Abstract
Objective
To examine mortality rates in UK patients with early rheumatoid arthritis (RA) from 1990–2011 and compare with population trends.
Methods
The Norfolk Arthritis Register (NOAR) recruited adults with ≥2 swollen joints for ≥4 weeks: cohort 1 (1990–1994), cohort 2 (1995–1999), and cohort 3 (2000–2004). At baseline, serum rheumatoid factor and anti–citrullinated protein antibody were measured and the 2010 American College of Rheumatology/European League Against Rheumatism RA classification criteria were applied. Patients were followed for 7 years, until emigration or death. The UK Office for National Statistics notified the NOAR of the date and cause of deaths, and provided mortality rates for the Norfolk population. All-cause and cardiovascular-specific standardized mortality ratios (SMRs) were calculated. Poisson regression was used to compare mortality rate ratios (MRRs) between cohorts and then, with cubic splines, to model rates by calendar year. Analyses were performed in patients 1) with early inflammatory arthritis, 2) classified as having RA, and 3) autoantibody positive.
Results
A total of 2,517 patients were included, with 1,639 women (65%) and median age 55 years, and 1,419 (56%) fulfilled the 2010 RA criteria. All-cause and cardiovascular-specific SMRs were significantly elevated in the antibody-positive groups. There was no change in mortality rates over time after accounting for changes in the population rates. In RA patients, all-cause MRRs, compared to cohort 1, were 1.13 (95% confidence interval [95% CI] 0.84–1.52) and 1.00 (95% CI 0.70–1.43) in cohorts 2 and 3, respectively.
Conclusion
Mortality rates were increased in patients with RA and SMRs were particularly elevated in those who were autoantibody positive. Compared to the general population, mortality rates have not improved over the past 20 years.
INTRODUCTION
It is well recognized that patients with rheumatoid arthritis (RA) die prematurely (1). Meta-analysis of studies published over the last 50 years suggest the standardized mortality ratio (SMR) is 1.47 (95% confidence interval [95% CI] 1.19–1.83) (2), i.e., patients with RA have a 47% increased risk of death compared to the general population, matched for age and sex. Causes of death in RA populations are similar to those in the wider population, with cardiovascular disease (CVD) being the most common cause (3). There is good evidence that improvements in CVD treatment, alongside public health interventions to aid primary and secondary prevention, have led to a fall in CVD mortality in the UK over the last 30 years (4). In addition, the prevalence of smoking, an important risk factor for both CVD and RA (5), has decreased in the UK by approximately 20% since 1980 (6). In RA, more aggressive treatment strategies and earlier intervention have also improved outcomes (7). Therefore, we might hypothesize that mortality in RA populations may also have improved, and may be approaching that of the general population. Indeed, some studies of patients with prevalent RA have suggested that such improvements have occurred (1). However, studies of prevalent cases are vulnerable to survivor bias, whereby a patient has to have survived with the disease long enough to be included in the study. By contrast, in a large incident cohort study from Rochester, Minnesota, Gonzalez et al reported that mortality rates increased over 40 years from 1965–2005 compared to the general population (8). They suggested that this was due to population-level improvements in mortality not being reflected in the RA population. Their study was limited to patients who fulfilled the 1987 American College of Rheumatology (ACR) classification criteria for RA (9) at baseline, which are poorly sensitive in early RA (10), and mortality is also recognized to be increased in patients with early inflammatory arthritis (EIA) before classification criteria have been met (11,12). Few large prospective cohort studies exist that are able to examine secular trends. In addition, we now have a new case definition of RA in the 2010 ACR/European League against Rheumatism (EULAR) classification criteria (13). The aim of this study was to describe trends in mortality, first among a cohort of patients with EIA, second in the subset of patients with RA defined by the 2010 RA criteria, and third in those positive for the autoantibodies rheumatoid factor (RF) and anti–citrullinated protein antibodies (ACPAs).
Significance & Innovations.
