Abstract
Objectives
We sought to characterize emergency department (ED) encounters for pediatric inflammatory bowel disease (IBD) to identify areas for prevention.
Methods
Retrospective chart review of 5 consecutive ED encounters at 7 centers was performed.
Results
Of 35 unique encounters by 32 patients, 3 main factors contributed to ED utilization: disease severity or course, day or time of care, and physician instruction. Of the ED encounters, approximately one-fifth were judged medically unnecessary, and one-half avoidable in a more optimal health care system.
Conclusions
ED visits by pediatric patients with IBD may be reduced in a more optimal health care system.
Keywords: chronic care model, emergency department, inflammatory bowel disease, pediatrics, reducing cost
The direct costs of managing inflammatory bowel disease (IBD) in the United States remain a substantial economic burden (1–3). Pharmaceuticals such as biological agents, hospitalization, and abdominal surgery make up the vast majority of the IBD-attributable costs (4). Reducing the need for these acute care services would represent an improvement in the quality of care for chronic IBD and IBD-related disease management (5). In particular, effective system-level efforts to decrease unnecessary emergency department (ED) encounters would decrease patient risk, reduce direct medical costs, and improve the overall value of IBD care.
Moving away from the traditional volume-based reimbursement model, the health care marketplace is evolving to a value-based reimbursement model, in which integrated delivery networks are incentivized to deliver the best care for lowest costs (6). Under this chronic care model, responsiveness and care coordination—2 characteristics that support patient-centric delivery of medical care—are described as key elements of an optimal health care system (7,8). In health systems, responsiveness refers to the timely delivery of disease-focused care with a patient-defined perspective integrating the individual patient’s needs and priorities (9,10). Care coordination refers to the well-implemented organization of medical care between multiple providers and the patient (11).
The Reducing Cost Strategic Initiative Team of the ImproveCareNow Network, a collaborative, data-driven health care network dedicated to improving the health of children and youth with IBD (12), sought to retrospectively evaluate patterns of ED use in IBD. We hypothesized that a substantial proportion of ED visits for pediatric IBD care would be avoidable in a care model in which providers’ responsiveness and care coordination were readily implementable and consistently reproducible—irrespective of center-, provider-, disease-, and patient-level differences. Specifically, we sought to describe the factors leading to pediatric IBD-related ED visits, and identify those that may be preventable in a more optimal health care system.
METHODS
A subgroup of physicians participating in ImproveCareNow met via a monthly conference call. Over several calls, we generated a list of factors believed to lead to ED visits. These factors were subsequently grouped into categories (Table 1). The categories were developed by general physician consensus as guided by clinical judgment and review of the existing literature on ED utilization.
TABLE 1.
List of factors attributed to ED visits by pediatric patients with IBD, grouped into categories
| Day or time |
| Arrival at ED after 4:00 PM |
| Arrival at ED on weekend or holiday |
| Disease severity or course |
| Acutely ill with mild disease activity |
| Acutely ill with moderate or severe disease activity |
| Worsening disease unresponsive to outpatient therapy |
| Stable disease but unable to manage as an outpatient (multiple calls) |
| Possible failure of outpatient medical management |
| Triggered by infection, including Clostridium difficile |
| Treatment otherwise unavailable |
| Diagnostic test not available on an outpatient basis |
| Medication not available on an outpatient basis |
| Patient preference |
| Anxiety of patient or family |
| Requested by patient or family; patient convenience |
| Patient went to ED without calling any clinician |
| Physician decision |
| Convenience (for the clinician) |
| Told to go to ED by primary care or another specialty physician |
| Told to go to ED by pediatric gastroenterology clinician |
| Management by fellow or resident |
| Communication factors |
| Poor communication to patient or family |
| Poor communication from patient or family |
| Patient not reporting (hiding) symptoms |
| Appointment access |
| Lack of access to timely appointments |
| Clinician not available to see patient in clinic |
| Not seen in clinic often enough |
| Transportation issue: lack of transportation or long distance from clinic |
| Diagnostic factors |
| Unclear diagnosis |
| Comorbidity |
| Consultation not available on an outpatient basis |
| Medication factors |
| Nonadherence |
| Wrong drug or wrong dose of medication |
| Weaning prednisone |
| Before next infliximab infusion |
ED = emergency department.
