Abstract
Rationale: Hospitalizations for severe sepsis are common, and a growing number of patients survive to hospital discharge. Nonetheless, little is known about survivors’ post-discharge healthcare use.
Objectives: To measure inpatient healthcare use of severe sepsis survivors compared with patients’ own presepsis resource use and the resource use of survivors of otherwise similar nonsepsis hospitalizations.
Methods: This is an observational cohort study of survivors of severe sepsis and nonsepsis hospitalizations identified from participants in the Health and Retirement Study with linked Medicare claims, 1998–2005. We matched severe sepsis and nonsepsis hospitalizations by demographics, comorbidity burden, premorbid disability, hospitalization length, and intensive care use.
Measurements and Main Results: Using Medicare claims, we measured patients’ use of inpatient facilities (hospitals, long-term acute care hospitals, and skilled nursing facilities) in the 2 years surrounding hospitalization. Severe sepsis survivors spent more days (median, 16 [interquartile range, 3–45] vs. 7 [0–29]; P < 0.001) and a higher proportion of days alive (median, 9.6% [interquartile range, 1.4–33.8%] vs. 1.9% [0.0–7.9%]; P < 0.001) admitted to facilities in the year after hospitalization, compared with the year prior. The increase in facility-days was similar for nonsepsis hospitalizations. However, the severe sepsis cohort experienced greater post-discharge mortality (44.2% [95% confidence interval, 41.3–47.2%] vs. 31.4% [95% confidence interval, 28.6–34.2%] at 1 year), a steeper decline in days spent at home (difference-in-differences, −38.6 d [95% confidence interval, −50.9 to 26.3]; P < 0.001), and a greater increase in the proportion of days alive spent in a facility (difference-in-differences, 5.4% [95% confidence interval, 2.8–8.1%]; P < 0.001).
Conclusions: Healthcare use is markedly elevated after severe sepsis, and post-discharge management may be an opportunity to reduce resource use.
Keywords: patient outcomes assessment, hospitalization, patient readmission, skilled nursing facility, healthcare facilities
At a Glance Commentary
Scientific Knowledge on the Subject
The existing literature on healthcare resource use after severe sepsis has focused on documenting the healthcare spending, and other indirect costs, incurred by patients surviving a severe sepsis hospitalization.
What This Study Adds to the Field
Our study adds to the literature in several important ways. First, we provide relevant comparisons with patients’ own baseline resource use, and with the resource use of matched survivors of nonsepsis hospitalizations so that the resource use of severe sepsis survivors can be understood within the appropriate context. Second, rather than measuring use as Medicare spending or other abstract measures of cost, we measure the daily use of inpatient healthcare facilities in the 2 years surrounding hospitalization. We believe this outcome is of high interest to both patients and payers.
Each year, hundreds of thousands of patients in the United States are hospitalized with severe sepsis (1, 2), and a growing number survive to hospital discharge (2–4). Severe sepsis survivors experience increased mortality (5, 6), cognitive and functional decline (7–9), and decreased quality of life (10, 11) that persist for years after their acute illness. The growing population of severe sepsis survivors has been deemed a “hidden public health disaster” (12). Yet, despite rising attention to the long-term consequences of severe sepsis (9, 12), and hospitalization more generally (13–16), newly updated sepsis treatment guidelines have literally no mention of post-discharge care (17).
The Agency for Healthcare Research and Utilization recently reported that the United States spends more money on hospitalizations for sepsis than for any other cause (18), yet the full impact of severe sepsis survivorship on the US healthcare system is unknown. A recent study of survivors of a less common acute illness (those requiring prolonged mechanical ventilation) revealed significant post-discharge care needs (19). Such granular information on the clinical course of severe sepsis survivors is not currently available, despite the larger population and budgetary impact of severe sepsis survivors.
With the growing prominence of readmissions as a subject of attention and potential financial penalties (13, 20), and concern that the burden of illness is shifting to the post–acute care setting (9, 21–23), it has become increasingly important to understand the post-discharge needs of severe sepsis survivors as a health system, beyond the compelling patient-centered reasons. Therefore, we analyzed Medicare claims from a nationally representative cohort of older Americans to quantify the inpatient healthcare use of severe sepsis survivors.
We compared the healthcare use of severe sepsis survivors with their own presepsis resource use to examine the extent to which changes are associated with severe sepsis, rather than simply patients’ propensity to use care (24). By letting patients serve as their own control subjects, we distinguish use associated with severe sepsis from that of patients’ baseline health status, demographic characteristics, and socioeconomic factors that influence healthcare consumption. We also examined the resource use of survivors of matched nonsepsis hospitalizations to understand whether the impact of severe sepsis on subsequent use is different from that of patients with otherwise similar hospitalizations for different reasons. We have previously reported some of these results in an abstract (25).
