Abstract
Background
Underrepresentation of minorities within academic surgery is an ever present problem with a profound impact on healthcare. The factors influencing surgery residents to pursue an academic career have yet to be formally investigated. We sought to elucidate these factors, with a focus on minority status.
Methods
A web-based questionnaire was sent to all administered to all ACGME-accredited general surgery programs in the United States. The main outcome was the decision to pursue a fully academic versus non-academic career. Multivariable logistic regression was used to identify characteristics impacting career choice.
Results
Of the 3,726 residents who received the survey, a total of 1,217 residents completed it – a response rate of 33%. Forty-seven percent planned to pursue non-academic careers, 35% academic careers, and 18% were undecided. There was no association between underrepresented minority status and academic career choice (Odds Ratio = 1.0, 95% Confidence Interval 0.6 – 1.6). Among all residents, research during training (OR=4.0, 95% CI 2.7-5.9), mentorship (OR=2.1, 95% CI 1.6-2.9), and attending a residency program requiring research (OR=2.3, 95% CI 1.5-3.4) were factors associated with choosing an academic career. When the analysis was performed among only senior residents (i.e., 4th and 5th year residents), a debt burden >$150,000 was associated with choosing a non-academic career (OR=0.4, 95% CI 0.1-0.9).
Conclusions
Underrepresented minority status is not associated with career choice. Intentional recruitment of minorities into research-oriented training programs, increased mentorship and research support among current minority residents, and improved financial options for minorities may increase the number choosing an academic surgical career.
Keywords: Academic surgery, survey, underrepresented minorities, career choice
Introduction
Underrepresentation of minority groups in medicine is well documented. Within the academic setting, minority faculty in predominantly white medical schools comprise only 7.3% of all faculty [1]. This disparity is even more apparent within academic surgery, where African Americans and Hispanic Americans comprise less than 3% and 4% of academic surgical faculty, respectively [2]. Historically, the field of surgery has been burdened with racial disparities limiting the mentorship needed to recruit and develop a diverse surgical workforce. However, the scope of this problem far outreaches the demographic distribution of surgical faculty – the nation's research agenda is largely shaped by physicians and scientists with research-oriented careers practicing in academic centers. It has been suggested that increasing diversity in research would allow for an expansion of this agenda to better address minority-specific issues, which in turn would enhance patient care and broaden the range of potential solutions for eliminating health disparities.[1]
Several factors have been noted to influence medical student career choices, such as mentorship and role models[3-6], debt[7], and even mistreatment during medical school.[8] There have also been studies documenting that minority faculty in academia are more frequently unhappy in their position than non-minorities, and consider it substantially more difficult to advance [9, 10]. However, it is during residency or fellowship where most physicians decide their ultimate career path – whether it be private practice, academia, or some combination of the two. There are studies demonstrating that mentorship plays a positive and important role in surgery resident subspecialty selection [11, 12], but there has been no systematic evaluation of the factors influencing surgery residents' decision to pursue an academic or non-academic career. This is an important gap in the knowledge needed to properly address the ever present problem of underrepresentation for certain groups in academic surgery. Once we understand the factors and influences on career path choices, we will be better suited to develop appropriate interventions that might remove barriers perpetuating such discrepancies.
We conducted a nationwide survey of general surgery residents to determine factors influencing their decision to pursue a fully academic versus non-academic career. We hypothesized that race/ethnicity would be associated with career choice, and that underrepresented minorities would more frequently pursue non-academic careers.
Methods
Questionnaire
A web-based questionnaire was developed to ascertain the following information: demographics (age, gender, race/ethnicity, marital status, number of children, foreign medical graduate status), program level information (name of program, year in training), career trajectory (type of practice planned, interest in underserved population), professional factors (mentorship, research experience, prior advanced degrees), and socioeconomic factors (debt burden, presence of a physician in the family, highest level of parental education). There was also a subset of questions evaluating the amount of subjective influence certain factors had on their career decisions. The questionnaire consisted of a total of 43 questions, and was designed to take only 2 to 3 minutes to complete.
Study data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at Vanderbilt University Medical Center.[13] REDCap is a secure, web-based application designed to support data capture for research studies. The Vanderbilt University Institutional Review Board approved this study.
