partner may have been missed. Joint interviews with one couple at each time may disclose more informative findings due to the potential interaction between the partners. It should be noted that some influence or constraint may be exerted by the spousal partner’s presence, and the answers provided can be influenced by the couple’s relationship and their decision-making style. In this case, a follow-up interview for individual spouses may be appropriate after the joint interview.
E. Implications for interventions to improve CPAP adherence
A large body of literature demonstrates that spouses can make a significant difference in their partners’ health behaviors, including adherence behaviors.76, 80, 92, 93 Using a dyadic design including both diabetic patients and spouses, a study found that patients’ dietary adherence was best served when the spouse used more positively toned and less coercive influence.93 It has been shown that spousal involvement in CPAP treatment is not always helpful. 79, 80 It is critical to understand the characteristics, role and impact of spousal involvement in CPAP adherence before any successful interventions involving spouses can be developed to improve CPAP use.
Family-oriented and couple-based interventions have demonstrated effectiveness in weight control,94 drug addiction,95 and medication-taking behavior,96 and they have improved health outcomes in diseases such as diabetes mellitus,97 cancer,83 and chronic mental illness.98 Understanding the similarities and differences between how couples respond to OSA and CPAP versus other disorders and treatment may be useful in designing dyadic interventions for this population. It should be noted that spousal partners might change over the course of a lifetime, and expecting one partner to offer continuous support and assistance to the other may not be realistic. Instead of expecting the spouse to play a long-term care-giving role, a dyadic perspective should focus on how the couples cope together with OSA and CPAP therapy. A successful coping intervention has been developed by Kayser and colleagues83 for women with breast cancer and their partners: the Partners in Coping Program. Dyadic coping can be a potential appealing target for couple-based intervention to improve CPAP use.
Due to the multidimensional nature of CPAP adherence, one type of intervention is unlikely to meet the need of all patients. For patients living with spouses, spouses should be integrated into any educational, supportive, or behavioral strategies to improve CPAP adherence. Clinicians need to assess the burden of OSA to the spouses early in the process of disease diagnosis, and educate both patients and their spouses as to the positive health benefits of using CPAP, including increased sexual function and improved marital relations. Future investigations should empirically evaluate the methods of involving spouses to improve CPAP adherence.
A study found that involving a spouse enhanced the efficacy of cognitive behavioral therapy with victims of sexual assault suffering from posttraumatic stress disorder.99 In a recent review of interpersonal factors in insomnia, Rogojanski and colleagues100 presented a model for integrating bed partners into cognitive behavioral therapy to further enhance its efficacy. This model offers great insight into how to integrate spouses into behavioral interventions such as cognitive behavioral therapy69 and motivational enhancement therapy66, 67 to improve their effectiveness at increasing CPAP adherence.
It has been suggested that including partners as active participants in interventions may improve adherence and cost-effectiveness of medical treatments.32 Given the frequency and intensity of interaction that a patient has with the spouse, the interventions engaging the spouse may be more cost-effective and sustainable than other methods to promote CPAP adherence such as intensive support for patients alone by health professionals. This cost-saving potential of engaging spouses to promote CPAP adherence needs to be evaluated. Cost-effectiveness research would help to establish how resources can be allocated in implementing these interventions. Another important area of investigation is whether incorporating spouses can improve CPAP treatment outcomes for this already efficacious therapy, particularly whether it can have a positive impact on long-term outcomes such as relationship functioning and quality of life. In addition, engaging spouses may be a promising strategy for patients who have not successfully persisted with CPAP therapy.
Despite the potential benefit of incorporating spouses into CPAP treatment to improve adherence and treatment outcomes, the question of how best to engage the spouse in CPAP treatment remains unanswered. Future research should aim to evaluate the role of spousal involvement in CPAP treatment adherence by conducting prospective investigations including both patients and their spouses. Ideal types and level of spousal involvement and factors that may influence the impact of spousal involvement on CPAP use need to be determined. Meanwhile, clinicians should have a more open discussion of the negative health impact of OSA to spouses and of the benefits of CPAP treatment for both patients and spouses. We hope this review can expand the scope of current investigation of CPAP adherence to a broader context that includes both patients and their spouses, and we further hope it encourages more research to address the essential clinical need of improving CPAP adherence with a dyadic perspective.