All-cause and cardiovascular-specific mortality are increased in patients who satisfy the 2010 American College of Rheumatology/European League Against Rheumatism criteria for rheumatoid arthritis (RA) compared to the general population.
All-cause and, in particular, cardiovascular-specific mortality in patients with early inflammatory arthritis in the first 7 years appear to be decreasing over time.
The rate of decrease in mortality in patients with RA over the last 20 years is similar to the rate of decrease in mortality in the general population.
PATIENTS AND METHODS
Setting
This study was based in the Norfolk Arthritis Register (NOAR), UK. The NOAR has been described in detail elsewhere (14); briefly, since 1990 it has aimed to recruit adults registered with a general practitioner in the former Norwich Health Authority area presenting for the first time to primary or secondary care with EIA, defined as ≥2 swollen joints for ≥4 weeks. Patients recruited into the NOAR were divided into 3 cohorts, depending on the calendar year in which they were first enrolled on the register: cohort 1 (1990–1994), cohort 2 (1995–1999), or cohort 3 (2000–2004). All patients included in this study had <2 years' symptom duration at baseline assessment (89% of the total study population).
Assessment and followup
All patients recruited to the NOAR were seen by a research nurse at baseline, who conducted a structured interview and performed a 51 tender and swollen joint count. Blood samples were taken and the sera were stored frozen and later analyzed for C-reactive protein, RF (latex test), and ACPA (Axis-Shield Diastat anti-CCP kit). The 2010 ACR/EULAR criteria (13) were applied retrospectively using data collected at the baseline assessment. All patients were flagged with the Office for National Statistics (ONS), who notified dates of death to the NOAR and provided copies of death certificates. Deaths were attributed to CVD if the underlying cause of death was coded according to chapter I of the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (15). For any NOAR patients who left the UK, the ONS provided a date of embarkation; these patients were censored at that date. The ONS also provided age-, sex-, and cause-specific mortality rates by calendar year for the Norfolk County population, which covers a similar area to the patient population. The NOAR was approved by the Norwich Local Research Ethics Committee and all patients gave written consent.
Statistical analysis
Patients in each cohort were censored after 7 years of followup. This followup time was selected because it allowed inclusion of the most recent population mortality data available from the ONS (all deaths occurring prior to January 1, 2012) and provided a standardized length of time in which deaths could occur in each cohort, in order to facilitate comparisons. For each NOAR cohort, all-cause and CV-specific crude mortality rates were determined and 7-year SMRs were calculated by comparing the observed number of deaths to the expected number of deaths based on contemporary age-and sex-specific mortality rates from the ONS. This was done in the total population of EIA, for those classified as having RA according to the 2010 criteria, and in the subgroup of patients who were RF and/or ACPA positive. SMRs were not calculated if there were <15 observed deaths within a cohort, since CIs would be very wide and therefore it would not be possible to obtain a meaningful estimate. Mortality rate ratios (MRRs) were calculated using Poisson regression. MRRs allow statistical comparison of the mortality rates between the cohorts, while accounting for the expected mortality rate in each cohort based on age-and sex-specific mortality rates in the Norfolk population as an exposure variable. Cohort 1 was used as the reference standard. Mortality rates were then modeled by calendar year also using Poisson regression. A multivariate model, adjusted for age at symptom onset and sex and disease duration at baseline, and cubic splines were used to smooth the polynomial relationship between calendar year and mortality rates. All data were analyzed using the Stata 11 software package.
RESULTS
A total of 2,517 patients were included in this analysis, with 16,485 person-years of followup. A total of 1,419 patients (56%) fulfilled the 2010 RA criteria at baseline, 1,639 (65%) were women, and the median age at symptom onset was 55 years (interquartile range 44–68 years). Baseline demographic and clinical details for the 3 cohorts are shown in Table1. The median age at onset increased with each succeeding cohort, as did the median symptom duration. Crude 7-year mortality rates generally decreased slightly over time: in cohorts 1, 2, and 3, they were 21.25, 21.43, and 19.96 per 1,000 person-years for all-cause mortality, respectively, and were 8.78, 7.87, and 7.07 per 1,000 person-years for CV-specific mortality, respectively.