Population
The survey was sent to the program directors and coordinators of all Accreditation Council for Graduate Medical Education (ACGME)-accredited general surgery residency programs in the US (243 programs, approximately 7,357 residents).[14, 15] The survey was not sent to our own institution's general surgery program to prevent obtaining biased responses from residents involved in the development of the questionnaire. We did not have individual contact information for survey participants, thus the distribution of the survey was dependent on the program coordinators' willingness to forward the survey link to their residents.
Analysis
Program-level non-response bias was investigated using univariate analyses to compare programs that responded with those that did not. Continuous variables were compared between groups using the Student's t-test, and categorical variables were compared using Pearson's chi-square test. The generalizability of individual responses was assessed by comparing the demographic breakdown of respondents with national demographic data for all general surgery residents in the United States, as published in 2011 by the American Medical Association (AMA) and American Association of Medical Colleges' (AAMC)[16].
The primary outcome was the resident's plan to pursue a fully academic (versus non-academic) career, as determined by the response to the following question, “What type of practice are you planning to enter upon completion of your training?” The answer choices (respondents could choose more than one) were: academic, private, private with academic affiliation, international service, military, Veterans Affairs, and undecided. All responses other than “academic” were considered non-academic. Responses with multiple practice types selected were considered undecided, and all undecided respondents (N=220) were excluded from analyses. Respondent characteristics were compared between those choosing academic and non-academic practice using Pearson's chi-square test for categorical variables and the Student's t-test for continuous variables. A logistic regression model was created to evaluate the factors independently associated with choosing academic surgery. Covariates included self-reported race/ethnicity, age, gender, whether or not the resident had children, foreign medical graduate status, highest level of parental education, whether or not there was a physician in the family, presence of additional professional degrees, amount of debt, year in residency training, presence of a mentor, dedicated research time, whether there was a primary interest in caring for an underserved population, and whether the residency program required research. This model was used to assess all residents, as well as only the fourth- and fifth-year (i.e., senior) residents.
As a separate analysis, we evaluated the subjective influence of several factors on residents' decision to pursue academic or non-academic practice. Respondents were asked “How much did the following factors influence your decision to pursue the particular type of practice you chose?” For each of the 10 influence variables (income potential, parental/family influence, mentor, debt burden, patient population, current family situation, lifestyle, your personality, cultural influences, and research experience) they used a visual sliding scale to select a point between “Not at all” (zero) and “The most important factor” (100). Each influence was analyzed as a continuous variable. The mean score for each influence variable were compared between respondents choosing academic versus non-academic careers using the Student's t-test with a Bonferroni correction (0.05/10) for multiple comparisons.
Results
The questionnaire was sent to a total of 3,726 residents, and 1,247 residents completed the survey. Of the completed questionnaires, 13 duplicate submissions and one empty submission were excluded. There were 16 respondents excluded from institutions with distribution practices that deviated from the protocol. This resulted in a total of 1,217 respondents eligible for analyses. The resident response rate was therefore 33% (1,217/3,726). The program-level response rate was 44% (107/243 programs participated). Of the 1,217 respondents, 574 (57.6%) planned to pursue a non-academic career, 422 (42.4%) planned to pursue a fully academic career, 220 were undecided, and 1 respondent did not answer the question. Undecided residents were excluded from our analyses, resulting in a total of 996 respondents included in the analyses.
There was no evidence of non-response bias at the program-level (Table I). The racial/ethnic and gender distribution of the national pool of general surgery residents, as reported by the AMA/AAMC in 2011, was based on a total of 7,671residents in ACGME-accredited general surgery training programs. There were 4806 (62.7%) White, 635 (8.3%) Hispanic, 549 (7.2%) Black, 43 (0.6%) American Indian/Alaskan, 1652 (21.5%) Asian, 14 (0.2%) Hawaiian/Pacific Islander, and 607 (7.9%) Other[16]. The demographics of our study population of 1,217 respondents, as shown in Table 2, closely resemble the AMA/AAMC demographic distribution (Figure 1).