Practice Points.
Poor adherence to CPAP treatment remains a major obstacle to the effective management of OSA. Previous investigations of CPAP adherence, primarily focused on the diagnosed individual, have reflected limited success.
Because of the dyadic nature of sleep for the majority of adults, the impact of OSA and its treatment extends far beyond the context of the individual patient. OSA can be experienced as a stressor for both patients and their spouses, and positive effects of CPAP have been observed in both partners.
Spouses can make a significant difference in their partners’ health behaviors including adherence behaviors.
Interventions engaging spouses have the potential to be effective and sustainable strategies to promote CPAP adherence in patients with OSA.
Clinicians should have a more open discussion of the negative health impact of OSA to spouses and the benefits of CPAP treatment for both patients and spouses.
Research Agenda.
The investigation of CPAP adherence needs to be expanded from an exclusive focus on individual patients to a dyadic perspective involving both patients and their spouses.
It is critical for future research to develop an understanding of the nature of spousal involvement in CPAP adherence, with the goal of informing interventions to promote CPAP use.
Future prospective or longitudinal investigations should recruit both male and female patients and their spouses (heterosexual or same-sex couples) to investigate the role of spousal involvement in adherence to CPAP treatment.
Both positive and negative influence of the spouse on a patient’s adherence to CPAP should be evaluated.
Two factors that are important in the dyad and may influence the impact of spousal involvement on CPAP adherence need be investigated: dyadic coping (the ways that couples interact as they deal with stressors), and patient affective response to spousal involvement.
Qualitative inquiry should be considered to develop an in-depth understanding of the couple’s experiences with CPAP, how they manage treatment, and the nature of supportive and unsupportive behaviors.
Future research should evaluate whether incorporating spouses into educational, supportive, or behavioral strategies to improve CPAP adherence can enhance the efficacy of these interventions, and its effect on long-term treatment outcomes.
Acknowledgments
This work was supported by a grant from National Institutes of Health, National Institute of Nursing Research R15NR013274 (Ye, L).
List of Abbreviations
- OSA
obstructive sleep apnea
- CPAP
continuous positive airway pressure
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement: Dr. Weaver has received research grant support from TEVA, Inc., research equipment from Philips Respironics, Inc., royalty fees for use of the Functional Outcomes of Sleep Questionnaire from Nova Som, GlaxoSmithKline, Philips Respironics, TEVA, Inc., and Nova Nordsk, and has served on Board of Directors of ViMedicus, Inc. Dr. Aloia is a paid employee and stock holder for Philips Healthcare. The other authors have no pertinent personal financial interests.
