Abstract
Background
Depression during pregnancy has been demonstrated to be predictive of low birthweight, prematurity, and postpartum depression. These adverse outcomes potentially have lasting effects on maternal and child well-being. Socio-economically disadvantaged women are twice as likely as middle-class women to meet diagnostic criteria for antenatal major depression (MDD), but have proven difficult to engage and retain in treatment. Collaborative care treatment models for depression have not been evaluated for racially/ethnically diverse, pregnant women on Medicaid receiving care in a public health system. This paper describes the design, methodology, culturally relevant enhancements, and implementation of a randomized controlled trial of depression care management compared to public health Maternity Support Services(MSS).
Methods
Pregnant, public health patients, ≥18 years with a likely diagnosis of MDD or dysthymia, measured respectively by the Patient Health Questionnaire-9(PHQ-9) or the Mini-International Neuropsychiatric Interview(MINI), were randomized to the intervention or to public health MSS. The primary outcome was reduction in depression severity from baseline during pregnancy to 18-months post-baseline(one-year postpartum).
Baseline Results
168 women with likely MDD (96.4%) and/or dysthymia (24.4%) were randomized. Average age was 27.6 years and gestational age was 22.4 weeks; 58.3% racial/ethnic minority; 71.4% unmarried; 22% no high school degree/GED; 65.3% unemployed; 42.1% making ≤$10,000 annually; 80.4% having recurrent depression; 64.6% PTSD, and 72% an unplanned pregnancy.
Conclusions
A collaborative care team, including a psychiatrist, psychologist, project manager, and 3 social workers, met weekly, collaborated with the patients' obstetrics providers, and monitored depression severity using an electronic tracking system. Potential sustainability of the intervention within a public health system requires further study.
Keywords: perinatal depression, collaborative care model, public health, pregnancy, postpartum, obstetrics and gynecology
Introduction
A report from the Agency for Healthcare Research and Quality concluded that despite the fact that perinatal depression is a significant mental health and public health problem, there is a paucity of high-quality research on the identification and management of perinatal depression in “real world” systems of care.1 Depression during pregnancy has been demonstrated to be the most potent predictor of postpartum depression2 and has been linked to low birthweight and prematurity, especially for socio-economically disadvantaged women in the United States.3 Maternal postpartum depression, in turn, has potential lasting, adverse effects on maternal, infant and child well-being.4,5,6 Prevalence rates show that poor, urban women are at least twice as likely as middle-class women to meet diagnostic criteria for major depression during pregnancy.7,8,9 Critical gaps also exist in screening for perinatal depression in medical and non-medical settings and racially/ethnically diverse depressed women on low incomes have proven difficult to engage and retain in a minimally adequate course of mental health treatment.10,11,12,13
Socio-economically disadvantaged women face numerous barriers to care at the system, provider, and patient levels.14 System barriers (medical and mental health settings) may include: a culturally insensitive and/or stigmatizing environment, lack of minority health care providers and consumers;15 few strategies for maintaining evidence-based practices; lack of electronic technology; failure to align system and financial incentives for quality of care improvements;16,17,18 high staffing ratios and long waiting times.19 Provider barriers may involve the lack of: 1) culturally sensitive or minority health providers; 2) systematic depression screening; 3) time to educate patient about depression; 4) monitoring adherence and outcomes;and 5) exploration of patient's preferences about treatment(i.e., medication or psychotherapy).16,17,18
Potential patient barriers include: 1) practical barriers (e.g.,economic problems; lack of medical insurance, transportation, or childcare; competing priorities and limited time; inaccessible clinic locations);20,21,22 2) cultural barriers (e.g.,clinician insensitivity to cultural values, preferred ways of coping, and beliefs about depression);15,23,24and 3) psychological barriers (e.g.,previous negative experiences with service use;25 stigma of depression26). Another barrier appears to be an avoidant or fearful attachment style, often resulting from exposure to childhood or domestic trauma27,28 and characterized by strong self-reliance and/or distrust of others, potentially making it difficult to engagement in treatment.29
Collaborative care (CC) models for treating depression in primary care have received over a decade of substantial empirical support 30,31,32,33 and hold promise for improving access to evidence-based care for antenatal depression and for maintaining postpartum recovery. In brief, collaborative care is a systematic approach that includes: 1) a negotiated definition of the clinical problem in terms that both the patient and health care provider understand; 2) joint development of a care plan; 3) provision of support for self-management training and affective, cognitive, and behavioral change; and 4) active, sustained follow-up.14 CC models typically involve two stepped care principles:32 1) treatment should always have the best chance of delivering positive outcomes while burdening the patient as little as possible and 2) scheduled reviews, to detect and act on non-improvement, must be in place to enable stepping up to more intensive treatments, stepping down where a less intensive treatment becomes appropriate, and stepping out when an alternative treatment or no treatment become appropriate.