Table 1. Program-level Non-response Assessment.
| All Programs N=243 |
Responded N=107 |
Did Not Respond N=136 |
p-value | |
|---|---|---|---|---|
| Mean # Residents Per Program, (SD) | 30 (15) | 31 (15) | 29 (15) | 0.33 |
| Research Required, N (%) | 34 (14) | 10 (9) | 24 (18) | 0.06 |
| VA-affiliated, N (%) | 83 (34) | 38 (36) | 45 (33) | 0.69 |
| Mean NIH Funds in year 2010 | $1,129,724 | $ 985,950 | $1,242,840 | 0.52 |
| US Region, N (%) | 0.53 | |||
| Northeast | 74 (30) | 35 (33) | 39 (29) | |
| Midwest (Central) | 55 (23) | 26 (24) | 29 (21) | |
| South | 77 (32) | 34 (32) | 43 (32) | |
| West | 36 (15) | 12 (11) | 24 (18) |
Table 2. Resident Characteristics of Respondents.
| Characteristic | All Respondents | Non-Academic | Academic | p-value |
|---|---|---|---|---|
| Total, No (%) | 1217 (100) | 574 (57.6)* | 422 (42.4)* | -- |
| Career Plan | ||||
| Practice Type | ||||
| Academic only | 422 (34.7) | 422 | -- | |
| Private only | 181 (14.9) | 181 | -- | |
| Private w/ academic affiliation | 350 (28.8) | 350 | -- | |
| International | 21 (1.7) | 21 | -- | |
| Military | 22 (1.8) | 22 | -- | |
| VA | 0 | 0 | -- | |
| Undecided | 220 (18) | -- | ||
| Missing | 1 (0.1) | |||
| Demographics | ||||
| Age, yrs; mean (SD) | 30.4 (3.2) | 30.3 (3) | 30.7 (3.4) | 0.08 |
| Gender; No (%) | 0.82 | |||
| Male | 752 (61.8) | 373 (65) | 270 (64.3) | |
| Female | 462 (38) | 201 (35) | 150 (35.7) | |
| Missing | 3 (0.2) | 0 | 2 | |
| Race/Ethnicity | 0.10 | |||
| White | 781 (64.2) | 381 (66.6) | 259 (61.4) | |
| Hispanic | 71 (5.8) | 33 (5.8) | 24 (5.7) | |
| Black | 51 (4.2) | 25 (4.4) | 16 (3.8) | |
| American Indian/Alaskan | 0 | 0 | 0 | |
| Asian | 200 (16.4) | 92 (16.1) | 72 (17.1) | |
| Hawaiian/Pacific Islander | 0 | 0 | 0 | |
| Other | 112 (9.2) | 41 (7.2) | 51 (12.1) | |
| Missing | 2 (0.2) | 2 | 0 | |
| Number of Children; N (%) | 0.08 | |||
| 0 | 924 (75.9) | 415 (72.4) | 326 (77.2) | |
| 1 | 157 (12.9) | 76 (13.3) | 53 (12.6) | |
| 2 | 93 (7.6) | 53 (9.2) | 34 (8.1) | |
| 3+ | 42 (3.5) | 29 (5.1) | 9 (2.1) | |
| Missing | 1 (0.1) | 1 | 0 | |
| Pre-Residency Experience | ||||
| Highest Parental Education | 0.37 | |||
| < High School | 16 (1.3) | 10 (1.7) | 5 (1.2) | |
| GED | 4 (0.3) | 2 (0.3) | 0 | |
| High School | 77 (6.3) | 34 (5.9) | 32 (7.6) | |
| Some College | 109 (9) | 52 (9.1) | 35 (8.3) | |
| College Degree | 303 (24.9) | 145 (25.3) | 90 (21.3) | |
| Graduate Degree | 708 (58.2) | 331 (57.7) | 260 (61.6) | |
| Physician in family | 0.90 | |||
| No | 754 (62) | 358 (62.5) | 262 (62.1) | |
| Yes | 461 (37.8) | 215 (37.5) | 160 (37.9) | |
| Missing | 2 (0.2) | 1 | 0 | |
| Additional Degree(s) | 0.03 | |||
| No | 985 (80.9) | 476 (82.9) | 327 (77.5) | |
| Yes | 232 (19.1) | 98 (17.1) | 95 (22.5) | |
| Foreign Medical Graduate | 0.01 | |||
| No | 987 (81.1) | 475 (82.7) | 321 (76.1) | |
| Yes | 230 (18.9) | 99 (17.3) | 101 (23.9) | |