Methods
Study Population
The Health and Retirement Study (HRS) is an ongoing, nationally representative, prospective cohort study of older Americans (26). Started in 1992, the HRS has enrolled nearly 30,000 participants, of whom 16,772 have agreed to link their data with Medicare (26). The cohort is reinterviewed every 2 years, with a follow-up rate consistently over 90% (26).
Patients provided informed consent on enrollment in the HRS and again for linkage to Medicare. We screened all respondents with a baseline cognitive and physical function assessment (1998–2004) for whom there were claims-based data on a subsequent hospitalization (1998–2005). A similar cohort was identified previously for inclusion in a study of cognitive and functional disability among severe sepsis survivors (7). The University of Michigan institutional review board approved this research.
Identification of Severe Sepsis and Nonsepsis Hospitalizations
We used a commonly employed and externally validated claims-based definition of severe sepsis that requires documentation of infection and acute organ dysfunction during a single hospitalization (1, 27). This definition has a specificity of 96.3% and positive predictive value of 70.7% (27). For patients with more than one severe sepsis hospitalization, each hospitalization was included. We also identified all hospitalizations without severe sepsis within HRS-Medicare (1998–2005). We excluded all hospitalizations with inpatient mortality.
Data Abstraction
We abstracted characteristics of the index hospitalizations from Medicare Provider Analysis and Review (MedPAR) files, including acute organ dysfunctions, critical care use, and mechanical ventilation use (for further details on abstraction of hospitalization characteristics see online supplement). We abstracted baseline deficiencies of activities of daily living (ADLs) and instrumental ADLs from the biennial HRS survey immediately preceding index hospitalization (median, 1.1 yr prior). We determined patients’ baseline Charlson Comorbidity Index (28) score using a 1-year look-back in Medicare claims. We determined enrollment in hospice from the Hospice Standard Analytical File.
Matching of Severe Sepsis and Nonsepsis Hospitalizations
We used a coarsened exact matching approach, because this matching method often achieves the best possible covariate balance while retaining sample size (29). We matched severe sepsis and nonsepsis hospitalizations one-to-one, without replacement, on age, sex, Charlson Comorbidity Index score (28), premorbid limitations of the six ADLs and five instrumental ADLs, length of hospitalization, and intensive care use. For the dichotomous variables, sex and intensive care use, we matched exactly. For Charlson Comorbidity Index score, we matched on whether patients had 0, 1, or 2+ comorbidities. For premorbid limitations, we matched on whether patients had 0, 1, or 2+ total deficiencies of ADLs and instrumental ADLs. For length of hospitalization, we matched on lengths of 1, 2, 3, 4, 5, 6, 7, and 8 to 30, 31 to 60, or 61+ days. For age, we used the default automatic binning algorithm in the user-written “cem” command for Stata (StataCorp, College Station, TX) (30).
Outcomes
Our outcome of interest was use of three types of inpatient healthcare facilities: (1) short-term acute care hospitals (hospitals), (2) long-term acute care hospitals (LTACs) (31), and (3) skilled nursing facilities (SNFs) (32) (definitions provided in Table E1 in online supplement). To measure use, we determined the daily location of each patient for the 365 days preceding index hospitalization and the 365 days after index hospital discharge (or until death) using MedPAR files. Date of death was determined from National Death Index, and confirmed in Medicare denominator files and/or HRS exit interviews.
After determining the daily location of each patient in the 2 years surrounding index hospitalization, we measured the number of days spent at home, in each of the three types of inpatient facilities, and dead. We also determined the number of hospital readmissions and transitions of care locations. We did not include the index hospitalization or transition at index discharge in our use counts.
We considered days at home, days in inpatient facilities, and days dead to be mutually exclusive categories, according to the hierarchy: dead, hospital, LTAC, SNF, home, such that each patient’s total days of use could not exceed their days of observation. In contrast, readmission and transition of care counts measured all use. For example, if a patient was admitted from a SNF to a hospital and died the same day, this day would be coded as “dead” (not in a hospital or SNF), but would count as both a readmission and a transition of care.
We assumed that patients were at home for any day they were known to be alive and not admitted to an inpatient facility based on MedPAR records. Because Medicare does not pay for long-term custodial care provided by nursing facilities, patients residing in a nursing home on a permanent basis cannot be identified on a daily basis through MedPAR records (33, 34). Thus, although our results accurately measure healthcare use through Medicare, they likely underestimate total service use.
Statistical Analysis
We present patient characteristics as numbers (percentages), means (SDs), or medians (interquartile ranges [IQR]) as appropriate. We report mortality as means (95% confidence interval [CI]), use outcomes as medians (IQR), and rates per person-year. To compare use between and within cohorts, we used nonparametric tests to account for the skewed distribution of the outcomes (see online supplement). To compare changes in use between the severe sepsis and nonsepsis cohorts, we performed difference-in-differences analyses (35).
