Abstract
Background: The subclavian vein is the preferred site for central venous catheter placement due to infection risk and patient comfort. Ultrasound guidance is useful in cannulation of other veins, but for the subclavian vein, current ultrasound-guided techniques using high-frequency linear array probes are generally limited to axillary vein cannulation.
Methods: We report a series of patients who underwent clinically indicated subclavian venous catheter placement using a micro-convex pediatric probe for real-time guidance in the vein’s longitudinal axis. We identified rates of successful placement and complications by chart review.
Results: Twenty-four catheters were placed using the micro-convex pediatric probe with confirmation of placement of the needle medial to the lateral border of the first rib. Sixteen of the catheters were placed by trainee physicians. In 23 patients, the catheter was placed without complication (hematoma, pneumothorax, infection). In one patient, the vein could not be safely cannulated without risk of arterial puncture, so an alternative site was selected.
Conclusions: Infraclavicular subclavian vein cannulation using real-time ultrasound with a micro-convex pediatric probe appears to be a safe and effective method of placing subclavian vascular catheters. This technique merits further study to confirm safety and efficacy.
Keywords: vascular access, ultrasound, subclavian, central venous, catheter
Central venous access is a common requirement in the critically ill patient for a variety of indications, including poor peripheral venous access, hemodynamic monitoring, hemodialysis, plasmapheresis, intravascular cooling, cardiac pacing, administration of vasoactive agents, parenteral nutrition, or chemotherapy. In these patients, a central venous catheter is typically placed in the internal jugular, subclavian, or femoral vein. In the emergency department setting, the internal jugular is the most commonly selected site (1). The femoral site and the internal jugular site are typically associated with increased risk of infection compared with the subclavian site (2, 3). Furthermore, the risk of arterial puncture is greater at the jugular site than the subclavian site (4). Generally speaking, the subclavian vein is the preferred site of central venous access when the procedure is performed by an experienced operator, despite concern about risk of pneumothorax (2).
Ultrasound guidance for venous access is well described in the literature and increasingly common (5). Ultrasound guidance reduces time to venous cannulation and reduces risk of complications during central venous access (6). Ultrasound is frequently used for placement of central venous catheters in the internal jugular and femoral veins but less commonly used in subclavian venous access, perhaps due to poor visualization of the vein from acoustic shadowing from the overlying clavicle. Prior studies have described methods of using ultrasound for infraclavicular subclavian vein access using 7.5-MHz linear array probes. One approach images the vein in short axis (7) and another images the vein in long axis (Figure 1) (8). Both approaches are actually transpectoral axillary vein cannulation, rather than subclavian vein cannulation (9). Advances in ultrasound technology, including micro-convex probes and smaller footprint linear array probes, may allow for real-time ultrasound guidance of an infraclavicular subclavian vein cannulation rather than axillary vein cannulation (10).
Figure 1.

Demonstration of axillary vein cannulation using a standard linear array probe, in the long axis (top panel) and short axis (middle panel) positions. The needle entry point is often more than 4 cm distal from the subclavian vein (bottom panel).
We developed an approach to cannulate the subclavian vein using a micro-convex array pediatric ultrasound probe. Although independently developed, this approach is identical to the approach first described by Lichtenstein (11).
Methods
This is a case series of critically ill medical patients who received central venous catheterization using an ultrasound-guided infraclavicular subclavian vein approach. Patients in this chart review were identified by physician billing and review of all ultrasound imaging during the study period. The procedure was either performed by or supervised by one of four attending physicians who regularly place ultrasound-guided central venous catheters (M.J.L., E.L.H., C.K.G., or S.M.B.). The study occurred between October 2012 and June 2013. The population was a convenience sample of patients admitted to a 24-bed, tertiary care, teaching intensive care unit, who had clinical indication for a subclavian central venous catheter. This study was approved by the local institutional review board (#1024670) with waiver of informed consent for the chart review required to document rates of success or complication. We documented success of cannulation and occurrence of pneumothorax, hematoma, arterial puncture, or catheter-related bloodstream infection.