Providers from 3 academic and 4 private practice groups in the United States retrospectively evaluated the 5 most recent and consecutive ED encounters for care of pediatric patients with IBD. For each visit, the likely factors that led to the encounter and the most important contributing factors were recorded. Based on an agreed-upon scale, a clinical judgment was made regarding the necessity of the ED visit and a score was assigned. Similarly, a separate score was generated for the probability of avoiding the ED visit in a more responsive and coordinated health care system. The investigator retrospectively evaluating the medical records contributed only deidentified data for analysis.
RESULTS
We generated a list of 35 factors that may lead to ED visits. These were organized into 9 general categories (Table 1). Retrospective review of consecutive ED visits at each site identified 32 unique patients, representing 35 ED encounters. For the 32 unique patients, the type of IBD was Crohn disease in 21 (66%), ulcerative colitis in 9 (28%), and indeterminate colitis in 2 (6%). Of the 35 ED encounters, 8 (23%) were preplanned admissions, whereas 15 (43%) led to inpatient admission after evaluation in the ED. In sum, 23 of 35 (66%) of ED encounters resulted in admission.
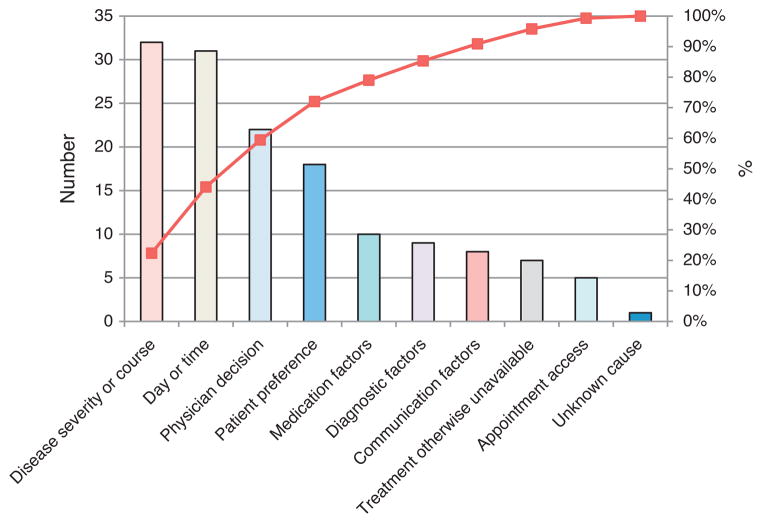
Analysis of the factors leading to the ED encounter identified 3 main categories as most common (Fig. 1). These were disease severity or course, day or time, and physician instruction to go to the ED. Factors in disease severity or course include items such as acute illness, progressive worsening of chronic illness, concern for failure of outpatient management, and suspected or known infection. Day or time referred to an evening or late night, weekend, or holiday outside of usual outpatient business hours and availability of the provider or IBD team. The physician decision category included instruction to the family to go to the ED by a primary care provider, the on-call gastroenterology attending, gastroenterology fellow, or other care provider.
FIGURE 1.
Pareto chart analysis of factors leading to emergency department visits by patients with IBD, ranked by category. The line plots the cumulative total. IBD = inflammatory bowel disease.
