Abstract
Theories of cognitive vulnerability to depression (CVD) imply that CVD is early-emerging and trait-like; however, little longitudinal work has tested this premise in middle childhood, or examined theoretically relevant predictors of child CVD. We examined test–retest correlations of self-referent encoding task performance and self-reported attributional styles and their associations with parental characteristics in 205 seven-year-olds. At baseline, child CVD was assessed, structured clinical interviews were conducted with parents, and ratings of observed maternal affective styles were made. Children’s CVD was re-assessed approximately one and two years later. Both measures of children’s CVD were prospectively and concurrently associated with children’s depressive symptoms and showed modest stability. Multilevel modeling indicated that maternal criticism and paternal depression were related to children’s CVD. Findings indicate that even early-emerging CVD is a valid marker of children’s depression risk.
Keywords: Depression, Childhood, Cognitive vulnerability
1. Introduction
Cognitive theories of depression (cognitive vulnerability to depression; CVD; e.g., Beck, 1967) are firmly established as central models of depression risk and treatment. Although these models hold that cognitive diatheses are early-emerging and stable (Ingram, Miranda, & Segal, 1998), few investigations have examined the stability of indices of CVD in early childhood. Measurement of cognitive risk in youth is important given that recent decades have seen a shift toward research on the validity of cognitive models of depression in adolescents and children. This work represents an important step in the further refinement of theories of CVD. More specifically, cognitive theories purport that CVD should be evident prior to depressive disorder and become increasingly consolidated during development. This increased stability could play an important role in potentiating the well-established increase in depression that occurs in adolescence. Thus, research that characterizes the stability of CVD early in life could inform prevention efforts by identifying early periods in which CVD shows some evidence of stability.
A surprisingly small body of work documents the stability of adult CVD (e.g., Hankin, Fraley, & Abela, 2005). Many of these studies comprise two waves only, and most examine the stability of self-reported CVD rather than laboratory measures, despite their widespread use (e.g., self-referent encoding tasks; SRET). The latter issue is underappreciated, as the stability of laboratory measures may be a more stringent test of the trait-like properties of CVD, as performance-based measures do not capitalize on the stability of response style biases as self-reports might. Furthermore, laboratory measures might better capture negative cognition in younger participants, who may lack the introspection and self-reflection required to provide valid self-reports of their cognition. Important work that speaks to the stability of childhood CVD is accruing (e.g., Cole et al., 2009), with evidence suggesting both stability and change (Hankin, 2008; Hankin et al., 2009). However, this work has focused on self-reported CVD in later childhood and early adolescence across relatively brief follow-ups, factors which may increase estimates of stability relative to work on younger samples using information processing measures, and longer follow-up intervals.
Based on this literature, there is ongoing debate regarding when meaningful, stable aspects of CVD emerge (e.g., Abela & Hankin, 2011; Cole et al., 2008), and evidence may vary depending on how it is measured. The developmental literature indicates that children develop a more stable yet differentiated sense of self in middle childhood (Abela & Hankin, 2008), suggesting that measures of CVD that tap self-schemas may yield meaningful information about depressive cognition in children this age. However, no data are available with respect to the long-term stability of widely used measures of children’s schemas (e.g., self-referent encoding tasks; SRETs) in middle childhood; indeed, we know of no study examining the stability of self-referent encoding biases in any age group, an important omission if such biases are truly thought to be trait-like.
Therefore, as our first hypothesis, we examined the stability of information processing biases over multiple follow-up assessments spanning a lengthy two-year period, predicting at least modest stability across this time frame. We know of no other study of child CVD that has used such a lengthy follow-up period, thus providing a relatively stringent test of the stability of early cognitive risk. Furthermore, most studies that have tested the stability of CVD in youth have examined older children; we therefore looked at the middle childhood period. In addition to an information processing measure, we also included a self-report of CVD, the Children’s Attributional Styles Questionnaire-Revised (CASQR; Thompson, Kaslow, Weiss, & Nolen-Hoeksema, 1998) for comparison.
