Abstract
Background
The emerging evidence of the effects of sedentary time on health outcomes suggests a need to better measure this exposure. Healthcare settings, however, are not equipped with a tool that can quickly assess the sedentary habits of their patient population. The purpose of this study was to validate a tool for rapidly quantifying and tracking the sedentary time and low levels of daily lifestyle physical activity among primary care patients.
Methods
The study examined the test-retest reliability and validity of the Rapid Assessment Disuse Index (RADI) among adult patients from a large primary care clinic. Patients completed the RADI (comprised of 3 items: sitting, moving, and stair climbing) twice, followed by accelerometer monitoring. Test-retest reliability was computed, and the correlation between survey responses and accelerometry was determined. An ROC curve was constructed and the area under the curve (AUC) was calculated.
Results
RADI was temporally stable (intraclass correlation coefficients 0.79), and a higher score was significantly correlated with greater sedentary time (ρ=0.40; p<0.01), fewer sedentary to active transitions (ρ=−0.42; p<0.01), and less light-intensity physical activity (ρ=−0.40; p<0.01). The ability of RADI to detect patients with high levels of sedentary time was fair (AUC=0.72).
Conclusions
This brief assessment tool, designed to quickly identify patients with high levels of sitting and low daily physical activity, exhibits good reliability and moderate validity. RADI can assist in providing recommendations at the point of care pertaining to modifying sedentary behavior.
Introduction
The aetiological relation between sedentary behaviour, defined as time in a sitting or reclining posture with energy expenditure between 1.0 and 1.5 metabolic equivalents, and the risk of morbidity and mortality from chronic diseases throughout the lifespan is emerging.1–4 For example, van der Ploeg et al5 and Patel et al6, in large prospective cohort studies, found that sitting time independently predicted mortality, while adjusting for physical activity. Healy et al7, analysing data from the National Health and Nutrition Examination Survey, found that prolonged sedentary time (measured objectively via accelerometers) was independently associated with cardiometabolic risk, for example, elevated triglycerides and markers of insulin resistance. These findings suggest that the mechanism through which sedentary behaviour is linked to disease risk is not simply the inverse of those attributed to physical activity.
Indeed, experimental studies of glucose and lipid metabolism have demonstrated that sedentary behaviour elicits a number of cellular adaptations that are quite distinct from those elicited by exercise training.8,9 Prolonged sedentary time appears to decrease the levels of lipoprotein lipase (LPL), an enzyme facilitating the uptake of fatty acids into muscles and adipose tissue.9 Hence, high levels of sedentary behaviour result in low LPL levels, which lead to increased triglycerides and decreased high-density lipoprotein.10 In addition, brief periods of immobility have been found to affect the expression of numerous genes9; however, further research is needed to elucidate the causal role of sedentary behaviour on physiological function and related processes.
The evidence nonetheless supports the need to assess and promote the reduction of sedentary time alongside increasing physical activity levels.5,11 Historically, sedentary behaviour has been measured simply as the absence of any reported leisure time physical activity. More recently, researchers have begun to evaluate time spent sitting or in passive activities (eg, television viewing and computer use) at work and during discretionary time. A few studies have examined the validity of questionnaires (eg, Community Healthy Activities Model Program for Seniors (CHAMPS)) focusing on sedentary behaviours12–15; however, these surveys have not been designed specifically for the clinical setting. In the current study, we present a brief assessment tool designed for use in the clinical setting to quickly identify patients who would benefit from clinician counselling focusing on decreasing the time per day spent sitting and increasing the daily lifestyle physical activity. This tool, the Rapid Assessment Disuse Index (RADI), is comprised of three questions aimed at measuring sitting time as well as general moving about and stair climbing behaviours (ie, lifestyle physical activity parameters). We evaluated the reliability and validity of RADI among adult primary care patients. In addition, we established risk cutoff points based on RADI’s score cross-sectional association with objectively measured sedentary time (measured via accelerometers), which might guide the clinician when making recommendations pertaining to sedentary behaviour and lifestyle physical activity.