Table 1.
Demographic and baseline disease characteristics*
| Cohort 1 | Cohort 2 | Cohort 3 | Total | |
|---|---|---|---|---|
| EIA, n | 1,010 | 879 | 628 | 2,517 |
| Women | 655 (65) | 569 (65) | 407 (65) | 1,631 (65) |
| Age at symptom onset, median (IQR) years | 54 (42–67) | 55 (44–67) | 58 (47–70) | 55 (44–68) |
| Symptom duration, median (IQR) weeks | 22 (12–41) | 28 (16–51) | 29 (17–49) | 26 (14–46) |
| RF/ACPA positive | 299 (34) | 287 (36) | 235 (42) | 821 (37)† |
| 2010 ACR/EULAR RA criteria positive | 629 (69) | 451 (57) | 339 (61) | 1,419 (63)‡ |
| 2010 ACR/EULAR RA criteria negative | 287 (31) | 337 (43) | 218 (39) | 842 (37)‡ |
| 1987 ACR RA criteria positive | 458 (45) | 318 (36) | 289 (46) | 1,065 (42) |
| DAS28, median (IQR) | 3.97 (2.89–5.05) | 3.54 (2.64–4.66) | 3.60 (2.65–4.53) | 3.71 (2.75–4.78)§ |
| DMARDs at baseline assessment | 153 (15) | 258 (29) | 287 (46) | 698 (28) |
| 2010 RA criteria positive, n | 629 | 451 | 339 | 1,419 |
| Women | 412 (66) | 313 (69) | 234 (69) | 959 (68) |
| Age at symptom onset, median (IQR) years | 56 (44–68) | 57 (47–69) | 59 (49–69) | 57 (47–68) |
| Symptom duration, median (IQR) weeks | 23 (13–41) | 28 (16–52) | 31 (19–51) | 26 (15–47) |
| RF/ACPA positive | 270 (48) | 247 (58) | 198 (63) | 715 (55)† |
| 1987 ACR RA criteria positive | 411 (65) | 275 (61) | 241 (71) | 927 (65) |
| DAS28, median (IQR) | 4.61 (3.85–5.58) | 4.56 (3.55–5.37) | 4.31 (3.54–4.98) | 4.5 (3.68–5.40)§ |
| DMARDs at baseline assessment | 128 (20) | 170 (38) | 185 (55) | 483 (34) |
Values are the number (% nonmissing data) unless indicated otherwise. EIA = early inflammatory arthritis; IQR = interquartile range; RF = rheumatoid factor; ACPA = anti–citrullinated protein antibody; ACR = American College of Rheumatology; EULAR = European League Against Rheumatism; RA = rheumatoid arthritis; DAS28 = 28-joint Disease Activity Score; DMARDs = disease-modifying antirheumatic drugs.
Missing 280 (11%) EIA and 117 (8%) RA.
Missing 257 (10%) positive and 0 (0%) negative.
Missing 458 (23%) EIA and 217 (15%) RA.
Across the entire time span (all cohorts combined), the all-cause SMR was significantly elevated for the total EIA group (1.16, 95% CI 1.04–1.29) (Table2). The SMR was higher for the patients fulfilling the RA criteria (1.22, 95% CI 1.07–1.40), but not for patients who did not fulfill the 2010 criteria for RA at baseline (0.90, 95% CI 0.73–1.11). The highest SMR was observed in the antibody-positive subgroup (1.39, 95% CI 1.18–1.65).
Table 2.
