Abstract
Objective
To examine the amount of objectively measured MVPA and LPA that is associated with long-term weight loss and the maintenance of clinically significant weight loss.
Design and Methods
Adults (N=260; BMI: 25 to <40 kg/m2; age: 18–55 years) participated in an 18month behavioral weight loss intervention and were prescribed a low-calorie diet and increased physical activity. Change in weight and objectively measured physical activity were assessed. MVPA>10 (METmin/wk) was computed from bouts ≥10 minutes and ≥3.0 METS and MVPA<10 was computed from bouts <10 minutes in duration and ≥3.0 METS. LPA was computed from bouts between 1.5 to <3.0 METS.
Results
When grouped on percent weight loss at 18 months, there was a significant Group X Time interaction effect (p<0.0001) for both MVPA>10 and LPA, with both measures being significantly greater at 18 months in those with ≥10% weight loss. Similar results were observed for MVPA>10 and LPA with participants grouped on achieving ≥10% weight loss at 6 months and sustaining this at 18 months.
Conclusions
MVPA>10 of 200 to 300 minutes per week, coupled with increased amounts of LPA, are associated with improved long-term weight loss. Interventions should promote engagement in these amounts and types of physical activity.
Keywords: Physical Activity, Exercise, Obesity, Weight Loss, Weight Maintenance
INTRODUCTION
Overweight (BMI ≥25 kg/m2) and obesity (BMI ≥30 kg/m2) are significant public health concerns associated with chronic health conditions.(1, 2) The cornerstone of lifestyle interventions include reduced energy intake and increased energy expenditure, and a key behavior for enhancing weight loss is physical activity. Physical activity accounts for approximately 2–3 kg of weight loss beyond what is achieved through diet modification over a period of up to 6 months,(2, 3) and is associated with improved long-term weight loss.(4, 5, 6, 7, 8, 9, 10) The amount of moderate-to-vigorous intensity physical activity (MVPA) associated with improved long-term weight loss appears to be approximately 250–300 minutes per week.(3)
The amount of physical activity associated with improved long-term weight loss is based mostly on self-report of MVPA.(5, 6, 7, 8, 10) Given the potential for persons who are overweight or obese to over-report their physical activity,(11, 12) it is unclear if self-reported data accurately reflect the amount of MVPA that is associated with improved long-term weight loss. Moreover, reliance on self-report has limited the ability to understand the contribution of various intensities of physical activity, particularly light intensity activity (LPA), on weight loss, which has not been examined in prior studies. Use of objective assessment of physical activity would provide greater insight into the amount of MVPA required and the potential contribution of LPA related to weight loss.
Objectively measured physical activity was assessed within the context of an 18 month behavioral weight loss program to examine the amount of MVPA and the contribution of LPA that is associated with absolute weight loss and patterns of weight loss.
METHODS AND PROCEDURES
Participants
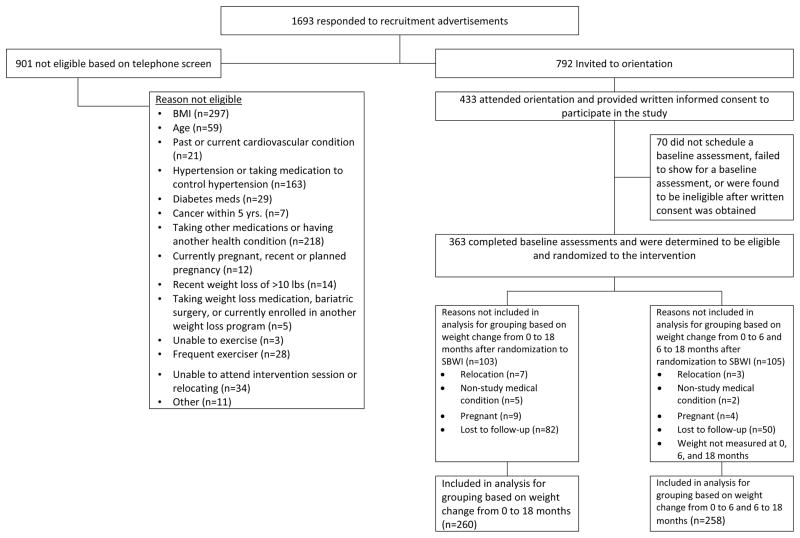
Participants were recruited between May 2008 and February 2010, with data collection completed by September 2011. Procedures were approved by the Institutional Review Boards at the University of Pittsburgh and University of North Carolina at Chapel Hill; the two clinical sites for this study.
Participants were recruited through television, newspaper, and other mass media advertisements. Interested individuals provided verbal consent prior to completion of a telephone screening that was used to determine initial eligibility, with this information being confirmed at an in-person visit after written informed consent was obtained. A medical history and a physical activity readiness questionnaire were completed, in addition to clearance from the individual’s physician that was obtained prior to any additional data collection and prior to randomization in the weight loss intervention. Eligibility criteria included body mass index (BMI) within 25.0 to <40.0 kg/m2 and age between 18 to 55 years, along with additional eligibility criteria previously reported.(13)
This study randomized 363 individuals; however, 2 participants did not provide objectively measured physical activity at baseline, resulting in 361 participants with valid data at baseline. Demographic characteristics are presented in Table 1. Justification for sample size, the process for randomization, and the consort diagram for the primary outcomes have previously been published.(13)
Table 1.