References
- 1.Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29:381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 2.Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev. 2006;3:CD001106. doi: 10.1002/14651858.CD001106.pub3. [DOI] [PubMed] [Google Scholar]
- 3.McDaid C, Duree KH, Griffin SC, Weatherly HL, Stradling JR, Davies RJ, et al. A systematic review of continuous positive airway pressure for obstructive sleep apnoea-hypopnoea syndrome. Sleep Med Rev. 2009;13:427–36. doi: 10.1016/j.smrv.2009.02.004. [DOI] [PubMed] [Google Scholar]
- *4.Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008;5:173–8. doi: 10.1513/pats.200708-119MG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weaver TE, Kribbs NB, Pack AI, Kline LR, Chugh DK, Maislin G, et al. Night-to-night variability in CPAP use over the first three months of treatment. Sleep. 1997;20:278–83. doi: 10.1093/sleep/20.4.278. [DOI] [PubMed] [Google Scholar]
- 6.Summary of Fundings of the 2005 Sleep in America Poll. Washington: National Sleep Foundation; 2005. pp. 27–31. [Google Scholar]
- *7.Aloia MS. Understanding the problem of poor CPAP adherence. Sleep Med Rev. 2011;15:341–2. doi: 10.1016/j.smrv.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased Prevalence of Sleep-Disordered Breathing in Adults. Am J Epidemiol. 2013 doi: 10.1093/aje/kws342. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kapur V, Blough DK, Sandblom RE, Hert R, de Maine JB, Sullivan SD, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22:749–55. doi: 10.1093/sleep/22.6.749. [DOI] [PubMed] [Google Scholar]
- 10.Black J. Sleepiness and residual sleepiness in adults with obstructive sleep apnea. Respir Physiol Neurobiol. 2003;136:211–20. doi: 10.1016/s1569-9048(03)00083-1. [DOI] [PubMed] [Google Scholar]
- 11.Ohayon MM. The effects of breathing-related sleep disorders on mood disturbances in the general population. J Clin Psychiatry. 2003;64:1195–200. doi: 10.4088/jcp.v64n1009. quiz, 274–6. [DOI] [PubMed] [Google Scholar]
- 12.Weaver TE, George CFP. Cognition and performance in patients with obstructive sleep apnea. In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. 4. Philadelphia: Elsevier Saunders; 2005. [Google Scholar]
- 13.Baldwin CM, Griffith KA, Nieto FJ, O’Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep. 2001;24:96–105. doi: 10.1093/sleep/24.1.96. [DOI] [PubMed] [Google Scholar]
- 14.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–85. [PMC free article] [PubMed] [Google Scholar]
- 15.O’Connor GT, Caffo B, Newman AB, Quan SF, Rapoport DM, Redline S, et al. Prospective study of sleep-disordered breathing and hypertension: the Sleep Heart Health Study. Am J Respir Crit Care Med. 2009;179:1159–64. doi: 10.1164/rccm.200712-1809OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 17.Redline S, Yenokyan G, Gottlieb DJ, Shahar E, O’Connor GT, Resnick HE, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010;182:269–77. doi: 10.1164/rccm.200911-1746OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ip MS, Lam B, Ng MM, Lam WK, Tsang KW, Lam KS. Obstructive sleep apnea is independently associated with insulin resistance. Am J Respir Crit Care Med. 2002;165:670–6. doi: 10.1164/ajrccm.165.5.2103001. [DOI] [PubMed] [Google Scholar]
- 19.Phillipson EA. Sleep apnea–a major public health problem. N Engl J Med. 1993;328:1271–3. doi: 10.1056/NEJM199304293281712. [DOI] [PubMed] [Google Scholar]
- 20.Ballester E, Badia JR, Hernandez L, Carrasco E, de Pablo J, Fornas C, et al. Evidence of the effectiveness of continuous positive airway pressure in the treatment of sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159:495–501. doi: 10.1164/ajrccm.159.2.9804061. [DOI] [PubMed] [Google Scholar]