We also examined links between children’s CVD and two well-established markers of children’s depression risk that may be mediated via their impact on children’s emerging negative cognition: maternal affective style and parental depression (Garber & Flynn, 2001). Theoretical accounts of the development of CVD have long posited a role of caregiver behavior, especially criticism, in fostering negative child cognition (e.g., Beck, 1967), perhaps by leading children to internalize negative self-views. Through such mechanisms, children’s CVD may mediate associations found between early caregiver behavior and offspring depression (Alloy, Abramson, Smith, Gibb, & Neeren, 2006). However, much of the research on parenting-CVD links has been conducted with adolescents, despite evidence that stress earlier in life, such as adverse parenting, may have particularly detrimental effects on young children’s development (Brown, 2012). Thus, as our second hypothesis, we predicted that negative caregiving styles would be associated with elevated initial and increased negative child cognition over follow-up.
Familial depression is the most robust marker of an individual’s depression risk (Goodman & Gotlib, 1999). Previous work has found that children with a maternal history of depression are at heightened risk for the development of CVD (Garber & Flynn, 2001), potentially through genetic, social learning, and other processes; however, associations between fathers’ depression history and child risk are poorly understood and understudied in the field, despite their implications for child outcomes (e.g., Connell & Goodman, 2002). We therefore expanded previous work by including measures of both parents’ depression; as our last hypothesis, we predicted that parental depression would predict heightened initial and increasing child cognitive risk.
2. Method
A community sample of 205 seven-year-olds (96 boys; 46.83%) and their parents were recruited from a psychology department database and advertisements. The mean age of children at baseline was 7.37 years (SD = 0.30). The Peabody Picture Vocabulary Test, Fourth Edition (Dunn & Dunn, 2007) was administered as a measure of cognitive functioning. Children performed within the normal range (M = 111.92; SD = 12.15). Parents identified their child’s race as Caucasian (n = 180; 87.80%), Asian (n = 4; 1.95%) or other (n = 16; 7.80%). Most children (n = 187; 91.22%) came from two-parent homes.
Of the 205 children, 181 (88.3%) participated in a follow-up visit in the family’s home approximately a year after the baseline assessment, when children were 8.48 years old (SD = 0.32). Comparing participants who did and did not participate in the first follow-up showed no significant differences in major study variables (all ps > 0.05). Approximately 2 years after baseline, a third assessment, conducted during a laboratory visit, occurred when children were 9.63 years old (SD = 0.38); 171 children (83% of the original sample) participated. We again compared participants who completed the third assessment to those who completed the baseline assessment only, and found no significant differences in study variables.
2.1. Assessment of parents
2.1.1. Parent mood disorder
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-NP; First, Spitzer, Gibbon, & Williams, 1996) was used to assess for lifetime history of depressive disorder (DD) at baseline. The majority of mothers (n = 202; 98.54%) and most fathers (n = 183; 89.27%) completed the SCID. Inter-rater reliability was high, with Cohen’s Kappa = 1.00, p < 0.001 for a diagnosis of DD (N = 14). In our sample, 68 (33%) mothers and 34 (17%) fathers had a lifetime history of DD; for mothers, 11 cases were current and 10 fathers had a current mood disorder.
2.1.2. Maternal affective style
As part of a laboratory visit at which the baseline SRET was collected, the experimenter supervising the visit completed a scale (Goldsmith, 1995) in which maternal affective styles while interacting with their child were rated. Ratings were made on a 0–5 scale by a trained post-baccalaureate experimenter with a background in child development, based on positive (i.e., maternal enjoyment/pleasure; sensitivity; connectedness) and negative (criticism; intrusiveness) maternal affect directed toward the child, across the entire two-hour-long visit. Maternal behavior with the child before and after the visit formally began was also considered in ratings. These ratings were significantly correlated with ratings made of the same behaviors during a five-minute standardized parent–child interaction task during the visit (mean r = 0.48; range = 0.34–0.61).
2.2. Child assessment
2.2.1. Child cognitive vulnerability
To activate latent cognitive vulnerability (Taylor & Ingram, 1999), a mood induction procedure (MIP) shown to be effective in multiple studies (e.g., Hayden, Klein, Durbin, & Olino, 2006) was administered, in which children were shown a sad movie clip. A novel clip was shown at each assessment. Next, a SRET (Kuiper & Derry, 1982), a widely used information-processing task used to assess memory biases for positive and negative self-referent information, was administered. Children were presented with 26 words (13 positive and 13 negative) taken from previous research using this task with young children (Hayden et al., 2006). Words were presented on flash cards and spoken aloud by the experimenter. Following each word, children were asked “Is this like you?” Words were presented in a different random order for each participant; the same word stimuli were used at each assessment. This portion of the task was followed by an incidental recall period in which children were asked to recall as many of the presented words as possible. Two indices of memory processing relevant to depression were calculated: a positive schematic processing score (the proportion of positive words both rated as self-descriptive and subsequently recalled relative to all words rated as self-descriptive) and a negative schematic processing score (derived in the same manner using negative words) (Johnson, Joorman, & Gotlib, 2007).