Methods
Study design and participants
This study examines the test–retest reliability and validity of the RADI survey among patients in a primary care setting. Participants were adult men and women aged 40–79 years from a large academic primary care clinic in Dallas, Texas, USA. Inclusion and exclusion criteria for this study as well as participants’ sociodemographics have been described previously.16 Briefly, patients were excluded if they: did not consent to participate; had physical disabilities that restricted lower limb function; were cognitively impaired; had a medical procedure in the past year that restricted their usual physical function and/or activity; were pregnant; or replied positively to one or more of the Physical Activity Readiness (PAR-Q) screening test questions, such as indicating feeling chest pain when physically active.17 Thus, a total of 179 patients were eligible and interested in the study and completed a questionnaire on a computer interface at baseline.18 Of these, 157 (87.7%) completed the survey again in the clinic 12–16 days after completing the baseline questionnaire. Completion time for the questionnaire ranged from 2 to 5 min. The participants who completed the survey in the clinic were given an accelerometer to wear on their right hip for 7 days and asked to wear it during all waking hours. They were asked to return the accelerometers to the research team by mail after the 7-day period. A total of 155 (98.7%) participants returned the accelerometers and of these 151 (97.4%) accelerometers had valid wear time (ie, accelerometers were worn for ≥10 h per day for at least 4 days). Data collection began in December 2010 and ended in June 2011. The study protocol was approved by the Institutional Review Boards of the University of Texas Health Science Center at Houston and the UT Southwestern Medical Center at Dallas, Texas, USA.
Measures
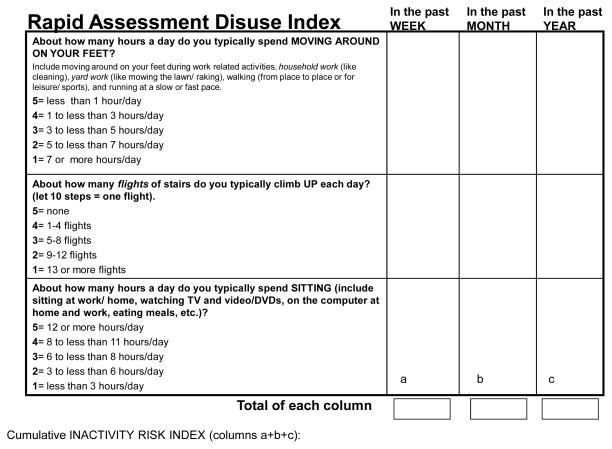
The RADI
RADI (figure 1) is a brief assessment tool for use in time-constrained clinical practice. It is based on three questions from the Yale Physical Activity Survey,19 pertaining to general domains of daily activity (eg, moving about and climbing stairs) and sitting behaviour. RADI is self-administered and is presented as a matrix that can be completed in 5 min or less. The participants were asked to complete the matrix with reference to the past week, month and year. They then answered each RADI question by selecting the number that best corresponded to their behaviour in the appropriate box (figure 1). The two RADI questions related to lifestyle activity (moving about and stair climbing) are reverse scored, that is, higher scores are indicative of less moving about and fewer stairs climbed; whereas the sitting score is directly scored, that is, a higher score is indicative of more sitting. The matrix is scored by summing the numbers for each column and then across the three time periods. The total for column ‘A’ corresponds to the current ‘disuse’ index score, which ranges from 3 to 15; the total across columns ‘A’, ‘B’ and ‘C’ is the cumulative ‘disuse’ index (ie, the cumulative RADI score), which ranges from 9 to 45. Higher scores indicate higher levels of ‘disuse’ (ie, a combination of more sitting and less activity).
Figure 1.