All-cause and cardiovascular-specific deaths and SMRs by cohort after 7 years of followup*
| No. of observed deaths | SMR (95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| EIA | 2010 RA criteria positive | 2010 RA criteria negative | RF/ACPA positive | EIA | 2010 RA criteria positive | 2010 RA criteria negative | RF/ACPA positive | |
| All cause | ||||||||
| Cohort 1 | 141 | 91 | 28 | 55 | 1.21 (1.02–1.41) | 1.18 (0.96–1.45) | 0.99 (0.69–1.44) | 1.54 (1.18–2.00) |
| Cohort 2 | 123 | 75 | 36 | 44 | 1.17 (0.98–1.40) | 1.30 (1.04–1.63) | 0.89 (0.64–1.23) | 1.25 (0.93–1.68) |
| Cohort 3 | 82 | 44 | 25 | 36 | 1.06 (0.85–1.32) | 1.19 (0.89–1.60) | 0.84 (0.57–1.24) | 1.39 (1.00–1.92) |
| Total | 346 | 210 | 89 | 135 | 1.16 (1.04–1.29) | 1.22 (1.07–1.40) | 0.90 (0.73–1.11) | 1.39 (1.18–1.65) |
| Cardiovascular | ||||||||
| Cohort 1 | 58 | 36 | 9 | 29 | 1.16 (0.90–1.50) | 1.11 (0.80–1.54) | –* | 1.87 (1.30–2.69) |
| Cohort 2 | 45 | 26 | 15 | 12 | 1.07 (0.80–1.43) | 1.13 (0.77–1.66) | 0.92 (0.55–1.52) | –* |
| Cohort 3 | 29 | 15 | 9 | 10 | 1.02 (0.71–1.47) | 1.19 (0.72–1.98) | –* | –* |
| Total | 132 | 77 | 33 | 51 | 1.09 (0.92–1.30) | 1.13 (0.91–1.42) | 0.85 (0.60–1.19) | 1.31 (1.00–1.73) |
SMR = standardized mortality ratio; 95% CI = 95% confidence interval; EIA = early inflammatory arthritis; RA = rheumatoid arthritis; RF = rheumatoid factor; ACPA = anti–citrullinated protein antibody.
Too few events to calculate the SMR.
SMRs were calculated cross-sectionally for each of the 3 consecutive cohorts of patients recruited to the NOAR between 1990 and 2004. There did not appear to be any trend in the SMRs over time among the total EIA population, patients with RA, or those who were antibody positive (Table2). This was confirmed in the Poisson regression, which assessed differences in mortality incidence after taking account of changes within the background population. This analysis showed no significant change in the MRRs in cohorts 2 and 3 compared to cohort 1 for patients with EIA, with RA, or who were antibody positive (Table3).
Table 3.
Poisson regression model by cohort after 7 years of followup*
| MRR (95% CI), unadjusted | MRR (95% CI), adjusted† | |||||||
|---|---|---|---|---|---|---|---|---|
| EIA | 2010 RA criteria positive | 2010 RA criteria negative | RF/ACPA positive | EIA | 2010 RA criteria positive | 2010 RA criteria negative | RF/ACPA positive | |
| All cause | ||||||||
| Cohort 1 | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Cohort 2 | 0.97 (0.77–1.23) | 1.10 (0.81–1.49) | 0.89 (0.55–1.46) | 0.81 (0.55–1.20) | 0.97 (0.77–1.24) | 1.13 (0.84–1.52) | 0.89 (0.54–1.49) | 0.82 (0.56–1.19) |
| Cohort 3 | 0.88 (0.67–1.15) | 1.01 (0.71–1.45) | 0.84 (0.49–1.46) | 0.90 (0.58–1.38) | 0.89 (0.68–1.17) | 1.00 (0.70–1.43) | 0.84 (0.47–1.51) | 0.89 (0.58–1.35) |
| Cardiovascular | ||||||||
| Cohort 1 | Ref. | Ref. | –‡ | –‡ | Ref. | Ref. | –‡ | –‡ |
| Cohort 2 | 0.92 (0.62–1.37) | 1.02 (0.61–1.69) | –‡ | –‡ | 0.94 (0.63–1.39) | 1.07 (0.65–1.76) | –‡ | –‡ |
| Cohort 3 | 0.88 (0.56–1.39) | 1.07 (0.58–1.99) | –‡ | –‡ | 0.93 (0.59–1.46) | 1.08 (0.58–1.98) | –‡ | –‡ |
MRR = mortality rate ratio; 95% CI = 95% confidence interval; EIA = early inflammatory arthritis; RA = rheumatoid arthritis; RF = rheumatoid factor; ACPA = anti–citrullinated protein antibody.