The Child Attributional Style Questionnaire (CASQ-R; Thompson et al., 1998) is a self-report of attributions for 12 positive and 12 negative life events. This measure yields a Positive Composite (PC) and a Negative Composite (NC). Lower CASQ-R PC scores reflect a tendency to attribute positive events to external, unstable, and specific factors, while higher CASQ-R NC scores reflect a tendency to attribute negative events to internal, stable, and global factors; thus, lower CASQ-R PC and higher CASQ-R NC scores are viewed as “depressogenic.” A research assistant read the CASQ-R items aloud to children in this study. The internal consistency of the CASQ-R NC was modest at child ages 7, 8, and 9 (αs = 0.50, 0.52, and 0.51, respectively), but consistent with previous research (e.g., Conley, Haines, Hilt, & Metalsky, 2001; Hayden et al., 2006; Thompson et al., 1998). The internal consistency of the CASQ-R PC at the follow-ups at ages 8 and 9 was also modest (αs = 0.56, 0.59); however, its internal consistency at baseline was poor (Cronbach’s α = 0.29). Although it could be improved (Cronbach’s α = 0.40) by removing five items from the scale (items 1, 5, 13, 16, and 23), analyses revealed that the nature of the relations between the revised scale and other study measures was the same as those observed with the original; thus, the original CASQ-R PC was retained for all subsequent analyses. Despite low internal consistency, higher scores on the NC and lower scores on the PC are consistently related to children’s depressive symptoms (e.g., Hayden et al., 2006; Thompson et al., 1998).
2.2.2. Child depressive symptoms
The Depression Self Rating Scale (DSRS; Birleson, 1981) is a 24-item self-report measure of cognitive, emotional, and behavioral symptoms of depression in children. Symptoms are rated on a three-point scale. DSRS scores demonstrated good internal consistency at all time points (α = 0.73, 0.72, and 0.86, at Times 1, 2, and 3). Means at all time points were low and consistent with those reported in samples of non-depressed children (e.g., Hayden et al., 2006).
2.3. Data analysis
Our primary analyses used mPlus (6th version; Muthén & Muthén, 1998–2010) to estimate linear growth to examine mean-level changes of indices of cognitive vulnerability. The intercept is the estimated value of the outcome variable at a defined time. We centered time such that the intercept reflected CVD at age 7. The slope is the estimated value of the average rate of change across all time intervals. The intercept and slope parameters are also characterized by variance estimates, which show whether there is significant inter-individual variability in initial status (i.e., intercept) and rate of change (i.e., slope). Due to the small values of the SRET scores, growth models were conducted after multiplying the raw proportion values by 100 to ease computational burden. Lastly, we examine associations between indices of risk, including maternal and paternal depression and maternal affective styles, and growth trajectories of CVD.
3. Results
Bivariate associations between children’s SRET and CASQ-R scores are in Table 1. Correlations between the same index of CVD across time were typically significant, albeit of modest magnitude. Table 2 shows correlations between measures of children’s CVD and depressive symptoms. Examination suggests that associations between the SRET and children’s depression increased with age; only modest associations were found at baseline with stronger associations at ages 8 and 9. Associations between the CASQ-R and DSRS scores were generally stronger than those between the SRET and the DSRS; however, this is to be expected due to shared methodology.
Table 1.