We conducted all analyses with Stata software version 13 (StataCorp). We used hospitalization as the unit of analysis, unless otherwise specified. We used two-sided significance testing and considered a P value less than 0.05 to be significant.
Additional Analyses
We performed a subgroup analysis of the patients who used intensive care during their hospitalization. Also, because of potential temporal changes in in-hospital mortality, SNF use, and LTAC use, we performed a sensitivity analysis in which we matched severe sepsis and nonsepsis hospitalizations by year of hospital admission, in addition to the six other matching variables.
Results
Severe Sepsis and Nonsepsis Cohorts
We identified 1,162 severe sepsis and 23,803 nonsepsis hospitalizations without inpatient mortality (Figure 1). After matching hospitalizations one-to-one on age, sex, premorbid functional limitations, Charlson Comorbidity Index, length of hospitalization, and use of intensive care, we included 1,083 severe sepsis hospitalizations (93.2% of those identified) and 1,083 nonsepsis hospitalizations in the analysis.
Figure 1.
Identification and matching of severe sepsis and nonsepsis cohorts. We measured premorbid disability as the number of limitations in activities and instrumental activities of daily living. HRS = Health and Retirement Study.
In general, the cohorts were older (mean age, 78.6 ± 8.6 yr), predominantly female (53.5%), with a moderate comorbidity burden (mean Charlson Comorbidity Index score, 2.1 ± 1.7), and mild to moderate baseline functional limitations (median total limitations of baseline ADL and instrumental ADLs, 1; IQR, 0–5) (Table 1). Median hospital length of stay was 8 days (IQR, 5–13 d) and 420 patients (38.8%) in each cohort used intensive care during their hospitalization. As expected, the severe sepsis and nonsepsis cohorts did not differ by any of the six matched characteristics.
Table 1.
Demographic Information and Hospitalization Characteristics for Matched Survivors of Severe Sepsis and Nonsepsis Hospitalizations
| Demographic or Hospitalization Characteristic | Severe Sepsis Cohort (n = 1,083) | Nonsepsis Cohort (n = 1,083) | P Value |
|---|---|---|---|
| Matched characteristics | |||
| Age, mean (SD) | 78.5 (8.6) | 78.6 (8.6) | 0.91 |
| Male, n (%) | 503 (46.5) | 503 (46.5) | 1.00 |
| Charlson score, mean (SD) | 2.1 (1.7) | 2.2 (1.8) | 0.93 |
| Premorbid physical disability, median (IQR) | |||
| Basic ADL limitations | 1 (0–3) | 1 (0–3) | 0.53 |
| Instrumental ADL limitations | 0 (0–2) | 0 (0–2) | 0.08 |
| Total ADL limitations | 1 (0–5) | 1 (0–5) | 0.27 |
| Hospital length of stay (d), median (IQR) | 8 (5–14) | 8 (5–12) | 0.11 |
| Used an intensive care unit, n (%) | 420 (38.8) | 420 (38.8) | 1.00 |
| Unmatched characteristics | |||
| Self-reported race/ethnicity, n (%) | 0.51 | ||
| White | 841 (77.7) | 860 (79.4) | |
| Black/African American | 219 (20.2) | 198 (18.3) | |
| Other | 23 (2.1) | 24 (2.2) | |
| Premorbid cognitive function, n (%) | 0.01 | ||
| Normal | 911 (84.1) | 945 (87.3) | |
| Mild Impairment | 89 (8.2) | 54 (5.0) | |
| Moderate/severe impairment | 83 (7.7) | 84 (7.8) | |
| Received mechanical ventilation, n (%) | 210 (19.4) | 29 (2.7) | <0.01 |
Definition of abbreviations: ADL = activity of daily living; IQR = interquartile range.
The sepsis cohort experienced a mean of 1.1 ± 0.4 acute organ dysfunctions. Of the 1,083 severe sepsis hospitalizations, 452 (41.7%) had renal dysfunction, 252 (23.3%) had cardiovascular dysfunction, 211 (19.5%) had hematologic dysfunction, 210 (19.4%) had respiratory dysfunction, 104 (9.6%) had neurologic dysfunction, and 7 (0.7%) had hepatic dysfunction.
The 77 (6.6%) unmatched severe sepsis hospitalizations were younger, had longer hospitalizations, and were more likely to use intensive care than the severe sepsis hospitalizations included in the analysis (see Table E2). Compared with the matched hospitalization, the unmatched severe sepsis hospitalizations had similar presepsis use, but greater post-sepsis use and greater mortality.
Mortality, Place of Death, and Hospice Use
The severe sepsis cohort experienced 27.5% 90-day mortality (95% CI, 24.8–30.2%) and 44.2% 1-year mortality (95% CI, 41.3–47.2%), markedly higher than the nonsepsis cohort who experienced 15.5% 90-day (95% CI, 13.4–17.7%) and 31.4% 1-year mortality (95% CI, 28.6–34.2%) (P < 0.01 for each time-point).