| Debt Burden | 0.02 | |||
| None | 521 (20.6) | 108 (18.8) | 103 (24.4) | |
| < $100,000 | 166 (13.6) | 70 (12.2) | 68 (16.1) | |
| $100,001 – 150,000 | 159 (13.1) | 71 (12.4) | 57 (13.5) | |
| $150,001 – 200,000 | 282 (23.2) | 139 (24.2) | 87 (20.6) | |
| > $200,000 | 359 (29.5) | 186 (32.4) | 107 (25.4) | |
| Within-Residency Experience | ||||
| Mentor | <0.001 | |||
| No | 513 (42.2) | 278 (48.4) | 124 (29.4) | |
| Yes | 704 (57.8) | 296 (51.6) | 298 (70.6) | |
| Dedicated Research Time | <0.001 | |||
| No | 900 (73.9) | 483 (84.3) | 242 (57.3) | |
| Yes | 316 (26) | 90 (15.7) | 180 (42.7) | |
| Missing | 1 (0.1) | 1 | 0 | |
| Year in Training | 0.01 | |||
| 1st Year | 395 (32.4) | 177 (30.8) | 125 (29.6) | |
| 2nd Year | 203 (16.7) | 100 (17.4) | 68 (16.1) | |
| 3rd Year | 210 (17.3) | 102 (17.8) | 66 (15.6) | |
| 4th Year | 168 (13.8) | 86 (15) | 65 (15.4) | |
| 5th Year | 158 (13) | 85 (14.8) | 49 (11.6) | |
| Residents in Research | 83 (6.8) | 24 (4.2) | 49 (11.6) | |
| Interest in Underserved Pop. | 0.13 | |||
| No | 854 (70.2) | 420 (73.2) | 290 (68.7) | |
| Yes | 363 (29.8) | 154 (26.8) | 132 (31.3) | |
The combined total of the Non-Academic and Academic groups is 996. This is the total study population (N=1217) minus the participants with “undecided” and “missing” practice types (N=221).
Figure 1.
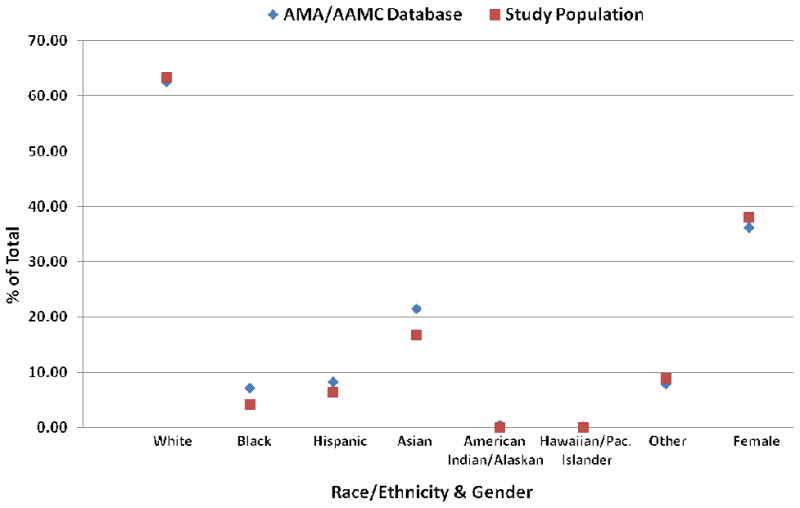
Demographics of Study Respondents versus National Resident Pool. The racial/ethnic and gender distribution of the study population (red) and the national pool of general surgery residents[16] (blue) are shown to be very similar
The mean age of our study population was 30.4 years. The majority of responding residents were male (62%) and Caucasian (64%), and approximately 25% had at least one child. Residents with additional professional degrees, less debt burden, those who identified a mentor or performed research during training, and foreign medical graduates were more likely to choose an academic rather than non-academic career. Respondent characteristics are detailed in Table II.
Using multivariable logistic regression, we tested the independent association of multiple variables with the plan to pursue an academic versus non-academic career. Among all residents (Table III), mentorship, research, and attending a training program that requires research were independently associated with pursuit of an academic career. Being in the third, fourth, or fifth year of training, and having one or more children were associated with pursuit of a non-academic career. When the analysis was performed among only senior residents (i.e., 4th and 5th year residents), the associations remained – and were in fact magnified – for mentorship, research, and having one or more children (Table III). Additionally, a debt burden of greater than $150,000 was associated with choosing a non-academic career.
