Abstract
Poverty increases maternal stress by heightening exposure to negative life events, job loss, chronic strains, poor housing, dangerous neighborhoods, and conflict with partners, culminating in crippling depressive symptoms, the most prevalent mental health threat. Depressive symptoms interfere with the provision of the strong maternal support needed to counter the hardships of poverty, thus placing infants and toddlers at risk for delayed language, social, and emotional development. Initial clinical trials in high-risk mothers have shown promise, and successive tests of interventions will be strengthened if mothers who have mental health risks can be accurately targeted for inclusion. This article reports on a sequential, data-driven process by which high-risk mothers were targeted for intervention in two trials currently in progress to reduce depressive symptoms. An iterative process of using data to identify at-risk mothers and validate the presence of risk factors helped hone the recruitment and design of the intervention trials. This report also offers guidance for further study.
Keywords: mothers, depression, poverty, low income, infants/toddlers, targeting, intervention trials
Introduction
Currently, 18% of America’s children are growing up in poverty amidst widespread conspicuous wealth. Half of these children live in families where the annual income is less than $10,000,a while 19 million U.S. citizens live in extreme poverty (incomes below 50% of the poverty threshold), the highest percentage since 1993.1 The overall poverty rate in the United States of 12.6% has increased steadily since 2000, as has the proportion of people living in extreme poverty (a 1.1% rise since 2000). Percentages are misleading, however, because what appears to be a small increase represents an additional 5.4 million more people and 1.3 million more children living in poverty.2 The picture is further clouded by the 40-year-old computations used to establish “poverty” (U.S. Department of Health and Human Services 2006) that “mask the reality [in today’s economy] that families with incomes up to twice that associated with poverty status … face difficulties … including food insecurity, residential instability and lack of medical insurance”(p. 71).3 These families live “one or two crises away from official poverty”(p. 2).4 If these at-risk families are added to those who meet “official” poverty guidelines, 39% of America’s children are growing up poor and suffering multiple risks to their physical, cognitive, and social development.
For the U.S. population, the burden of poverty falls heavily on mothers who are the head of household, and often, sole wage earner for the family. Female-headed households are highly vulnerable to the rise in poverty, with 42% of female-headed households now living in poverty.2 The number of children living in female-headed poverty households is the highest since 1998 and, in comparison with five other Western industrialized countries, the economic conditions for U.S. female-headed households have been found to be significantly worse.5 In the context of poverty, any potential that a child has to grow up healthy rests with the health and mental health of the parent and, in light of the demographics of poverty, the mother. A mentally healthy mother supplies the security, stimulation, and behavioral guidance needed by the infant and toddler to develop appropriate language, motor, and social skills. To take on the problem of maternal mental health in poverty can seem too difficult until the consequences for the child are considered. Recent evidence has shown that as little as 6 months of exposure to maternal depression can create negative changes in the affect and behavior of infants and toddlers,6 and 3 months’ remission in maternal depression has significantly reduced child anxiety, disruptive behavior, and depression.7 These stunning figures beg us to intervene swiftly and effectively with our most at-risk mothers on behalf of the generation of children currently living in poverty.
How do we design and test interventions that will work for these mothers? In this report, we explore the initial step—“targeting” low-income mothers whose mental health is in jeopardy and who are likely to respond to an intervention. We will begin with a review of what we know about how poverty threatens maternal mental health and then focus on serious depressive symptoms, the most common mental health threat in these mothers. We will review the work on the effect of maternal depressive symptoms on the youngest children—infants and toddlers—and some examples of how mental health interventions to support mothers rearing their children in poverty have been implemented and tested. Given the questions we have raised about how poverty is defined in today’s economy, we will include studies of low-income mothers (above the poverty threshold) as well. We will argue that data on sound interventions are limited and that with evidence-supported targeting methods we can improve the accuracy of intervention trials and improve the human developmental potential of symptomatic mothers and their at-risk children. Throughout, we will use our current experiences and data from a cumulative program of mental health intervention directed toward two different populations of mothers living in poverty with depressive symptomsb to illustrate how we have successfully targeted them for testing an in-home intervention to relieve their depressive symptoms. Finally, we will conclude with recommendations on how targeting interventions can be applied to future research with mothers in poverty.
Significance of Maternal Mental Health in Poverty
Poverty increases maternal stress by heightening exposure to negative life events, job loss, chronic strains, poor housing, dangerous neighborhoods, and conflict with partners, culminating in crippling depressive symptoms.8–13 Single mothers without supporting networks are especially vulnerable to the everyday stressors of poverty as well as being exposed to adverse events characterized by loss, danger, humiliation, and entrapment that increase the likelihood of depressive symptoms.14,15
Depressive symptoms and close partner conflict are two routes through which poverty diminishes investments in children and increases the development of negative child behaviors.8,16,17 Of the two factors, depressive symptoms clearly diminish maternal sensitivity and nurturing, and they increase the use of punitive, inconsistent, and ineffective parenting that is correlated with child aggression and behavioral problems.17,18
Help from close supporters buffers the effect of adverse events and shields children from the negative effects of harsh parenting, but by necessitating living in dangerous, run-down neighborhoods, poverty reduces mothers’ opportunities to access good-quality support.19,20 The reversal of these relationships was demonstrated in a dramatic natural experiment where the opening of a southeastern mountain casino created a sudden upswing for longtime poverty-dwelling families. Within 4 years, relief of severe financial stress was accompanied by a reduction in stress, greater parental investment and competence, and a decrease in child conduct disorders.21
Is poverty so powerful that it is impossible for mothers to be mentally healthy? For sure, economic constraints have such a strong effect on parenting that it is difficult to imagine that any mother living in poverty can exert the strong, consistent parenting needed to support optimal child development. Yet there is evidence that mentally healthy mothers can and do shield children from poverty-related stressors, losses, and stigma through watchful protection, provision of compensatory resources, and investment in the child through advocacy and emotional presence.22–27 For any child to thrive, the mother needs all the qualities of mental health—accurate perception, logical thought processes, appropriate emotional responses, adequate energy for action and maintenance of consistent relationships with the child and significant others, containment of stressors, skills in maintaining role functions, and pursuit of personal growth and development.28,29
Healthy, strong mothers provide a safe, nurturing home environment; developmental support; and, for the child in poverty, gain access to compensatory child enrichment resources such as U.S. government–funded Early Head Start (EHS; 0- to 3-year-olds) and Head Start (4- to 5-year-olds programs).9,19,23,27,30–32 These resources shield the child from being damaged by deficient housing, substandard schools, dangerous neighborhoods, and negative role models.23,33–40 Ultimately, it is possible that an organized, sensitive mother can produce a resilient child who realizes his or her full potential.22,34,38,41,42 Hence, interventions to support mothers and reduce threats to their mental health can yield substantial benefits to their children as well.43
Depressive Symptoms in Low-income Mothers
The most common threat to the mental health of mothers in poverty is depressive symptoms, or depression. The prevalence is high—40%–59%44–46—four times the percentage documented in middle-income mothers. Depressive symptoms may well be generated by the intense stressors that accompany a life in poverty—low education, hourly work, multiple losses, and exposure to trauma and violence—as well as affect mothers’ ability to use available resources, such as educational support to escape poverty.23,47–49 The term “depressive symptoms” describes changes in thinking, feeling, motivation, and body functions that accompany a consistently sad mood. These changes may differ in severity and duration from major depressive episode (MDE), which is a severe, distinct syndrome characterized by persistent sad mood, loss of pleasure in most things, and other specific diagnostic symptoms.50 The two phenomena are related, however, because within a year, 25% of individuals with depressive symptoms progress to MDE.51
Even at moderate levels, depressive symptoms in the mothers of infants or toddlers have as strong an effect on the development of low-income infants/toddlers as the limited home environment, family pressures, and poor neighborhoods associated with economic disadvantage.52 In part, that is because depressive symptoms rob the mother of energy, focus, and patience for mothering.53 Depressive symptoms further impair mothering by slowing the mother’s response or by provoking intrusive responses that do not match the infant’s or toddler’s cues.54 Overall, symptomatic mothers have shorter, less frequent interactions with the child, talk less often with their children, play less,62 and express less joy and positive affect.55–58 These interactions fail to foster learning and behavioral regulation in the infant and toddler.59
Infants of symptomatic mothers vocalize less, are more irritable, and play and explore less than infants of nondepressed mothers.60,61 If the mother’s depressive symptoms persist longer than 6 months, poor developmental outcomes and distinct behavioral dysregulation in their infants is observed.62 Also, because the infant-directed speech of symptomatic mothers lacks the qualities that facilitate associative learning, their infants lag in performance on standardized language.60 The language lags associated with maternal depressive symptoms are devastating when added to the negative effect that poverty alone has on language acquisition. By third grade, children reared in poverty have a vocabulary of 4000 words, compared with 12,000 words in the middle-class child.63 With less maternal stimulation, children of symptomatic mothers living in poverty lag even farther behind.59 Infants of mothers with depressive symptoms also fall behind on mental development scales, and their deficits persist into the toddler era.64 Toddlers of symptomatic mothers demonstrate less social interaction, more behavior problems, and more negative affect toward themselves.65–68 For many children in poverty, their only parent is the mother. These children are highly dependent on a mother’s attentiveness and sensitivity, making the effect of depressive symptoms even greater than that of a child in a two-parent or extended kin family.