Adjusted for age at symptom onset and sex and symptom duration at baseline.
Too few events to calculate the MRR.
CV mortality was not significantly elevated compared to the general population for the total EIA group overall or for any of the time cohorts. CV mortality was significantly elevated in the antibody-positive subgroup of cohort 1 (SMR 1.87, 95% CI 1.30–2.69). There were insufficient deaths in cohorts 2 and 3 to examine the CV-specific SMR. There was a nonsignificant trend toward increasing CV-specific MRR in the Poisson regression model for the RA subgroup. Again, there were insufficient numbers of deaths to explore this for the antibody subgroup (Tables2 and 3).
Overall, persistently increasing, but stable, mortality rates over time were seen in patients with RA, when modeled by calendar year (Figures 1A and B). The Poisson regression used to create these plots demonstrated no evidence of change in all-cause or CV-specific mortality over time (P = 0.92 and 0.40, respectively).
Figure 1.
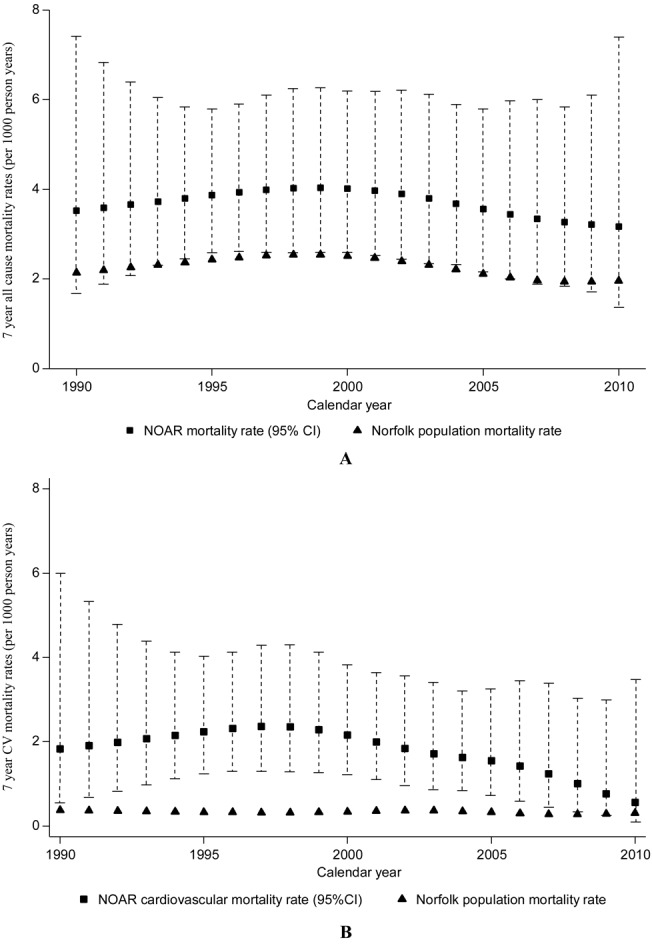
Observed and expected mortality rates by calendar year for all-cause (A) and cardiovascular (CV)–specific (B) mortality. Observed rates were modeled using Poisson regression with natural splines and expected rates were calculated from mortality rates for Norfolk, age and sex standardized to the study population. The y-axes show rates per 1,000 person-years and 95% confidence intervals (95% CIs). NOAR = Norfolk Arthritis Register.