Of the 479 severe sepsis patients who died in the year after hospitalization, 231 (48.2%) died at home, 162 (33.8%) died in a hospital, and 86 (18.0%) died in a SNF or LTAC. One hundred sixty-two (33.8%) enrolled in hospice before their death. For nonsepsis patients who died in the year after hospitalization, death location and proportion enrolled in hospice were similar to the severe sepsis cohort (P > 0.05 for each).
Healthcare Use in the Year after Severe Sepsis
The 1,083 severe sepsis survivors required substantial healthcare resources in the year after hospitalization (see Table E3). On average, they spent a median 16 days (IQR, 2–45) or 9.6% (IQR, 1.4–33.8%) of their days alive in the year after discharge admitted to an inpatient healthcare facility. Mean use is presented in Table E4.
Two hundred eighty-seven (26.5%) were readmitted within 30 days of hospital discharge, 444 (41.0%) were readmitted within 90 days, and 682 (63.0%) were readmitted at some point in the first year. Three hundred sixty-one (33.3%) were readmitted more than once during the year. Only 222 (20.5%) of the severe sepsis survivors remained alive for 1 year after discharge without being readmitted to a hospital.
Visual inspection of patients’ daily use in the year after severe sepsis hospitalization suggests that much of the increased healthcare use occurs in the first 90 days (Figure 2B). Indeed, severe sepsis survivors spent a median 9 (IQR, 0–28) days admitted to a healthcare facility in the first 90 days after hospital discharge, compared with a median 0 days (IQR, 0–13) in days 91–365 (P < 0.001). Severe sepsis survivors were hospitalized at a rate of 2.94 hospitalization per patient-year in the first 90 days, compared with 1.54 hospitalization per patient-year in the 91–365 days after hospital discharge.
Figure 2.
Use and mortality for 1,083 matched survivors in the 2 years surrounding severe sepsis and nonsepsis hospitalizations. This figure displays the daily location of 1,083 matched survivors of severe sepsis and nonsepsis hospitalizations in the 1 year before (A and C) and 1 year after hospitalization (B and D). The index admission is not included. The year prior ends at the day before hospitalization; the year after begins the day after hospital discharge. Patients are depicted as being at home (blue), admitted to a healthcare facility (red), or dead (black).
We present use counts and rates for specific components of care in Tables E3–E5.
Healthcare Use before and after Severe Sepsis
The healthcare use of the severe sepsis survivors surpassed their own baseline presepsis healthcare use. Patients spent more days (median, 16 [IQR, 3–45] vs. 7 [0–29]; P < 0.001) and a markedly higher proportion of their days alive (median, 9.6% [IQR, 1.4–33.8%] vs. 1.9% [0.0–7.9%]; P < 0.001) admitted to an inpatient healthcare facility in the year after compared with the year before severe sepsis hospitalization. The rate of hospitalization increased from 1.44 hospitalizations per patient-year before severe sepsis to 1.95 hospitalizations per patient-year after severe sepsis. The rate of inpatient healthcare use increased from 24.2 days per patient-year presevere sepsis to 47.9 days per patient-year post-severe sepsis.
Changes in Healthcare Use after Severe Sepsis versus Nonsepsis Hospitalizations: A Difference-in-Differences Analysis
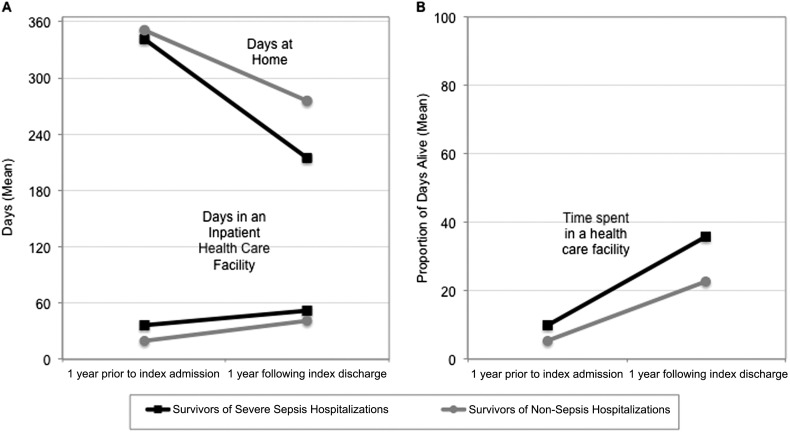
The change in facility-days was similar in the severe sepsis and nonsepsis cohorts (Figure 3, Table 2). However, as a result of the increased post-discharge mortality experienced by the severe sepsis cohort, severe sepsis survivors had a steeper decline in the number of days spent at home (difference-in-differences, −38.6 d [95% CI, −50.9 to 26.3]; P < 0.001) and a steeper rise in the proportion of days alive spent admitted to an inpatient healthcare facility (difference-in-differences, 5.4% [95% CI, 2.8–8.1%]; P < 0.001).