The factors that contribute to the development of depressive symptoms in low-income mothers also make it difficult for mothers to use traditional mental health treatment. In a recent study of barriers that prevented mothers from seeking treatment, mothers “normalized” their anxiety and depression as reasonable to them because of their extreme life issues and the pressure of “living at the edge” of crisis provoked by poverty.69 Cumulative shortages in work, income, transportation, social support, insurance, and sick leave all added up to keeping their lives in a precarious balance. The mothers participating in the Anderson et al.69 study had little belief that treatment could help them with these overwhelming problems. Also, they had partnered with abusive men for various reasons and worried that if they sought formal treatment, their partners would use it against them. Moreover, the participants were mothers of children who had been referred to treatment for conduct or other behavioral issues; hence, mothers struggled with children who had extremely difficult behavioral issues. The mothers’ belief that they had caused these problems propelled them to put their needs last out of guilt.
Throughout the Anderson et al.69 study, the theme of losing their children if they allowed themselves to be formally diagnosed and accepted treatment was a palpable fear. The overriding theme, however, was the difficulty mothers had of engaging in treatment in the midst of an uncertain, survival-focused life—themes that have remained the same for 23 years.44,70 This focus on survival may explain why, despite the prevalence of depressive symptoms in mothers in poverty, only limited trials that have specifically targeted them have been performed. Several trials of interventions focusing on maternal depressive symptoms have included low-income mothers, and a few trials of parenting effectiveness programs have added mental health components in an attempt to reach symptomatic mothers.
Tests of Interventions to Reduce Maternal Depressive Symptoms
Clinic-based trials of psychotherapies for maternal depression or depressive symptoms have been effective in short-term reduction of maternal depression and parenting stress.71,72 Overall, however, trials of programs to reduce maternal depressive symptoms alone without specific intervention to change mothers’ interactions with their children have shown limited effect on cognitive functioning or behavioral problems in the child over time.73 The absence of a long-term effect may be related to attrition, an insufficiently strong or sustained intervention, or a lack of emphasis on improving mother–child interactions. Few low-income mothers were included in these trials, and few clinic-based trials specifically targeting these mothers for these therapies have been completed.74
Trials of home-based psychotherapy have focused on maternal postpartum depression. Home-based intervention is a promising approach to reduce the problems of transportation and child care that wreck havoc with scheduled clinic-based mental health care in poverty-dwelling mothers. Several British and Swedish trials of in-home intervention showed effectiveness,75–78 but only one of these trials included low-income mothers.77 Unfortunately, the trial used non–mental health interventionists and a general counseling approach that was not specific to depression or mental health concerns. One of two studies that used a tested psychotherapy for depression compared cognitive behavioral therapy (CBT) delivered by non–mental health specialists to fluoxetine, a common antidepressant.75 Despite having non–mental health interventionists, CBT was effective. This study, however, was limited by the high refusal rate of mothers who were reluctant to take medication and by the high dropout rate in the most intense treatment group (CBT plus medication). Another study using CBT by a trained therapist also had a high dropout rate between screening and admission. This outcome suggests that difficult-to-reach mothers did not receive the intervention.76 Despite these limitations, both studies found reductions in depressive symptoms by using short-term interventions delivered in a home-based model. However, because low-income mothers were not specifically targeted, we lack data about the effect over time and the effect of these programs on child development and behavior in these high-risk mothers.
Tests of Interventions to Enhance Parent Training Programs
A second approach, adding mental health intervention to parent effectiveness training programs, has targeted low-income mothers directly. These programs were developed to change the aggressive, oppositional, and noncompliant behaviors in children that interfered with their classroom success. Such behaviors have been linked to difficulties throughout the child’s life and failure to achieve a full range of adult behaviors.79 Stressors accompanying poverty have been correlated with higher parental reactivity and physical punishment. This finding leads researchers to reason that helping parents to become more aware of their own emotional reactions and to increase their repertoire of effective disciplinary strategies would reduce punitive parenting.80 Evaluation of large trials of a well-tested program (e.g., the Incredible Years) in low-income Head Start children indicated that increasing parenting capability reduced child conduct problems at home as well as in the classroom and found that levels and duration of maternal participation were associated with positive child outcomes.81,82 Depressive symptoms did reduce maternal engagement in the program, but overall, symptomatic mothers did as well as, or in some instances better than, nonsymptomatic mothers. Such success was important because symptomatic mothers had poorer parenting skills at the beginning of the program.82 A recent meta-analysis of two decades of research on parent training showed consistent positive outcomes with families in poverty. Depressive symptoms posed the greatest threat to the success of parent training interventions.83 The authors concluded that the success of parent training programs rests on the mother’s motivation to attend and consistently apply the techniques that are taught. Maternal depressive symptoms work against these requirements, a problem noted in EHS program data that show a high (50%) dropout rate of children whose mothers have significant depressive symptom severity.84
Because maternal depressive symptoms work against program engagement and in favor of inconsistent, harsh parenting behaviors, the addition of counseling to parent training programs have been tested, with mixed results. Some researchers found that the addition of stress-reduction training to parent training did not improve child outcomes.85,86 In contrast, others found modest improvements with the addition of counseling to reduce interpersonal conflict and enhance support in single parents.87,88 In their 20-year meta-analysis, Reyno and McGrath conclude that when parent effectiveness training is used with low-income populations, mental health enhancements “addressing parental distress and mental health concerns may positively influence treatment outcomes” (p. 107) and potentially create a recursive effect by reducing depressive symptoms as an outcome of increased parental self-efficacy.83 Taylor and Biglan proposed that, especially for single parents, assistance in coping with nonparenting stressors reduces pressure and helps parents address issues with their children’s behaviors.89 Other benefits included the reduction of stigma by including mental health intervention into a strength-based, non–mental health program.
There are several important messages in these trials. First, attempts to bring depressive symptom interventions to mothers in clinics or at home have shown promise but have only minimally targeted low-income mothers. Second, enhancements to parenting efficacy programs have yielded initial positive results. However, these approaches have not specifically targeted mothers with depressive symptoms, the most common mental health threat. For the latter approach, program retention has been correlated with positive results. Moreover, data predict that maternal depressive symptoms, if not addressed, work against the mother remaining in the program and achieving the positive outcomes.
To advance this work further, a more targeted approach to including low-income mothers in clinical trials of interventions is needed. The next section will discuss the methods of targeting and verification that we used to determine that we were reaching mothers who might be ready to engage in an intervention.
Targeting Mothers in Need of Mental Health Intervention
Two Intervention Studies
The data used to illustrate targeting were generated in two randomized trials of an in-home, interpersonally based intervention with two populations of poverty-dwelling mothers—recently immigrated, Spanish-speaking Latina mothers and English-speaking mothers. Both groups of mothers had U.S.-born infants and toddlers enrolled in EHS. The research was funded through two U.S. government grantsc in partnership with six EHS programs in a southeastern state and a seventh one in a northeastern state. A third grant funded the addition of non-depressed Latina mothers for comparison purposes.d The relationship-based intervention, a modification of interpersonal therapy, was delivered by master’s degree–prepared psychiatric mental health nurses in 11 face-to-face sessions and five booster sessions over a 5-month period. The intervention was customized to each mother but standardized through content organizers devoted to (1) managing depressive symptoms, (2) confronting difficult life issues, (3) identifying and using effective social support, (4) improving parenting interactions, and (5) developing anticipatory strategies for recurrence of symptoms. Additional content for fathers and intimate partners was added when appropriate. The intervention was delivered to the Spanish-speaking Latina mothers by an English-speaking nurse and a specially trained lay interpreter working in partnership with the mother. At four points, data were collected on maternal, child, and family demographics; maternal depressive symptoms; Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-R) diagnosis of MDE (English-speaking mothers only); maternal self-efficacy; and maternal and child behaviors. Mother–child interactions were also observed and coded from 45-min unstructured, in-home videotapes.