Table 3. Multivariable logistic regression model for pursuit of academic surgery among all residents (N=989) and senior residents only (N = 282).
| Covariatea | Odds Ratio | 95% CI | P value |
|---|---|---|---|
| All Residents | |||
| Race/Ethnicity | |||
| White (reference) | 1.0 | -- | -- |
| Black or Hispanic | 1.0 | 0.62 - 1.60 | 0.99 |
| Asian | 0.92 | 0.62 - 1.37 | 0.69 |
| Other | 1.74 | 1.06 - 2.85 | 0.03 |
| Year in Training | |||
| First (reference) | 1.0 | -- | -- |
| Second | 0.67 | 0.44 - 1.03 | 0.07 |
| Third | 0.50 | 0.32 - 0.78 | <0.01 |
| Fourth | 0.53 | 0.32 - 0.87 | 0.01 |
| Fifth | 0.42 | 0.25 - 0.72 | <0.01 |
| Research Resident | 0.55 | 0.28 - 1.09 | 0.09 |
| Gender | |||
| Male (reference) | 1.0 | -- | -- |
| Female | 0.96 | 0.71 - 1.29 | 0.77 |
| Age (years) | 1.03 | 0.97 - 1.08 | 0.35 |
| Have children | 0.62 | 0.43 - 0.90 | 0.01 |
| Parental Education Level | |||
| College degree or less (reference) | 1.0 | -- | -- |
| Graduate degree | 1.09 | 0.80 - 1.48 | 0.60 |
| Interest in Underserved Population | 1.26 | 0.91 - 1.73 | 0.16 |
| Physician in Family | 0.97 | 0.70 - 1.34 | 0.85 |
| Additional Degree(s) | 1.15 | 0.79 - 1.66 | 0.47 |
| Debt Burden | |||
| None (reference) | 1.0 | -- | -- |
| < $100,000 | 1.21 | 0.74 - 2.00 | 0.45 |
| $100,001 - $150,000 | 0.95 | 0.56 - 1.60 | 0.85 |
| $150,001 - $200,000 | 0.86 | 0.54 - 1.36 | 0.52 |
| > $200,000 | 0.74 | 0.48 - 1.15 | 0.18 |
| Mentor | 2.12 | 1.57 - 2.87 | <0.001 |
| Research | 4.01 | 2.71 - 5.94 | <0.001 |
| Foreign Medical Graduate | 1.35 | 0.92 - 1.97 | 0.12 |
| Program Requires Research | 2.30 | 1.54 - 3.43 | <0.001 |
| Senior Residentsb | |||
| Have children | 0.43 | 0.22 – 0.88 | 0.02 |
| Debt Burden | |||
| None (reference) | 1.0 | -- | -- |
| $150,001 - $200,000 | 0.35 | 0.14 – 0.88 | 0.03 |
| > $200,000 | 0.39 | 0.15 – 0.97 | 0.04 |
| Mentor | 3.68 | 1.73 – 7.81 | 0.001 |
| Research | 5.52 | 2.87 – 10.61 | <0.001 |
| Program Requires Research | 2.69 | 1.11 – 6.49 | 0.03 |
Covariates without a specified reference group are binary (yes/no), where the reference group is “no”.
Only significant associations are shown for Senior Resident model.
The perceived influences with the highest overall mean influence scores, irrespective of career choice, were personality and lifestyle. When comparing the mean influence scores between residents choosing academic and non-academic careers (Table IV, Figure 2), mentorship and research experience were significantly more influential to those choosing academic careers than to those choosing non-academic careers. Conversely, lifestyle, income potential, current family situation, and debt burden were all significantly more influential to those choosing non-academic careers.
Table 4. Mean influence scores of residents pursuing academic versus private practice.
| Influence | Residents choosing Academics N = 422 Mean (SD) |
Residents choosing Non-Academics N = 574 Mean (SD) |
P value* |
|---|---|---|---|
| Your Personality, mean (SD) | 76.8 (0.9) | 76.4 (0.8) | 1.0 |
| Lifestyle | 50.0 (1.2) | 63.7 (1.1) | <0.001 |
| Mentorship | 49.7 (1.3) | 36.5 (1.2) | <0.001 |
| Research Experience | 49.5 (1.4) | 25.5 (1.1) | <0.001 |
| Income Potential | 45.3 (1.2) | 55.5 (1.0) | <0.001 |
| Patient Population | 44.2 (1.4) | 43.6 (1.2) | 1.0 |
| Current Family Situation | 39.0 (1.5) | 50.0 (1.3) | <0.001 |
| Debt Burden | 28.2 (1.3) | 39.9 (1.3) | <0.001 |
| Cultural Factors | 27.4 (1.3) | 29.5 (1.1) | 1.0 |
| Parents/Family | 25.7 (1.3) | 30.1 (1.2) | 0.13 |
Bonferroni-corrected p-values
Influence scores are a self-reported influence on choosing academic or private practice on a 0-100 scale for each factor
Figure 2.