Figure 3.
Difference-in-differences analysis of healthcare use in the severe sepsis and nonsepsis cohorts. The difference-in-differences between the severe sepsis and nonsepsis cohorts was (A) −38.6 days spent at home (95% confidence interval [CI], −50.9 to −26.3 d; P < 0.001), and (B) +5.4% of days alive spent in an inpatient healthcare facility (95% CI, +2.8 to +8,1%; P < 0.001). The difference-in-differences for days spent in a healthcare facility was not significant (−4.2 d; 95% CI, −9.0 to +0.7 d; P = 0.09).
Table 2.
Difference-in-Differences Analyses Comparing Changes in Healthcare Use between the Severe Sepsis and Nonsepsis Cohorts*
| Primary Cohorts (1,083 Matched
Pairs) |
ICU Subgroup (420 Matched
Pairs) |
Year-matched Cohorts (795 Matched
Pairs) |
||||
|---|---|---|---|---|---|---|
| DID Estimate (95% CI) | P Value | DID Estimate (95% CI) | P Value | DID Estimate (95% CI) | P Value | |
| Days at home | −38.6 (−50.9 to −26.3) | <0.01 | −43.6 (−63.4 to −23.7) | <0.01 | −33.9 (−48.4 to −19.4) | <0.01 |
| Days in an inpatient facility | −4.2 (−9.0 to 0.7) | 0.09 | −2.5 (−10.4 to 5.5) | 0.54 | −3.2 (−8.8 to 2.4) | 0.26 |
| Days in a hospital | −1.9 (−4.0 to 0.2) | 0.08 | −2.5 (−6.1 to 1.1) | 0.18 | −1.2 (−3.6 to 1.1) | 0.31 |
| Days in an LTAC | 0.1 (−0.8 to 1.0) | 0.87 | −0.3 (−2.2 to 1.5) | 0.72 | 1.2 (0.3 to 2.2) | 0.01 |
| Days in a SNF | −2.4 (−6.0 to 1.3) | 0.20 | 0.4 (−5.2 to 5.9) | 0.90 | −3.2 (−7.5 to 1.1) | 0.14 |
| Transitions of care location | −0.6 (−1.0 to −0.2) | 0.01 | −0.6 (−1.3 to 0.2) | 0.13 | −0.5 (−1.0 to −0.2) | 0.04 |
| Proportion of days alive in an inpatient facility | 5.4% (2.8 to 8.1%) | <0.01 | 7.8% (3.3 to 12.3%) | <0.01 | 4.1% (0.9 to 7.3%) | 0.01 |
Definition of abbreviations: CI = confidence interval; DID = difference-in-differences; ICU = intensive care unit; LTAC = long-term acute care hospital; SNF = skilled nursing facility.
For each of the three analyses presented here, the severe sepsis and nonsepsis cohorts are matched on age, sex, premorbid disability, Charlson score for comorbidities, length of hospitalization, and whether or not intensive care was used for any portion of the hospitalization. The ICU subgroup is the subset of the primary analysis that used intensive care. The year-matched cohorts were matched on year, in addition to the other six matching variables, and are not a subset of the primary cohort.
Subgroup Analysis: Hospitalizations with Intensive Care Use
The 420 (38.8%) severe sepsis hospitalizations that used intensive care had increases in use of a similar magnitude to the whole cohort (see Table E6). The difference-in-differences analysis for the 420 matched severe sepsis and nonsepsis hospitalizations was similar to the difference-in-differences analysis for the full cohorts (Table 2).
Sensitivity Analysis: Matching on Year
We were able to match 795 (68.4%) of the severe sepsis hospitalizations to nonsepsis hospitalizations by year of admission, in addition to the six other matching variables. The results of pre versus post and difference-in-differences analyses for the year-matched cohorts were not substantially different from the primary analysis (Table 2; see Table E7).
Discussion
Using a nationally representative cohort of older adults, we have shown that the inpatient healthcare facility use of severe sepsis survivors is markedly elevated compared with patients’ own presepsis healthcare use. In the year after a severe sepsis hospitalization, patients spent a median of 10% (mean, 25%) of their days alive admitted to an inpatient healthcare facility (a hospital, LTAC, or SNF). Most patients were rehospitalized, many more than once. Only one in five severe sepsis survivors remained alive for a full year after severe sepsis without being rehospitalized.
When compared with survivors of nonsepsis hospitalizations, severe sepsis survivors had similar increases in use, but greater mortality, a steeper decline in days spent at home, and a more dramatic rise in the proportion of days alive spent in an inpatient healthcare facility.