The CC approach has been adapted to patients with chronic medical illness 34,35 and socio-economically disadvantaged populations.10 Studies have shown that CC interventions that activate and educate patients to become active partners and that extend a masters-level social worker or nurse (depression care specialist), supervised by a mental health team, into the primary care setting are highly effective in improving outcomes.14 CC models address patient-level barriers by providing education about depression and by offering patients a choice of evidence-based brief psychotherapy and/or pharmacotherapy, and if the patient does not respond to the initial line of treatment, augmenting care with the alternative treatment.14 These models also address provider-level barriers by using a collaborative approach to integrate mental health specialty knowledge into primary care, closely monitoring patient symptoms and adherence14, and using the telephone as well as in-person visits.
Pregnancy is known to be an opportune time for suggesting health interventions36 because pregnant women may be unusually open to making changes to improve their mental health and health risk behaviors, such as smoking and/or substance use, before their baby is born.37 This paper reports on the design and methods of a National Institute of Mental Health-funded randomized controlled trial, MOMCare, which provided a multi-component, collaborative care model for engaging and retaining depressed, pregnant women in treatment to ameliorate antenatal depression and reduce the risk of postpartum depression. The MOMCare study built upon a previous randomized pilot study of a pre-treatment engagement session and brief interpersonal psychotherapy, enhanced to be culturally relevant to a diverse population of low-income women during the perinatal period.12,38 By “culturally relevant”, we mean an intervention adapted to be relevant both to the culture of poverty and the culture of race/ethnicity. This paper also describes the process whereby the MOMCare study was implemented in a unique, progressive service environment -- the 10 public health centers of Public Health Seattle-King County (PHSKC) of Western Washington.
Methods
Study design and objectives
The aims of the MOMCare study were to evaluate the impact of collaborative care treatment compared to usual MSS public health care on engagement and retention in depression treatment at 3-and 6-months post-baseline and on antenatal and postpartum depression severity and functional outcomes at critical time points from baseline (pregnancy) to 18-months post-baseline (one-year postpartum). We also planned to conduct an incremental cost-effectiveness and net benefit analysis from a health care and welfare agency perspective that included the following components during the first postpartum year: tracking the medical costs of maternal health service use (including the costs of administering the MOMCare study); examining the rates and costs of adverse birth outcomes; and monitoring the use and costs of infant preventative health services (well-child visits, required immunizations). The intervention began at 12-32 weeks gestation and treatment maintenance continued up to one-year postpartum. The local institutional review board approved the study; participants gave written informed consent and signed HIPAA release forms.
Setting and population
The MOMCare study was developed in partnership with the administrative leadership and clinical staff of Maternity Support Services (MSS) of Public Health Seattle and King County (PHSKC) of the First Steps Program, which operates in each of its 35 counties of Washington State. MSS routinely provides enhanced prenatal and postpartum services to a diverse population of pregnant women on Medicaid. Goals of MSS include identifying the dietary, health, mental health, and psychosocial needs of the expectant mother and offering a range of services to promote healthy pregnancies and positive birth and parenting outcomes. MSS is delivered by a multi-disciplinary team of public health social workers, nurses, and nutritionists, who routinely screen, at least once, for perinatal depression from pregnancy up to at least 2-months postpartum.