Rapid Assessment Disuse Index Tool
Accelerometers
The ActiGraph GT3X accelerometer (Pensacola, Florida, USA) is a small, triaxial piezoelectric device (4.6×3.3×1.5 cm; 19 g) that measures physical activity including raw acceleration, activity counts (ct) and vector magnitude. The data output from the accelerometer are activity cts, which quantify the amplitude and frequency of detected accelerations; the activity cts are summed over an investigator-specified time interval (ie, epoch). For the current study, a 60 s epoch was utilised. Technical specifications, as well as reliability and validity of the ActiGraph accelerometer, have been described previously.20,21 Data from the accelerometer were downloaded and screened for wear time using the methods described by Troiano et al.22 Briefly, device non-wear was defined as 60 consecutive minutes of 0 cts, with an allowance of 1–2 min for cts detected between 0 and 100. Wear time was determined by subtracting derived non-wear time from 24 h. Time spent per day (min/day) in different intensity levels was estimated using the following cut-off points: sedentary [0–99 ct/min], light (100–1951 ct/min), moderate (1952–5724 ct/min) and vigorous (≥5725 ct/min) intensity.23,24 Sedentary to active transitions (ie, sedentary breaks) were defined as an interruption in which a period of sedentary time was immediately followed by a minute or more ≥100 cts; breaks were summed over each day and are presented after adjustment for sedentary time.1,25 A summary estimate of time spent per day in moderate-to-vigorous intensity physical activity (MVPA) was computed using a threshold of ≥1952 ct/min. Summary estimates were computed by averaging the daily estimates across the total number of days worn for participants with ≥4 days with ≥10 h/day of wear time.
Covariates
Personal information (ie, age, gender and race/ethnicity) was gleaned from responses to a survey, and body mass index (BMI) was abstracted from the patients’ electronic medical records and based on measurements within the past 12 months. Based on BMI (kg/m2), participants were classified as normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) or obese (≥30.0 kg/m2).26
Statistical analysis
We computed intraclass correlation coefficients and 95% CIs to determine the degree of shared variance between the two administrations of RADI. To establish criterion validity, we compared RADI scores from the second administration to accelerometer estimates, since the survey completion was temporally sequenced with accelerometer wear time. Hence, we computed the correlation coefficient (Spearman’s ρ) among each survey item, the cumulative RADI scores (past week, month and year) and accelerometer-derived estimates of sedentary time, sedentary breaks and light intensity and MVPA, after adjustment for average daily accelerometer wear time. We also calculated Spearman’s partial correlations to adjust for age, gender, race/ethnicity and BMI. For the cumulative RADI score, we combined reports from the past week, month and year due to high internal consistency (Cronbach’s α range: 0.935–0.955). In addition, to determine the accuracy of RADI, a receiver operating characteristic (ROC) curve was constructed by comparing the cumulative RADI score (second administration) to accelerometer-derived sedentary time (highest quartile of sedentary time vs lower quartile). In the ROC curve, the sensitivity is plotted as a function of 1-specificity, thus enabling us to calculate the sensitivity and specificity for several cut-off points. Furthermore, to determine the accuracy of the test, the area under the curve (AUC) was calculated, where an AUC of 1.0 indicates a perfect test and 0.5, for example, is indicative of a poor test.
Results
The test–retest reliability for the RADI domains (moving, stair climbing and sitting) ranged from moderate to strong agreement (ie, ICCs 0.5–0.7), with the cumulative score exhibiting a strong agreement (table 1). Results pertaining to the criterion validity of RADI, assessed by comparing survey responses to accelerometer estimates, appear in table 2. The cumulative RADI score was directly correlated with sedentary time (Spearman’s ρ=0.402; p<0.001) and inversely correlated with sedentary breaks (Spearman’s ρ=−0.425; p<0.001) and light activity (Spearman’s ρ=−0.406; p<0.001), while adjusting for accelerometer wear time, age, gender, race/ethnicity and BMI. The RADI cumulative score was not significantly correlated with MVPA. Similarly, the sitting scores (past week, past month and past year) were significantly associated with sedentary time (direct correlation), sedentary breaks and light activity (inverse correlations), but not MVPA. In addition, the moving scores were inversely correlated with sedentary breaks and light activity and were directly correlated with sedentary time (table 2). In contrast, stair climbing was not significantly correlated with accelerometer estimates in the adjusted models.
Table 1.
Test-retest Reliability* of the Rapid Assessment Disuse Index (RADI): RADI and domain-specific Scores- (N=157)
| Domain | ICC (95%CI) |
|---|---|
| Moving† | |
| Week | 0.726 (0.642–0.793) |
| Month | 0.672 (0.573–0.751) |
| Year | 0.665 (0.568–0.744) |
| Stairs‡ | |
| Week | 0.735 (0.652–0.800) |
| Month | 0.644 (0.542–0.727) |
| Year | 0.588 (0.476–0.681) |
| Sitting§ | |
| Week | 0.559 (0.442–0.658) |
| Month | 0.576 (0.462–0.672) |
| Year | 0.602 (0.491–0.693) |
| RADI Scores¶ | |
| Week | 0.775 (0.704–0.830) |
| Month | 0.737 (0.656–0.801) |
| Year | 0.710 (0.623–0.780) |
| Cumulative RADI score** | 0.793 (0.727–0.845) |
RADI, Rapid Assessment Disuse Index.