Description of Venipuncture
The method of venipuncture is detailed in the accompanying video. Several different venous catheters were used in this study, including hemodialysis catheters, triple-lumen catheters, and percutaneous pacemaker–introducing catheters. All ultrasound imaging was performed on a CX50 (Philips Healthcare, Andover, MA) using an 8-MHz micro-convex array pediatric probe. We sterilized the selected site with chlorhexidine and draped the patient using full barrier precautions. We covered the probe with a sterile plastic sleeve and positioned it at the inferior margin of the clavicle. We imaged the subclavian vein in short axis and rotated the probe 90°, visualizing the vein continuously, until it was in long axis, with visualization of the vein beneath the clavicle. It is important to identify surrounding structures such as the pleura and the artery before venipuncture. We found that resting the probe against the clavicle improved visualization and prevented translation of the probe. We positioned the needle at a 45° angle at the center of the probe, aligned along the ultrasound plane, and entered the skin with visualization of the needle shaft and tip throughout the entire procedure. Subclavian placement is confirmed by visualizing the needle and wire entering the vein medial to the lateral margin of the first rib, which is the anatomic boundary between subclavian and axillary vein (Figure 2, Video 1).
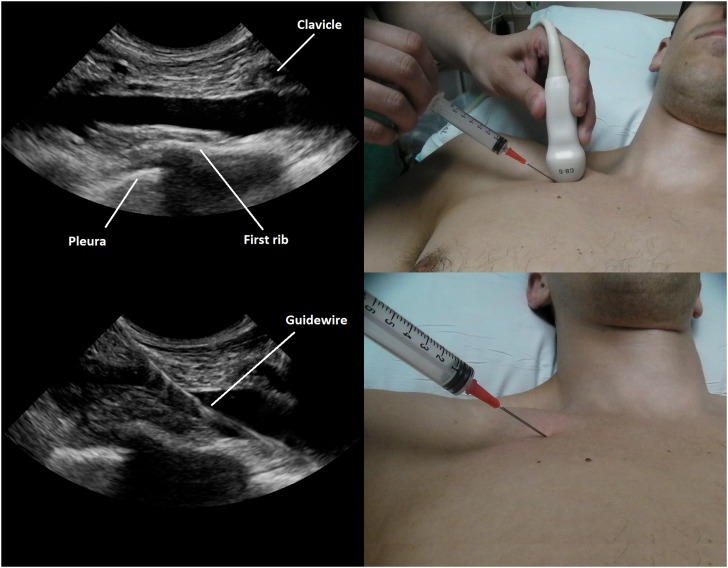
Figure 2.
Ultrasound image of a right subclavian cannulation. The probe is placed at the inferior margin of the clavicle (top right), and the subclavian vein is imaged (top left). The needle is placed directly under the curved portion of the probe, entering at a 45°angle (top right). The guidewire is seen entering the subclavian vein. Subclavian placement is confirmed because the needle and wire entry are medial to the lateral margin of the first rib (bottom left). This method allows for needle entry within 1 to 2 cm from the clavicle (bottom right).
Video 1:
Demonstration of the subclavian access technique.
Results
We identified on chart review 24 patients who underwent this procedure. We included all patients known to have undergone this procedure. No patient screened was found to have inadequate ultrasound windows. Sixteen of the catheter attempts were performed by trainees. In one trainee attempt, the subclavian vein of a slender patient completely collapsed when attempting venipuncture, and the procedure was aborted out of concern for damaging distal structures. In that patient, a small hematoma was noted. In the remaining 23 patients, there was no subsequent documented hematoma, pneumothorax, or catheter-related bloodstream infection. During the period covered by this review, the only pneumothorax in our intensive care unit attributed to subclavian vein catheterization occurred during a blind landmark technique performed by a physician who does not use ultrasound guidance for subclavian catheterization. Ten procedure notes documented the number of needle punctures, with eight successful on the first attempt and one requiring two attempts. In one patient, four attempts were made, and then the procedure was handed over to the supervising physician, who successfully placed the catheter.
Discussion
It appears that ultrasound-guided infraclavicular subclavian vein catheter placement using a pediatric micro-convex array probe, as described in the accompanying video, can be successfully performed with low risk of complication.