Descriptive characteristics of participants [mean±S.E.M.]
| Subjects Randomized | Subjects with both Baseline and 18 Month Weight Measured | Subjects with both Baseline, 6, and 18 Month Weight Measured | |
|---|---|---|---|
| Demographic Variable | Number (%) | Number (%) | Number (%) |
| Number of Subjects [Number (% of total)] | 363 (100%) | 260 (100%) | 258 (100%) |
| Gender(Females) [Number (% of total)] | 300 (82.6%) | 206 (79.2%) | 206 (79.8%) |
| Age(years) | 42.2±9.0 | 42.8±8.9 | 42.9±8.9 |
| Body Mass Index(kg/m2) | 33.0±3.6 | 32.7±3.5 | 32.8±3.5 |
| Ethnicity [Number (% of total)] | |||
| Asian | N=2 (0.6%) | N=2 (0.8%) | N=2 (0.8%) |
| Black or AfricanAmerican | N=103 (28.4%) | N=69 (26.5%) | N=68 (26.4%) |
| Hispanic, Latino, Portuguese, Cape Verdean | N=7 (1.9%) | N=5 (1.9%) | N=5 (1.9%) |
| White | N=243 (66.9%) | N=181 (69.6%) | N=180 (69.8%) |
| Other | N=8 (2.2%) | N=3 (1.2%) | N=3 (1.2%) |
| Education Level [Number (% of total)] | |||
| High School(1012 years) | N=24 (6.6%) | N=15 (5.8%) | N=15 (5.8%) |
| Vocational Training(beyond High School) | N=18 (5.0%) | N=11 (4.2%) | N=11 (4.3%) |
| Some College(less than 4 years) | N=105 (28.9%) | N=75 (28.9%) | N=74 (28.7%) |
| College/University Degree | N=122 (33.6%) | N=90 (34.6%) | N=89 (34.5%) |
| Graduate or Professional Education | N=92 (25.3%) | N=68 (26.2%) | N=68 (26.4%) |
Outcome Assessments
Body weight was assessed at 0, 3, 6, 9, 12, 15, and 18 months, and objectively measured physical activity assessed at 0, 6, 12, and 18 months. Participants were compensated $25 for completion of assessments at 0, 6, 12, and 18 months, and compensated $10 for completion of assessments at 3, 9, and 15 months. Assessment staff knew that the participants were in an active weight loss intervention program because this study did not include a no-treatment control group. To minimize the potential for bias, the staff did not have access to the prior assessment data when assessments were being conducted.
Weight was assessed on a scale to the nearest 0.1 kg with the participant clothed in a hospital gown or light-weight clothing. Height was measured only at baseline to the nearest 0.1 cm. BMI was computed as kg/m2.
Physical activity was measured using a device worn as an armband for one week (SenseWear Pro Armband, BodyMedia, Inc.) at each of the assessment periods to provide an estimate of minute-byminute energy expenditure. This device has been shown to provide a valid measure of energy expenditure.(14, 15) Minute-by-minute energy expenditure was converted to metabolic equivalents (METs). These data were used to identify minutes of LPA (1.5 to <3.0 METS) and MVPA (≥3.0 METs). Data were considered valid and used for analysis only if the participants wore the device for ≥10 hours per day for ≥4 days, as it has been reported that this amount of objectively measured physical activity is sufficient to determine a consistent pattern of physical activity.(16, 17) Data are presented as MET-minutes per week (MET-min/wk).
Behavioral Weight Loss Intervention
Participants were randomized to one of two 18 month behavior weight loss interventions, a standard behavioral weight loss intervention (SBWL) or a stepped-care intervention (STEP). The details of the intervention and the main study results have previously been published,(13) and a brief description is provided below.
Diet Recommendations
SBWL and STEP were prescribed an energy-reduced diet consisting of 1200 to 1800 kcal/day based on initial body weight, and reduce fat intake of 20 to 30% of total energy intake.
Physical Activity
SBWL and STEP were prescribed a physical activity program. Physical activity was initially prescribed at 100 min/week and progressed by 50 minutes every 4 weeks until a prescription of 300 min/week was achieved. Participants were encouraged to be physically active in bouts that were ≥10 minutes in duration and at a moderate-to-vigorous intensity.
SBWL Intervention
SBWL was instructed to attend group-based intervention sessions. These intervention sessions were conducted weekly during months 1–6, bi-weekly during months 7–12, and monthly during months 13–18. Each group session was focused on a specific topic related to weight loss that addressed diet, physical activity, or specific behavioral strategies to support the prescribed diet and physical activity recommendations. Participants who were unable to attend a group session were offered an individual make-up session, and if this was not possible an attempt was made for the interventionist to speak with the participant by telephone.
STEP Intervention
STEP was instructed to attend one group-based intervention session per month over the 18 month intervention period. As previously reported,(13) participants were given weight loss goals of 5% at 3 months, 7% at 6 months, and 10% at 9, 12, and 15 months. Failure to achieve any of these a-priori weight loss goals resulted in additional intervention contact by telephone or in-person, or additional weight loss strategies (e.g. supervised exercise, meal replacements) being added to the intervention in a stepped-care manner as previously reported. Each intervention contact focused on a specific topic related to weight loss that addressed diet, physical activity, or specific behavioral strategies to support the prescribed diet and physical activity recommendations. Participants who were unable to attend a scheduled intervention session were offered make-up sessions.
Statistical Analysis
Statistical analyses were performed using SAS (version 9.2), with the type I error rate fixed at 0.05 (two-tailed). Normality of outcome variables was checked using the Kolmogorov-Smirnov test.
Two grouping variables were created: one based on weight change over the 18-months and the other based on weight change patterns at both 6-and 18-months. Separate mixed effects models using the first-order autoregressive dependence structure, AR(1), were fit to the outcomes. Weight measured at baseline, 3-, 6-, 9-, 12-, 15-and 18-months were analyzed using a mixed effects model with 7 time points. Inferences were focused on the main effects of weight change groups, time and the interaction effect between these two. Randomization stratification factors such as clinic, gender, and race were adjusted in the mixed effects model as covariates. Missing weight measures were handled using the multiple imputation methods implemented in SAS using the PROC MI and PROC MIANALYZE. A total of 10 imputation datasets were generated, analyzed, and summarized. The least square means obtained from the mixed effects model were presented. Weight changes from baseline and % weight change from baseline were analyzed similarly using separate mixed effects models with 6 time points with additional adjustment for the baseline weight.