Test–retest reliability was determined through intraclass correlation coefficients and 95% CIs to determine the degree of shared variance between two survey administrations.
Moving—a score based on the number of hours spent per day ‘moving about’ (eg, during household work) in the past week, month and year.
Stairs—a score based on the number of flights of stairs climbed up each day in the past week, month and year.
Sitting—a score based on the number of hours per day sitting in the past week, month and year.
RADI score—a combination of the moving, stairs, and sitting scores summed separately for the past week, month and year.
The cumulative RADI score is a sum of the RADI scores in the past week, month and year.
Table 2.
Correlation (Spearman) between Rapid Assessment Disuse Index (RADI) Scores and accelerometer estimates (N=151)
| Accelerometers | Sedentary Time,† min/day | Sedentary Breaks† | Light Activity,† min/day | MVPA,† min/day | ||||
|---|---|---|---|---|---|---|---|---|
| RADI | Models‡ | Models‡ | Models‡ | Models‡ | ||||
| 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | |
| Moving§ | ||||||||
| past week | 0.376*** | 0.396*** | −0.420*** | −0.436 | −0.399*** | −0.418*** | −0.038 | −0.056 |
| past month | 0.390*** | 0.398*** | 0.492*** | −0.490* | −0.427*** | −0.432*** | 0.004 | −0.002 |
| past year | 0.397*** | 0.394*** | −0.467*** | −0.460*** | −0.418*** | −0.412*** | −0.065 | −0.059 |
| Stairs¶ | ||||||||
| past week | 0.065 | 0.047 | −0.057 | −0.008 | −0.029 | −0.006 | −0.128 | −0.091 |
| past month | 0.155* | 0.136 | −0.138 * | −0.088 | −0.126) | −0.103 | −0.136* | −0.097 |
| past year | 0.160* | 0.116 | −0.167** | −0.127 | −0.151* | −0.101 | −0.077 | −0.048 |
| Sitting†† | ||||||||
| past week | 0.291*** | 0.279*** | −0.297*** | −0.290*** | −0.302*** | −0.291*** | −0.004 | −0.008 |
| past month | 0.189** | 0.170** | −0.214*** | −0.204*** | −0.201*** | −0.187** | 0.051 | 0.062 |
| past year | 0.245*** | 0.231*** | −0.218*** | −0.221*** | −0.244*** | −0.233*** | −0.038 | −0.040 |
| RADI Scores‡‡ | ||||||||
| past week | 0.392*** | 0.379*** | −0.406*** | −0.370*** | −0.391*** | −0.376*** | −0.088 | −0.077 |
| past month | 0.392*** | 0.371*** | −0.437*** | −0.403*** | −0.400*** | −0.379*** | −0.056 | −0.030 |
| past year | 0.399*** | 0.372*** | −0.424*** | −0.407*** | −0.407*** | −0.377*** | −0.077 | −0.067 |
| Cumulative RADI score§§ | 0.425*** | 0.402*** | −0.453*** | −0.425*** | −0.431*** | −0.406*** | −0.081 | −0.063 |
p<0.10.
p<0.05.
p≤0.01
Time spent per day (min/day) in different intensity levels was estimated using threshold values proposed by Freedson. Resulting activity count (ct) ranges for sedentary (0–99 ct/min), light—(100–1951 ct/min) and moderate-to-vigorous (MVPA) intensity (≥1952). Sedentary to active transitions (ie, sedentary breaks) were defined as an interruption in which a period of sedentary time was immediately followed by a minute or more ≥100 cts; breaks were summed over each day and are presented after adjustment for sedentary time.