Targeting the Intervention
Targeting an intervention is the systematic process through which a specific population is chosen to receive an intervention.90 Knowing beforehand that the targeted individuals are likely to have a specific condition and respond favorably to an intervention for the condition increases the likelihood that a randomized trial will yield a valid test that can be replicated. Specifically, data from the population should show that (1) a known percentage of the population members have the particular condition, (2) the chosen condition is detectable through screening, (3) the condition causes a specific outcome, (4) the outcome is associated with risk for the population, and (5) the relationship between the condition and the outcome can be altered.91 Contextual factors, such as access to the population, their receptivity and readiness for the intervention, and the presence of enabling relationships that broker the intervention to potential recipients can facilitate an intervention’s success. Thus, they are important to consider in determining what population to target. Targeting a population with the known condition and the risk factors and characteristics that favor retention decreases heterogeneity and increases the likelihood of a detectable effect size between intervention and control participants.92
Supporting the Five Dimensions
As we considered our populations of low-income mothers of infants and toddlers (newly immigrated, Spanish-speaking Latina mothers and low-income, English-speaking mothers), we used findings from the existing literature and our own direct evidence to verify the five dimensions. As noted earlier, the linkages among poverty, stressors, maternal depressive symptoms, and negative child outcomes were well established by studies of mothers living in poverty. Considering both the presence of an MDE and depressive symptoms, Hammen’s study yielded two findings relevant to targeting an intervention for maternal depression.53 First, the severity of the current depressive symptoms of mothers, not whether the mother had been formally diagnosed with depression, was associated with impaired interactions with their children. Second, children of mothers with elevated depressive symptoms showed greater negative outcomes than did children of mothers who had a formal diagnosis of depression but whose symptoms were in remission. Hammen concluded that regardless of the diagnostic status of the mother, the current severity of depressive symptoms was the most critical to mother–child interactions and child outcomes. Other researchers had established that the presence of symptoms limited function even when not severe enough for a clinical diagnosis.50
These findings suggested that intervention would be justified in mothers who had significant symptom severity but who had not met the diagnostic criteria for MDE. We knew that there was a high likelihood of finding low-income mothers with significant symptom severity and reasoned that an intervention that included all symptomatic mothers would reach the most at-risk children. If all mothers scoring above the cut-point were included, mothers with the most severe symptoms and probable MDE would be identified as well. From a practical standpoint, it was unlikely that low-income mothers would have access to clinicians and unlikely that they could afford treatment. Offering a focused intervention in a destigmatized way by embedding it in EHS services seemed arguably the best way to reach these mothers and their infants and toddlers. Finally, the evidence that chronicity of maternal depressive symptoms and reduced maternal sensitivity were associated with negative child outcomes supported the decision to focus the intervention on limiting symptoms, increasing maternal sensitivity, and helping mothers provide appropriate developmental support to their infants or toddlers.
Designing the Study to Enhance Recruitment of Targeted Mothers
On the basis of evidence that mothers in poverty underuse mental health resources, we knew that there were barriers to gaining access to mothers.69 Therefore, we established a partnership with EHS, a federal enrichment program for infants and toddlers growing up in poverty. EHS already targets mothers living in poverty and provides them with child care, parent effectiveness training, and social services. The last dimension was important because we could not focus on the mental health needs of mothers unless they had help meeting housing, food, health care, and children’s schooling needs. EHS requires a long application process including documentation of income and commitment by the mother to goals for herself and her family. The success of a mother in enrolling her child signaled a level of investment in the child and readiness for personal change that would maximize the acceptance of an intervention for depressive symptoms. The EHS staff believed that the project would help them meet federal performance standards requiring programs to support the mental health needs of their enrolled families. Finally, an important factor was that of stigma. By aligning with EHS, we could offer mental health care to mothers as part of a less-stigmatizing service and in a more confidential manner.
We conducted focus groups to gain more detailed information directly from mothers. Initially, we conducted four focus groups with a total of 25 English-speaking mothers of various ethnic backgrounds and ages. It was important to include mothers from all ethnic groups served by EHS to discover whether there was a common core of depressive symptoms and whether there were differences in acceptability and expression among mothers of different ethnic groups. Mothers confirmed that they were aware of the full spectrum of depressive symptoms and that these symptoms severely hampered their functioning. They felt emotionally isolated and physically unable to leave their homes. Moreover, their sadness, lethargy, and discomfort around others kept them from talking to EHS staff or using EHS parent resources. Although all of them were aware that something was wrong, they did not want to acknowledge it to themselves. Stigma was a factor in their silence. Rural mothers worried that their close-knit communities would find out and think they were “crazy,” whereas suburban mothers feared that seeking formal help might put a negative label on them and increase the isolation they felt already. The African American mothers were outspoken in feeling deep shame and failure about being depressed when they expected themselves to be strong for others. Nonetheless, there was a shared sense among all the mothers that the stigma of living in poverty was a shared adversity that united them, regardless of ethnicity, and made them reluctant to adopt another negative label (e.g., “mentally ill”). As one mother stated, “I’m a high school dropout, an unwed mother, I’m on welfare, and now you want me to say I’m depressed? Please! Not another bad label!” Mothers also reported that the pressure of day-to-day survival needs, changing schedules in their Temporary Aid to Needy Families Act–mandatede hourly jobs, reliance on public transportation, and difficulty in getting someone to watch the children were also barriers to seeking help for themselves. When asked what form an intervention needed to take to be helpful, mothers emphasized that the intervention needed to be confidential, convenient, flexibly scheduled, low profile, and empowering. These concerns led us to design our intervention as an in-home program delivered by nurses in partnership with EHS home-visiting services.
We then tested whether we could access these high-risk mothers by using traditional recruitment methods. We sent explanatory letters with consent forms, brief demographic questionnaires, and a depressive symptom screening questionnaire to every enrolled mother in one EHS program in a midsized northeastern city. We were stunned by the low return rate for screening questionnaires (5%) and an even lower rate for identifying symptomatic mothers (1%). We concluded that we were missing symptomatic mothers and barely saturating the available pool of potential participants. We met with our EHS program partner and developed a new procedure whereby we trained EHS staff to consent and screen mothers directly. The procedure increased the return of screening questionnaires (70%) and identification of mothers scoring above the cutoff of 16 on the Center for Epidemiologic Studies Depression scale (CES-D). The change in procedure was more labor intensive and required more investment of investigator and research staff time. The process, however, brought the research and site teams closer and promoted more dialogue and participation by the site in shaping the research design. Ultimately, the ongoing dialogue and close teamwork between EHS and the projects was essential in recruiting targeted mothers.
When targeting English-speaking mothers, we became aware that many of the U.S.-born infants and toddlers of newly immigrated Latinos were being enrolled in three of the southeastern U.S. sites. Latina EHS staff observed that the mothers of these children were coping with stressors of poverty, trauma, loss, adverse life issues, and rapid acculturation, and these mothers appeared to have depressive symptoms. Also, these mothers were isolated by not being able to speak English and had lost familial social support in the process of immigration. To target the intervention toward Spanish-speaking, newly immigrated Latina mothers, we enlisted the assistance of influential EHS staff who were part of the Latino community. In targeting this population, we first established that the depressive symptoms among Spanish-speaking mothers were similar to symptoms among English-speaking mothers.93 Therefore, we drew from previous work94,95 and instituted a process of decentering to establish that Spanish-speaking mothers were experiencing the depressive symptoms that our intervention was designed to reduce.
Decentering describes a process by which a construct is removed from the social context in which it has evolved.96 The literature described Latinos as presenting their depressive symptoms as somatic changes, such as pain, headaches, and stomach upset, rather than the thought and mood alterations consistent with U.S. diagnostic and symptom measurement devices.101 We were not sure that the construct of “depressive symptoms” was equivalent. Therefore, we brought the issue to the target population who would receive the intervention: Latina mothers, their husbands, and the bilingual community helpers who were working with them.