- 21.Engleman HM, Cheshire KE, Deary IJ, Douglas NJ. Daytime sleepiness, cognitive performance and mood after continuous positive airway pressure for the sleep apnoea/hypopnoea syndrome. Thorax. 1993;48:911–4. doi: 10.1136/thx.48.9.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med. 2012;8:587–96. doi: 10.5664/jcsm.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campos-Rodriguez F, Pena-Grinan N, Reyes-Nunez N, De la Cruz-Moron I, Perez-Ronchel J, De la Vega-Gallardo F, et al. Mortality in obstructive sleep apnea-hypopnea patients treated with positive airway pressure. Chest. 2005;128:624–33. doi: 10.1378/chest.128.2.624. [DOI] [PubMed] [Google Scholar]
- 24.Kribbs NB, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry JN, et al. Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. Am Rev Respir Dis. 1993;147:1162–8. doi: 10.1164/ajrccm/147.5.1162. [DOI] [PubMed] [Google Scholar]
- 25.Grote L, Hedner J, Grunstein R, Kraiczi H. Therapy with nCPAP: incomplete elimination of Sleep Related Breathing Disorder. Eur Respir J. 2000;16:921–7. doi: 10.1183/09031936.00.16592100. [DOI] [PubMed] [Google Scholar]
- 26.Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007;30:711–9. doi: 10.1093/sleep/30.6.711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang Q, Phillips CL, Melehan KL, Rogers NL, Seale JP, Grunstein RR. Effects of short-term CPAP withdrawal on neurobehavioral performance in patients with obstructive sleep apnea. Sleep. 2006;29:545–52. doi: 10.1093/sleep/29.4.545. [DOI] [PubMed] [Google Scholar]
- 28.Phillips CL, Yang Q, Williams A, Roth M, Yee BJ, Hedner JA, et al. The effect of short-term withdrawal from continuous positive airway pressure therapy on sympathetic activity and markers of vascular inflammation in subjects with obstructive sleep apnoea. J Sleep Res. 2007;16:217–25. doi: 10.1111/j.1365-2869.2007.00589.x. [DOI] [PubMed] [Google Scholar]
- 29.Filtness AJ, Reyner LA, Horne JA. One night’s CPAP withdrawal in otherwise compliant OSA patients: marked driving impairment but good awareness of increased sleepiness. Sleep Breath. 2012;16:865–71. doi: 10.1007/s11325-011-0588-8. [DOI] [PubMed] [Google Scholar]
- 30.Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245–58. [PMC free article] [PubMed] [Google Scholar]
- *31.Troxel WM. It’s more than sex: exploring the dyadic nature of sleep and implications for health. Psychosom Med. 2010;72:578–86. doi: 10.1097/PSY.0b013e3181de7ff8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Troxel WM, Robles TF, Hall M, Buysse DJ. Marital quality and the marital bed: examining the covariation between relationship quality and sleep. Sleep Med Rev. 2007;11:389–404. doi: 10.1016/j.smrv.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ashtyani H, Hutter DA. Collateral damage: the effects of obstructive sleep apnea on bed partners. Chest. 2003;124:780–1. doi: 10.1378/chest.124.3.780. [DOI] [PubMed] [Google Scholar]
- 34.Parish JM, Lyng PJ. Quality of life in bed partners of patients with obstructive sleep apnea or hypopnea after treatment with continuous positive airway pressure. Chest. 2003;124:942–7. doi: 10.1378/chest.124.3.942. [DOI] [PubMed] [Google Scholar]
- 35.Billmann SJ, Ware JC. Marital satisfaction of wives of untreated sleep apneic men. Sleep Med. 2002;3:55–9. doi: 10.1016/s1389-9457(01)00118-6. [DOI] [PubMed] [Google Scholar]