Our analysis provides two complementary perspectives on healthcare use after severe sepsis. The before versus after severe sepsis comparison (also known as within-person analysis) addresses the question: does severe sepsis represent an important change in patients’ healthcare use? The answer is a compelling “yes” with, for example, inpatient days increasing from 24.2 per patient-year before severe sepsis to 47.9 days per patient-year after severe sepsis. The comparison to matched nonsepsis hospitalizations addresses the question: is severe sepsis particularly worse in its disruption to patients’ premorbid use than other illnesses with comparably severe inpatient stays? The answer here is more nuanced, with severe sepsis associated with much worse ongoing mortality, a finding that has been seen in many studies (5, 11), but similar changes in absolute healthcare needs relative to other similar hospitalizations. Altogether, we interpret this as meaning that severe sepsis is followed by a significant increased burden of healthcare use, but that increase is not uniquely worse than other severe illnesses requiring significant hospitalization.
Only 39% of the patients in our study were treated in an intensive care unit. Our findings suggest that patients with severe sepsis, even the majority who do not require intensive care unit admission, often need prolonged and recurrent care in inpatient facilities after hospital discharge. Our findings are consistent a recent study by Liu and coworkers (36) demonstrating that sepsis survivors spend a threefold higher proportion of days alive admitted to a healthcare facility in the year after sepsis hospitalization compared with before. They are also consistent with prior studies that have quantified post-sepsis resource use (37–42), but have not included clear comparisons, control for presepsis healthcare use, or a focus on patient-centered transitions of care.
With the mounting attention on repeat admissions as a quality measure and potentially preventable expense for healthcare systems (13, 20), severe sepsis may be an important opportunity for targeted interventions. The rate of repeat hospitalization observed in our study exceeds the average readmission rate for Medicare beneficiaries (13, 43) and the rate observed in our matched nonsepsis hospitalizations, suggesting that severe sepsis survivors may benefit from more intensive post-discharge care management. This might include improved coordination of care, more frequent geriatric medicine involvement to help with new disabilities and functional limitations, support for caretakers (44), or an increased focus on in-hospital maintenance of the ability to live independently.
As the case fatality rate for severe sepsis continues to decline (45), it is important to consider additional metrics to measure the quality of care provided to severe sepsis patients. Post-discharge healthcare use is an attractive metric for several reasons. First, it is meaningful to patients whether, and to what extent, they need to spend time in LTACs and SNFs. Second, to decrease case fatality rates, hospitals may selectively transfer patients to post–acute care facilities, such as LTACs and SNFs (21), shifting the burden of severe sepsis to less studied silos. Third, post–acute care facility use represents the largest source of variation in healthcare spending across the United States (46), so it is worthy of study in and of itself. Thus, we urge researchers to consider post-discharge use as an important outcome for future observational and interventional studies of severe sepsis patients.
Our study has several potential limitations. We analyzed inpatient healthcare use through Medicare claims. Because of this, we were unable to assess long-term residence in nursing homes that is not covered by Medicare. In addition, we have not quantified informal care needs. Therefore, our results underestimate the magnitude of severe sepsis survivors’ total needs (7), concentrating instead on those most relevant to the public cost of severe sepsis. We were not able to assess the extent to which an integrated health system may reduce healthcare use. Rather, our results focus on Medicare, the only data source with national scale and the payer for more than half of severe sepsis hospitalizations (47).
We excluded 7% of the severe sepsis sample because they could not be matched to nonsepsis hospitalizations using our matching algorithm. The excluded severe sepsis hospitalizations had similar baseline use to those included in the analysis. However, they had notably higher use and mortality in the year after severe sepsis. As such, our estimates may underestimate the true impact of severe sepsis on subsequent use. This decision was made so that a consistent group of severe sepsis patients was used for all comparisons.
Conclusions
We have shown that healthcare use of severe sepsis survivors is markedly elevated relative to their own premorbid resource use. The change in resource use was similar to that of otherwise similar nonsepsis hospitalizations. This finding suggests that, after controlling for comorbidity burden and functional limitations, much of a patient’s subsequent use can be attributed to severity of illness and hospitalization. That is, severe sepsis may be a sufficient cause for a substantial increase in healthcare needs, but it is not a uniquely necessary cause of such an increase relative to other severe illnesses. However, severe sepsis survivors experienced increased mortality relative to matched nonsepsis survivors. As a result, severe sepsis survivors spent a greater proportion of their days alive admitted to an inpatient healthcare facility and far fewer days at home in the year after hospital discharge. Our findings suggest a need for greater attention to the post-discharge management of severe sepsis survivors and further investigation into the excess mortality experienced by this population. As the case fatality rate for severe sepsis continues to fall, we believe it would be worthwhile to measure post-discharge use in studies of severe sepsis outcomes.