Stability of, and cross-method associations between, measures of children’s cognitive vulnerability.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age 7 Pos SRET | – | |||||||||||
| 2. Age 7 Neg SRET | −0.12 | – | ||||||||||
| 3. Age 8 Pos SRET | 0.26** | 0.02 | – | |||||||||
| 4. Age 8 Neg SRET | 0.03 | 0.24** | −0.18* | – | ||||||||
| 5. Age 9 Pos SRET | 0.13 | 0.00 | 0.39** | −0.10 | – | |||||||
| 6. Age 9 Neg SRET | −0.08 | 0.22** | −0.09 | 0.25** | −0.29** | – | ||||||
| 7. Age 7 CASQ-R PC | 0.14 | −0.19** | 0.02 | −0.14 | 0.11 | −0.21** | – | |||||
| 8. Age 7 CASQ-R NC | −0.10 | 0.09 | −0.06 | 0.20** | −0.06 | 0.20** | −0.27** | – | ||||
| 9. Age 8 CASQ-R PC | 0.16* | −0.04 | 0.16* | −0.26** | 0.13 | −0.06 | 0.31** | −0.23** | – | |||
| 10. Age 8 CASQ-R NC | −0.06 | 0.04 | −0.15* | 0.31** | −0.14 | 0.26** | −0.10 | 0.41** | −0.35** | – | ||
| 11. Age 9 CASQ-R PC | 0.07 | −0.13 | 0.16* | −0.23** | 0.31** | −0.26** | 0.34** | −0.26** | 0.52** | −0.28** | – | |
| 12. Age 9 CASQ-R NC | 0.09 | 0.00 | −0.01 | 0.20* | −0.16* | 0.39** | 0.04 | 0.30** | −0.15 | 0.45** | −0.28** | – |
| M | 0.18 | 0.01 | 0.23 | 0.02 | 0.30 | 0.02 | 8.18 | 2.45 | 8.19 | 2.33 | 8.58 | 2.42 |
| SD | 0.13 | 0.03 | 0.14 | 0.04 | 0.15 | 0.05 | 1.77 | 1.81 | 2.13 | 1.77 | 2.14 | 1.78 |
p < 0.05.
p < 0.01.
Table 2.
Correlations between measures of cognitive vulnerability and children’s self-reported internalizing symptoms.
| Age 7 DSRS | Age 8 DSRS | Age 9 DSRS | |
|---|---|---|---|
| Age 7 Pos SRET | −0.15* | −0.19* | −0.20* |
| Age 7 Neg SRET | 0.12 | 0.04 | 0.07 |
| Age 8 Pos SRET | −0.06 | −0.20** | −0.12 |
| Age 8 Neg SRET | 0.08 | 0.18** | 0.16* |
| Age 9 Pos SRET | −0.06 | −0.08 | −0.34** |
| Age 9 Neg SRET | 0.18* | 0.14 | 0.29** |
| Age 7 CASQ-R PC | −0.32** | −0.09 | −0.13 |
| Age 7 CASQ-R NC | 0.39** | 0.34** | 0.24** |
| Age 8 CASQ-R PC | −0.22** | −0.36** | −0.32** |
| Age 8 CASQ-R NC | 0.32** | 0.37** | 0.22** |
| Age 9 CASQ-R PC | −0.23** | −0.27** | −0.35** |
| Age 9 CASQ-R NC | 0.24** | 0.26** | 0.30** |
| M | 12.45 | 13.15 | 14.11 |
| SD | 5.29 | 4.96 | 7.23 |
p < 0.05.
p < 0.01.
Associations between maternal affective style, parental depression, and child cognitive risk are shown in Table 3. No associations were found between positive maternal affective styles and children’s CVD. There were multiple associations between maternal criticism and children’s CVD, with criticism predicting CASQ-R PC scores (at all assessments) and CASQ-R NC scores at ages 8 and 9. Intrusiveness was associated with age 9 negative SRET scores. Significant associations between maternal depression and children’s CVD were limited to a negative relationship with age 8 positive SRET scores. Paternal depression was associated with greater negative SRET scores at ages 8 and 9.
Table 3.
Associations between maternal affective styles, parental depression history, and child CVD.