For MET-min/wk, the square root transformation was used to correct for the skewedness in its distribution. Only participants with objective physical activity measured for at least one time point (0, 6, 12, or 18 months) were included in the analysis, and missing MET-min/wk were imputed to be zero. Separate mixed effects models with 4 time points were fitted to the MET-min/wk for each of the following activity bouts: ≥1 minute in duration and between 1.5 to <3.0 METS (LPA), ≥1 minute in duration and ≥3.0 METs (MVPA-TOTAL), between 1 and <10 minutes in duration and ≥3.0 METs (MVPA<10), and ≥10 minute in duration and ≥3.0 METS (MVPA≥10). The least square means obtained from these models were back-transformed and so were the 95% confidence limits. Pairwise comparisons were performed at a significance level that was adjusted using the Bonferroni method, resulting in a type I error rate of 0.008 for 6 pairwise comparisons among the 4 groups.
RESULTS
Physical Activity Comparison based on 18 Month Weight Loss
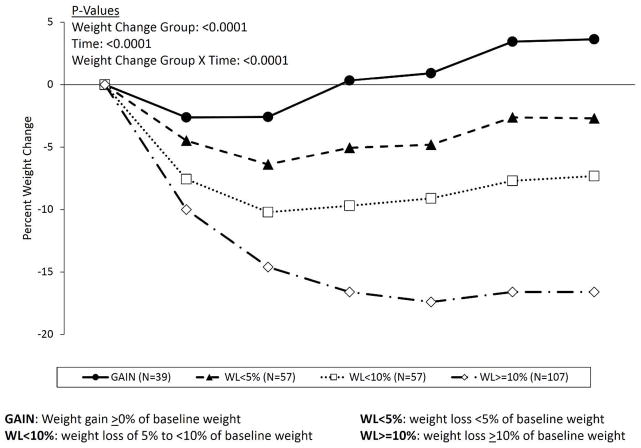
Participants were grouped on the magnitude of percent weight change from baseline to 18 months. It has been suggested that health benefits can be realized with 5% weight loss, (18, 19) and weight loss of 10% has been recommended as an important clinical target.(2) Therefore, these weight loss targets were used to categorize participants, with groups consisting of weight gain (GAIN), weight loss <5% (WL<5%), weight loss of 5% to <10% (WL<10%), and weight loss ≥10% (WL≥10%). To be placed into the appropriate group the participant needed to provide weight data at 0 and 18 months, resulting in 260 (71.6%) of the 363 randomized participants being included in the analyses. Demographic characteristics of the sample of the 260 are presented in Table 1 and closely resemble the demographic characteristics of the randomized sample with complete data at baseline. The pattern of weight change over the 18 month intervention is shown in Table 2 and Figure 2. Weight loss at 18 months was significantly different between GAIN (mean±S.E.M.; +3.63±0.72%), WL<5% (−2.70±0.62%), WL<10% (7.33±0.62%), and WL≥10% (−16.6±0.47%) (p<0.0001).
Table 2.
Change in weight by weight loss category.
| Variable | Group Based On 18-Month Weight Change | Assessment Periods | P-Values | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Baseline | 3 Months | 6 Months | 9 Months | 12 Months | 15 Months | 18 Months | Weight Change Group | Time | Weight Change Group X Time | ||
|
| |||||||||||
| Weight(kg) | GAIN (N=39) | 98.65±2.10 | 96.36±2.10 | 96.45±2.10 | 99.19±2.10 | 99.74±2.10 | 102.0±2.10 | 102.2±2.10 | <0.0001 | <0.0001 | <0.0001 |
| WL<5% (N=57) | 99.12±1.82 | 95.02±1.82 | 93.21±1.82 | 94.43±1.82 | 94.78±1.82 | 96.76±1.82 | 96.70±1.82 | ||||
| WL<10% (N=57) | 100.9±1.79 | 93.55±1.79 | 91.09±1.79 | 91.63±1.79 | 92.19±1.79 | 93.49±1.79 | 93.85±1.79 | ||||
| WL≥10% (N=107) | 99.00±1.39 | 89.22±1.39 | 84.90±1.39 | 83.11±1.39 | 82.41±1.39 | 83.09±1.39 | 83.10±1.39 | ||||
|
| |||||||||||
| Weight Change from Baseline (kg) | GAIN | −2.65±0.70 | −2.57±0.70 | 0.17±0.71 | 0.72±0.70 | 2.98±0.71 | 3.17±0.70 | <0.0001 | <0.0001 | <0.0001 | |
| WL<5% | −4.36±0.61 | −6.17±0.60 | −4.95±0.61 | −4.60±0.60 | −2.62±0.60 | −2.68±0.60 | |||||
| WL<10% | −7.17±0.60 | −9.63±0.60 | −9.08±0.60 | −8.53±0.60 | −7.22±0.60 | −6.87±0.60 | |||||
| WL≥10% | −9.37±0.46 | −13.7±0.46 | −15.5±0.46 | −16.2±0.46 | −15.5±0.46 | −15.5±0.46 | |||||
|
| |||||||||||
| Percent Weight Change from Baseline (%) | GAIN | −2.63±0.72 | −2.58±0.72 | 0.33±0.73 | 0.92±0.72 | 3.45±0.72 | 3.63±0.72 | <0.0001 | <0.0001 | <0.0001 | |
| WL<5% | −4.49±0.62 | −6.40±0.62 | −5.06±0.62 | −4.80±0.62 | −2.63±0.62 | −2.70±0.62 | |||||
| WL<10% | −7.58±0.62 | −10.2±0.62 | −9.70±0.62 | −9.10±0.62 | −7.71±0.62 | −7.33±0.62 | |||||
| WL≥10% | −10.0±0.47 | −14.6±0.47 | −16.6±0.47 | −17.4±0.47 | −16.6±0.47 | −16.6±0.47 | |||||
|
| |||||||||||
| Group Based On 6 and 18-Month Weight Change | |||||||||||
|
| |||||||||||
| Weight(kg) | NON-LOSS (N=107) | 99.06±1.44 | 96.04±1.44 | 95.13±1.44 | 96.54±1.44 | 96.56±1.44 | 98.19±1.44 | 97.99±1.44 | <0.0001 | <0.0001 | <0.0001 |