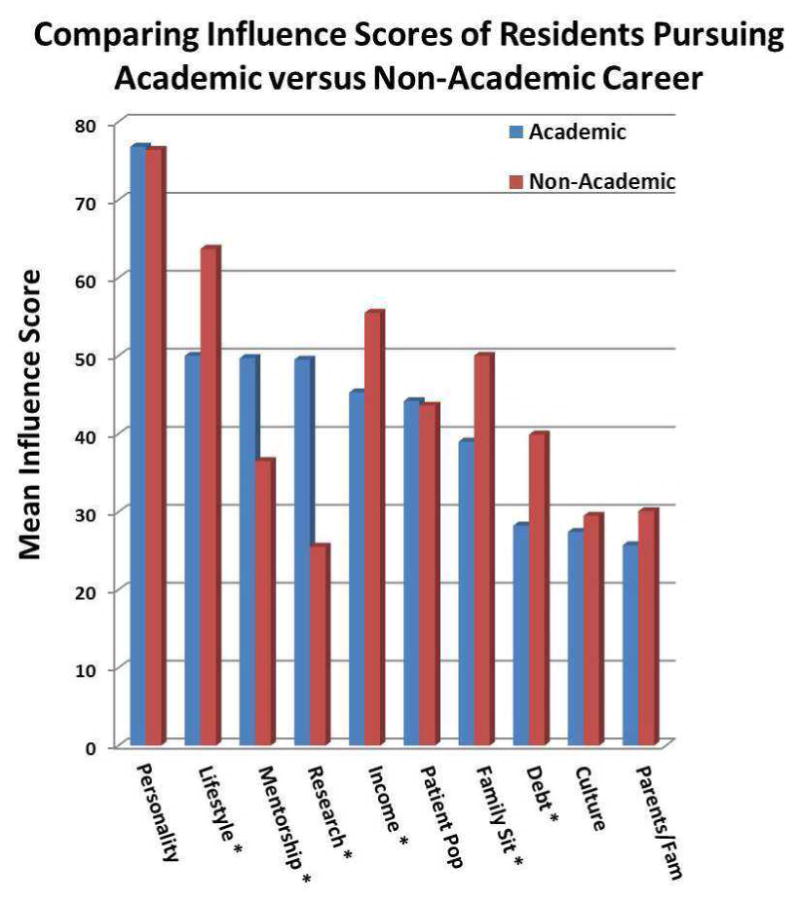
Mean influence scores comparing residents pursuing academic versus non-academic careers. The influences with statistically significant differences between groups are marked with *.
Discussion
In this study, we sought to understand the factors driving surgical residents to choose a fully academic or non-academic career, and thereby potentially explain the underrepresentation of minorities in academic surgery. We hypothesized that race/ethnicity and minority status would be associated with career choice, but our results did not support this association. This study is important because to the authors' knowledge it is the first study specifically addressing this question among a surgery resident population, and it has identified several explicit factors associated with choosing either type of career that can be directly translated into avenues of intervention.
The underrepresentation of minorities in academic surgery is an ever-present, pervasive problem with significant implications. Research suggests that the continued under-representation of African Americans, Hispanics, and Native Americans in the health professions has a profound negative public health effect exemplified by lack of access to care for minority patients.[17, 18] It has been shown that minority physicians have an important and unique role in caring for low-income minority patients,[19] and some have suggested that lack of access to care is, in part, a direct result of the underrepresentation of minorities in health care professions.[20] Also, in a report commissioned by the Joint Center for Political and Economic Studies, it was determined that more than 30% of direct medical costs faced by African Americans, Hispanics, and Asian Americans were excess costs due to health inequities – more than $230 billion over a 4-year period (2003 – 2006). When also considering the indirect costs of these inequities during the same time period, the combined costs in the US were $1.24 trillion.[21] Collectively these reports emphasize the necessity and importance of having minority physicians working in a variety of clinical and academic settings.