In January 2006, the MSS program at PHSKC installed a HIPAA compliant, electronic charting system to keep track of patient services, including the results of routine perinatal depression screening via the Patient Health Questionnaire (PHQ-9).39,40 Typically, once a pregnant woman screens positive for depression (≥10 on the PHQ-9), her MSS social worker or nurse refers her for mental health treatment in the community. Despite improvements in perinatal depression screening, the leadership of PHSKC recognized that only a minority of depressed, pregnant women actually received evidence-based psychotherapy or pharmacotherapy in community mental health centers. This finding mirrors the results of two decades of mental health services research, showing that depression screening alone and referral to care are inadequate to improve patient outcomes.36 Thus, they were very supportive of examining the effectiveness of MOMCare with their pregnant public health patients who screened positive for depression.
Recruitment
Recruitment for the MOMCare study took place in all ten public health centers in Seattle-King County between January 2010 and July 2012 and was conducted by 3 MOMCare depression care specialists (masters level social workers who were former MSS providers). Each depression care specialist (DCS) was responsible for recruitment in 3 or 4 public health centers and travelled to their respective centers. MSS social workers and public health nurses were the study's primary referral sources who routinely screened pregnant patients for depression on the PHQ-9 and referred patients scoring ≥ 10 to the MOMCare study. Because a 33% reduction in staff due to stage budget cuts occurred in 2011 (about a year after the study began) and jeopardized referrals, the research study employed a MSS social worker who made calls from the PHSKC central office to potentially eligible, depressed public health patients in order to provide information and refer them to the MOMCare program.
An additional source of recruitment involved the placement of human subjects-approved MOMCare flyers in the waiting areas of the 10 public health centers. The flyer did not use the word, ‘depression’, but described it in non-stigmatizing terms (i.e., stressed, hassled, no energy, etc.) and gave women referral information to contact the depression care specialist in their public health center for further evaluation. We had considered sending letters to all public health patients who scored ≥10 on the PHQ-9 informing them about the MOMCare program. The MSS leadership and staff advised us against this approach, however, because of their previous lack of success (e.g., low response rate) using this method to engage public health patients in other programs. Alternatively, we expected that a more personalized approach to recruiting depressed, pregnant women via their MSS social worker or nurse would be more effective than sending out letters.
Inclusion/exclusion criteria
After receiving referrals from MSS social workers and nurses, as well as self-referrals, MOMCare depression care specialists conducted initial and secondary screenings to assess for the following inclusion criteria: ≥18 years, a likely diagnosis of major depression on the PHQ-9, a likely diagnosis of dysthymia based on the MINI-International Neuropsychiatric Interview (MINI 5.0.0)41, 12-32 weeks gestation, access to a telephone and English speaking. Although dysthymia was traditionally considered less severe than major depression, we decided to include dysthymia for study eligibility because the consequences of dysthymia are recognized as grave; they include persistent symptoms and a protracted course; chronic social and occupational functional impairment; increased morbidity from physical disease, increased risk of suicide; and poor long-term outcomes.42,43,44 The time frame of 12-32 weeks gestation was chosen for several reasons: first, the neurovegetative symptoms of depression may be confounded with the somatic symptoms of pregnancy,45 particularly during the first 12 weeks of pregnancy, resulting in an unacceptable high rate of false positives; second, a cut-off of 32 weeks gestation would still allow time for the acute treatment of depression to be conducted before the birth. With respect to the English speaking criterion, estimates based on PHSKC data showed a low percentage (6%) of Spanish-speaking only women, so it was decided we could augment the intervention with linguistic adaptations in the future, once it showed promising results and was designated cost-effective. Exclusion criteria consisted of acute suicidal behavior or multiple (≥2) prior suicide attempts, lifetime history of schizophrenia or bipolar disorder I and II, substance abuse/dependence within the previous three months, current severe intimate partner violence, or currently in psychotherapy or seeing a psychiatrist. If the patient did not meet study criteria, but presented with significant psychiatric symptomatology, she was referred for appropriate mental health care in the community or with her OB provider.