Sixteen Latina mothers who were identified by their EHS staff as symptomatic were prescreened on the CES-D for significant symptoms and invited to two different focus groups at the EHS program site. Participants in both focus groups were asked to talk about their struggle with depressive symptoms. The group facilitator did not use the term “depression” or refer to mental illness. Mothers used the term “depression” (depresión) and other identifiers—“deep sadness,” “my struggle,” “bad days,” and “sick days.” When given the categories of “thinking,” “feeling,” “actions,” and “body changes” and asked to identify in which of these domains they felt the symptoms most strongly, mothers immediately spoke of how their thinking processes were disrupted by depressive symptoms. They described being distracted, unable to think clearly, “in a cloud,” and unable to plan their work and stay focused on tasks. They readily spoke of changes in their ability to act (being immobilized and unable to leave their bed) and changes in their feelings (anger and irritability, sadness and tearfulness without an obvious reason). They spoke of having great difficulty with their toddlers around issues of setting limits and disciplining. They worried that any disciplinary actions would be seen as being a bad mother and yearned for guidance from older parents living abroad.
The mothers also identified several barriers to seeking help, such as lack of providers; shame about being depressed; fear of deportation; and for several who were familiar with the mental health system in their country, fear of being removed from their family, institutionalized, and being given electroshock therapy against their will. Seeking care for physical ailments and symptoms seemed safer to them, and they “hoped” that the providers would recognize that they were struggling with depressive symptoms. The women who had sought help were quick to say that their depressive symptoms had not been recognized or treated by the U.S. providers. Repetition of these themes in both focus groups affirmed that the mothers were experiencing similar feelings; that stigma, shame, and fear were formidable barriers to care; and that we needed to be sensitive to mothers’ needs for privacy and confidentiality. The mothers readily acknowledged suicidal thoughts and in response to our questions about whether they would acknowledge these symptoms to a U.S. nurse, the mothers adamantly stated that providers needed to ask. They said, “If you don’t, no one will, and we won’t tell you about it unless you ask.” Mothers expressed great respect and trust for nurses and felt that they would try to answer any questions if the nurses asked respectfully.
Finally, the recent emphasis on postpartum depressive symptoms has brought attention to the importance of maternal depression in the child’s first year of life. However, most of the mothers in these initial studies had toddlers. We elected to increase the window and screen mothers of newborns through 40-month-old EHS children. At the recent completion of our intervention study with Latina mothers, the age of children was 15.9 ± 11.5 (mean ± standard deviation) months, well beyond the postpartum period. Our clinical data from the intervention have indicated that the toddler era is stressful for mothers with depressive symptoms, particularly around issues of emotional regulation and discipline. Using the data from our pilot studies was valuable in helping us determine a targeted age of children that would allow us to understand when the symptomatic mothers we sampled were having difficulty.
In a narrower sense, decentering is the process of removing culture-specific idioms and terms that are embedded in the wording of a measurement instrument. This process occurs as an outcome of the translation and back-translation of an instrument from its source language into another language.97 In meeting the five dimensions associated with targeting, we also needed evidence that our screening tool (the CES-D) would correctly identify depressive symptoms in a Latino population. Data on the CES-D in Latinos were reasonably positive, with similar reliability and factor structures in comparative samples of Mexican Americans, blacks, and Anglos.98–100 In our initial evaluation of the CES-D, we ascertained that the translated version that had comparable psychometric data was the one that we chose to use. Some instruments have more than one translated version with variation among them in psychometrics. The comparability of the CES-D has been attributed to the presence of only one somatic depressive symptom item, which may control for overreporting of somatic depressive symptoms by Latino respondents.101 On the basis of these data, we chose the Spanish version as the screening instrument of the CES-D. As in our studies with English-speaking mothers, we anticipated that some mothers would not be literate and so we trained personnel to read the CES-D and other instruments aloud. Data from our current study of Latina mothers have confirmed that doing so was wise. Thirty percent of our sample (
 = 80) had less than 6 years of formal schooling. Some mothers had as little as 3 years of formal schooling.
= 80) had less than 6 years of formal schooling. Some mothers had as little as 3 years of formal schooling.
Verifying That Targeting Had Been Achieved
At an early point in our first intervention study with Spanish-speaking, newly immigrated Mexican mothers, we were able to verify that our approach to targeting was effective in reaching the most at-risk mothers. We hypothesized that if our recruitment methods were reaching the targeted population, data would confirm that poverty and its associated stressors eroded self-efficacy, increased parental conflict and maternal depressive symptoms, and negatively affected mother–child interactions.
We gathered data from 25 asymptomatic mothers and 32 mothers (
 = 57) who scored over the standard cutpoint of 16 on the CES-D. We asked them about demographic characteristics (maternal age and years of education), social support (employment outside the home, no partner at home in the home, moved within the last year), family conflict, and maternal burdens (children’s chronic health, access to transportation, debt, legal difficulties). Using standardized instruments,f we also interviewed them about acculturation, maternal health status, maternal self-efficacy, mother–child interactions, and depressive symptom severity. Table 1 presents descriptive data on the variables.
= 57) who scored over the standard cutpoint of 16 on the CES-D. We asked them about demographic characteristics (maternal age and years of education), social support (employment outside the home, no partner at home in the home, moved within the last year), family conflict, and maternal burdens (children’s chronic health, access to transportation, debt, legal difficulties). Using standardized instruments,f we also interviewed them about acculturation, maternal health status, maternal self-efficacy, mother–child interactions, and depressive symptom severity. Table 1 presents descriptive data on the variables.
TABLE 1.
Sample characteristics (N = 57)
| Variable | Mean or % | SD |
|---|---|---|
| Maternal demographic | ||
| Mother’s age | 27.47 | 5.34 |
| Years of education | 8.79 | 2.78 |
| Works outside home | 26% | |
| Not living with spouse/partner | 9% | |
| Acculturation | ||
| Years in United States | 5.93 | 3.86 |
| No English skills (SASH = 4 of 20) | 67% | |
| Low acculturation to Anglo- American norms (PAS = 10 of 30) | 37% | |
| Maternal burden | ||
| ≥2 children under age 6 | 60% | |
| Child health/learning problem | 32% | |
| Financial stress | 39% | |
| Family conflict | ||
| Family conflict | 8.09 | 3.23 |
| High family conflict (≥10) | 21% | |
| Self-reported health (1 = poor … 5 = excellent) | 2.77 | 1.07 |
| General self-efficacy | 59.25 | 12.59 |
| Mental health | ||
| CES-D score | 16.60 | 14.73 |
| CES-D score >16 | 46% | |
| Maternal parenting behavior | ||
| Modified parental distress score (PSI) | 14.67 | 5.14 |
| Parent–child dysfunctional interaction (PSI) | 21.86 | 7.22 |
| Modified total stress score (PSI) | 36.53 | 10.64 |
| HOME (verbal and emotional) | 9.53 | 1.95 |
| HOME (avoidances of restrictions and punishment) | 5.98 | 1.23 |
| HOME (organization of environment) | 4.98 | 0.86 |
| HOME (play materials) | 6.96 | 1.75 |
| HOME (maternal involvement) | 4.61 | 2.02 |
| HOME (variety) | 3.35 | 1.41 |
| Total HOME score | 35.42 | 5.98 |
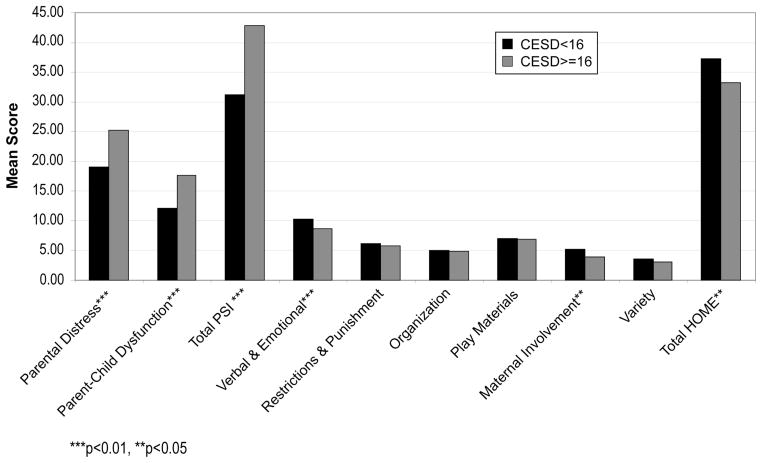
We then estimated three sets of regressions to identify the pathways leading to a loss of self-efficacy: (1) primary risk factors for financial stress, (2) the relationship between financial stress and family conflict, and finally (3) the relationship between family conflict and self-efficacy (Table 2). In our last set of regressions, we evaluated the association between depressive symptoms and total parenting stress and the quality of the home environment (Table 3). Using two-sample independent groups t-test, we also evaluated unadjusted differences in mean scores on each sub-scale of the PSI and HOME for mothers with (CES-D ≥ 16) and without (CES-D < 16) substantial depressive symptoms (Fig. 1).