Our results demonstrate that underrepresented minorities were just as likely to pursue an academic career as non-minority residents -- a finding that held true after adjusting for multiple demographic, socioeconomic, and education-related factors. This finding that race/ethnicity alone is not associated with career choice among residents suggests there is perhaps yet another point in the pipeline into an academic surgery – a point beyond residency training – where the career plans of minorities are redirected toward non-academic opportunities. This may be due to changes in interest or family responsibilities during subspecialty fellowship training, or reflective of the poor level of minority faculty retention by academic institutions.[9, 10]
Mentorship and research experience during training (or attending a training program requiring research) were the strongest factors associated with plans to pursue an academic career. These findings are consistent with our expectations, as mentorship has been repeatedly demonstrated to have a crucial role in the personal and career development of trainees[6, 11, 12, 22, 23] and research experience during residency is a crucial component of training both to those with interest in academic careers, as well as those planning to enter competitive fellowships. These are both “modifiable” factors that can be targeted as areas to specifically address among minority trainees. The factors associated with pursuit of a non-academic career – year in training, having children – are largely non-modifiable. Among senior residents, debt burden was also associated with pursuit of a non-academic career. When asked what factors they felt were most influential to their career decisions, the responses were supportive of the results of the main analysis. Mentorship and research were considered more important to those pursuing academic surgery, whereas financial and family-oriented factors were more important to those pursuing non-academic practice (Table IV). Therefore, interventions such as structured mentorship programs, improved encouragement and funding for minorities to pursue research, financial counseling from college through medical school and residency, and debt forgiveness programs for minorities in academia could make a significant impact on the number of minorities ultimately choosing academic careers.
This study has several important limitations which must be considered. The main outcome is the intent to pursue a certain career, rather than the objective measure of actually having pursued it. Intent may change over time for various reasons, which we addressed within our analysis by examining senior residents only; however, we cannot control for those who change their minds after completing the survey – whether it be during residency or thereafter. Also, race/ethnicity is self-defined in this study. This may cause some bias in racial/ethnic groupings (e.g., some Indian residents may classify themselves as Asian, while some may consider themselves “Other”). A major concern of our study is the low response rate (33%). However, surgical residents are notoriously poor at participating in research surveys, with typical response rates in the low 20% range. Comparatively our response rate is quite high, and certainly satisfactory among this study population. The major strengths of our study are the absence of measured response-bias, and the generalizability of our sample to the national pool of residents. The 33% of residents who completed the survey represents approximately 17% of general surgery residents in ACGME-accredited programs across the US (N ≈ 7,357).[24] We have shown that this study sample is demographically representative of the national pool. Also, the questionnaire was carefully designed to identify racial differences in career choice among residents. The wording of the questions and responses, and the order with which they were asked were carefully decided to minimize ambiguity, as well as to minimize any influence that one question may have on subsequent questions. To further minimize any pre-conceived bias while filling out the questionnaire, the respondents were blind to the fact that the study was specifically assessing race/ethnicity and its role in career choice – only that we were investigating factors associated with resident career choices. The end results are responses that can be considered as accurate and non-biased as possible.
Underrepresented minority status was not found to be associated with the decision to pursue academic surgery in our study. Intentional recruitment of minorities into research-oriented training programs, increased mentorship and research support among current minority residents, and improved financial options for minorities entering academia may increase the number choosing an academic surgical career.
Acknowledgments
This study was supported by two grants. Dr. Grogan is a recipient of the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service Career Development Award (10-024). Dr. St. Julien is a recipient of the Vanderbilt University Surgical Oncology T32 Training Grant (3T32CA106183-07S1). The primary and corresponding authors had full control of the study design, methods, outcome parameters and results, data analysis, and manuscript production. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. Research Electronic Data Capture (REDCap) utilized for survey questionnaire development and distribution, and data collection. Vanderbilt Institute for Clinical and Translational Research grant support (1 UL1 RR024975 from NCRR/NIH). There are no other financial disclosures to report.
Footnotes
Conflict of Interest: There are no other financial disclosures or conflicts of interest to report. Specifically, the authors St. Julien, Lang, Brown, Aldrich, Deppen, Wu, Feurer, M. Tarpley, Hill, J. Tarpley, Beauchamp, and Grogan declare that they have no conflict of interest.