Randomization
All eligible public health patients who consented were scheduled for initial and secondary screenings. Women received $10 for completing the secondary screen. If they were found to be eligible for the study, the research was explained and consent elicited, followed by randomization and a baseline interview. Our data manager ensured that the study interviewer and coders remained blind to group assignment. Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL-20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks).46,47 Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerized program by the depression care specialist (DCS) responsible for screening in 3-4 public health centers. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment. See Table 1 showing the differences between services provided by MSS public health care and the MOMCare intervention. The MOMCare intervention added a pretreatment engagement session and depression care onto routine MSS.
Table 1. Comparison of Maternal Support Services (MSS) and MOMCare Collaborative Care Intervention.
| MSS | MOMCare |
|---|---|
|
| |
| 1) MSS social worker screens for depression severity (PHQ-9 ≥ 10) | 1) MSS social worker screens for depression severity (PHQ-9 ≥ 10) |
| 2) MSS social worker refers to MOMCare depression care specialist (DCS) for study screening, consenting, and randomization | 2) MSS social worker refers to MOMCare depression care specialist (DCS) for study screening, consenting, and randomization |
| 3) NO pre-treatment engagement session | 3) pre-treatment engagement session delivered by MOMCare DCS |
| 4) MOMCare DCS delivers psychoeducation about depression and depression self-help book, notifies MSS social worker, and makes a referral for depression care in the community and/or from OB provider | 4) MOMCare DCS delivers psychoeducation about depression and depression self-help book, notifies MSS social worker, coordinates care with OB provider, and provides acute brief interpersonal psychotherapy and/or pharmacotherapy, with maintenance treatment to 1-year postpartum |
| 5) MSS social worker, or nurse still provide usual support services, but do not provide depression care and refer to community mental health or OB provider | 5) MSS social worker, nurse, nutritionist still provides usual support services |
| 6) NO weekly/bimonthly/monthly assessments on PHQ-9 depression severity from baseline to 1-year postpartum by MSS social worker | 6) Weekly/bimonthly/monthly assessments on PHQ-9 depression severity from baseline to 1 year postpartum by DCS using Excel tracking form |
| 7) NO weekly group and individual supervision for depression care management | 7) Weekly group and individual supervision for the DCSs in brief IPT and/or medication management by team PI and psychiatrist |
Emboldened text represents how the MOMCare intervention differs from MSS Public Health Services.
If the patient was assigned to MSS services alone and treatment referral, the DCS said, “You have been assigned to usual care in public health and a referral for treatment in the community. What this means is that I would like to spend some time with you now to talk more about how you are feeling, to give you some information about the nature of depression and effective treatments for depression, and how you can receive treatment for your depression in the community, if you wish. I will also give you some educational materials on depression and treatment options. With your permission, I can also inform your MSS social worker and OB provider about your depression so they can help you get the treatment you want.” If the patient was assigned to the MOMCare intervention, the DCS said, “You have been assigned to the MOMCare treatment. What this means is that I would like to schedule a time when I can get to know you better, find out more about how you are feeling and what is stressful in your life, how you see treatment for depression, and what would make it hard for you to participate in treatment (pre-treatment engagement session). I will also provide you with you some educational materials on depression and treatment options. If you choose to pursue treatment, our MOMCare program can provide that for you in the public health center and by phone.”