Although the difference between subclavian and axillary venipuncture is largely academic, there are potential benefits of subclavian venipuncture over axillary venipuncture. Cannulation of the smaller and more distal axillary vein may have increased risk of damaging the medial cutaneous nerve, as it runs medial to the axillary vein in this location (12). Axillary venipuncture is typically deeper than subclavian venipuncture, which may increase the technical difficulty of safely performing the procedure. Transpectoral axillary vein cannulation may also require longer puncture needles and longer introducer sheaths, as the catheter must traverse through more tissue. Catheter-related thrombosis is related to impedance of blood flow (13). Cannulation of the larger subclavian vein may, in principle, cause less reduction in blood flow than the smaller axillary vein.
This technique exploits the shape and frequency of the probe. This probe has a tightly curved, small footprint. Consequently, the skin entry point is often directly beneath the center of the probe, rather than along a lateral edge. Venipuncture is typically subclavian or proximal axillary, rather than the mid-distal axillary venipuncture that occurs with a standard linear array vascular access probe. One can also generally visualize the distal subclavian vein without acoustic shadowing from the clavicle. In ultrasound imaging, visual resolution is related to the probe frequency. The pediatric micro-convex probe has a decreased frequency (and therefore decreased resolution) compared with the standard linear probe (8 vs. 12 MHz), although it offers good resolution for visualization of vascular structures and far superior resolution than the typical phased array/sector array probe (≤5 MHz) used for chest or abdominal imaging. It is possible that an endocavitary probe may also be applied in this technique, as it has a similar shape, size, and frequency as the pediatric curvilinear probe. The endocavitary probe has been described for supraclavicular visualization of the subclavian vein (14). Clinicians wishing to use this technique should be aware that the pediatric micro-convex probe costs around $8,000 to $10,000 (cheaper alternatives may exist), and the probe has several applications other than vascular access and pediatric imaging. We find this probe well suited for pleural and lung ultrasonography.
Although not tested in this study, we believe the micro-convex array approach may also have a niche in internal jugular central venous catheter placement. In some patients (i.e., those with short necks or morbid obesity), a standard vascular access probe may have too great a footprint to allow for a long-axis approach of the internal jugular vein. The approach we describe may allow for use of long-axis approach in more patients.
This is an uncontrolled case series, with convenience sampling and no comparator group. We acknowledge that such a study cannot assess the relative safety and usefulness of the various alternative approaches to subclavian vein cannulation. A formal randomized controlled trial would be necessary to answer that question, although current linear-array techniques have been reported to have low complications and high success rates. A previous trial demonstrated no difference between a linear-array technique and blind cannulation (15). Although we witnessed no major complications, we conceive of some potential problems that can occur with this approach. The vein is visualized in long axis, with the needle placed at a steep angle of approach (45°). An advantage of a long-axis view over a short-axis view is that the operator can visualize the entire subcutaneous portion of the needle, avoiding inadvertent puncture of distal structures. A disadvantage is that often only one vessel (vein or artery) is seen at a time. Although an experienced operator should have no difficulty discerning vein from artery, an inexperienced operator could use an ultrasound to unwittingly perform subclavian artery puncture. Similarly, an inexperienced operator, while manipulating the needle, syringe, or wire, could inadvertently move the needle deeper and puncture distal structures. Many of our trainees, who were familiar with short-axis internal jugular access, reported greater difficulty in performing this technique their first time compared with their usual approach, as it requires alignment of the needle with the ultrasound plane.
With increasing emphasis placed on use of ultrasound guidance for venous catheterization, there is need for a safe and easy technique to cannulate the subclavian vein. Other published methods that use the standard linear probe result in axillary vein cannulation. We describe a method that uses a probe that allows for an infraclavicular subclavian vein cannulation.
Footnotes
Supported by Career Development Award K23GM094465 from the National Institute of General Medical Sciences (S.M.B.).