| Parent characteristic |
Age 7 Pos SRET |
Age 7 Neg SRET |
Age 8 Pos SRET |
Age 8 Neg SRET |
Age 9 Pos SRET |
Age 9 Neg SRET |
Age 7 CASQ-R PC |
Age 7 CASQ-R NC |
Age 8 CASQ-R PC |
Age 8 CASQ-R NC |
Age 9 CASQ-R PC |
Age 9 CASQ-R NC |
M (SD) or N (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Criticism | 0.07 | 0.00 | −0.07 | 0.21** | −0.09 | 0.15 | −0.18* | 0.06 | −0.20** | 0.19* | −0.20* | 0.16* | 1.76 (0.80) |
| Enjoyment | 0.05 | 0.03 | 0.05 | 0.01 | 0.01 | 0.02 | 0.05 | −0.11 | −0.01 | 0.01 | −0.03 | −0.06 | 3.71 (0.91) |
| Sensitivity | −0.05 | −0.05 | 0.00 | −0.04 | 0.01 | −0.08 | 0.13 | −0.03 | 0.06 | 0.01 | 0.02 | −0.02 | 3.89 (0.65) |
| Connectedness | 0.05 | 0.01 | 0.04 | −0.07 | 0.11 | −0.08 | 0.06 | −0.06 | 0.04 | 0.03 | 0.03 | −0.03 | 3.75 (0.96) |
| Intrusiveness | 0.00 | 0.07 | 0.03 | 0.08 | 0.01 | 0.15* | −0.07 | 0.04 | −0.08 | 0.14 | −0.06 | 0.12 | 1.78 (0.79) |
| Maternal depression | 0.00 | −0.07 | −0.15* | 0.05 | −0.02 | 0.04 | −0.02 | 0.02 | −0.10 | −0.04 | 0.04 | 0.06 | 68 (33) |
| Paternal depression | 0.04 | 0.16* | 0.02 | 0.10 | −0.09 | 0.23** | 0.05 | −0.01 | 0.03 | 0.13 | 0.02 | 0.13 | 34 (17) |
Note: Maternal and paternal depression coded as 0 = no lifetime history of major depressive disorder or dysthymic disorder and 1 = a lifetime history of major depressive disorder or dysthymic disorder.
p < 0.05.
p < 0.01.
3.1. Mean-level changes
Unconditional growth models were estimated for each index of CVD (Table 4). The linear growth model for the CASQ-R NC showed a significant intercept with significant inter-individual variability, but non-significant slope and non-significant variance in the slope parameter. For CASQ-R PC, the linear growth model also showed a significant intercept with significant inter-individual variability, and a significant slope, with significant inter-individual variability. For performance on the SRET, the linear growth model for the negative SRET scores found a significant intercept and a significant slope, with significant inter-individual variability. For positive SRET scores, the linear growth model found a significant intercept, with significant inter-individual variability, and a significant slope, with significant inter-individual variability. It is important to note that the significant intercepts of all measures of CVD reflect the presence of stable aspects of cognitive vulnerability across time (i.e., the intercept is the reliable portion of the construct, after removing the error of measurement and time-related trends), providing support for our study hypothesis that evidence for modest stability of children’s CVD would be found in middle childhood.
Table 4.
Growth parameters.
| Intercept | Slope | |||||||
|---|---|---|---|---|---|---|---|---|
| Estimate (B00) | Variance (r00) | Estimate (B01) | Variance (r01) | |||||
| M | SE | M | SE | M | SE | M | SE | |
| CASQ-Neg | 2.43*** | 0.12 | 1.19*** | 0.28 | −0.002 | 0.07 | 0.03 | 0.08 |
| CASQ-Pos | 8.13*** | 0.12 | 1.31*** | 0.20 | 0.15* | 0.08 | 0.23* | 0.09 |
| SRET-Neg | 1.46*** | 0.21 | 2.02 | 1.22 | 0.34* | 0.16 | 1.43* | 0.71 |
| SRET-Pos | 17.70*** | 0.81 | 32.51*** | 8.73 | 5.22*** | 0.59 | 14.81*** | 5.11 |
Intercept and slope refer to the growth parameters from individual linear growth models.
p < 0.05.
p < 0.001.