TABLE 2.
Regression results on financial burdens, family conflict, and maternal self-efficacy
| Variable | Model 1 Financial stress
|
Model 2 Family conflict
|
Model 3 Self-efficacy
|
|||
|---|---|---|---|---|---|---|
| β | SE | β | SE | β | SE | |
| Maternal demographic | ||||||
| Mother’s age | −0.01 | 0.06 | −0.05 | 0.08 | 0.55 | 0.26** |
| Years of education | 0.07 | 0.11 | 0.07 | 0.16 | −1.80 | 0.54*** |
| Works outside home | −0.15 | 0.65 | 1.18 | 0.95 | 11.53 | 3.19*** |
| Acculturation | ||||||
| No English skills | 1.48 | 0.74** | 1.54 | 1.00 | −5.15 | 3.39 |
| Maternal burden | ||||||
| ≥2 children under age 6 | −0.17 | 0.61 | 1.07 | 0.85 | 0.78 | 2.84 |
| Child health/learning problem | 1.16 | 0.63* | −0.65 | 0.92 | −3.01 | 3.04 |
| Financial stress | — | — | 1.62 | 0.90* | −1.70 | 3.07 |
| Family conflict | — | — | — | — | −1.22 | 0.47** |

|
57 | 57 | 57 | |||
| Pseudo-R2/R2 | 0.10 | 0.20 | 0.44 | |||
Note: The financial stress equation (model 1) is estimated using the logit of the response. Therefore, β coefficients in model 1 may be exponentiated and interpreted as odds ratios. Family conflict and self-efficacy equations are estimated with ordinary least squares. Constant not shown. Dashes (−) indicate that this variable was not included.
P < 0.01;
P < 0.05;
P < 0.10.
TABLE 3.
Regression results on CES-D
| Variable | β | SE |
|---|---|---|
| Mother’s age | −0.40 | 0.25 |
| No partner at home | 8.89 | 4.55* |
| Child health/learning problem | 6.85 | 2.87** |
| Financial stress | −0.81 | 2.94 |
| Family conflict | 2.08 | 0.43*** |
| General self-efficacy | −0.40 | 0.11*** |
| Low psychological acculturation | 5.71 | 2.81** |

|
57 | |
| R2 | 0.63 |
Constant not shown.
P < 0.01;
P < 0.05;
P < 0.10.
FIGURE 1.
Maternal parenting differences, by depressive symptoms.
Our results demonstrated that we were correctly targeting a population in which poverty was affecting maternal mental health in the expected fashion. We found that worry or frustration with financial debt was most strongly associated with a lack of English language skills (odds ratio = 4.42; P < 0.05). Families who had one or more children with a chronic health problem or learning disability were nearly three times more likely to report concerns about financial debt (odds ratio = 3.19; P < 0.10). Maternal characteristics (e.g., age and years of education) and social support had no significant association with the mother’s sense of financial burden.
Financial worries, in turn, were significantly associated with the levels of family conflict reported by the mothers. The presence of financial burdens was associated with an average increase of 1.7 points on the family conflict scale (range, 5–20). A lack of English language abilities and the presence of two or more children younger than 6 years also exacerbated the potential for family conflict. Other maternal burdens, maternal characteristics, and social support were not associated with higher family conflict scores. Although maternal characteristics and social supports had little influence on financial stress or family conflict, they were strongly associated with maternal self-efficacy. Finally, as hypothesized, higher family conflict levels were associated with lower levels of maternal self-efficacy.
Having established the linkages among financial worries, family conflict, and maternal self-efficacy, we examined the relationship between maternal self-efficacy and depressive symptoms. Though the causal direction could not be confirmed with our cross-sectional data, maternal self-efficacy explained 31% of the variance in CES-D scores (results not shown). Adding family conflict to the regressions increased the explained variance to 49%. The remaining factors (i.e., social support, multiple family burdens, and acculturation) hypothesized to affect depressive symptoms were not nearly as influential as self-efficacy and family conflict. The presence of multiple family burdens (e.g., child health/learning problems, financial worries, transportation needs, or legal/social service assistance needs) also approached significance in each model.
Finally, in our analyses of depressive symptoms and mother–child interactions, we found significantly higher levels of maternal distress and dysfunctional parent–child interactions among depressed (CES-D ≥ 16) mothers than among nondepressed (CES-D < 16) mothers (Fig. 1). We also found that depressed mothers reported a significantly less stimulating and affirming home environment than non-depressed mothers. The aspects of the home environment that varied most strongly by depressive symptoms were verbal/emotional stimulation and maternal involvement.
In results not shown, these associations continued to be strong when adjusted for potential confounders, such as maternal burden, self-efficacy, family conflict, and acculturation. With the exception of maternal burden, all other factors had only indirect associations with mother–child interactions through their effects on depression.
This set of analyses demonstrated that Latina immigrant mothers who had limited English skills and faced multiple family burdens (e.g., one or more children with a chronic health problem or learning disability, financial debt, or transportation problems) were at risk of experiencing family conflict and subsequently developing both a low sense of self-efficacy and symptoms of depression. Thus, an intervention targeting mothers with these characteristics and designed to promote mother’s self-efficacy by empowering her with various life skills (e.g., language skills, skills to navigate the U.S. health care and the public transportation systems, and the skills needed to garner supportive resources for her child in the United States) could promote a reduction in maternal depressive symptoms and a subsequent improvement in parenting stress and the quality of the home environment.
Conclusions
We have presented a rationale for more intervention trials that support maternal mental health in poverty populations. Maternal survival needs, fatigue, language and cultural factors, and depressive symptoms pose formidable barriers to recruitment into clinical trials of interventions. Yet the need is high when vulnerable children are considered. We have proposed that careful targeting can increase the precision of intervention trials and produce accurate data about an intervention’s efficacy in low-income mothers. Targeting a population of mothers begins by building an evidence-based understanding of the empirical factors that create the risks to their mental health. However, to be successful, an iterative process of narrowing one’s sights, gathering more detailed data directly from potential participants, and allowing the data to hone the process of targeting further is needed.
For a population that is new or not the dominant group, decentering should be used before intervention trials are performed. Poverty can be conceptualized as requiring such different lifestyle and management processes that the same process needs to be carried out even if potential participants are of the same race or culture as that of the researchers. Designing studies to correctly target a population of mothers living in poverty requires researchers from the cultures being studied or, for a population who speaks another language, a bilingual/bicultural research team. The presence of bilingual, bicultural researchers as full and equal members of the research team can guard against an unexamined exportation of ideas and methods developed in one culture to drive the intervention with the other culture. In our case, EHS staff partnered with us for our studies of both English- and Spanish-speaking mothers. As our verification data have shown, through our partnership with these experienced and trusted providers, we were able to correctly target, screen, and recruit symptomatic mothers into our studies and thus reach vulnerable infants and toddlers.
Acknowledgments
We gratefully acknowledge funding from the National Institute of Mental Health (Grant no. RO1 MH065524-01A2), the Foundation for Child Development, young scholars program (Grant no. UNCCH-6-03), and the Department of Health and Human Services, ACYF Early Head Start–University Partnership (Grant no. 90YF0042/01). We thank Regina Canuso and Dr. Diane Holditch-Davis for their collaboration and Ginny Lewis and Hjordis Blanchard for their excellent management of these projects.
Footnotes
According to the 2007 official poverty guidelines (annual income level at which or below basic needs cannot be met), an annual income of $10,000 would be less than needed to support one adult. An annual income of $13,690.00 would qualify a single mother and child for official poverty status (DHHS Poverty Guidelines 2007 http://aspe.hhs.gov/poverty/07poverty.shtml).
The two clinical trials in progress are testing an in-home interpersonal psychotherapy-focused intervention with newly immigrated, Spanish-speaking, low-income mothers and English-speaking mothers in Early Head Start. To be included, these mothers had to have “significant” levels of depressive symptoms, i.e., a score greater than 16 on the Center for Epidemiological Studies Depression scale (Radloff, 1970).
EHS Latina Mothers: Reducing Depressive Symptoms and Improving Infant–Toddler Mental Health, 90YF0042/01 was funded by the DHHS/Administration for Children and Families/Administration for Children, Youth and Families Early Head Start–University Partnership Grant, Linda S. Beeber, PI. Reducing Depressive Symptoms in Low-Income Mothers (English-speaking mothers) was funded by the National Institute of Mental Health RO1 MH065524-01A2, Linda S. Beeber, PI.