Model 1 adjusts for accelerometer wear time, and model 2 adjusts for accelerometer wear time+age, gender, race/ethnicity and body mass index. The rapid assessment disuse index time two score is compared to the accelerometer estimates since it is temporally sequenced.
Moving—a score based on the number of hours spent per day ‘moving about’ (eg, during household work) in the past week, month and year.
Stairs—a score based on the number of flights of stairs climbed up each day in the past week, month and year.
Sitting—a score based on the number of hours per day sitting in the past week, month and year.
RADI score—a combination of the moving, stairs and sitting scores summed separately for the past week, month and year.
The cumulative RADI score is a sum of the RADI scores in the past week, month and year.
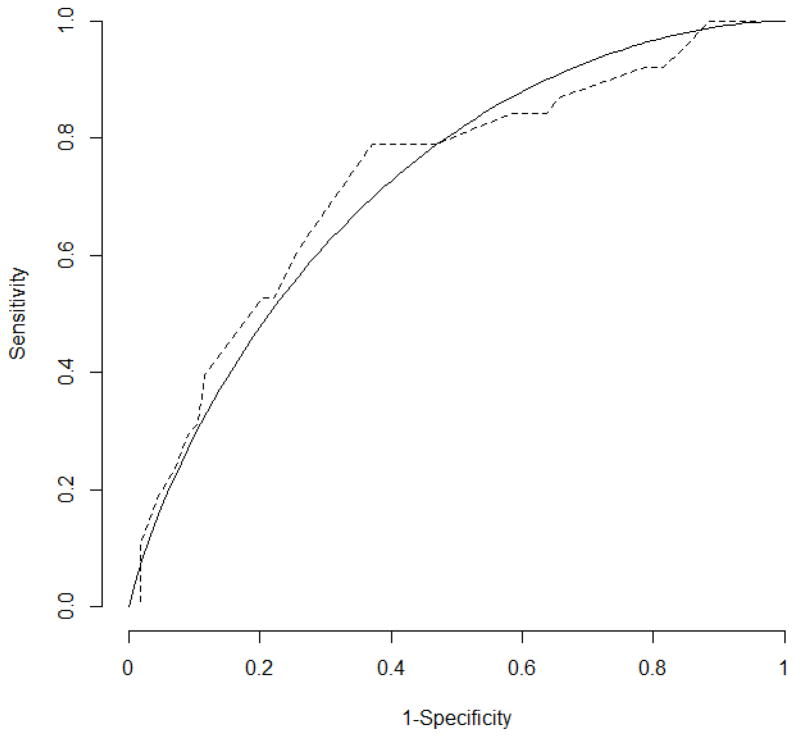
The accuracy of RADI, as well as the ability of the survey to distinguish between individuals with high levels of sedentary time and those with lower levels, was determined through an ROC curve (figure 2). The results revealed that the accuracy of the survey was fair (AUC=0.722). Overall, there was a general trend towards higher sensitivity and lower specificity with lower cut-off points. Hence, an RADI score of 27 resulted in a sensitivity of 0.60 and specificity of 0.74; a score of 26 resulted in sensitivity 0.79 and specificity 0.63, and when the RADI score was 25, the sensitivity remained constant (0.79) and specificity decreased (0.59).
Figure 2.
Receiver operating characteristics curves for the Rapid Assessment Disuse Index cumulative score compared to accelerometer-derived sedentary time. The dotted line is the empirical ROC curve whereas the solid line is the parametric ROC curve. The area under the curve is 0.722. The RADI score is compared to the highest quartile of accelerometer derived sedentary time (adjusted for wear time). The RADI time two score is compared to accelerometer estimates since it is temporally sequenced.
Discussion
The present study aimed to establish the test–retest reliability and validity of an assessment tool designed for use in clinical practice to identify patients who are at risk of high levels of inactivity and who would benefit from clinician counselling pertaining to decreasing time per day spent sitting while increasing daily lifestyle activity. RADI is the first such instrument designed for a clinical setting that can be utilised by providers and patients to identify and modify sedentary time and physical inactivity, which are modifiable risk factors for chronic disease morbidity and mortality.1–3,11 Study findings reveal that the cumulative RADI scale’s test–retest reliability was strong. In terms of validity, a higher cumulative RADI score was significantly correlated with increased sedentary time, as well as with fewer sedentary breaks and decreased light physical activity, as measured by accelerometers. The ability of RADI to distinguish between patients with high levels of sedentary time was fair.