3.2. Predictors of growth trajectories
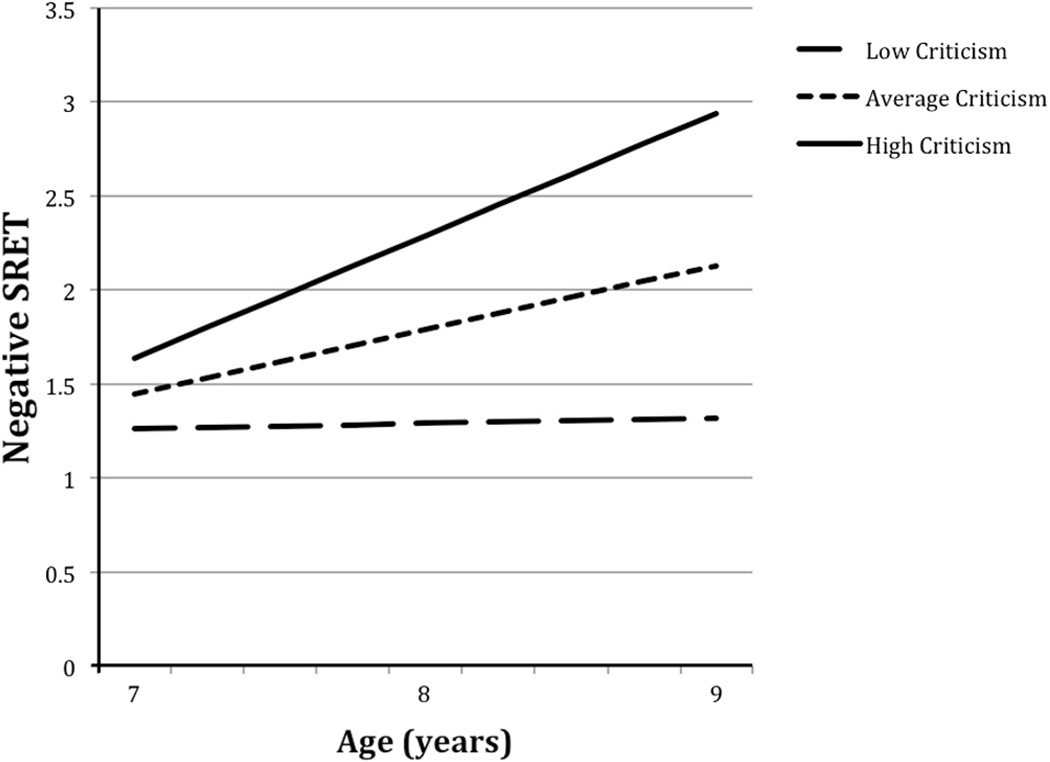
We examined associations between parental depression and observed maternal affective styles and these growth trajectories, predicting that poor maternal caregiving and parental depression would predict elevated initial levels of CVD and greater increases across time. Predictors were examined individually to conserve power. To conserve space, figures are not provided for models in which significant predictors were found for intercepts only. Maternal criticism was negatively associated with the intercepts for the CASQ-R PC (B = −0.47, SE = .15, p < 0.01) and positively associated with the CASQ-R NC (B = 0.26, SE = 0.13, p < 0.05); i.e., maternal criticism was associated with significantly lower initial positive attributions and higher initial negative attributions. Maternal sensitivity was also positively associated with initial levels of CASQ-R PC (B = 0.33, SE = 0.16, p < 0.05). Criticism was positively associated with the slope of negative SRET such that higher levels of criticism were associated with faster increases in negative SRET scores (B = 0.39, SE = 0.23, p < 0.10; Fig. 1); however, this effect failed to reach accepted thresholds of significance. No significant associations were found between maternal or paternal depression and positive SRET scores.
Fig. 1.
Negative SRET scores as a function of maternal criticism. Note: SRET = self-referent encoding task.
4. Discussion
We examined the long-term stability and correlates of measures of children’s CVD across middle childhood. Children’s self-referent encoding task performance and self-reported attributions for positive and negative events were meaningfully related to their depressive symptoms, concurrently and prospectively, supporting the validity of these measures of children’s cognitive risk. Further, child CVD showed modest stability over three waves of data collection separated by one-year intervals. While admittedly small, the stability coefficients we obtained are comparable to those found over much shorter follow-ups of older children and adolescents (e.g., Hankin, 2008). Results from growth modeling, which showed significant intercepts of all measures of CVD, further supported the presence of stable aspects of cognitive vulnerability across time. Our findings suggest that CVD emerges as a marker of children’s risk for depression earlier than previously established; assuming future research replicates our findings, even early negative cognition may be a meaningful target of prevention efforts.
As far as family-level correlates were concerned, the most robust associations with child CVD were obtained for maternal criticism, which was related to both information processing measures and attributional styles at multiple waves of data collection, consistent with a larger literature (Alloy et al., 2006) implicating caregiver behavior in CVD. We cannot claim that maternal criticism caused children to develop CVD, as it is also possible that children with greater levels of negative cognition elicit more maternal criticism. However, our work bolsters the broader literature on the role of parental criticism in depression by suggesting a possible mechanism by which criticism increases depression risk-by virtue of its influence on children’s negative cognition (for example, through children’s internalization of negative self-views). Although replication of our findings is important, focusing on reducing maternal criticism could play an important role in preventative efforts for young children’s depression risk, particularly interventions focusing on parent–child relationships (e.g., Compas et al., 2010), which have historically focused on older youth. Given the increased neural plasticity of young children, such efforts could prove even more effective than those aimed at adolescents.