All authors contributed to study design, acquisition of patients and images, and revision of the manuscript for intellectual content. M.J.L., J.F., and C.K.G. contributed to acquisition of video material for the instructional video. M.J.L. drafted the manuscript and performed image and video editing.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Balls A, LoVecchio F, Kroeger A, Stapczynski JS, Mulrow M, Drachman D Central Line Emergency Access Registry Investigators. Ultrasound guidance for central venous catheter placement: results from the Central Line Emergency Access Registry Database. Am J Emerg Med. 2010;28:561–567. doi: 10.1016/j.ajem.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Lorente L, Henry C, Martín MM, Jiménez A, Mora ML. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care. 2005;9:R631–R635. doi: 10.1186/cc3824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, Rigaud JP, Casciani D, Misset B, Bosquet C, et al. French Catheter Study Group in Intensive Care. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA. 2001;286:700–707. doi: 10.1001/jama.286.6.700. [DOI] [PubMed] [Google Scholar]
- 4.Ruesch S, Walder B, Tramèr MR. Complications of central venous catheters: internal jugular versus subclavian access—a systematic review. Crit Care Med. 2002;30:454–460. doi: 10.1097/00003246-200202000-00031. [DOI] [PubMed] [Google Scholar]
- 5.Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, Reeves ST Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2011;24:1291–1318. doi: 10.1016/j.echo.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 6.Rabindranath KS, Kumar E, Shail R, Vaux EC. Ultrasound use for the placement of haemodialysis catheters. Cochrane Database Syst Rev. 2011;(11):CD005279. doi: 10.1002/14651858.CD005279.pub4. [DOI] [PubMed] [Google Scholar]
- 7.O’Leary R, Ahmed SM, McLure H, Oram J, Mallick A, Bhambra B, Bodenham AR. Ultrasound-guided infraclavicular axillary vein cannulation: a useful alternative to the internal jugular vein. Br J Anaesth. 2012;109:762–768. doi: 10.1093/bja/aes262. [DOI] [PubMed] [Google Scholar]
- 8.Fragou M, Gravvanis A, Dimitriou V, Papalois A, Kouraklis G, Karabinis A, Saranteas T, Poularas J, Papanikolaou J, Davlouros P, et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011;39:1607–1612. doi: 10.1097/CCM.0b013e318218a1ae. [DOI] [PubMed] [Google Scholar]
- 9.Bodenham AR. Ultrasound-guided subclavian vein catheterization: beyond just the jugular vein. Crit Care Med. 2011;39:1819–1820. doi: 10.1097/CCM.0b013e31821b813b. [DOI] [PubMed] [Google Scholar]
- 10.Shiloh AL, Eisen LA, Yee M, Langner JB, LeDonne J, Karakitsos D. Ultrasound-guided subclavian and axillary vein cannulation via an infraclavicular approach: in the tradition of Robert Aubaniac. Crit Care Med. 2012;40:2922–2923. doi: 10.1097/CCM.0b013e31825cea64. [DOI] [PubMed] [Google Scholar]
- 11.Lichtenstein D. Cathétérisme écho-guidé de la veine sous-clavière en réanimation. Ann Fr Anesth Reanim. 2000;19:266s. [Google Scholar]
- 12.Nickalls RW. A new percutaneous infraclavicular approach to the axillary vein. Anaesthesia. 1987;42:151–154. doi: 10.1111/j.1365-2044.1987.tb02988.x. [DOI] [PubMed] [Google Scholar]
- 13.Joffe HV, Goldhaber SZ. Upper-extremity deep vein thrombosis. Circulation. 2002;106:1874–1880. doi: 10.1161/01.cir.0000031705.57473.1c. [DOI] [PubMed] [Google Scholar]
- 14.Mallin M, Louis H, Madsen T. A novel technique for ultrasound-guided supraclavicular subclavian cannulation. Am J Emerg Med. 2010;28:966–969. doi: 10.1016/j.ajem.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 15.Mansfield PF, Hohn DC, Fornage BD, Gregurich MA, Ota DM. Complications and failures of subclavian-vein catheterization. N Engl J Med. 1994;331:1735–1738. doi: 10.1056/NEJM199412293312602. [DOI] [PubMed] [Google Scholar]