- 36.McArdle N, Kingshott R, Engleman HM, Mackay TW, Douglas NJ. Partners of patients with sleep apnoea/hypopnoea syndrome: effect of CPAP treatment on sleep quality and quality of life. Thorax. 2001;56:513–8. doi: 10.1136/thorax.56.7.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brin YS, Reuveni H, Greenberg S, Tal A, Tarasiuk A. Determinants affecting initiation of continuous positive airway pressure treatment. Isr Med Assoc J. 2005;7:13–8. [PubMed] [Google Scholar]
- 38.Virkkula P, Bachour A, Hytonen M, Malmberg H, Salmi T, Maasilta P. Patient- and bed partner-reported symptoms, smoking, and nasal resistance in sleep-disordered breathing. Chest. 2005;128:2176–82. doi: 10.1378/chest.128.4.2176. [DOI] [PubMed] [Google Scholar]
- 39.Ulfberg J, Carter N, Talback M, Edling C. Adverse health effects among women living with heavy snorers. Health Care Women Int. 2000;21:81–90. doi: 10.1080/073993300245311. [DOI] [PubMed] [Google Scholar]
- 40.Cartwright RD, Knight S. Silent partners: the wives of sleep apneic patients. Sleep. 1987;10:244–8. doi: 10.1093/sleep/10.3.244. [DOI] [PubMed] [Google Scholar]
- 41.Kiely JL, McNicholas WT. Bed partners’ assessment of nasal continuous positive airway pressure therapy in obstructive sleep apnea. Chest. 1997;111:1261–5. doi: 10.1378/chest.111.5.1261. [DOI] [PubMed] [Google Scholar]
- 42.Smith AK, Togeiro SM, Tufik S, Roizenblatt S. Disturbed sleep and musculoskeletal pain in the bed partner of patients with obstructive sleep apnea. Sleep Med. 2009;10:904–12. doi: 10.1016/j.sleep.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 43.Doherty LS, Kiely JL, Lawless G, McNicholas WT. Impact of nasal continuous positive airway pressure therapy on the quality of life of bed partners of patients with obstructive sleep apnea syndrome. Chest. 2003;124:2209–14. doi: 10.1378/chest.124.6.2209. [DOI] [PubMed] [Google Scholar]
- 44.McFadyen TA, Espie CA, McArdle N, Douglas NJ, Engleman HM. Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. Eur Respir J. 2001;18:996–1002. doi: 10.1183/09031936.01.00209301. [DOI] [PubMed] [Google Scholar]
- 45.Beninati W, Harris CD, Herold DL, Shepard JW., Jr The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clin Proc. 1999;74:955–8. doi: 10.4065/74.10.955. [DOI] [PubMed] [Google Scholar]
- 46.Baron KG, Smith TW, Czajkowski LA, Gunn HE, Jones CR. Relationship quality and CPAP adherence in patients with obstructive sleep apnea. Behav Sleep Med. 2009;7:22–36. doi: 10.1080/15402000802577751. [DOI] [PubMed] [Google Scholar]
- 47.Reishtein JL, Maislin G, Weaver TE. Outcome of CPAP treatment on intimate and sexual relationships in men with obstructive sleep apnea. J Clin Sleep Med. 2010;6:221–6. [PMC free article] [PubMed] [Google Scholar]
- 48.Ye L, Pien GW, Ratcliffe SJ, Weaver TE. Gender differences in obstructive sleep apnea and treatment response to continuous positive airway pressure. J Clin Sleep Med. 2009;5:512–8. [PMC free article] [PubMed] [Google Scholar]
- 49.Budweiser S, Luigart R, Jorres RA, Kollert F, Kleemann Y, Wieland WF, et al. Long-term changes of sexual function in men with obstructive sleep apnea after initiation of continuous positive airway pressure. J Sex Med. 2013;10:524–31. doi: 10.1111/j.1743-6109.2012.02968.x. [DOI] [PubMed] [Google Scholar]
- 50.McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med. 1999;159:1108–14. doi: 10.1164/ajrccm.159.4.9807111. [DOI] [PubMed] [Google Scholar]