We also examined associations between children’s CVD and parental depression, and were somewhat surprised to find stronger associations between fathers’ depression and children’s negative cognition than mothers’ depression; maternal depression history predicted lower positive SRET scores at age 8 only, while paternal depression was associated with greater negative SRET scores at ages 8 and 9. Recent work indicates that paternal depression is associated with youth psychopathology symptoms (Kane & Garber, 2009), including internalizing symptoms. Our findings suggest that the effect of paternal depression on child negative cognition might be a mediator of the risk conferred to offspring by a family history of depression, and suggests the merit of involving both parents in intervention efforts, and targeting both maternal and paternal depression in family-level interventions.
Our study had a number of strengths, including multiple waves of assessment and low attrition. We used laboratory measures of CVD and structured clinical interviews. However, the reliability of the CASQ-R was low/moderate, albeit consistent with internal consistency estimates reported for this measure in the literature (e.g., Conley et al., 2001; Thompson et al., 1998), and random error of measures of cognition was generally high, as might be expected in children this age. Low reliability should have limited our ability to detect significant associations, thus making our analyses conservative. In other words, low internal consistency makes it less likely that significant results will be detected, but does not inflate Type I error (i.e., spuriously significant findings; Rosenthal, 1995). We were unable to provide interrater reliability statistics for our maternal ratings. In this unique data set, we ran analyses without statistical adjustment for several reasons. First, many of our results are bivariate correlations, which are fundamental, descriptive statistics. Further, overly stringent p values might deter other investigators from attempting replication of our findings. Although our analyses were hypothesis-driven, replication of our findings is important.
In conclusion, children’s early-emerging CVD shows modest homotypic continuity and meaningful associations with depressive symptoms across middle childhood. Early CVD is also associated with parental criticism and, to a lesser extent, parental depression. This work suggests that even early-emerging negative cognition might be a useful target for preventation, and that such work might yield greater effects if depression in both parents is addressed, and if negative caregiving, especially criticism, is targeted.
Acknowledgments
This research was supported by an Early Researcher Award from the Ontario Ministry of Research and Innovation, a SSHRC Standard Research Grant to Elizabeth P. Hayden, and a Career Development Award from the National Institute of Mental Health (K01 MH092603) to Thomas M. Olino. The Ontario Mental Health Foundation and the Children’s Health Research Institute provided student support.
References
- Abela JR, Hankin BL. Cognitive vulnerability to depression in children and adolescentsIn. In: Abela JR, Hankin BL, editors. Handbook of depression in children and adolescents. New York, NY: The Guilford Press; 2008. pp. 35–78. [Google Scholar]
- Abela JR, Hankin BL. Rumination as a vulnerability factor to depression during the transition from early to middle adolescence: A multiwave longitudinal study. Journal of Abnormal Psychology. 2011;120:259–271. doi: 10.1037/a0022796. http://dx.doi.org/10.1037/a0022796. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Abramson LY, Smith JM, Gibb BE, Neeren AM. Role of parenting and maltreatment histories in unipolar and bipolar mood disorders: mediation by cognitive vulnerability to depression. Clinical Child and Family Psychology Review. 2006;9:23–64. doi: 10.1007/s10567-006-0002-4. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: clinical, experimental, and theoretical aspects. New York, NY: Harper & Row; 1967. [Google Scholar]
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: a research report. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1981;22:73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. http://dx.doi.org/10.1111/ j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- Brown GW. The promoter of the serotonin transporter genotype, environment and depression: a hypothesis supported? Journal of Affective Disorders. 2012;137:1–3. doi: 10.1016/j.jad.2011.09.015. http://dx.doi.org/10.1016/j.jad.2011.09.015. [DOI] [PubMed] [Google Scholar]
- Cole DA, Ciesla JA, Dallaire DH, Jacquez FM, Pineda AQ, LaGrange B, et al. Emergence of attributional style and its relation to depressive symptoms. Journal of Abnormal Psychology. 2008;117:16–31. doi: 10.1037/0021-843X.117.1.16. [DOI] [PubMed] [Google Scholar]