DISCUSSION
We have shown that all-cause mortality in the first 7 years of EIA and RA, defined according to the 2010 ACR/EULAR criteria, is higher than that in the general population, but the SMR has remained stable over the past 20 years. We have demonstrated, for the first time, increased SMRs in patients classified as having RA according to the 2010 ACR/EULAR classification criteria. In addition, crude all-cause and CV mortality rates in the first 7 years from baseline assessment in these patient groups decreased slightly over time; however, this decrease is occurring at the same rate as in the general population.
We were unable to confirm the findings of Gonzalez et al of a widening mortality gap between patients with RA and the general population (8). This may be because we have identified trends in mortality emerging in the 5 years since their study was completed in January 2007. Alternatively, it may be due to case definition; we used the 2010 classification criteria at baseline assessment to define RA, whereas in their study, incident cases of RA were recruited into the study when they fulfilled 4 of 7 of the 1987 criteria, which is likely to be further into the disease process than our baseline assessment. In addition, we restricted our analysis to deaths within the first 7 years of followup in order to standardize comparisons between the cohorts, whereas median followup in Minnesota was 11.7 years, which may have allowed more time for excess deaths to occur. The importance of latency in detecting excess mortality as an outcome was highlighted in a recent study from The Netherlands, which identified increased mortality in an incident cohort of RA patients (symptom duration <1 year at baseline) only after 10 years of followup (3). We also found no decrease in mortality rates over time after accounting for trends in the background population. These findings are consistent with a recent meta-analysis by Dadoun et al (2), who collated 8 studies reporting SMRs of patients with early RA (<2 years' duration) published in 1955–1995. They found that mortality rates in RA patients remain elevated compared to the general population, and had not altered significantly over time. It remains to be seen whether even more aggressive remission-targeted therapy will alter this, whether there will be an impact on mortality in the longer term, or whether, for example, antibody status is an unmodifiable risk factor for decreased survival in patients with IA.
In keeping with previous results from the NOAR (11,12) we found that, in the subgroup of patients who were ACPA or RF positive, there were 40% more deaths than expected. This proportion was higher than in patients who met the RA classification criteria and suggests antibody status plays an important role in the increased mortality seen in RA. RF is an established risk factor for increased mortality in RA (1) and even has been identified as a risk factor in subjects without joint symptoms (16). Since ACPA testing has only been routinely available in the past 5–10 years, the literature examining the relationship between ACPA and mortality in RA is limited. However, a similar association with RF appears to exist (17).
There are limitations to this study. Although SMRs are a widely used measure of mortality risk, comparisons between SMRs measured in different cohorts and time periods must be made with caution. This is because the expected number of deaths is dependent on the length of followup, the age and sex structure of the disease cohort, and the mortality rates in the general population. Although we kept the period of followup constant between the cohorts, the age at onset of EIA increased during the period of the study, and so the expected number of deaths will have risen. We used MRRs to make comparisons between the cohorts and modeled the rates using Poisson regression, adjusted for age at onset and sex and symptom duration at presentation, to allow for these differences.
In conclusion, we have shown that mortality in EIA remains elevated compared to the general population, and mortality rates have not changed significantly over the past 20 years. We have demonstrated, for the first time, increased SMRs in patients satisfying the 2010 ACR/EULAR classification criteria for RA, and further demonstrated the importance of autoantibody status in the excess mortality seen in patients with IA.
AUTHOR CONTRIBUTIONS
All axuthors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Verstappen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design. Humphreys, Warner, Marshall, Symmons, Verstappen.
Acquisition of data. Chipping, Marshall.
Analysis and interpretation of data. Humphreys, Warner, Lunt, Symmons, Verstappen.