- 51.Billings ME, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, Redline S, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34:1653–8. doi: 10.5665/sleep.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ye L, Pack AI, Maislin G, Dinges D, Hurley S, McCloskey S, et al. Predictors of Continuous Positive Airway Pressure Use during the First Week of Treatment. J Sleep Res. 2012;21:419–26. doi: 10.1111/j.1365-2869.2011.00969.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Simon-Tuval T, Reuveni H, Greenberg-Dotan S, Oksenberg A, Tal A, Tarasiuk A. Low socioeconomic status is a risk factor for CPAP acceptance among adult OSAS patients requiring treatment. Sleep. 2009;32:545–52. doi: 10.1093/sleep/32.4.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pelletier-Fleury N, Rakotonanahary D, Fleury B. The age and other factors in the evaluation of compliance with nasal continuous positive airway pressure for obstructive sleep apnea syndrome. A Cox’s proportional hazard analysis. Sleep Med. 2001;2:225–32. doi: 10.1016/s1389-9457(00)00063-0. [DOI] [PubMed] [Google Scholar]
- 55.Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121:430–5. doi: 10.1378/chest.121.2.430. [DOI] [PubMed] [Google Scholar]
- 56.Budhiraja R, Parthasarathy S, Drake CL, Roth T, Sharief I, Budhiraja P, et al. Early CPAP use identifies subsequent adherence to CPAP therapy. Sleep. 2007;30:320–4. [PubMed] [Google Scholar]
- 57.Aloia MS, Arnedt JT, Stepnowsky C, Hecht J, Borrelli B. Predicting treatment adherence in obstructive sleep apnea using principles of behavior change. J Clin Sleep Med. 2005;1:346–53. [PubMed] [Google Scholar]
- 58.Stepnowsky CJ, Jr, Bardwell WA, Moore PJ, Ancoli-Israel S, Dimsdale JE. Psychologic correlates of compliance with continuous positive airway pressure. Sleep. 2002;25:758–62. doi: 10.1093/sleep/25.7.758. [DOI] [PubMed] [Google Scholar]
- 59.Stepnowsky CJ, Jr, Marler MR, Ancoli-Israel S. Determinants of nasal CPAP compliance. Sleep Med. 2002;3:239–47. doi: 10.1016/s1389-9457(01)00162-9. [DOI] [PubMed] [Google Scholar]
- 60.Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24:461–5. doi: 10.1183/09031936.04.00114603. [DOI] [PubMed] [Google Scholar]
- 61.Wells RD, Freedland KE, Carney RM, Duntley SP, Stepanski EJ. Adherence, reports of benefits, and depression among patients treated with continuous positive airway pressure. Psychosom Med. 2007;69:449–54. doi: 10.1097/psy.0b013e318068b2f7. [DOI] [PubMed] [Google Scholar]
- 62.Chasens ER, Pack AI, Maislin G, Dinges DF, Weaver TE. Claustrophobia and adherence to CPAP treatment. West J Nurs Res. 2005;27:307–21. doi: 10.1177/0193945904273283. [DOI] [PubMed] [Google Scholar]
- *63.Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev. 2011;15:343–56. doi: 10.1016/j.smrv.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med. 1999;159:1096–100. doi: 10.1164/ajrccm.159.4.9808008. [DOI] [PubMed] [Google Scholar]
- 65.Hui DS, Chan JK, Choy DK, Ko FW, Li TS, Leung RC, et al. Effects of augmented continuous positive airway pressure education and support on compliance and outcome in a Chinese population. Chest. 2000;117:1410–6. doi: 10.1378/chest.117.5.1410. [DOI] [PubMed] [Google Scholar]
- 66.Aloia MS, Di Dio L, Ilniczky N, Perlis ML, Greenblatt DW, Giles DE. Improving compliance with nasal CPAP and vigilance in older adults with OAHS. Sleep Breath. 2001;5:13–21. doi: 10.1007/s11325-001-0013-9. [DOI] [PubMed] [Google Scholar]
- 67.Aloia MS, Smith K, Arnedt JT, Millman RP, Stanchina M, Carlisle C, et al. Brief behavioral therapies reduce early positive airway pressure discontinuation rates in sleep apnea syndrome: preliminary findings. Behav Sleep Med. 2007;5:89–104. doi: 10.1080/15402000701190549. [DOI] [PubMed] [Google Scholar]