| LATE-LOSS (N=19) | 97.74±2.99 | 93.01±2.99 | 91.35±2.99 | 89.77±2.99 | 88.19±2.99 | 87.18±2.99 | 85.53±2.99 | ||||
| NON-MAINTAIN (N=45) | 101.0±2.00 | 91.75±2.00 | 88.49±2.00 | 89.67±2.00 | 91.25±2.00 | 93.62±2.00 | 94.82±2.00 | ||||
| MAINTAIN (N=87) | 99.34±1.54 | 88.48±1.54 | 83.58±1.54 | 81.71±1.54 | 81.19±1.54 | 82.21±1.54 | 82.60±1.54 | ||||
|
| |||||||||||
| Weight Change from Baseline (kg) | NON-LOSS | −3.14±0.46 | −4.05±0.46 | −2.64±0.46 | −2.62±0.46 | −0.99±0.46 | −1.19±0.46 | <0.0001 | <0.0001 | <0.0001 | |
| LATE-LOSS | −4.87±0.97 | −6.54±0.97 | −8.12±0.97 | −9.70±0.97 | −10.7±0.97 | −12.4±0.97 | |||||
| NON-MAINTAIN | −8.89±0.66 | −12.1±0.66 | −11.0±0.66 | −9.39±0.66 | −7.02±0.66 | −5.82±0.66 | |||||
| MAINTAIN | −10.3±0.50 | −15.2±0.50 | −17.1±0.50 | −17.6±0.50 | −16.6±0.50 | −16.2±0.50 | |||||
|
| |||||||||||
| Percent Weight Change from Baseline (%) | NON-LOSS | −3.16±0.48 | −4.15±0.48 | −2.67±0.48 | −2.70±0.48 | −0.88±0.48 | −1.12±0.48 | <0.0001 | <0.0001 | <0.0001 | |
| LATE-LOSS | −5.11±1.00 | −7.05±1.00 | −8.76±1.01 | −10.5±1.00 | −11.5±1.00 | −13.3±1.00 | |||||
| NON-MAINTAIN | −9.44±0.68 | −12.9±0.68 | −11.6±0.68 | −9.93±0.68 | −7.46±0.68 | −6.16±0.68 | |||||
| MAINTAIN | −11.1±0.51 | −16.3±0.51 | −18.3±0.51 | −18.9±0.51 | −17.8±0.51 | −17.4±0.51 | |||||
GAIN: Weight gain ≥0% of baseline weight
WL<5%: weight loss <5% of baseline weight
WL<10%: weight loss of 5% to <10% of baseline weight
WL>10%: weight loss >10% of baseline weight
NON-LOSS: <10% weight loss at both 6 and 18 months
LATE-LOSS: <10% weight loss at 6 months and ≥10 weight loss at 18 months
NON-MAINTAIN: ≥10% weight loss at 6 months and <10% weight loss at 18 months
MAINTAIN: >10% weight loss at both 6 and 18 months
Figure 2.
Percent weight loss based on weight loss achieved at 18 months. 254×190mm (300 × 300 DPI)
The results of the analysis of the physical activity data was not significantly influenced by randomized treatment group assignment (SBWL vs. STEP) and therefore this was not considered further in these analyses. Comparison of MVPA≥10 showed a significant Group X Time interaction (p<0.0001) (Table 3). Post-hoc analysis with Bonferroni adjustment for multiple comparisons (α=0.008) revealed that MET-min/wk for MVPA≥10 was significantly greater in WL≥10% compared to GAIN, WL<5%, and WL<10% at 6, 12 and 18 months. A similar pattern of results was observed for MVPA-TOTAL at 18 months, although relationships were not as strong at 12 months and even less so at 6 months, compared to MVPA≥10. There was no significant difference between 18 month weight loss categories (GAIN, WL<5%, WL<10%, WL≥10%) for MVPA accumulated in bouts 1 to <10 minutes (MVPA<10) (Table 3).
Table 3.
Change in objectively measured physical activity by weight loss at 18 months [LS Means (95% confidence interval)].
| Physical Activity Variable | Group Based On 18-Month Weight Change | Assessment Periods (MET-minutes per Week) | P-Values* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Baseline | 6 Months | 12 Months | 18 Months | Time | Weight Change Group | Weight Change Group X Time | |||||
|
| |||||||||||
| LPA (Bouts ≥1 minute in duration and between 1.5 to <3.0 METS) | GAIN (N=39) | 2922 (2652.6, 3204.8) | 2785.6 (2519.8, 3064.8) | 2472.2 A (2216.7, 2741.6) | 2332.1 A (2080.7, 2597.8) | 0.0014 | 0.0350 | 0.0001 | |||
| WL<5% (N=57) | 3225.0 (2628.1, 3882.9) | 3100.5 (2515.9, 3746.1) | 3079.8 B (2497.3, 3723.4) | 2509.1 B (1986.3, 3093.0) | |||||||
| WL<10% (N=57) | 2909.4 (2530.1, 3315.1) | 3095.1 (2705.5, 3511.0) | 2844.1 (2469.6, 3244.9) | 2613.0 (2247.3, 3006.3) | |||||||
| WL≥10% (N=107) | 2715.3 (2436.0, 3009.6) | 3247.8 (2942.7, 3567.9) | 3185.9 A,B (2881.6, 3505.4) | 3160.0 A,B (2855.8, 3479.6) | |||||||
|
| |||||||||||
| MVPA-TOTAL (Bouts ≥1 minute in duration and ≥3.0 METS) | GAIN | 1484.6 (1273.1, 1712.3) | 1835.4 A,B,C (1596.0, 2091.5) | 1462.3 A (1244.0, 1698.1) | 1377.9 A (1163.6, 1610.3) | <0.0001 | 0.0001 | <0.00001 | |||
| WL<5% | 1662.9 (1194.9, 2208.0) | 2325.2 A (1764.8, 2962.8) | 1961.0 B (1449.5, 2549.7) | 1895.4 B (1393.2, 2474.8) | |||||||