Ethical Standard: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- 1.Nivet MA. Minorities in academic medicine: review of the literature. J Vasc Surg. 2010;51(4 Suppl):53S–58S. doi: 10.1016/j.jvs.2009.09.064. [DOI] [PubMed] [Google Scholar]
- 2.Butler PD, Longaker MT, Britt LD. Major deficit in the number of underrepresented minority academic surgeons persists. Ann Surg. 2008;248(5):704–11. doi: 10.1097/SLA.0b013e31817f2c30. [DOI] [PubMed] [Google Scholar]
- 3.Aagaard EM, Hauer KE. A cross-sectional descriptive study of mentoring relationships formed by medical students. J Gen Intern Med. 2003;18(4):298–302. doi: 10.1046/j.1525-1497.2003.20334.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wakeford R, et al. Where do medically qualified researchers come from? Lancet. 1985;2(8449):262–5. doi: 10.1016/s0140-6736(85)90303-4. [DOI] [PubMed] [Google Scholar]
- 5.Straus SE, Straus C, Tzanetos K. Career choice in academic medicine: systematic review. J Gen Intern Med. 2006;21(12):1222–9. doi: 10.1111/j.1525-1497.2006.00599.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sambunjak D, Straus SE, Marusic A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–15. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 7.Rosenblatt RA, Andrilla CH. The impact of U.S. medical students' debt on their choice of primary care careers: an analysis of data from the 2002 medical school graduation questionnaire. Acad Med. 2005;80(9):815–9. doi: 10.1097/00001888-200509000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Haviland MG, et al. Student mistreatment in medical school and planning a career in academic medicine. Teach Learn Med. 2011;23(3):231–7. doi: 10.1080/10401334.2011.586914. [DOI] [PubMed] [Google Scholar]
- 9.Price EG, et al. The role of cultural diversity climate in recruitment, promotion, and retention of faculty in academic medicine. J Gen Intern Med. 2005;20(7):565–71. doi: 10.1111/j.1525-1497.2005.0127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palepu A, et al. Minority faculty and academic rank in medicine. JAMA. 1998;280(9):767–71. doi: 10.1001/jama.280.9.767. [DOI] [PubMed] [Google Scholar]
- 11.Thakur A, et al. Impact of mentor guidance in surgical career selection. J Pediatr Surg. 2001;36(12):1802–4. doi: 10.1053/jpsu.2001.28842. [DOI] [PubMed] [Google Scholar]
- 12.McCord JH, et al. Surgical career choices: the vital impact of mentoring. J Surg Res. 2009;155(1):136–41. doi: 10.1016/j.jss.2008.06.048. [DOI] [PubMed] [Google Scholar]
- 13.Harris PA, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Association of Program Directors in Surgery. [cited 2011 February 1st]; Available from: http://www.apds.org/index.htm.
- 15.Accreditation Council for Graduate Medical Education. Program Search. [cited 2011 March 1st]; Available from: http://www.acgme.org/adspublic/
- 16.Brotherton SE, Etzel SI. Graduate medical education, 2010-2011. JAMA. 2011;306(9):1015–30. doi: 10.1001/jama.2011.1236. [DOI] [PubMed] [Google Scholar]
- 17.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. Journal of the National Medical Association. 2002;94(8):666–8. [PMC free article] [PubMed] [Google Scholar]
- 18.Thurmond VB, Kirch DG. Impact of minority physicians on health care. South Med J. 1998;91(11):1009–13. doi: 10.1097/00007611-199811000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Komaromy M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. The New England journal of medicine. 1996;334(20):1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 20.Cooper RS. Health and the social status of blacks in the United States. Annals of epidemiology. 1993;3(2):137–44. doi: 10.1016/1047-2797(93)90126-o. [DOI] [PubMed] [Google Scholar]
- 21.LaVeist TA, G D, Richard P. The Economic Burden of Health Inequalities in the United States. Joint Center for Political and Economic Studies. 2009:1–20. [Google Scholar]
- 22.Newman LA, Pollock RE, Johnson-Thompson MC. Increasing the pool of academically oriented African-American medical and surgical oncologists. Cancer. 2003;97(1 Suppl):329–34. doi: 10.1002/cncr.11027. [DOI] [PubMed] [Google Scholar]
- 23.Ramanan RA, et al. Mentoring matters. Mentoring and career preparation in internal medicine residency training. J Gen Intern Med. 2006;21(4):340–5. doi: 10.1111/j.1525-1497.2006.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Accreditation Council for Graduate Medical Education Data Resource Book: Academic Year 2010 - 2011. [cited November 15, 2011]; Available from: http://www.acgme.org/acWebsite/dataBook/2010-2011_ACGME_Data_Resource_Book.pdf.