- 68.Sparrow D, Aloia M, Demolles DA, Gottlieb DJ. A telemedicine intervention to improve adherence to continuous positive airway pressure: a randomised controlled trial. Thorax. 2010;65:1061–6. doi: 10.1136/thx.2009.133215. [DOI] [PubMed] [Google Scholar]
- 69.Richards D, Bartlett DJ, Wong K, Malouff J, Grunstein RR. Increased adherence to CPAP with a group cognitive behavioral treatment intervention: a randomized trial. Sleep. 2007;30:635–40. doi: 10.1093/sleep/30.5.635. [DOI] [PubMed] [Google Scholar]
- 70.Weaver TE, Maislin G, Dinges DF, Younger J, Cantor C, McCloskey S, et al. Self-efficacy in sleep apnea: instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep. 2003;26:727–32. doi: 10.1093/sleep/26.6.727. [DOI] [PubMed] [Google Scholar]
- 71.Cutrona CE. Social Support in Couples: Marriage as a Rescource in Times of Stress. Thousand Oaks: Sage Publications; 1996. [Google Scholar]
- *72.Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev. 2014;1:CD007736. doi: 10.1002/14651858.CD007736.pub2. [DOI] [PubMed] [Google Scholar]
- 73.Lewis KE, Seale L, Bartle IE, Watkins AJ, Ebden P. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep. 2004;27:134–8. doi: 10.1093/sleep/27.1.134. [DOI] [PubMed] [Google Scholar]
- 74.Cartwright R. Sleeping together: a pilot study of the effects of shared sleeping on adherence to CPAP treatment in obstructive sleep apnea. J Clin Sleep Med. 2008;4:123–7. [PMC free article] [PubMed] [Google Scholar]
- *75.Brostrom A, Nilsen P, Johansson P, Ulander M, Stromberg A, Svanborg E, et al. Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: a qualitative content analysis. Sleep Med. 2010;11:126–30. doi: 10.1016/j.sleep.2009.04.010. [DOI] [PubMed] [Google Scholar]
- *76.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–18. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- *77.Baron KG, Smith TW, Berg CA, Czajkowski LA, Gunn H, Jones CR. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep Breath. 2011;15:525–34. doi: 10.1007/s11325-010-0374-z. [DOI] [PubMed] [Google Scholar]
- *78.Baron KG, Gunn HE, Czajkowski LA, Smith TW, Jones CR. Spousal involvement in CPAP: does pressure help? J Clin Sleep Med. 2012;8:147–53. doi: 10.5664/jcsm.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lewis MA, Rook KS. Social control in personal relationships: impact on health behaviors and psychological distress. Health Psychol. 1999;18:63–71. doi: 10.1037//0278-6133.18.1.63. [DOI] [PubMed] [Google Scholar]
- 80.Tucker JS, Anders SL. Social Control of Health Behaviors in marriage. J Appl Soc Psychol. 2001;31:467–85. [Google Scholar]
- 81.Bodenmann G. Dyadic coping and its significance for marital functioning. In: Revenson TA, Kayser K, Bodenmann G, editors. Couples coping with stress: Emerging perspectives on dyadic coping. Washington D.C.: American Psychological Association; 2005. pp. 33–49. [Google Scholar]
- 82.Revenson TA, Kayser K, Bodenmann G. Couples coping with stress: Emerging perspectives on dyadic coping. Washington D.C.: American Psychological Association; 2005. [Google Scholar]
- 83.Kayser K, Feldman B, Borstelmann N, Daniels A. Effects of a Randomized Couple-based Intervention on Quality of Life of Breast Cancer Patients and Their Partners. Soc Work Res. 2010;34:20–32. [Google Scholar]
- 84.Bodenmann G, Plancherel B, Beach SR, Widmer K, Gabriel B, Meuwly N, et al. Effects of coping-oriented couples therapy on depression: a randomized clinical trial. J Consult Clin Psychol. 2008;76:944–54. doi: 10.1037/a0013467. [DOI] [PubMed] [Google Scholar]
- 85.Bodenmann G. Dyadic Coping Inventar: Manual [Dyadic Coping Inventory: Manual] Bern, Switzerland: Huber; 2008. [Google Scholar]