| WL<10% | 1572.3 (1264.5, 1913.6) | 2463.3 B (2076.2, 2883.5) | 1875.6 (1538.2, 2246.5) | 1602.0 C (1283.8, 1955.3) | |||||||
| WL≥10% | 1377.2 (1158.3, 1615.0) | 2724.4 C (2413.9, 3053.6) | 2345.5 A,B (2055.4, 2654.7) | 2365.4 A,B,C (2072.9, 2677.2) | |||||||
|
| |||||||||||
| MVPA<10 (Bouts 1 to <10 minutes in duration and ≥3.0 METS) | GAIN | 1041.5 (925.1, 1164.8) | 1048.4 (930.0, 1173.9) | 899.3 (787.2, 1018.9) | 890.7 (777.6, 1011.4) | 0.0121 | 0.0962 | 0.1576 | |||
| WL<5% | 1134.1 (878.2, 1422.7) | 1195.7 (932.5, 1491.6) | 1125.9 (871.0, 1413.5) | 1066.2 (818.5, 1346.5) | |||||||
| WL<10% | 1156.1 (982.1, 1344.3) | 1268.5 (1087.0, 1464.1) | 1150.4 (977.0, 1337.9) | 1009.1 (843.2, 1189.8) | |||||||
| WL≥10% | 947.8 (828.4, 1075.2) | 1138.7 (1008.0, 1277.4) | 1056.9 (930.0, 1192.0) | 1097.4 (967.5, 1235.6) | |||||||
|
| |||||||||||
| MVPA≥10 (Bouts ≥10 minutes in duration and ≥3.0 METS) | GAIN (N=39) | 337.7 (234.2, 460.2) | 673.3 A,B,C (521.5, 844.5) | 456.9 A (330.3, 604.0) | 392.8 A (274.9, 531.7) | <0.0001 | <0.0001 | <0.0001 | |||
| WL<5% (N=57) | 401.5 (178.6, 713.5) | 1004.5 A,D (626.0, 1472.1) | 694.9 B (387.6, 1091.3) | 709.5 B (398.5, 1109.6) | |||||||
| WL<10% (N=57) | 314.9 (178.1, 490.33 | 1062.1 B,E (796.6, 1365.8) | 616.6 C (417.7, 854.2) | 483.9 C (305.5, 703.2) | |||||||
| WL≥10% (N=107) | 305.2 (200.9, 431.2) | 1515.8 C,D,E (1271.2, 1781.9) | 1156.3 A,B,C (941.7, 1392.8) | 1165.0 A,B,C (948.8, 1403.3) | |||||||
indicates no significant difference between randomized groups (data not presented)
Note: Groups with the same superscript at the same assessment point are significantly different at α<0.008 (p-value of 0.05 adjusted using Bonferroni adjustment for 6 group comparisons at that time point.)
Group Based On 18-Month Weight Change
GAIN: Weight gain ≥0% of baseline weight
WL<5%: weight loss <5% of baseline weight
WL<10%: weight loss of 5% to <10% of baseline weight
WL≥10%: weight loss >10% of baseline weight
LPA showed a significant Group X Time interaction (p<0.0001) (Table 3). Post-hoc analysis with Bonferroni adjustment for multiple comparisons revealed that MET-min/wk for LPA was significantly greater in WL≥10% compared to GAIN and WL<5% at 12 and 18 months.
Physical Activity Comparison by Pattern of Weight Loss at 6 and 18 Months
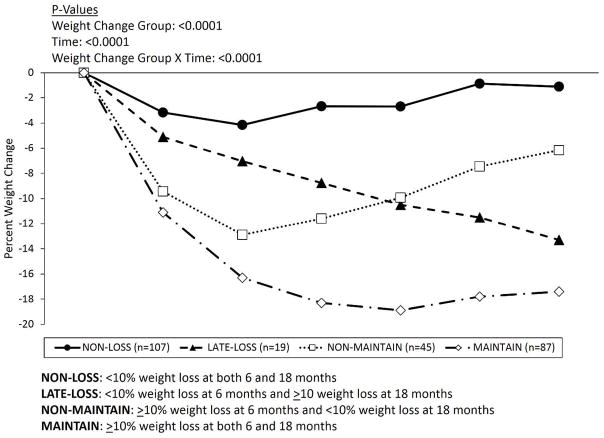
Participants were also grouped on the magnitude of percent weight change that was achieved at both 6 and 18 months. Weight loss of 10% has been recommended as an important clinical target.(2) Therefore, participants were grouped based on <10% weight loss at both 6 and 18 months (NON-LOSS, N=104), <10% weight loss at 6 months and ≥10 weight loss at 18 months (LATE-LOSS, N=19), ≥10% weight loss at 6 months and <10% weight loss at 18 months (NON-MAINTAIN, N=44), or ≥10% weight loss at both 6 and 18 months (MAINTAIN, N=86). To be placed into the appropriate category, weight data at 0, 6, and 18 months was required, resulting in 258 (71.1%) of the 363 randomized participants being included in the analyses. Demographic characteristics of the 258 participants are presented in Table 1 and closely resemble the demographic characteristics of the randomized sample with complete data at baseline. The pattern of weight change over the 18 month intervention is shown in Table 2 and Figure 3.
Figure 3.
Percent weight loss based on weight loss achieved at 6 and 18 months. 254×190mm (300 × 300 DPI)
The results of the analysis of the physical activity data here was not significantly influenced by randomized treatment group assignment (SBWL vs. STEP) and therefore this was not considered further in these analyses. Physical activity data are presented as MET-min/wk. Comparison of MVPA≥10 showed a significant Group X Time interaction (p<0.0001) (Table 4). Post-hoc analysis with Bonferroni adjustment for multiple comparisons (α=0.008) revealed that MVPA≥10 was significantly greater in MAINTAIN vs. NON-LOSS at 6 months, and in MAINTAIN vs. both NON-LOSS and NON-MAINTAIN at 12 and 18 months. However, there was no significant difference between the groups when MVPA<10 was examined (Table 4).
Table 4.
