Abstract
Background
The advent of combined antiretroviral therapy (ART) in the past decade has led to HIV suppression in most cases. Virological failure was the main reason for ART switch a few years ago; however, toxicity and treatment simplification have now gained importance due to the availability of more effective and convenient drugs. This study assessed the reasons for ART switch in daily practice.
Material and Methods
Observational retrospective study that included patients whose ART was switched between January 2011 and July 2012. Patients with any other switch during the follow-up period (until September 2013) were excluded.
Results
A total of 246 patients were included. Main reasons for ART switch were simplification (33%) and toxicity (31%), followed by clinical trial inclusion (13%), virological failure (6%), drug interaction (4%), patient decision (3%), lack of adherence (2%), pregnancy (1%) and other (8%). Eighty patients switched to a simpler regimen (median age 48 [40–53], mean CD4 count 608±265 cells/cl, 89% <50 copies/ml, mean number of previous regimens 6±5, mean time on previous ART 3±2 years). In this case, previous ART mostly included 2NRTI+1PI/r (54%) (Figure 1). The simplification strategy mainly contained nuke-sparing regimens (60%) based on PI (DRV/r 48%): monotherapy 46%, dual therapy 13% (PI/r+maraviroc 9%, PI/r+NNRTI 4%) and triple therapy 1% (PI/r+maraviroc+raltegravir). The second preferred simplification option was 2NRTI+1NNRTI (24%). Seventy-seven patients switched due to toxicities (median age 47 [43–53], mean CD4 count 606±350 cells/μl, <50 copies/ml 82%, mean number of previous regimens 4±3, mean time on previous ART 3±3 years). Renal (25%) and CNS (18%) toxicities were the main reasons for ART switch, followed by diarrhoea (16%), liver enzyme elevation (ALT 10%; AST 9%; bilirubin 7%), lipid elevation (cholesterol 5%; triglycerides 8%), nausea (7%) and other (=5%) (Figure 2). All patients with renal toxicity were under TDF and in most cases this drug was removed from the new regimen (with 3TC/ABC or nuke-sparing). Among patients with CNS toxicity, 79% were taking EFV; the main new treatment was a second-generation NNRTI (ETR)+2NRTI. Toxicities were completely resolved in 66% of patients, partially resolved in 22% and not resolved in only 12%; the median time from ART switch to toxicity resolution was 4 (2–8) months.
Conclusions
The main reasons for ART switch in daily practice are simplification and toxicities, renal and CNS toxicities being the most prevalent. The preferred simplification strategies are nuke-sparing regimens, mainly DRV/r-based monotherapy and dual therapy. ART switch leads to a complete resolution of toxicities in most cases in the short term.
Figure 1.
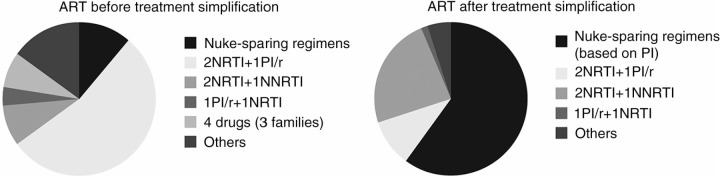
Antiretroviral therapy before and after treatment simplification (N=80).
Figure 2.
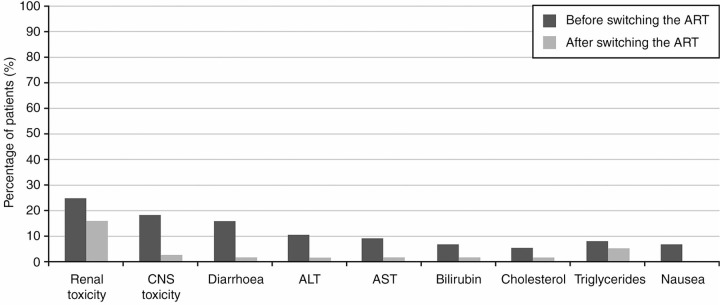
Main toxicities before and after switching the antiretroviral therapy (N=77).