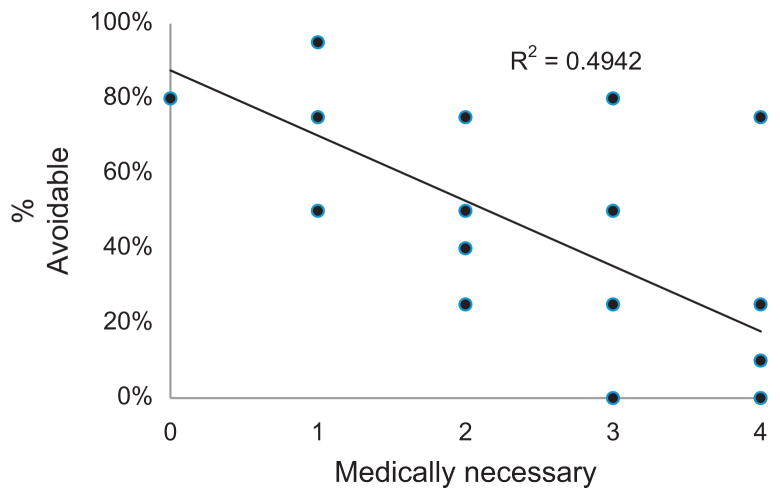
Of the 35 ED encounters, 7 (20%) were judged to be medically unnecessary and 17 (50%) avoidable in a more responsive and coordinated health care system. There was a strong correlation (r = 0.7) between the estimate of necessity for ED encounter and how preventable the visit may be in an optimal health care system (Fig. 2).
FIGURE 2.
Regression chart showing the correlation between the estimate of the medical necessity for the emergency department visit and the avoidability of the visit in a more optimal health care system.
DISCUSSION
We report a retrospective review of ED use for pediatric IBD care. We found that most ED encounters related to issues of disease management, day or time of need for care, and care provider instruction to go to the ED. In the present analysis, approximately one-half of all ED encounters by pediatric patients with IBD were considered to be avoidable in a more responsive and coordinated health care system.
The pilot work we showcase here stems from 2 assumptions. The first one is that a health care system delivering care with responsiveness and care coordination will improve quality of care for pediatric patients with IBD. The second is that many pediatric IBD encounters in the ED setting are avoidable in a more optimal health care system.
Our findings are consistent with a more in-depth analysis on typical ED use. In a recent analysis by the RAND Corporation (5), 354 million acute care visits per year account for more than one-third of all medical encounters in the United States. More than one-half of these visits were in the ED without the involvement of the patient’s primary care provider. These authors found that timeliness and medical complexity were the 2 main barriers to receive acute care in the primary care setting—consistent with our findings. An analysis of a nationally representative data set highlights that IBD-related ED visits are increasing and that younger, self-pay patients with IBD are more likely to use the ED instead of the ambulatory care setting (13).
Translating these data, there are several opportunities for pediatric gastroenterologists to improve IBD care. First is process improvement stemming from a value-based chronic care model that emphasizes evidence-based and individualized treatment. Achieving a high-value health care system for IBD may include personalized patient education and structuring multidisciplinary services around individualized, and often different, patient needs. For example, psychological support or social services may need more integration for one patient, whereas health coaching and a dietitian are needed for another. Second is IBD care planning, especially for ED triage, aimed to enhance responsiveness and care coordination. For example, each IBD center or program may develop plans to improve communication with providers and patients beyond usual business hours. Creative new ways may enable the “informed and activated” (14) patient with IBD and family to access their primary care services for acute care not requiring ED or subspecialty services. Third is for IBD programs to actively leverage innovation and health technology to engage patients in a responsive way. For example, the use of telemedicine (15) or a bidirectional electronic health record (16) has been shown to improve patient–provider connectedness and health outcomes in various chronic disease states, including IBD (17). Meaningful use of new technology to bridge the gap in care will continue to be an important evolving policy discussion.
Limitations of the present study include assessment of a small number of ED visits using a retrospective design and the fact that important data such as insurance type, presence of primary care provider, and distance to center were not obtained. The chart review by a nonblinded IBD clinician could introduce investigator bias when evaluating retrospectively the need for acute medical care in the ED. Strengths of the present study include the multicenter collaborative effort across geographical and practice model differences, the lack of pediatric-specific data, and development of initial tools to evaluate causes and need for pediatric IBD encounters in the ED.