Change in objectively measured physical activity by weight loss at 6 and 18 months [LS Means (95% confidence interval)].
| Physical Activity Variable |
Group Based On 6-and 18- Month Weight Change* |
Assessment Periods (MET-minutes per Week) | P-Values** | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Baseline | 6 Months | 12 Months | 18 Months | Time | Weight Change Group |
Weight Change Group X Time |
||
|
| ||||||||
| LPA (Bouts ≥1 minute in duration and between 1.5 to <3.0 METS) | NON-LOSS (N=107) | 3043.6 (2626.2, 3491.8) | 2798.4 (2394.0, 3234.4) | 2361.3 A (1976.0, 2781.0) | 2257.0 A (1870.1, 2680.1) | 0.0002 | 0.0326 | 0.0075 |
| LATE-LOSS (N=19) | 2811.6 (2470.4, 3174.9) | 2849.6 (2503.4, 3218.2) | 2498.8 (2170.3, 2850.5) | 2326.0 (2008.1, 2667.3) | ||||
| NON-MAINTAIN (N=45) | 2976.5 (2629.5, 3345.0) | 3006.0 (2654.4, 3379.4) | 2867.4 (2523.2, 3233.7) | 2642.1 (2304.9, 3002.3) | ||||
| MAINTAIN (N=87) | 2806.4 (2548.1, 3077.1) | 3223.5 (2945.9, 3513.5) | 3170.2 A (2892.8, 3460.3) | 3037.4 A (2764.6, 3322.9) | ||||
|
| ||||||||
| MVPA-TOTAL (Bouts ≥1 minute in duration and ≥3.0 METS) | NON-LOSS | 1676.6 (1334.9, 2057.3) | 1504.1 A,B (1176.7, 1871.7) | 1334.8 A (1013.4, 1700.3) | 1281.2 A (958.6, 1650.4) | <0.0001 | 0.0001 | <0.0001 |
| LATE-LOSS | 1382.7 (1120.1, 1673.0) | 2227.1 (1886.6, 2595.8) | 1549.2 (1262.3, 1865.6) | 1394.5 (1122.3, 1696.1) | ||||
| NON-MAINTAIN | 1577.1 (1299.4, 1881.6) | 2212.9 A (1878.1, 2575.0) | 1797.5 (1496.3, 2126.3) | 1654.7 B (1359.0, 1979.4) | ||||
| MAINTAIN | 1423.5 (1221.3, 1641.1) | 2647.7 B (2368.8, 2942.1) | 2272.1 A (2011.8, 2548.1) | 2275.1 A,B (2013.5, 2552.7) | ||||
|
| ||||||||
| MVPA<10 (Bouts 1 to <10 minutes in duration and ≥3.0 METS) | NON-LOSS | 1123.5 (939.1, 1324.6) | 1011.0 (833.9, 1205.2) | 930.7 (753.4, 1126.6) | 903.0 (723.9, 1101.9) | 0.0037 | 0.4512 | 0.0393 |
| LATE-LOSS | 986.9 (840.3, 1145.1) | 1168.3 (1006.9, 1341.8) | 914.0 (769.3, 1071.3) | 872.2 (730.6, 1026.4) | ||||
| NON-MAINTAIN | 1137.7 (982.1, 1304.8) | 1134.9 (978.0, 1303.5) | 1068.1 (915.6, 1232.4) | 1014.0 (861.9, 1178.5) | ||||
| MAINTAIN | 979.5 (869.1, 1096.5) | 1148.7 (1028.7, 1275.2) | 1069.4 (952.7, 1192.9) | 1091.7 (973.2, 1217.0) | ||||
|
| ||||||||
| MVPA≥10 (Bouts ≥10 minutes in duration and ≥3.0 METS) | NON-LOSS | 491.6 (297.5, 734.2) | 413.9 A (238.0, 638.1) | 321.4 A (162.8, 533.3) | 300.5 A (144.8, 512.3) | <0.0001 | <0.0001 | <0.0001 |
| LATE-LOSS | 291.1 (170.9, 443.1) | 946.8 (714.5, 1211.7) | 522.3 (350.5, 728.2) | 419.1 (267.0, 605.5) | ||||
| NON-MAINTAIN | 312.4 (189.0, 466.7) | 932.6 (705.6, 1191.3) | 607.9 B (427.2, 820.3) | 533.1 B (360.5, 739.3) | ||||
| MAINTAIN | 320.5 (222.8, 435.8) | 1414.6 A (1199.4, 1647.6) | 1062.9 A,B (875.6, 1268.3) | 1073.0 A,B (883.9, 1280.3) | ||||
indicates no significant difference between randomized groups (data not presented)
Note: Groups with the same superscript at the same assessment point are significantly different at α<0.008 (p-value of 0.05 adjusted using Bonferroni adjustment for 6 group comparisons at that time point.)
Groups
NON-LOSS: <10% weight loss at both 6 and 18 months
NON-MAINTAIN: ≥10% weight loss at 6 months and <10% weight loss at 18 months
LATE-LOSS: 6 month weight loss <10% & 18 month weight loss ≥10%
MAINTAIN: ≥10% weight loss at both 6 and 18 months
Total volume of LPA (MET-min/wk) showed a significant Group X Time interaction (p=0.0075) (Table 4). Post-hoc analysis with Bonferroni adjustment for multiple comparisons (α=0.008) revealed that for LPA was significantly greater in MAINTAIN compared to NON-LOSS at 12 months and 18 months.
DISCUSSION
Physical activity is associated with improved weight loss and the maintenance of weight loss.(3) However, the majority of the findings that support this association are based on self-reported physical activity. It is important to confirm that findings from self-report provide an accurate representation of the amount of physical activity that is associated with weight loss. The findings from the current study are based on objectively measured physical activity using a validated wearable monitor, which may provide valuable insight regarding the dose, duration, and intensity of physical activity that is associated with long-term weight loss.
When participants were grouped based on weight loss achieved at 18 months (GAIN, WL<5%, WL<10%, WL≥10%), MVPA-TOTAL was significantly greater in WL≥10% compared to all other categories (GAIN, WL<5%, and WL<10%) (Table 3). However, it appears that the difference in MVPA is a result of WL≥10% engaging in more MVPA≥10 at 6, 12, and 18 months when compared to those participants achieving less magnitudes of weight loss, and not a result of differences in MVPA<10. This is an important finding because public health recommendation for physical activity recommend the engagement in bouts of MVPA that are at least 10 minutes in duration, and these findings appear to support this recommendation for weight loss.