- 86.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–70. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 87.Grunstein RR, Stenlof K, Hedner JA, Sjostrom L. Impact of self-reported sleep-breathing disturbances on psychosocial performance in the Swedish Obese Subjects (SOS) Study. Sleep. 1995;18:635–43. doi: 10.1093/sleep/18.8.635. [DOI] [PubMed] [Google Scholar]
- 88.Ubbiali A, Donati D, Chiorri C, Bregani V, Cattaneo E, Maffei C, et al. Prediction of adherence to antiretroviral therapy: can patients’ gender play some role? An Italian pilot study. AIDS Care. 2008;20:571–5. doi: 10.1080/09540120701867172. [DOI] [PubMed] [Google Scholar]
- 89.Bolger N, Zuckerman A, Kessler RC. Invisible support and adjustment to stress. J Pers Soc Psychol. 2000;79:953–61. doi: 10.1037//0022-3514.79.6.953. [DOI] [PubMed] [Google Scholar]
- 90.Lewis MA, Butterfiled R, Darbes L, Johnston-Brooks C. The conceptualization and assessment of health-related social control. J Soc Pers Relatsh. 2004;21:669–87. [Google Scholar]
- 91.Elfstrom M, Karlsson S, Nilsen P, Fridlund B, Svanborg E, Brostrom A. Decisive situations affecting partners’ support to continuous positive airway pressure-treated patients with obstructive sleep apnea syndrome: a critical incident technique analysis of the initial treatment phase. J Cardiovasc Nurs. 2012;27:228–39. doi: 10.1097/JCN.0b013e3182189c34. [DOI] [PubMed] [Google Scholar]
- 92.Stephens MA, Fekete EM, Franks MM, Rook KS, Druley JA, Greene K. Spouses’ use of pressure and persuasion to promote osteoarthritis patients’ medical adherence after orthopedic surgery. Health Psychol. 2009;28:48–55. doi: 10.1037/a0012385. [DOI] [PubMed] [Google Scholar]
- 93.Stephens MA, Rook KS, Franks MM, Khan C, Iida M. Spouses use of social control to improve diabetic patients’ dietary adherence. Fam Syst Health. 2010;28:199–208. doi: 10.1037/a0020513. [DOI] [PubMed] [Google Scholar]
- 94.Black DR, Gleser LJ, Kooyers KJ. A meta-analytic evaluation of couples weight-loss programs. Health Psychol. 1990;9:330–47. doi: 10.1037//0278-6133.9.3.330. [DOI] [PubMed] [Google Scholar]
- 95.Wermuth L, Scheidt S. Enlisting family support in drug treatment. Fam Process. 1986;25:25–33. doi: 10.1111/j.1545-5300.1986.00025.x. [DOI] [PubMed] [Google Scholar]
- 96.Remien RH, Stirratt MJ, Dolezal C, Dognin JS, Wagner GJ, Carballo-Dieguez A, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19:807–14. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- 97.van Dam HA, van der Horst FG, Knoops L, Ryckman RM, Crebolder HF, van den Borne BH. Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ Couns. 2005;59:1–12. doi: 10.1016/j.pec.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 98.Rea MM, Tompson MC, Miklowitz DJ, Goldstein MJ, Hwang S, Mintz J. Family-focused treatment versus individual treatment for bipolar disorder: results of a randomized clinical trial. J Consult Clin Psychol. 2003;71:482–92. doi: 10.1037/0022-006x.71.3.482. [DOI] [PubMed] [Google Scholar]
- 99.Billette V, Guay S, Marchand A. Posttraumatic stress disorder and social support in female victims of sexual assault: the impact of spousal involvement on the efficacy of cognitive-behavioral therapy. Behav Modif. 2008;32:876–96. doi: 10.1177/0145445508319280. [DOI] [PubMed] [Google Scholar]
- *100.Rogojanski J, Carney CE, Monson CM. Interpersonal factors in insomnia: a model for integrating bed partners into cognitive behavioral therapy for insomnia. Sleep Med Rev. 2013;17:55–64. doi: 10.1016/j.smrv.2012.02.003. [DOI] [PubMed] [Google Scholar]