When compared with other studies, the RADI tool exhibited similar reliability and validity traits to longer, more cumbersome questionnaires. For example, the CHAMPS questionnaire, which assesses sedentary behaviour and physical activity in older adults, displayed similar test–retest reliability (correlation coefficients ranging from 0.56 to 0.70).15 Our tool displayed higher correlations when comparing some self-report measures to accelerometry, such as the correlation between reported sedentary behaviour (or sitting time) to accelerometer estimated sedentary time (current study–Spearman’s ρ=0.40; CHAMPS–Spearman’s ρ=0.12).15 Though the study by Gardiner et al12 observed comparable reliability and validity attributes to our study, their survey was longer and measured a number of sedentary behaviours (eg, TV viewing and commute time), rather than a global index in the present study.
The current study extends previous work not only by developing a useful, brief assessment tool, but also by developing a global ‘disuse’ score that combines sitting and lifestyle activity. This index can be used for clinical screening of inactivity as well as an intervention tool for decreasing sitting and encouraging lifestyle activity. For screening, various cut-off points of the cumulative RADI score provide different sensitivity (the ability to correctly detect those with high levels of sedentary time) and specificity (the ability to correctly identify individuals with lower levels of sedentary time) values.26 In general, a lower RADI cut-off point was associated with higher sensitivity and lower specificity of RADI. This trade-off between sensitivity and specificity is common when changing the cut-off levels, and entails deciding between higher percentages of false positives or, conversely, a higher level of false negatives.27 In this case, since RADI can be utilised as a screening measure to capture high levels of sedentary time, we suggest an RADI score of 26. This cut-off point provides a sensitivity of 79% with fewer false negatives and more false positives (63% specificity). Though not a perfect measure, it is the first instrument intended for primary care and is comparable to the Stanford Brief Activity Survey, which exhibited a sensitivity of 73% and specificity of 61% in detecting meeting physical activity guidelines.28 Therefore, patients receiving an RADI score of 26 or higher should reduce this score by decreasing sitting as well as increasing lifestyle activity (via moving and stair climbing). In addition, since higher RADI scores were linked in this study to fewer sedentary breaks, patients should also be encouraged to take intermittent ‘activity’ breaks from sitting, such as walking around the office or home, which have been linked to reduced metabolic risk.1
Interpretation of the study’s findings should be tempered by its limitations. The study sample consists of adults and older adults from one primary care clinic in Dallas (Texas, USA) which impacts the external validity of the study. Further validation of this tool is needed in additional samples and settings. Furthermore, though the number of participants is comparable to other validation studies, 12,14,29 the sample consists of more women than men, thus limiting our ability to stratify by gender in the analysis, which we attempted to compensate for by adjusting for this variable. In addition, when determining the criterion validity of RADI, we compared self-reported sitting time and lifestyle activity to accelerometer estimates. Though accelerometers are often used to establish criterion validity, they are not a gold standard for free-living activity since they underestimate upper body movement and are not worn during water activities, such as swimming.29 Moreover, the accelerometers utilised in this study are mounted on the waist and are not sufficiently sensitive to postural changes, thus making it difficult to discern sitting from standing or reclining and activity type. This might explain the lack of significant association observed (in adjusted models) when comparing stair climbing to accelerometry. Hence, further validation of RADI is warranted with sensors that are able to detect body as well as postural positioning (eg, activPAL accelerometer).
In conclusion, given the increasing trends of sedentary and physical inactivity in the population, there are enormous public health benefits in identifying and modifying these behaviours, which have demonstrated a strong correlation with impaired health and function.5,18 The current study offers a tool that is tailored to the primary care setting and is comparable in its measurement properties to longer, more cumbersome surveys.12,14 RADI can assist in providing recommendations for decreasing sedentary behaviour and increasing lifestyle activity at the point of care. It could be integrated into a sedentary behaviour/lifestyle activity prescription for which specific goals would be set jointly by the patient and clinician based on the RADI score.16,30,31 Future research, however, is needed that explores ways to integrate the RADI tool into clinical practice, followed by testing its feasibility, utility and efficacy in modifying patients’ sedentary behaviour and lifestyle activity in the primary care setting.