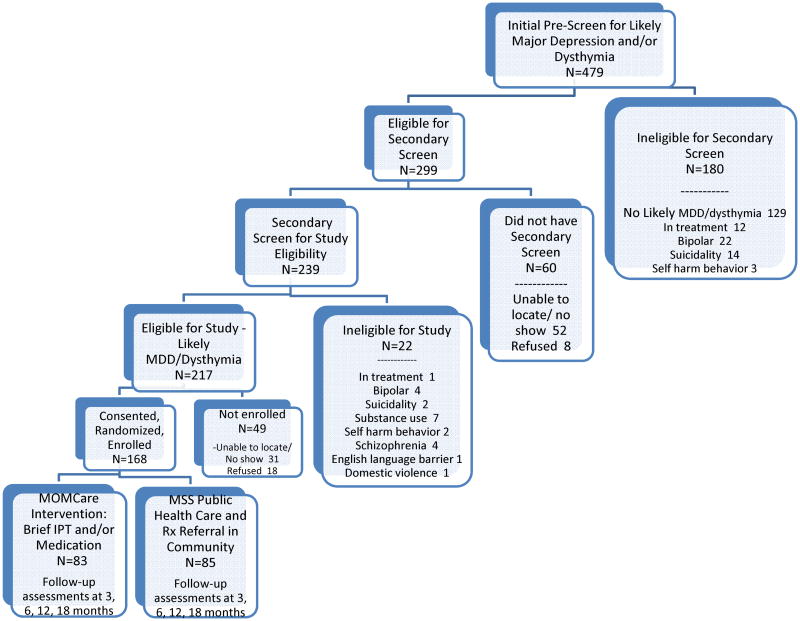
Figure 1 shows that of the 479 non-treatment seeking, public health patients who scored ≥ 10 on the PHQ-9 and were referred by MSS social workers or nurses to MOMCare depression care specialists for the initial pre-screening, 62.5% (n=299) met diagnostic criteria for likely MDD or dysthymia. This rate of likely MDD in this population is higher than we originally estimated (50-55%) based on the PHQ-9,48 possibly due to the considerable socio-economic disadvantage these women experienced. 49,50 Screening for study enrollment took place in a two-step process to minimize participant burden. The purpose of the secondary screening was to rule out exclusion criteria, such as already being in treatment or having bipolar disorder. Of the 299 initially eligible patients, 239 (75%) received the secondary screening, of which 91% or 217 were deemed eligible for the study. Sixty initially eligible patients (25%) did not have the secondary screening because they did not show or refused. Of the 217 ultimately eligible patients, 77% or 168 were consented and enrolled; 49 (23%) did not show or refused. In sum, 83 MSS patients were randomized to the study intervention and 85 to the public health care they were already receiving. Our study's rate of enrollment of non-treatment seeking pregnant women with likely MDD or dysthymia in the study (77%) exceeds that (17%) observed in low income, depressed women seeking mental health treatment in the community10 and is similar to rates of enrolling socio-economically disadvantaged, depressed, pregnant women in previous randomized controlled trials.38,51
Figure 1. Screening and randomization process for participation in the MOMCare Study.
Management of potential patient-self harm in the MOMCare study
A self-harm assessment protocol was developed for determining what clinical deterioration is or what an emergency is -- defined as emergent suicidal ideation or plan, development of serious substance abuse, emergence of a new psychiatric or medical diagnosis, or behavior posing significant risk to self or others. Evidence has shown that collaborative care models which followed this protocol decrease suicidal ideation in both intervention and usual care patients. 14,32
With respect to suicidality, study clinical and research staff were trained on a conservative procedure to follow when a patient in the intervention or MSS public health care group responded at least “1” (several days) to the question in the PHQ-9, “Over the last 2 weeks, how often have you been bothered by any of the following problems? Thoughts that you would be better off dead or thoughts of hurting yourself in some way.” OR responded at least “2” (a little bit) to the question in the SCL, “Overall, in the past 2 weeks, how much were you distressed by thoughts that you would be better off dead or thoughts of ending your life?” Study staff was instructed to report suicidal risk immediately to the principal investigator and study psychiatrist and to the patient's clinically trained depression care specialist, who originally screened and consented the patient into the study.
The depression care specialist (DCS) evaluated the suicidal patient usually within several hours of the notification and always within 24 hours. Suicidal assessments included questions about the patient's access to weapons, current alcohol or drug use, the patient's immediate plans to harm herself, and a history of the patient's suicide attempts. Patients were assessed at “low”, “moderate”, or “high” risk, with associated protocols for each level. Regardless of risk, each assessment was discussed with the principal investigator. In the event of an elective or spontaneous abortion or fetal death, patients were encouraged to remain in the study and to receive extra emotional support from their depression care specialist study or the patient's MSS social worker or nurse.