Brisk walking, or activities similar in intensity, were recommended as the form of physical activity within this weight loss intervention. Assuming an intensity of 4.5 METS, which reflects brisk walking, the minutes of weekly MVPA≥10 in WL≥10% at 6, 12, and 18 months would be approximately 337, 257, and 260 minutes per week, respectively. Similar magnitudes of MVPA≥10 were observed for individuals who lost ≥10% of their initial weight at 6 months and sustained this magnitude of weight loss at 18 months (MAINTAIN), with the duration of MVPA≥10 being 314.4, 236.2, and 238.4 minutes per week at 6, 12, and 18 months respectively. These durations of MVPA are comparable to the 200 to 300 minutes per week of physical activity recommended to enhance long-term weight loss and to minimize weight regain.(3) These recommendations based primarily on studies that relied on self-reported physical activity are largely confirmed by the results of this study using an objective physical activity monitor.
Limited studies have used objectively measured physical activity to examine the association with long-term weight loss,(4, 9) and there are limitations to these studies. Schoeller et al.(9) recruited patients after they had lost >12 kg, and used physical activity measured with doubly-labeled water to predict weight regain over the subsequent 12 months. Catenacci et al.(4) used accelerometry in a cross-sectional design to compare physical activity in a subsample of successful weight losers to both normal weight and overweight control participants. By comparison, the current study measured physical activity objectively at 6 month intervals throughout the entire 18 month intervention, which provides greater detail regarding the dose, duration, and intensity of physical activity in individuals achieving different magnitudes of weight loss within a behavioral weight loss intervention.
Objective measurement of physical activity also allowed for the examination of LPA, which has received little attention within the scientific literature on long-term weight loss. Individuals achieving the greatest weight loss (Table 3) or maintaining significant weight loss (Table 4) were participating in a greater amount of LPA compared to individuals less successful at long-term weight loss. This is an important contribution and may suggest that the combination of increasing both MVPA≥10 and LPA contribute to long-term weight loss success, and the role of LPA warrants further investigation.
MVPA≥10 and LPA may both contribute to increase energy expenditure, which facilitates energy balance and body weight regulation. However, there may be additional metabolic and physiological pathways by which the dose, duration, and intensity of physical activity shown to be associated with long-term weight loss success in this study contribute to the regulation of energy balance and body weight. These may include influences of physical activity on energy intake and eating behavior, fat metabolism, and other hormonal or physiological processes, and these warrant further investigation.
The intervention in this study also included recommendations for reducing energy intake, and therefore physical activity was not solely responsible for the weight loss observed in this study. However, the interaction between physical activity and energy intake can be complex. For example, that greater engagement in physical activity is not necessarily associated with improved compliance to reduced energy intake.(20, 21) It has also been shown that physical activity is associated with a reduction in energy intake in some individuals and with an increase in others.(22) The complex interaction between physical activity and energy intake warrants further investigation.
This study did show that a comprehensive behavioral weight loss program can elicit significant long-term weight loss, and the magnitude of weight loss achieved is comparable to what is achieved with other medical-based clinical interventions. For example, individuals classified as WL≥10 or MAINTAIN achieved 18 month weight loss of 16.6±0.5% and 17.4±0.5%, respectively (Table 2, Figure 2, Figure 3). This study also showed that 130 of the 253 participants lost ≥10% of initial body weight at 6 months; however, 44 of the 130 participants (33.8%) were unable to maintain ≥10% weight loss at 18 months (Table 2, Figure 3), and lower levels of physical activity may have contributed to this weight regain (Table 4). Few participants (7.5%) who did not achieve a 10% weight loss at 6 months were ever able to achieve this magnitude of weight loss at 18 months (LATE-LOSS), suggesting that it is unlikely that most individuals who initially do not respond favorably to a behavioral weight loss intervention will ultimately observe longer-term success in such a program. This may have important implications for the clinical management of overweight and obesity. Moreover, the small sample defined as LATE-LOSS may have reduced the statistical power to detect difference in physical activity between this weight loss pattern and other weight loss patterns (GAIN, NON-MAINTAIN, MAINTAIN).
This study is not without limitations. While prospective data were used to examine the dose, duration, and intensity of physical activity and weight loss, participants were grouped in a post-hoc manner based on weight loss achieved in the intervention. This may result in selection bias and additional confounding factors that could influence the findings reported. Moreover, the majority of study participants were female (82.6%), which prohibited analysis to determine if these findings were consistent between males and females. This study included adults 18 to 55 years of age with BMI between 25 to <40 kg/m2, and therefore is it unclear whether these findings would apply to older adults or individuals at higher levels of obesity. Objective measurement of physical activity also occurred for 1 week at 0, 6, 12, and 18 months, which does not provide a comprehensive perspective of physical activity across the entire 18 month period. It is possible that physical activity may have differed during this assessment period compared to normal physical activity behavior; however, we have previously shown that activity does not differ during weeks when participants wear an activity monitor compared to weeks where they do not wear an activity monitor.(11)
The results provided objective information on the dose, duration, and intensity of physical activity that is associated with successful long-term weight loss. These findings appear to confirm clinical recommendations for MVPA≥10 that have been based mostly on self-reported physical activity. The findings suggest that LPA may also contribute to successful long-term weight loss when combined with appropriate amounts of MVPA≥10. While the pathways and mechanisms by which the dose, duration, and intensity of physical activity influence weight loss and body weight regulation within the context of behavioral weight loss interventions require further study, promoting the adoption and maintenance of 200 to 300 minutes per week of MVPA≥10 and encouraging engagement in increased amounts of LPA may improve long-term weight loss in adults.
Figure 1.
Consort Diagram
What is already known about this subject
Physical activity has been recommended as an important lifestyle behavior to enhance long-term weight loss and to maintain weight loss.
Clinical guidelines, in general, recommend 200–300 minutes per week of moderate-to-vigorous intensity physical activity within the context of a comprehensive weight management program.
What this study adds
Clinical guidelines for the dose of moderate-to-vigorous physical activity (≥3.0 METs) to promote long-term weight loss are based primarily on self-report. This study included objective assessment of physical activity to quantify the dose of moderate-to-vigorous physical activity that is associated with improved long-term weight loss outcomes.