Immigrants, Parenting, and Infant-Toddler Well-Being Study was funded by the Foundation for Child Development, New York, NY (Krista Perreira, PI).
The Personal Responsibility and Work Opportunity Act of 1996 allows cash benefits (Welfare) for up to 60 months. In most states, the Temporary Aid to Needy Families (TANF) act requires that a mother must work if she accepts benefits http://www.acf.dhhs.gov/programs/ofa/prwora96.htm. All of the mothers in our focus groups were in minimum–wage or lower, variable shift jobs with unpredictable schedules.
Standardized questionnaires were administered. Acculturation was measured by two instruments, 1) The Short Acculturation Scale for Hispanics (SASH) α = 0.87) and 2) the Psychological Acculturation Scale-PAS (α = 0.85)102,103 Maternal health status were measured with one item on self-reported health.104 Maternal Self-efficacy was measured using the General Self-Efficacy Scale-Spanish version (α = 0.91).105 Maternal-child interactions were measured by the HOME Inventory (α = 0.83).106 Parenting stress was measured by the Parenting Stress Index (PSI), Short-Form, Spanish version, (α = 0.88).107 Maternal depressive symptom severity was measured using the Center for Epidemiological Studies Depression Scale (CES-D)–Spanish version (α = 0.84).101,108
Conflicts of Interest
The authors declare no conflicts of interest.
References
- 1.U.S. Department of Health and Human Services. [Accessed June 1, 2007];Federal Poverty Guidelines. Available at: http://aspe.hhs.gov/poverty/07poverty.shtml.
- 2.Lambrew J, Irons J, Greenberg M. New census data shows deteriorating income and health coverage 2000–2005. Center for American Progress; 2007. [Accessed June 1, 2007]. Available at: http://www.americanprogress.org/issues/2006/08/census_data.pdf. [Google Scholar]
- 3.Gershoff ET, Aber JL, Raver CC, Lennon MC. Income is not enough: incorporating material hardship into models of income associations with parenting and child development. Child Dev. 2007;78:70–95. doi: 10.1111/j.1467-8624.2007.00986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knitzer J. Hearing on economic and societal costs of poverty. National Center for Children in Poverty Columbia University Mailman School of Public Health; New York: 2007. Jan 24, 2007. [Google Scholar]
- 5.Lee Y, Ozawa M. The effect of children on the income status of female-headed households between the United States and five Western industrialized countries. Paper presented at: Meeting the challenge: Research in and with diverse communities; San Antonio, TX. 2006. [Google Scholar]
- 6.Field T. Infants of depressed mothers. Infant Behav Dev. 1995;18:1–13. doi: 10.1016/j.infbeh.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Weissman MM, Pilowsky DJ, Wickramaratne PJ, et al. Remissions in maternal depression and child psychopathology: a STAR* D-child report. JAMA. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 8.Linver MR, Brooks-Gunn J, Kohen DE. Family processes as pathways from income to young children’s development. Dev Psychol. 2002;38:719–734. [PubMed] [Google Scholar]
- 9.Mistry RS, Vandewater EA, Huston AC, McLoyd VC. Economic well-being and children’s social adjustment: the role of family process in an ethnically diverse low-income sample. Child Dev. 2002;73:935–951. doi: 10.1111/1467-8624.00448. [DOI] [PubMed] [Google Scholar]
- 10.Mistry RS, Biesanz JC, Taylor LC, et al. Family income and its relation to preschool children’s adjustment for families in the NICHD Study of Early Child Care. Dev Psychol. 2004;40:727–745. doi: 10.1037/0012-1649.40.5.727. [DOI] [PubMed] [Google Scholar]
- 11.Parke RD, Coltrane S, Duffy S, et al. Economic stress, parenting, and child adjustment in Mexican American and European American families. Child Dev. 2004;75:1632–1656. doi: 10.1111/j.1467-8624.2004.00807.x. [DOI] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 13.Stockdale SE, Wells KB, Tang L, et al. The importance of social context: neighborhood stressors, stress-buffering mechanisms, and alcohol, drug, and mental health disorders. Soc Sci Med. 2007;65:1867–1881. doi: 10.1016/j.socscimed.2007.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown GW, Moran PM. Single mothers, poverty and depression. Psychol Med. 1997;27:21–33. doi: 10.1017/s0033291796004060. [DOI] [PubMed] [Google Scholar]
- 15.Cutrona CE, Russell DW, Brown PA, et al. Neighborhood context, personality, and stressful life events as predictors of depression among African American women. J Abnorm Psychol. 2005;114:3–15. doi: 10.1037/0021-843X.114.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo G, Harris KM. The mechanisms mediating the effects of poverty on children’s intellectual development. Demography. 2000;37:431–447. doi: 10.1353/dem.2000.0005. [DOI] [PubMed] [Google Scholar]
- 17.Conger RD, Wallace LE, Sun Y, et al. Economic pressure in African American families: a replication and extension of the family stress model. Dev Psychol. 2002;38:179–193. [PubMed] [Google Scholar]
- 18.McLoyd VC, Jayaratne TE, Ceballo R, Borquez J. Unemployment and work interruption among African American single mothers: effects on parenting and adolescent socioemotional functioning. Child Dev. 1994;65(2 Spec):562–589. [PubMed] [Google Scholar]
- 19.NICHD Early Child Care Research Network. Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Dev Psychol. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- 20.Ceballo R, McLoyd VC. Social support and parenting in poor, dangerous neighborhoods. Child Dev. 2002;73:1310–1321. doi: 10.1111/1467-8624.00473. [DOI] [PubMed] [Google Scholar]
- 21.Costello EJ, Compton SN, Keeler G, An-gold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290:2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- 22.Brody GH, Flor DL. Maternal resources, parenting practices, and child competence in rural, single-parent African American families. Child Dev. 1998;69:803–816. [PubMed] [Google Scholar]
- 23.Duncan GJ, Brooks-Gunn J. Family poverty, welfare reform, and child development. Child Dev. 2000;71:188–196. doi: 10.1111/1467-8624.00133. [DOI] [PubMed] [Google Scholar]
- 24.Furstenberg FF., Jr . How Families Manage Risk and Opportunity in Dangerous Neighborhoods. Sage Publications; Newbury Park, CA: 1993. [Google Scholar]
- 25.Jarrett R, Jefferson S, Roach A. Family and parenting strategies in high risk African American neighborhoods. Paper presented at Head Start’s Fifth National Research Conference; Washington, DC. 2000. [Google Scholar]
- 26.Jarrett R, Burton L. Dynamic dimensions of family structure in low-income African American families: Emergent themes in qualitative research. J Comp Fam Studies. 1999;30:177–187. [Google Scholar]
- 27.Petterson SM, Albers AB. Effects of poverty and maternal depression on early child development. Child Dev. 2001;72:1794–1813. doi: 10.1111/1467-8624.00379. [DOI] [PubMed] [Google Scholar]
- 28.Jahoda M. Current Concepts of Positive Mental Health. Basic Books; New York: 1958. [Google Scholar]
- 29.Beeber LS, Miles MS. Maternal mental health and parenting in poverty. Annu Rev Nurs Res. 2003;21:303–331. [PubMed] [Google Scholar]
- 30.Brooks-Gunn J, Klebanov PK, Duncan GJ. Ethnic differences in children’s intelligence test scores: role of economic deprivation, home environment, and maternal characteristics. Child Dev. 1996;67:396–408. [PubMed] [Google Scholar]
- 31.Goodman S, Gotlib I. Risk of psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- 32.Samaan RA. The influence of race, ethnicity, and poverty on the mental health of children. J Health Care Poor Underserved. 2000;11:100–110. doi: 10.1353/hpu.2010.0557. [DOI] [PubMed] [Google Scholar]
- 33.Cutrona CE, Cole V, Colangelo N, et al. Perceived parental social support and academic achievement: an attachment theory perspective. J Pers Soc Psychol. 1994;66:369–378. doi: 10.1037//0022-3514.66.2.369. [DOI] [PubMed] [Google Scholar]