Study Interventions (see Table 1)
Usual Care: Maternity Support Services (MSS) Public Health Care
From pregnancy up to at least 2 months postpartum, the MSS public health social worker or nurse routinely screened women for depression using the Patient Health Questionnaire-9 (PHQ-9). When a pregnant woman scored ≥10 on the PHQ-9, she was placed in the highest risk category making her eligible for increased, more frequently delivered MSS services from her multi-disciplinary team, and eligible for the MOMCare study. For example, relative to those at lower risk, a high-risk pregnant woman could receive more visits with MSS social workers and/or nurses at the public health center and/or home (up to 10-15 prenatal visits ranging from 30-45 minutes). MSS providers do not provide intensive depression care, but typically refer the patient to community mental health or her OB provider.
Beginning in April 2009, the principal investigator and project manager worked with MSS administrators and staff to enable the 10 public health centers to make referrals to the MOMCare study. They also sent out a newsletter every 3 months to MSS and OB providers to review referral procedures for the study and share brief articles on maternal and child health. Once a MOMCare depression care specialist (DCS) screened, enrolled, and randomized a high risk, depressed MSS public health patient to the usual care MSS group, the DCS spent about 30 minutes giving the patient psychoeducation about perinatal depression along with a gift of The Depression HelpBook,52 which is a patient educational book written in 7th grade language. The DCS also provided the MSS patient enhanced linkages to community mental health treatment and, with the patient's permission, notified her MSS social worker and OB provider of her antenatal depression. The DCS did not conduct an engagement session with the patient, as described below in the MOMCare intervention.
The MOMCare Collaborative Care intervention
The MOMCare intervention included key elements of collaborative care (CC) interventions (brief interpersonal psychotherapy and/or medication) and stepped care principles that have been shown to improve quality and outcomes of depression treatment in primary care30,31,32, and extended the CC model to include the management of perinatal depression in socio-economically disadvantaged women. A number of novel design components aimed at dealing with provider-level and patient-level barriers to care may be seen in Table 2 and included: a pretreatment engagement session; culturally relevant enhancements to brief IPT and/or pharmacotherapy; and ongoing treatment maintenance up to one-year postpartum.
Table 2. Key Elements and Culturally Relevant Enhancements of the MOMCare Collaborative Care Model.
Recruitment Enhancements
|
Public Health System and Provider Level Enhancements
|
Patient Level Enhancements
|
Using stepped care principles, the intervention employed the following approaches. If patients had an inadequate response to their first-line treatment (less than 50% improvement in depressive symptoms after 8 treatment sessions), the medically supervised DCS assisted them (and their OB provider) in specific ways: for patients initially receiving brief IPT – increasing the number of IPT sessions or augmenting with or switching to an antidepressant medication; for patients initially taking an anti-depressant medication -- increasing the dose, switching to a different medication, and/or augmenting with brief IPT. Every 1-2 weeks of the acute treatment phase, the DCS monitored intervention patients' depressive symptoms on the PHQ-9, choice of treatment, dates of treatment sessions, and treatment adherence and recorded this information into an electronic tracking system. We describe the following components of the MOMcare intervention” the engagement session; culturally relevant brief IPT, pharmacotherapy; maintenance treatment and relapse prevention; and intervention team roles, training, and supervision.