In conclusion, our pilot investigation provides a unique snapshot of the types of pediatric patients with IBD managed in the ED setting. Although validation is needed with larger sample size, our work strengthens the notion that ED services are overused in pediatric IBD. A rapidly changing national health care system provides the contextual framework to generate informed discussion and develop collaborative quality improvement strategies to reduce unnecessary ED encounters by pediatric patients with IBD.
Footnotes
The authors report no conflicts of interest.
References
- 1.Gunnarsson C, Chen J, Rizzo JA, et al. Direct health care insurer and out-of-pocket expenditures of inflammatory bowel disease: evidence from a US national survey. Dig Dis Sci. 2012;57:3080–91. doi: 10.1007/s10620-012-2289-y. [DOI] [PubMed] [Google Scholar]
- 2.Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007;5:1424–9. doi: 10.1016/j.cgh.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Park KT, Bass D. Inflammatory bowel disease-attributable costs and cost-effective strategies in the United States: a review. Inflamm Bowel Dis. 2011;17:1603–9. doi: 10.1002/ibd.21488. [DOI] [PubMed] [Google Scholar]
- 4.Stone CD. The economic burden of inflammatory bowel disease: clear problem, unclear solution. Dig Dis Sci. 2012;57:3042–4. doi: 10.1007/s10620-012-2417-8. [DOI] [PubMed] [Google Scholar]
- 5.Pitts SR, Carrier ER, Rich EC, et al. Where Americans get acute care: increasingly, it’s not at their doctor’s office. Health Aff (Millwood) 2010;29:1620–9. doi: 10.1377/hlthaff.2009.1026. [DOI] [PubMed] [Google Scholar]
- 6.Allen JI. Health care reform 3. 0: the road gets bumpy. Clin Gastroenterol Hepatol. 2013;11:1527–8. doi: 10.1016/j.cgh.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Smith M, Saunders R, Stuckhardt L, et al. [Accessed August 5, 2014];Best care at lower cost: the path to continuously learning health care in America. http://www.iom.edu/reports/2012/best-care-at-lower-cost-the-path-to-continuously-learning-health-care-in-america.aspx. Published 2012. [PubMed]
- 8.Coleman K, Austin BT, Brach C, et al. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28:75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nolte E, McKee M. Caring for People With Chronic Conditions: A Health System Perspective. Berkshire, UK: World Health Organization; 2008. [Google Scholar]
- 10.Wagner EH, Austin BT, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 11.McDonald K, Schultz E, Albin L, et al. Care Coordination Atlas Version 3. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 12.Billett AL, Colletti RB, Mandel KE, et al. Exemplar pediatric collaborative improvement networks: achieving results. Pediatrics. 2013;131 (suppl 4):S196–203. doi: 10.1542/peds.2012-3786F. [DOI] [PubMed] [Google Scholar]
- 13.Ananthakrishnan AN, McGinley EL, Saeian K, et al. Trends in ambulatory and emergency room visits for inflammatory bowel diseases in the United States: 1994–2005. Am J Gastroenterol. 2010;105:363–70. doi: 10.1038/ajg.2009.580. [DOI] [PubMed] [Google Scholar]
- 14.Hibbard JH, Stockard J, Mahoney ER, et al. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39 (4 pt 1):1005–26. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krier M, Kaltenbach T, McQuaid K, et al. Potential use of telemedicine to provide outpatient care for inflammatory bowel disease. Am J Gastroenterol. 2011;106:2063–7. doi: 10.1038/ajg.2011.329. [DOI] [PubMed] [Google Scholar]
- 16.Adler-Milstein J, DesRoches CM, Jha AK. Health information exchange among US hospitals. Am J Manag Care. 2011;17:761–8. [PubMed] [Google Scholar]
- 17.Rejler M, Spangeus A, Tholstrup J, et al. Improved population-based care: implementing patient-and demand-directed care for inflammatory bowel disease and evaluating the redesign with a population-based registry. Qual Manag Health Care. 2007;16:38–50. doi: 10.1097/00019514-200701000-00006. [DOI] [PubMed] [Google Scholar]