Acknowledgments
Acknowledgment
The Health and Retirement Study is performed at the Institute for Social Research, University of Michigan. We appreciate the expert programming of Laetitia Shapiro, M.S., and Ryan McCammon, M.S., at the University of Michigan. Dr. Prescott has had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Supported by grants K08 HL091249, R01 AG030155, U01 AG09740, and T32 HL007749 from the National Institutes of Health, and IIR 11-109 from the Department of Veterans Affairs Health Services Research and Development Service.
Author Contributions: H.C.P. designed the study, performed the statistical analyses, interpreted the results, and compiled the manuscript. T.J.I. designed the study, requested relevant data from the Health and Retirement Study, refined the analyses, assisted in interpreting the findings, and provided critical revisions of the manuscript. V.L., G.J.E., and K.M.L. helped interpret the results and provided critical revisions for the manuscript.
Originally Published in Press as DOI: 10.1164/rccm.201403-0471OC on May 28, 2014
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Iwashyna TJ, Cooke CR, Wunsch H, Kahn JM. Population burden of long-term survivorship after severe sepsis in older Americans. J Am Geriatr Soc. 2012;60:1070–1077. doi: 10.1111/j.1532-5415.2012.03989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar G, Kumar N, Taneja A, Kaleekal T, Tarima S, McGinley E, Jimenez E, Mohan A, Khan RA, Whittle J, et al. Milwaukee Initiative in Critical Care Outcomes Research Group of Investigators. Nationwide trends of severe sepsis in the 21st century (2000-2007) Chest. 2011;140:1223–1231. doi: 10.1378/chest.11-0352. [DOI] [PubMed] [Google Scholar]
- 4.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 5.Quartin AA, Schein RM, Kett DH, Peduzzi PN Department of Veterans Affairs Systemic Sepsis Cooperative Studies Group. Magnitude and duration of the effect of sepsis on survival. JAMA. 1997;277:1058–1063. [PubMed] [Google Scholar]
- 6.Wunsch H, Guerra C, Barnato AE, Angus DC, Li G, Linde-Zwirble WT. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA. 2010;303:849–856. doi: 10.1001/jama.2010.216. [DOI] [PubMed] [Google Scholar]
- 7.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guerra C, Linde-Zwirble WT, Wunsch H. Risk factors for dementia after critical illness in elderly Medicare beneficiaries. Crit Care. 2012;16:R233. doi: 10.1186/cc11901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yende S, Angus DC. Long-term outcomes from sepsis. Curr Infect Dis Rep. 2007;9:382–386. doi: 10.1007/s11908-007-0059-3. [DOI] [PubMed] [Google Scholar]
- 10.Karlsson S, Ruokonen E, Varpula T, Ala-Kokko TI, Pettilä V Finnsepsis Study Group. Long-term outcome and quality-adjusted life years after severe sepsis. Crit Care Med. 2009;37:1268–1274. doi: 10.1097/CCM.0b013e31819c13ac. [DOI] [PubMed] [Google Scholar]
- 11.Winters BD, Eberlein M, Leung J, Needham DM, Pronovost PJ, Sevransky JE. Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med. 2010;38:1276–1283. doi: 10.1097/CCM.0b013e3181d8cc1d. [DOI] [PubMed] [Google Scholar]
- 12.Angus DC. The lingering consequences of sepsis: a hidden public health disaster? JAMA. 2010;304:1833–1834. doi: 10.1001/jama.2010.1546. [DOI] [PubMed] [Google Scholar]
- 13.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 14.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304:1919–1928. doi: 10.1001/jama.2010.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krumholz HM. Post-hospital syndrome: an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, et al. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 18.Torio CM, Andrews RM.National inpatient hospital costs: the most expensive conditions by payer, 2011HCUP Statistical Brief #160. Rockville, MD: Agency for Healthcare Research and Quality2013Aug [PubMed] [Google Scholar]
- 19.Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, Clay AS, Chia J, Gray A, Tulsky JA, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153:167–175. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–505. doi: 10.1001/jama.2011.72. [DOI] [PubMed] [Google Scholar]
- 21.Hall WB, Willis LE, Medvedev S, Carson SS. The implications of long-term acute care hospital transfer practices for measures of in-hospital mortality and length of stay. Am J Respir Crit Care Med. 2012;185:53–57. doi: 10.1164/rccm.201106-1084OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahn JM, Benson NM, Appleby D, Carson SS, Iwashyna TJ. Long-term acute care hospital utilization after critical illness. JAMA. 2010;303:2253–2259. doi: 10.1001/jama.2010.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahn JM, Kramer AA, Rubenfeld GD. Transferring critically ill patients out of hospital improves the standardized mortality ratio: a simulation study. Chest. 2007;131:68–75. doi: 10.1378/chest.06-0741. [DOI] [PubMed] [Google Scholar]