- Cole DA, Jacquez FM, Truss AE, Pineda AQ, Weitlauf AS, Tilghman-Osborne CE, et al. Gender differences in the longitudinal structure of cognitive diatheses for depression in children and adolescents. Journal of Clinical Psychology. 2009;65:1312–1326. doi: 10.1002/jclp.20631. http://dx.doi.org/10.1002/jclp.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, et al. Coping and parenting: mediators of 12-month outcomes of a family group cognitive–behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology. 2010;78:623–634. doi: 10.1037/a0020459. http://dx.doi.org/10.1037/a0024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley CS, Haines BA, Hilt LM, Metalsky GI. The children’s attributional style interview: developmental tests of cognitive diathesis-stress theories of depression. Journal of Abnormal Child Psychology. 2001;29:445–463. doi: 10.1023/a:1010451604161. http:/ dx.doi.org/10.1023/A:1010451604161. [DOI] [PubMed] [Google Scholar]
- Connell AM, Goodman SH. The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: a meta-analysis. Psychological Bulletin. 2002;128:746–773. doi: 10.1037/0033-2909.128.5.746. http://dx.doi.org/10.1037/0033-2909.128.5.746. [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody picture vocabulary test. 4th ed. Bloomington, MN: Pearson; 2007. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, non-patient edition. New York, NY: Biometrics research, New York State Psychiatric institute; 1996. [Google Scholar]
- Garber J, Flynn C. Predictors of depressive cognitions in young adolescents. Cognitive Therapy and Research. 2001;25:353–376. [Google Scholar]
- Goldsmith HH. Observer impressions of the mother and dyad. 1995 Unpublished measure. [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. http://dx.doi.org/10.1037/0033-295X.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hankin BL. Stability of cognitive vulnerabilities to depression: a short-term prospective multiwave study. Journal of Abnormal Psychology. 2008;117:324–333. doi: 10.1037/0021-843X.117.2.324. http://dx.doi.org/10.1037/0021-843X.117.2.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Fraley RC, Abela JR. Daily depression and cognitions about stress: evidence for a traitlike depressogenic cognitive style and the prediction of depressive symptoms in a prospective daily diary study. Journal of Personality and Social Psychology. 2005;88:673–685. doi: 10.1037/0022-3514.88.4.673. http://dx.doi.org/10.1037/0022-3514.88.4.673. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Oppenheimer C, Jenness J, Barrocas A, Shapero BG, Goldband J. Developmental origins of cognitive vulnerabilities to depression: review of processes contributing to stability and change across time. Journal of Clinical Psychology. 2009;65:1327–1338. doi: 10.1002/jclp.20625. http://dx.doi.org/10.1002/jclp.20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden EP, Klein DN, Durbin CE, Olino TM. Positive emotionality at age three predicts cognitive styles in seven-year-old children. Development & Psychopathology. 2006;18:409–423. doi: 10.1017/S0954579406060226. [DOI] [PubMed] [Google Scholar]
- Ingram RE, Miranda J, Segal ZV. Cognitive vulnerability to depression. New York: The Guilford Press; 1998. [Google Scholar]
- Johnson SL, Joorman J, Gotlib IH. Does processing of emotional stimuli predict symptomatic improvement and diagnostic recovery from major depression? Emotion. 2007;7:201–206. doi: 10.1037/1528-3542.7.1.201. http://dx.doi.org/10.1037/1528-3542.7.1.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane P, Garber J. Parental depression and child externalizing and internalizing symptoms: unique effects of fathers’ symptoms and perceived conflict as a mediator. Journal of Child and Family Studies. 2009;18:465–472. http://dx.doi.org/10.1007/s10826-008-9250-x. [Google Scholar]
- Kuiper NA, Derry PA. Depressed and nondepressed content self-reference in mild depressives. Journal of Personality. 1982;50:67–80. doi: 10.1111/j.1467-6494.1982.tb00746.x. http:// dx.doi.org/10.1111/j.1467-6494.1982.tb00746.x. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6th ed. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Rosenthal R. Methodology. In: Tesser A, editor. Advanced social psychology. Boston, MA: McGraw-Hill; 1995. pp. 17–49. [Google Scholar]
- Taylor L, Ingram RE. Cognitive reactivity and depressotypic information processing in children of depressed mothers. Journal of Abnormal Psychology. 1999;108:202–210. doi: 10.1037//0021-843x.108.2.202. http://dx.doi.org/10.1037/0021-843X.108.2.202. [DOI] [PubMed] [Google Scholar]
- Thompson M, Kaslow NJ, Weiss B, Nolen-Hoeksema S. Children’s attributional style questionnaire-revised: psychometric examination. Psychological Assessment. 1998;10:166–170. http://dx.doi.org/10.1037//1040-3590.10.2.166. [Google Scholar]