- 34.Furstenberg FF. How Families Manage Risk and Opportunity in Dangerous Neighborhoods. Sage Publications; Newbury Park, CA: 1993. [Google Scholar]
- 35.Hess CR, Papas MA, Black MM. Resilience among African American adolescent mothers: predictors of positive parenting in early infancy. J Pediatr Psychol. 2002;27:619–629. doi: 10.1093/jpepsy/27.7.619. [DOI] [PubMed] [Google Scholar]
- 36.Jackson A, Brooks-Dunn J, Huang C, Glassman M. Single mothers in low-wage jobs: financial strain, parenting, and preschoolers’ outcomes. Child Dev. 2000;71:1409–1423. doi: 10.1111/1467-8624.00236. [DOI] [PubMed] [Google Scholar]
- 37.Jarrett R. Working Paper. Russell Sage Foundation; New York, NY: 1993. Parental management strategies: two approaches. [Google Scholar]
- 38.Jarrett R, Burton L. Dynamic dimensions of family structure in low-income African American families: emergent themes in qualitative research. J Comp Fam Studies. 1999;30:177–187. [Google Scholar]
- 39.Jarrett R, Jefferson S, Roach A. Family and parenting strategies in high risk African American neighborhoods. Paper presented at Head Start’s Fifth National Research Conference; Washington, DC. 2000. [Google Scholar]
- 40.Wakschlag LS, Chase-Lansdale PL, Brooks-Gunn J. Not just “ghosts in the nursery”: contemporaneous intergenerational relationships and parenting in young African-American families. Child Dev. 1996;67:2131–2147. doi: 10.1111/j.1467-8624.1996.tb01848.x. [DOI] [PubMed] [Google Scholar]
- 41.Jarrett R. Living poor: life among single parent, African American women. Soc Probl. 1994;41:30–49. [Google Scholar]
- 42.Natsuaki MN, Ge X, Brody GH, et al. African American children’s depressive symptoms: the prospective effects of neighborhood disorder, stressful life events, and parenting. Am J Community Psychol. 2007;39:163–176. doi: 10.1007/s10464-007-9092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heckman JJ, Masterov DV. The Productivity Argument for Investing in Young Children. University of Chicago; Chicago: 2005. [Google Scholar]
- 44.Belle D. Lives in Stress: Women and Depression. Sage; Beverly Hills, CA: 1982. [Google Scholar]
- 45.Brown GW, Moran PM. Single mothers, poverty and depression. Psychol Med. 1997;27:21–33. doi: 10.1017/s0033291796004060. [DOI] [PubMed] [Google Scholar]
- 46.Gross D. Implications of maternal depression for the development of young children. IMAGE. 1989;44:103–107. doi: 10.1111/j.1547-5069.1989.tb00108.x. [DOI] [PubMed] [Google Scholar]
- 47.Jackson A, Brooks-Dunn J, Huang C, Glassman M. Single mothers in low-wage jobs: financial strain, parenting, and preschoolers’ outcomes. Child Dev. 2000;71:1409–1423. doi: 10.1111/1467-8624.00236. [DOI] [PubMed] [Google Scholar]
- 48.Black AR, Cook JL, Murry VM, Cutrona CE. Ties that bind: implications of social support for rural, partnered African American women’s health functioning. Womens Health Issues. 2005;15:216–223. doi: 10.1016/j.whi.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 49.Ennis NE, Hobfoll SE, Schroder KE. Money doesn’t talk, it swears: how economic stress and resistance resources impact inner-city women’s depressive mood. Am J Community Psychol. 2000;28:149–173. doi: 10.1023/A:1005183100610. [DOI] [PubMed] [Google Scholar]
- 50.Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. J Consult Clin Psychol. 1995;63:90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- 51.Sherbourne CD, Wells KB, Hays RD, et al. Subthreshold depression and depressive disorder: clinical characteristics of general medical and mental health specialty. Am J Psychiatry. 1994;151:1777–1784. doi: 10.1176/ajp.151.12.1777. [DOI] [PubMed] [Google Scholar]
- 52.Bornstein M. Handbook of Parenting. Erlbaum; Hillsdale, NJ: 1995. [Google Scholar]
- 53.Hammen C. Depression Runs in Families. Springer; New York: 1991. [Google Scholar]
- 54.Rosenblum O, Mazet P, Benony H. Mother and infant affective involvement states and maternal depression. Infant Mental Health. 1997;181:350–363. [Google Scholar]
- 55.Breznitz Z, Sherman T. Speech patterning of natural discourse of well and depressed mothers and their young children. Child Dev. 1987;58:395–400. [PubMed] [Google Scholar]
- 56.Zlochower A, Cohn J. Vocal timing in face-to-face interaction of clinically depressed and nondepressed mothers and their 4-month-old infants. Infant Behav Dev. 1996;19:371–374. [Google Scholar]
- 57.Field T, Healy B, Goldstein S, et al. Infants of depressed mothers show “depressed” behavior even with nondepressed adults. Child Dev. 1988;59:1569–1579. doi: 10.1111/j.1467-8624.1988.tb03684.x. [DOI] [PubMed] [Google Scholar]
- 58.Cohn JF, Matias R, Tronick EZ, et al. Face-to-face interactions of depressed mothers and their infants. New Dir Child Dev. 1986 Winter;:31–45. doi: 10.1002/cd.23219863405. [DOI] [PubMed] [Google Scholar]
- 59.Lyons-Ruth K, Wolfe R, Lyubchik A. Depression and the parenting of young children: making the case for early preventive mental health services. Harv Rev Psychiatry. 2000;8:148–153. [PubMed] [Google Scholar]
- 60.Murray L, Fiori-Crowley A, Hooper R, Cooper P. The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev. 1996;67:2512–2526. [PubMed] [Google Scholar]
- 61.Zeanah C, Boris N, Larrieu J. Infant development and developmental risk: a review of the past 10 years. J Am Child Adolesc Psychiatry. 1997;36:165–178. doi: 10.1097/00004583-199702000-00007. [DOI] [PubMed] [Google Scholar]
- 62.Field T. Maternal depression effects on infants and early interventions. Prev Med. 1998;27:200–203. doi: 10.1006/pmed.1998.0293. [DOI] [PubMed] [Google Scholar]
- 63.Poverty NNCfCi. Testimony of Jane Knitzer to the House Ways and Means Committee, US Congress. National Center for Children in Poverty Columbia University Mailman School of Public Health; 2007. [Accessed May 15, 2007]. Available at: http://www.mailman.hs.columbia.edu/news/pdf/wmt07_text1.pdf. [Google Scholar]
- 64.Kaplan PS, Bachorowski JA, Zarlengo-Strouse P. Child-directed speech produced by mothers with symptoms of depression fails to promote associative learning in 4-month-old infants. Child Dev. 1999;70:560–570. doi: 10.1111/1467-8624.00041. [DOI] [PubMed] [Google Scholar]
- 65.Hart S, Jones NA, Field T, Lundy B. One-year-old infants of intrusive and withdrawn depressed mothers. Child Psychiatry Hum Dev. 1999;30:111–120. doi: 10.1023/a:1021902418770. [DOI] [PubMed] [Google Scholar]
- 66.Gross D, Conrad B, Fogg L, et al. A longitudinal study of maternal depression and preschool children’s mental health. Nurs Res. 1995;44:96–101. [PubMed] [Google Scholar]
- 67.Lang C, Field T, Pickens J, et al. Preschoolers of dysphoric mothers. J Child Psychol Psychiatry. 1996;37:221–224. doi: 10.1111/j.1469-7610.1996.tb01394.x. [DOI] [PubMed] [Google Scholar]
- 68.Cicchetti D, Rogosch R, Toth S, Spagnola M. Affect, cognition, and the emergence of self-knowledge in the toddler offspring of depressed mothers. J Exp Child Psychol. 1997;67:338–362. doi: 10.1006/jecp.1997.2412. [DOI] [PubMed] [Google Scholar]
- 69.Anderson CM, Robins CS, Greeno CG, et al. Why lower income mothers do not engage with the formal mental health care system: perceived barriers to care. Qual Health Res. 2006;16:926–943. doi: 10.1177/1049732306289224. [DOI] [PubMed] [Google Scholar]
- 70.Belle D, Doucet J. Poverty, inequality, and discrimination as sources of depression among U. A. women. Psychol Women Quart. 2003;27:101–113. [Google Scholar]
- 71.O’Hara M, Stuart S, Gorman L, Wenzel A. Efficacy of interpersonal psychotherapy for post-partum depression. Arch Gen Psychiatry. 2000;57:1039–1044. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- 72.Stuart S, O’Hara MW, Gorman LL. The prevention and psychotherapeutic treatment of postpartum depression. Arch Womens Ment Health. 2003;6(Suppl 2):S57–S69. doi: 10.1007/s00737-003-0003-y. [DOI] [PubMed] [Google Scholar]