Pre-treatment engagement session
If a depressed, pregnant public health patient was randomized to the MOMCare intervention, the study depression care specialist (DCS) provided educational depression materials (The Depression HelpBook52) and conducted a previously tested, pre-treatment engagement session12,53,129 either on the phone or in the public health center where she received MSS services. The engagement session, based on ethnographic and motivational interviewing, is designed a) to address the depressed patient's ambivalence about, and ultimately, commitment to treatment and b) to identify and attempt to resolve her unique practical, psychological and cultural barriers to care, including finances, transportation, scheduling problems, childcare, previous negative experiences with treatment, the stigma of depression, or fear of being misunderstood by a therapist of a different background. In the spirit of Ethnographic Interviewing,54 the DCS tried to understand the woman's cultural perspectives and values without bias, inquired about her view of depression, health-related beliefs, and cultural coping practices (i.e., the importance of spirituality) and asked what she would like in a therapist, including the perceived importance of race/ethnicity. Core features of Motivational Interviewing (MI)55 were used to problem solve the barriers and to enhance intrinsic motivation for change in a non-confrontational manner. In addition, psychoeducation about depression and its treatment was provided by the DCS to address stigma and empower patients to make an informed choice about the type of treatment they prefer – psychotherapy or medication or both. Most pregnant participants were initially reticent about taking anti-depressant medication for fear of harmful effects on the fetus.
Culturally Relevant Brief Interpersonal Psychotherapy (Brief IPT)
Inasmuch as perinatal depression appears to be strongly related to lack of social support, particularly from the spouse or partner,2 an interpersonal approach to the treatment of antenatal depression seemed highly relevant. Interpersonal Psychotherapy (IPT; 16 sessions) has demonstrated efficacy in treating acute depression,56,57,58 preventing depressive relapse through maintenance,59,60 treating antenatal and postpartum depression,38,45,61 and treating depression in primary care.62 A brief version of IPT has been developed 63 and has received empirical support in a number of studies of pregnant and parenting women with depression.38,63,64 Brief IPT consists of 8 individual sessions provided over 8 or more weeks. It retains the core features of standard IPT,65 such as strengthening social supports, building on patient strengths and coping strategies, and resolving interpersonal problems. At the same time, brief IPT offers several advantages over standard IPT. First, it reduces the treatment burden for overwhelmed, pregnant or parenting women with multiple acute and chronic stressors. Second, to promote a quicker treatment response, brief IPT techniques have been expanded to include behavioral activation strategies66,67 that can be shared with family members/friends and assigned as weekly homework68 with an interpersonal focus.
Brief IPT has also been enhanced to be culturally relevant to economically disadvantaged, racially/ethnically diverse women with depression.65,69 Pragmatic enhancements to brief IPT relevant to the culture of poverty70 included integrating a case management component into brief IPT and using the telephone to conduct acute brief IPT, a practice found to be effective in the delivery of psychotherapy and pharmacotherapy for depression.71 The DCS also engaged in intensive outreach to retain their patients in treatment, with telephone calls, texting, email, showing up at the patient's non-stigmatizing public health setting, meeting in coffee shops, or at the patient's home. Further, as previously described,72 brief IPT was enhanced to be relevant to the culture of race/ethnicity. For example, each DCS provided psychoeducation about depression congruent with the patient's cultural preferences and incorporated the patient's goals, cultural resources and strengths into treatment.
Pharmacotherapy
Although several studies of perinatal patients' preferences for mental health treatment concur that they prefer psychotherapy over pharmacotherapy, largely due to concerns about effects on their fetus/infant,73,74,75 there is strong, recent evidence that antidepressant medication use during pregnancy is increasing, that Selective Serotonin Reuptake Inhibitors (SSRIs) are the most common antidepressants prescribed during pregnancy,76,77 and some depressed, pregnant women may appreciate having the option to use anti-depressant medication as their first line of treatment. Is it safe to offer the choice of anti-depressant medication for antenatal depression?
In April 2008 the American College of Obstetricians and Gynecologists (ACOG) Committee on Obstetric Practice published an updated practice bulletin78 on this topic, recommending that treatment with SSRIs or selective norepinephrine reuptake inhibitors (SNRIs) or both during pregnancy be individualized, incorporating the patient's values and perceptions when discussing the risks and benefits of treatment with the OB provider. The committee also pointed out that multiple studies have not identified an increased risk for major congenital malformations associated with the use of SSRIs, SNRIs, or tricyclics during pregnancy, but advised against paroxetine use among pregnant women due to some research showing that first-trimester exposure to paroxetine is associated with a greater risk of fetal cardiac defects. With respect to the risks of taking anti-depressant medication during lactation, recent available data on the tricyclic antidepressants (e.g., nortriptyline)79 or on the SSRIs (e.g., paroxetine, sertraline)80,81 have been encouraging and suggest that the amount of drug to which the nursing infant is exposed is low and that complications related to neonatal exposure to these drugs in breast milk are rare.