- 24.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118:219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 25.Prescott HC, Langa KL, Iwashyna TJ. Post-discharge health care use is markedly higher in survivors of severe sepsis. Am J Respir Crit Care Med. 2013;187:A1573. [Google Scholar]
- 26.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JWR, Weir DR. Cohort profile: the Health and Retirement Study (HRS) Int J Epidemiol. 2014;43:576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iwashyna TJ, Odden A, Rohde J, Bonham C, Kuhn L, Malani P, Chen L, Flanders S.Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus Implementation of the International Consensus Conference Definition of Severe Sepsis. Med Care201452e39–e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 29.King G, Neilsen R, Coberley C, Pope JE, Wells A.Comparative effectiveness of matching methods for causal inference. 2011[accessed 2014 May 1]. Available from: http://gking.harvard.edu/files/gking/files/psparadox.pdf
- 30.Blackwell M, Iacus S, King G, Porro G. cem: Coarsened Exact Matching in Stata. Stata J. 2009;9:524–546. [Google Scholar]
- 31.Munoz-Price LS. Long-term acute care hospitals. Clin Infect Dis. 2009;49:438–443. doi: 10.1086/600391. [DOI] [PubMed] [Google Scholar]
- 32.CMSMedicare coverage of skilled nursing facility care. 2014[accessed 2014 March 4]. Available from: http://www.medicare.gov/pubs/pdf/10153.pdf
- 33.Iwashyna TJ. On the detection of nursing home use in Medicare claims. Health Serv Outcomes Res Methodol. 2003;4:187–196. [Google Scholar]
- 34.Yun H, Kilgore ML, Curtis JR, Delzell E, Gary LC, Saag KG, Morrisey MA, Becker D, Matthews R, Smith W, et al. Identifying types of nursing facilities using Medicare claims data: an algorithm and validation. Health Serv Outcomes Res Methodol. 2010;10:100–110. [Google Scholar]
- 35.Abadie A. Semiparametric difference-in-difference estimators. Rev Econ Stud. 2005;72:1–19. [Google Scholar]
- 36.Liu V, Lei X, Prescott HC, Kipnis P, Iwashyna TJ, Escobar GJ.Hospital readmission and healthcare utilization following sepsis in community settings J Hosp Med(In press) [DOI] [PMC free article] [PubMed]
- 37.Dick A, Liu H, Zwanziger J, Perencevich E, Furuya EY, Larson E, Pogorzelska-Maziarz M, Stone PW. Long-term survival and healthcare utilization outcomes attributable to sepsis and pneumonia. BMC Health Serv Res. 2012;12:432. doi: 10.1186/1472-6963-12-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weycker D, Akhras KS, Edelsberg J, Angus DC, Oster G. Long-term mortality and medical care charges in patients with severe sepsis. Crit Care Med. 2003;31:2316–2323. doi: 10.1097/01.CCM.0000085178.80226.0B. [DOI] [PubMed] [Google Scholar]
- 39.Lee H, Doig CJ, Ghali WA, Donaldson C, Johnson D, Manns B. Detailed cost analysis of care for survivors of severe sepsis. Crit Care Med. 2004;32:981–985. doi: 10.1097/01.ccm.0000120053.98734.2c. [DOI] [PubMed] [Google Scholar]
- 40.Braun L, Riedel AA, Cooper LM. Severe sepsis in managed care: analysis of incidence, one-year mortality, and associated costs of care. J Manag Care Pharm. 2004;10:521–530. doi: 10.18553/jmcp.2004.10.6.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Letarte J, Longo CJ, Pelletier J, Nabonne B, Fisher HN. Patient characteristics and costs of severe sepsis and septic shock in Quebec. J Crit Care. 2002;17:39–49. doi: 10.1053/jcrc.2002.33028. [DOI] [PubMed] [Google Scholar]
- 42.Schmid A, Burchardi H, Clouth J, Schneider H. Burden of illness imposed by severe sepsis in Germany. Eur J Health Econ. 2002;3:77–82. doi: 10.1007/s10198-002-0095-8. [DOI] [PubMed] [Google Scholar]
- 43.Wier LM.Barrett ML, Steiner C, Jiang HJ. All-cause readmissions by payer and age, 2008. HCUP Statistical Brief #115. Rockville, MD: Agency for Healthcare Research and Quality; 2011 Jun [accessed 2013 Jan 30]. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb115/pdf [PubMed]
- 44.Davydow DS, Hough CL, Langa KM, Iwashyna TJ. Depressive symptoms in spouses of older patients with severe sepsis. Crit Care Med. 2012;40:2335–2341. doi: 10.1097/CCM.0b013e3182536a81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42:625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.2013. Institute of Medicine. Variation in health care spending: target decision making, not geography. Washington, DC: The National Academies Press.
- 47.Elixhauser A, Friedman B, Stranges E.Septicemia in US hospitals, 2009. HCUP Statistical Brief #122. Rockville, MD: Agency for Healthcare Research and Quality; 2011. Oct [accessed 2013 Jan 23]. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb122.pdf [PubMed]