- 73.Forman DR, O’Hara MW, Stuart S, et al. Effective treatment for postpartum depression is not sufficient to improve the developing mother–child relationship. Dev Psychopathol. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- 74.Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–220. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 75.Appleby L, Warner R, Whitton A, Faragher B. A controlled study of fluoxetine and cognitive-behavioural counselling in the treatment of postnatal depression. BMJ. 1997;314:932–936. doi: 10.1136/bmj.314.7085.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chabrol H, Teissedre F, Saint-Jean M, et al. Prevention and treatment of post-partum depression: a controlled randomized study on women at risk. Psychol Med. 2002;32:1039–1047. doi: 10.1017/s0033291702006062. [DOI] [PubMed] [Google Scholar]
- 77.Holden JM, Sagovsky R, Cox JL. Counseling in a general practice setting: controlled study of health visitor intervention in treatment of postnatal depression. BMJ. 1989;298:223–226. doi: 10.1136/bmj.298.6668.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wickberg B, Hwang C. Counseling of postnatal depression: a controlled study on a population based Swedish sample. J Affect Disord. 1996;39:209–216. doi: 10.1016/0165-0327(96)00034-1. [DOI] [PubMed] [Google Scholar]
- 79.Champion LA, Goodall G, Rutter M. Behaviour problems in childhood and stressors in early adult life. I. A 20 year follow-up of London school children. Psychol Med. 1995;25:231–246. doi: 10.1017/s003329170003614x. [DOI] [PubMed] [Google Scholar]
- 80.Pinderhughes EE, Dodge KA, Bates JE, et al. Discipline responses: influences of parents’ socioeconomic status, ethnicity, beliefs about parenting, stress, and cognitive-emotional processes. J Fam Psychol. 2000;14:380–400. doi: 10.1037//0893-3200.14.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Reid MJ, Webster-Stratton C, Baydar N. Halting the development of conduct problems in head start children: the effects of parent training. J Clin Child Adolesc Psychol. 2004;33:279–291. doi: 10.1207/s15374424jccp3302_10. [DOI] [PubMed] [Google Scholar]
- 82.Baydar N, Reid MJ, Webster-Stratton C. The role of mental health factors and program engagement in the effectiveness of a preventive parenting program for Head Start mothers. Child Dev. 2003;74:1433–1453. doi: 10.1111/1467-8624.00616. [DOI] [PubMed] [Google Scholar]
- 83.Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems–a meta-analytic review. J Child Psychol Psychiatry. 2006;47:99–111. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- 84.Jones SM, Lamb-Parker F, Schweder A, Ripple C. Parent Involvement in Head Start: Context and Consequences. Columbia University; New York: 2001. [Google Scholar]
- 85.Hartman RR, Stage SA, Webster-Stratton C. A growth curve analysis of parent training outcomes: examining the influence of child risk factors (inattention, impulsivity, and hyperactivity problems), parental and family risk factors. J Child Psychol Psychiatry. 2003;44:388–398. doi: 10.1111/1469-7610.00129. [DOI] [PubMed] [Google Scholar]
- 86.Webster-Stratton C. Advancing videotape parent training: a comparison study. J Consult Clin Psychol. 1994;62:583–593. doi: 10.1037//0022-006x.62.3.583. [DOI] [PubMed] [Google Scholar]
- 87.Sanders MR, Markie-Dadds C, Tully LA, Bor W. The Triple P-Positive Parenting Program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol. 2000;68:624–640. [PubMed] [Google Scholar]
- 88.Bor W, Sanders MR, Markie-Dadds C. The effects of the Triple P-Positive Parenting Program on preschool children with co-occurring disruptive behavior and attentional/hyperactive difficulties. J Abnorm Child Psychol. 2002;30:571–587. doi: 10.1023/a:1020807613155. [DOI] [PubMed] [Google Scholar]
- 89.Taylor TK, Biglan A. Behavioral family interventions for improving child-rearing: a review of the literature for clinicians and policy makers. Clin Child Fam Psychol Rev. 1998;1:41–60. doi: 10.1023/a:1021848315541. [DOI] [PubMed] [Google Scholar]
- 90.Centers for Disease Control and Prevention. The Community Guide. 2007 http://www.thecommunityguide.org.
- 91.McLennan JD, Offord DR. Should post-partum depression be targeted to improve child mental health? J Am Acad Child Adolesc Psychiatry. 2002;41:28–35. doi: 10.1097/00004583-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 92.Lipsey MW. Design Sensitivity: Statistical Power for Experimental Research. Sage; Newbury Park, CA: 1990. [Google Scholar]
- 93.Beeber LS, Holditch-Davis D, Belyea MJ, et al. In-home intervention for depressive symptoms with low-income mothers of infants and toddlers in the United States. Health Care Women Int. 2004;25:561–580. doi: 10.1080/07399330490444830. [DOI] [PubMed] [Google Scholar]
- 94.Miranda J, Azocar F, Organista KC, et al. Recruiting and retaining low-income Latinos in psychotherapy research. J Consult Clin Psychol. 1996;64:868–874. doi: 10.1037//0022-006x.64.5.868. [DOI] [PubMed] [Google Scholar]
- 95.Munoz RF, Ying YW, Bernal G, et al. Prevention of depression with primary care patients: a randomized controlled trial. Am J Community Psychol. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- 96.Globe DR, Schoua-Glusberg A, Paz S, et al. Using focus groups to develop a culturally sensitive methodology for epidemiological surveys in a Latino population: findings from the Los Angeles Latino Eye Study (LALES) Ethn Dis. 2002;12:259–266. [PubMed] [Google Scholar]
- 97.Lange JW. Methodological concerns for non-Hispanic investigators conducting research with Hispanic Americans. Res Nurs Health. 2002;25:411–419. doi: 10.1002/nur.10049. [DOI] [PubMed] [Google Scholar]
- 98.Munet-Vilaro F, Folkman S, Gregorish S. Depressive symptomatology in three Latino Groups. West J Nurs Res. 1999;21:209–224. doi: 10.1177/01939459922043848. [DOI] [PubMed] [Google Scholar]
- 99.Posner SF, Stewart AL, Marin G, Perez-Stable EJ. Factor variability of the Center for Epidemiological Studies Depression Scale (CES-D) among urban Latinos. Ethn Health. 2001;6:137–144. doi: 10.1080/13557850120068469. [DOI] [PubMed] [Google Scholar]
- 100.Roberts RE, Vernon SW, Rhoades HM. Effects of language and ethnic status on reliability and validity of the Center for Epidemiologic Studies-Depression Scale with psychiatric patients. J Nerv Ment Dis. 1989;177:581–592. doi: 10.1097/00005053-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 101.Vega WA, Kolody B, Valle R, Hough R. Depressive symptoms and their correlates among immigrant Mexican women in the United States. Soc Sci Med. 1986;22:645–652. doi: 10.1016/0277-9536(86)90037-7. [DOI] [PubMed] [Google Scholar]
- 102.Marin G, Sabogal F, Marin B, et al. Development of a short acculturation scale for Hispanics. Hispanic. J Behav Sci. 1987;9:183–205. [Google Scholar]
- 103.Tropp LR, Coll CG, Alarcon O, Vazquez-Garcia HA. Psychological acculturation: development of a new measure for Puerto Ricans on the U.S. mainland. Educ Psychol Meas. 1999;59:351–367. doi: 10.1177/00131649921969794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.McGee DL, Liao Y, Cao G, Cooper RS. Self-reported health status and mortality in a multiethnic, U.S. cohort. Am J Epidemiol. 1999;149:41–46. doi: 10.1093/oxfordjournals.aje.a009725. [DOI] [PubMed] [Google Scholar]
- 105.Luszczynska A, Scholz U, Schwarzer R. The general self-efficacy scale: multicultural validation studies. J Psychol. 2005;139:439–457. doi: 10.3200/JRLP.139.5.439-457. [DOI] [PubMed] [Google Scholar]
- 106.Caldwell BB, Bradley R. Home Observation for Measurement of the Environment. University of Arkansas; Little Rock, AR: 1980. [Google Scholar]
- 107.Loyd BH, Abidin RR. Revision of the parenting stress index. J Pediatr Psychol. 1985;10:169–177. doi: 10.1093/jpepsy/10.2.169. [DOI] [PubMed] [Google Scholar]
- 108.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:285–401. [Google Scholar]