What are the new findings?
Accumulating evidence linking prolonged sedentary time to increased risk for chronic disease morbidity and mortality suggests a need to better measure this exposure.
Although a number of studies have examined the validity of sedentary behaviour surveys, none are designed specifically for a clinical setting.
The current study validates The Rapid Assessment Disuse Index (RADI), an assessment tool which measures sedentary time and low levels of lifestyle physical activity among primary care patients.
This brief assessment tool (2–5 min to complete) exhibits good reliability and moderate validity in a primary care setting.
How might it impact on clinical practice in the near future?
The Rapid Assessment Disuse Index (RADI) could assist in providing recommendations for decreasing sedentary behaviour and increasing lifestyle activity at the point of care.
It could be integrated into a sedentary behaviour/lifestyle activity prescription for which specific goals would be set jointly by the patient and clinician based on the RADI score.
Future research, however, is needed that explores ways to effectively integrate RADI into clinical practice.
Acknowledgments
The authors would like to thank Katharine McAlister (project manager), Emily Hébert, Master of Public Health and the research team from the University of Texas Southwestern Medical Center. They also wish to express their gratitude to the patients who took part in the study. In addition, the authors confirm that all patient/personal identifiers have been removed or disguised so that the patient/person(s) described are not identifiable and cannot be identified through the details of the case.
Funding This work was conducted with support from the Center for Translational Medicine, NIH/NCATS Grant Number UL1TR000451. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Center for Translational Medicine, UT Southwestern Medical Center and its affiliated academic and healthcare centres, the National Center for Advancing Translational Sciences, or the National Institutes of Health.
Footnotes
Contributors All authors contributed significantly to justify authorship. KS, HWK, IB, DC, KPG, CEB, LY and LDP contributed to the interpretation and discussion of findings and participated in the editing and rewriting of the article lead by KS (guarantor). LDP, KS and HWK were responsible for the study conception and design. KS, IB, DC and KPG were responsible for the data analysis.
Ethics approval The study protocol was approved by the Institutional Review Boards (IRB) of the University of Texas (UT) Health Science Center at Houston and the UT Southwestern Medical Center at Dallas, Texas, USA.
Data sharing statement The current validation study utilises data from the Rapid Assessment Disuse Index (RADI) study. A previous publication in the journal describes sedentary behaviour counselling practices in primary care.
References
- 1.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Simmet PZ, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–6. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 2.Wijndaele K, Healy GN, Dunstan DW, Barnet AG, Salmon J, Shaw JE, et al. Increased Cardio-Metabolic Risk is Associated with Increased TV Viewing Time. Med Sci Sports Exerc. 2010;42:1511–18. doi: 10.1249/MSS.0b013e3181d322ac. [DOI] [PubMed] [Google Scholar]
- 3.Thorp AA, Healy GN, Owen N, Salmon J, Ball K, Shaw JE, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004–2005. Diabetes Care. 2010;33:327–34. doi: 10.2337/dc09-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sedentary Behaviour Research Network. Letter to the editor: Standardized use of the terms “sedentary” and “sedentary behaviours”. Appl Physiol Nutr Metab 2012. 2012;37:540–42. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 5.van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med. 2012;172:494–500. doi: 10.1001/archinternmed.2011.2174. [DOI] [PubMed] [Google Scholar]