REFERENCES
- Sokka T, Abelson B, Pincus T. Mortality in rheumatoid arthritis: 2008 update. Clin Exp Rheumatol. 2008;26(Suppl):S35–61. [PubMed] [Google Scholar]
- Dadoun S, Zeboulon-Ktorza N, Combescure C, Elhai M, Rozenberg S, Gossec L, et al. Mortality in rheumatoid arthritis over the last fifty years: systematic review and meta-analysis. Joint Bone Spine. 2013;80:29–33. doi: 10.1016/j.jbspin.2012.02.005. [DOI] [PubMed] [Google Scholar]
- Radovits BJ, Fransen J, Al Shamma S, Eijsbouts AM, van Riel PL, Laan RF. Excess mortality emerges after 10 years in an inception cohort of early rheumatoid arthritis. Arthritis Care Res (Hoboken) 2010;62:362–70. doi: 10.1002/acr.20105. [DOI] [PubMed] [Google Scholar]
- Smolina K, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database study. BMJ. 2012;344:d8059. doi: 10.1136/bmj.d8059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiyama D, Nishimura K, Tamaki K, Tsuji G, Nakazawa T, Morinobu A, et al. Impact of smoking as a risk factor for developing rheumatoid arthritis: a meta-analysis of observational studies. Ann Rheum Dis. 2010;69:70–81. doi: 10.1136/ard.2008.096487. [DOI] [PubMed] [Google Scholar]
- Health & Social Care Information Centre. 2011. Statistics on smoking: England, 2011. URL: http://www.hscic.gov.uk/
- Saunders SA, Capell HA, Stirling A, Vallance R, Kincaid W, McMahon AD, et al. Triple therapy in early active rheumatoid arthritis: a randomized, single-blind, controlled trial comparing step-up and parallel treatment strategies. Arthritis Rheum. 2008;58:1310–7. doi: 10.1002/art.23449. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Maradit Kremers H, Crowson CS, Nicola PJ, Davis JM, Therneau TM, et al. The widening mortality gap between rheumatoid arthritis patients and the general population. Arthritis Rheum. 2007;56:3583–7. doi: 10.1002/art.22979. III. [DOI] [PubMed] [Google Scholar]
- Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31:315–24. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- Harrison BJ, Symmons DP, Barrett EM, Silman AJ. The performance of the 1987 ARA classification criteria for rheumatoid arthritis in a population based cohort of patients with early inflammatory polyarthritis. J Rheumatol. 1998;25:2324–30. [PubMed] [Google Scholar]
- Goodson NJ, Wiles NJ, Lunt M, Barrett EM, Silman AJ, Symmons DP. Mortality in early inflammatory polyarthritis: cardiovascular mortality is increased in seropositive patients. Arthritis Rheum. 2002;46:2010–9. doi: 10.1002/art.10419. [DOI] [PubMed] [Google Scholar]
- Naz SM, Farragher TM, Bunn DK, Symmons DP, Bruce IN. The influence of age at symptom onset and length of followup on mortality in patients with recent-onset inflammatory polyarthritis. Arthritis Rheum. 2008;58:985–9. doi: 10.1002/art.23402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569–81. doi: 10.1002/art.27584. III. [DOI] [PubMed] [Google Scholar]
- Symmons DP, Barrett EM, Bankhead CR, Scott DG, Silman AJ. The incidence of rheumatoid arthritis in the United Kingdom: results from the Norfolk Arthritis Register. Br J Rheumatol. 1994;33:735–9. doi: 10.1093/rheumatology/33.8.735. [DOI] [PubMed] [Google Scholar]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, tenth revision (ICD-10) 4th ed. Geneva: WHO; 2010. [Google Scholar]
- Tomasson G, Aspelund T, Jonsson T, Valdimarsson H, Felson DT, Gudnason V. Effect of rheumatoid factor on mortality and coronary heart disease. Ann Rheum Dis. 2010;69:1649–54. doi: 10.1136/ard.2009.110536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farragher TM, Goodson NJ, Naseem H, Silman AJ, Thomson W, Symmons D, et al. Association of the HLA–DRB1 gene with premature death, particularly from cardiovascular disease, in patients with rheumatoid arthritis and inflammatory polyarthritis. Arthritis Rheum. 2008;58:359–69. doi: 10.1002/art.23149. [DOI] [PMC free article] [PubMed] [Google Scholar]