Little is known about the pattern of moderate-to-vigorous physical activity. The results of this study show that moderate-to-vigorous physical activity performed in bouts of ≥10 minutes are predictive of improved weight loss outcomes, whereas bouts <10 minutes are not predictive of weight loss outcomes. These findings have important implications for the promotion of moderate-to-vigorous physical activity for the purpose of improved weight loss.
Little is known about the importance of light intensity physical activity (1.5 to <3.0 METs) to long-term weight loss. This study objectively measured light intensity physical activity and found that participants with greater weight loss at 18 months engaged in more light intensity physical activity than participants with less weight loss. These findings have important implications for the promotion of light intensity physical activity, in addition to moderate-to-vigorous physical activity, for the purpose of improved weight loss.
Acknowledgments
We recognize the contribution of the Physical Activity and Weight Management Research Center at the University of Pittsburgh, the UNC Weight Research Program at the University of North Carolina at Chapel Hill, and the Department of Biostatistical Sciences at Wake Forest University.
Funding: Supported provided by grant HL084400 from the National Institutes of Health.
Footnotes
Clinical Trials Registration: clinicaltrials.gov NCT00714168
Conflicts of Interest: Dr. Jakicic received an honorarium for a scientific presentation from Kaiser Permanente, and was the Principal Investigator on grants awarded to the University of Pittsburgh by BodyMedia, Inc. Dr. Tate was a consultant to Weight Watchers, the Department of Veterans Affairs, and VioCare, and received an honorarium from MD Anderson Cancer Center.
Author Contributions:
Conception and design: JMJ, DFT, WL, KKD, ADR; Data acquisition: JMJ, DFT, KKD, KP, KE; Data analysis and interpretation: JMJ, DFT, WL, RHN; Drafting manuscript or critical revision: JMJ, DFT, WL, KKD, KP, RHN, ADR, KE; Obtaining funding: JMJ, DFT, WL; Administrative, technical, and material support: JMJ, DFT, KKD, ADR, KE; Supervision: JMJ, DFT
List of References
- 1.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and The Obesity Society. Circulation. 2013 [Google Scholar]
- 2.National Institutes of Health National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults -The Evidence Report. Obes Res. 1998;6(suppl 2) [PubMed] [Google Scholar]
- 3.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. ACSM position stand on appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;42:459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 4.Catenacci VA, Grunwald GK, Ingebrigtsen JP, Jakicic JM, McDermott MD, Phelan S, et al. Physical activity patterns using accelerometry in the National Weight Control Registry. Obesity. 2011;19:1163–1170. doi: 10.1038/oby.2010.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss in overweight women. Arch Int Med. 2008;168:1550–1559. doi: 10.1001/archinte.168.14.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. Journal of the American Medical Association. 1999;282:1554–1560. doi: 10.1001/jama.282.16.1554. [DOI] [PubMed] [Google Scholar]
- 7.Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: Does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–689. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 8.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. American Journal of Clinical Nutrition. 1997;66:239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 9.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women. American Journal of Clinical Nutrition. 1997;66:551–556. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 10.Tate DF, Jeffery RW, Sherwood NE, Wing RR. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? Am J Clin Nutr. 2007;85:954–959. doi: 10.1093/ajcn/85.4.954. [DOI] [PubMed] [Google Scholar]
- 11.Jakicic JM, Polley BA, Wing RR. Accuracy of self-reported exercise and the relationship with weight loss in overweight women. Med Sci Sports Exerc. 1998;30:634–638. doi: 10.1097/00005768-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 12.Litchman SW, Pisarska K, Berman ER, Pestone M, Dowling H, Offenbacher E, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327:1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 13.Jakicic JM, Tate D, Davis KK, Polzien K, Rickman AD, Erickson K, et al. Effect of a stepped-care intervention approach on weight loss in adults: The Step-Up Study Randomized Trial. JAMA. 2012;307:2617–2626. doi: 10.1001/jama.2012.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jakicic JM, Marcus MD, Gallagher KI, Randall C, Thomas E, Goss FL, et al. Evaluation of the SenseWear Pro Armband ™ to assess energy expenditure during exercise. Med Sci Sports Exerc. 2004;36:897–904. doi: 10.1249/01.mss.0000126805.32659.43. [DOI] [PubMed] [Google Scholar]
- 15.St-Onge M, Mignault D, Allison DB, Rabasa-Lhoret R. Evaluation of a portable device to measure daily energy expenditure in free-living adults. Am J Clin Nutr. 2007;85:742–749. doi: 10.1093/ajcn/85.3.742. [DOI] [PubMed] [Google Scholar]
- 16.Masse LC, Fuemmeler BF, Anderson CB, Matthews CE, Trost SG, Catellier DJ, et al. Accelerometer data reduction: a comparison of four reduction algorithms on select outcome variables. Med Sci Sports Exerc. 2005;37:S544–S554. doi: 10.1249/01.mss.0000185674.09066.8a. [DOI] [PubMed] [Google Scholar]
- 17.Miller GD, Jakicic JM, Rejeski WJ, Whitt-Glover M, Lang W, Walkup MP, et al. Effect of varying accelerometry criteria on physical activity: the Look AHEAD Study. Obesity. 2013;21:32–44. doi: 10.1038/oby.2012.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes. 1992;16:397–415. [PubMed] [Google Scholar]
- 19.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. International Journal of Obesity. 2006;30:391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 20.Jakicic JM, Wing RR, Winters-Hart C. Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc. 2002;34:1653–1659. doi: 10.1097/00005768-200210000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Unick JL, Jakicic JM, Marcus BH. Contribution of behavior intervention components to 24 month weight loss. Med Sci Sports Exerc. 2010;42:745–753. doi: 10.1249/MSS.0b013e3181bd1a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Unick JL, Otto AD, Helsel D, Dutton C, Goodpaster BH, Jakicic JM. The acute effect of exercise on energy intake in overweight/obese women. Appetite. 2010;55:413–419. doi: 10.1016/j.appet.2010.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]