- 6.Patel AV, Bernstein L, Deka A, Feigelson HS, Campbell PT, Gapstur SM, Colditz GA, Thun MJ. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419–29. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio- metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–97. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Booth FW, Gordon SE, Carlson CJ, Hamilton MT. Waging war on modern chronic diseases: primary prevention through exercise biology. J Appl Physiol. 2000;88:774–87. doi: 10.1152/jappl.2000.88.2.774. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56:2655–67. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 10.Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35:725–40. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- 11.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38:105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gardiner PA, Clark BK, Healy GN, Eakin EG, Winkler EA, Owen N. Measuring older adults’ sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc. 2011;43:2127–33. doi: 10.1249/MSS.0b013e31821b94f7. [DOI] [PubMed] [Google Scholar]
- 13.Clark BK, Thorp AA, Winkler EA, Gardiner PA, Healy GN, Owen N, Dunstan DW. Validity of self-reported measures of workplace sitting time and breaks in sitting time. Med Sci Sports Exerc. 2011;43:1907–12. doi: 10.1249/MSS.0b013e31821820a2. [DOI] [PubMed] [Google Scholar]
- 14.Chau JY, van der Ploeg HP, Dunn S, Kurko J, Bauman AE. A tool for measuring workers’ sitting time by domain: the Workforce Sitting Questionnaire. Br J Sports Med. 2011;45:1216–22. doi: 10.1136/bjsports-2011-090214. [DOI] [PubMed] [Google Scholar]
- 15.Hekler EB, Buman MP, Haskell WL, Conway TL, Cain KL, Sallis JF, Saelens BE, Frank LD, Kerr J, King AC. Reliability and validity of CHAMPS self-reported sedentary-to-vigorous intensity physical activity in older adults. J Phys Act Health. 2012;9:225–36. doi: 10.1123/jpah.9.2.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shuval K, Dipietro L, Skinner CS, Barlow CE, Morrow J, Goldsteen R, Kohl HW., 3rd ‘Sedentary behaviour counselling’: the next step in lifestyle counselling in primary care; pilot findings from the Rapid Assessment Disuse Index (RADI) study. Br J Sports Med. 2012 doi: 10.1136/bjsports-2012-091357. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams R. Revised Physical Activity Readiness Questionnaire. Can Fam Physician. 1999;46:2061–2. [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dipietro L, Caspersen CJ, Ostfeld AM, Nadel ER. A survey for assessing physical activity among older adults. Med Sci Sports Exerc. 1993;25:628–42. [PubMed] [Google Scholar]
- 20.Matthews CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37:S512–22. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- 21.Nichols JF, Morgan CG, Chabot LE, Sallis JF, Calfas KJ. Assessment of physical activity with the Computer Science and Applications, Inc., accelerometer: laboratory versus field validation. Res Q Exerc Sport. 2000;71:36–43. doi: 10.1080/02701367.2000.10608878. [DOI] [PubMed] [Google Scholar]
- 22.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–88. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 23.Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–81. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 24.Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–81. doi: 10.1093/aje/kwm390. 397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pettee Gabriel KK, McClain JJ, High RR, Schmid KK, Whitfield GP, Ainsworth BE. Patterns of accelerometer-derived estimates of physical inactivity in middle-aged women. Med Sci Sports Exerc. 2012;44:104–10. doi: 10.1249/MSS.0b013e318229056e. [DOI] [PubMed] [Google Scholar]
- 26.WHO. Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization; 2000. Obesity: preventing and managing the global epidemic. [PubMed] [Google Scholar]
- 27.Gordis L. Epidemiology. 4. Saunders, Elsevier; Philadelphia, PA: 2009. [Google Scholar]
- 28.Taylor-Piliae RE, Norton LC, Haskell WL, Mahbouda MH, Fair JM, Iribarren C, Hlatky MA, Go AS, Fortmann SP. Validation of a new brief physical activity survey among men and women aged 60–69 years. Am J Epidemiol. 2006;164:598–606. doi: 10.1093/aje/kwj248. [DOI] [PubMed] [Google Scholar]
- 29.van der Ploeg HP, Merom D, Chau JY, Bittman M, Trost SG, Bauman AE. Advances in population surveillance for physical activity and sedentary behavior: reliability and validity of time use surveys. Am J Epidemiol. 2010;172:1199–1206. doi: 10.1093/aje/kwq265. [DOI] [PubMed] [Google Scholar]
- 30.Hébert ET, Caughy MO, Shuval K. Primary care providers’ perceptions of physical activity counselling in a clinical setting: a systematic review. Br J Sports Med. 2012;46:625–31. doi: 10.1136/bjsports-2011-090734. [DOI] [PubMed] [Google Scholar]
- 31.Estabrooks PA, Glasgow RE, Dzewaltowski DA. Physical activity promotion through primary care. JAMA. 2003;289:2913–16. doi: 10.1001/jama.289.22.2913. [DOI] [PubMed] [Google Scholar]