At end of the engagement session, the DCS gives women the choice of initiating or continuing an anti-depressant medication during pregnancy via a risk-benefit decision making process82 in which their obstetrics (OB) or primary care (PCP) provider, and treatment team (DCS, psychiatrist) are involved. Given the ACOG guidelines and that MSS public health patients have this choice, we did not think it justifiable to take this decision away from patients in the intervention. Furthermore, risks of untreated maternal depression during pregnancy pose a serious concern and include poor compliance with prenatal care, inadequate nutrition, increased alcohol and tobacco use, potential deficits in mother-infant bonding after childbirth,83 increased risks of preterm birth and low birthweight,3 and depressive relapse from discontinuing anti-depressant medication during pregnancy.84
Most patients in the intervention (80%) chose brief IPT as their initial line of treatment based on concerns about taking anti-depressant medication when pregnant. For the 15% of intervention patients who chose brief IPT and medication or the 5% who chose medication alone, the DCS collaborated with the patient, her OB provider, and the study psychiatrist to initiate effective, guideline-based treatment. The OB providers wrote prescriptions, based on the psychiatrist's recommendation. Because most patients' OB providers were not located in a public health center, the DCS often contacted them by phone to coordinate care. The DCS met with the patient at the public health center or on the phone to monitor and track medication response, adherence and side effects. The DCS also provided emotional support and ongoing psychoeducation about medication management.
Maintenance Treatment and Relapse Prevention
Given robust evidence that major depression is a chronic or relapsing condition in which recurrence is expected,85 once a patient showed a treatment response, the DCS provided biweekly or monthly maintenance IPT and/or pharmacotherapy sessions, along with PHQ-9 depression monitoring, up to 18 months after study entry. Because the goal was to maintain recovery, the patient was encouraged to monitor early somatic, affective, and cognitive symptoms related to prior depressive episodes and to employ skills learned in Brief IPT and/or related to medication management. When entering the maintenance phase, patients completed a relapse prevention plan related to their interpersonal goals (such as effectively managing a dispute with a significant person or the transition of becoming a mother), and/or medication adherence and were monitored biweekly or monthly on the PHQ-9 for depressive relapse. If the patient showed depressive relapse, her DCS consulted with the supervisory team and offered her more intense, follow-up treatment, according to the stepped care algorithm described previously. For patients who either ended the study without a full remission, or who felt they would benefit from additional therapy or continued medication, DCSs assisted with referrals to therapists and clinics in the community who would serve patients on Medicaid.
MOMCare intervention team roles, training, and supervision
The MOMCare depression care specialists (DCSs; masters-level social workers) received an initial intensive two-week training and regular monthly advanced trainings on pertinent topics throughout the study period. Trainings included: 1) self-study of the 4 study manuals -- engagement manual, brief IPT manual, pharmacotherapy manual, and depression care by phone manual; 2) didactic orientation to perinatal medical complications by the team Ob/Gyn research physician; 3) training in the engagement session and motivational interviewing skills, e.g. reflective listening, affirming strengths, identifying and addressing treatment ambivalence, and problem solving barriers to care; 4) training in brief IPT, included readings, watching videos of skilled IPT therapists, role playing, and working with at least 2-3 training cases, which were audiotaped and evaluated to meet treatment fidelity; 5) training in cultural competence and implementing brief IPT culturally relevant enhancements for socio-economically disadvantaged patients; and 6) training in diagnosis and pharmacotherapy for depression and anxiety by the team psychiatrist. The DCSs received weekly group supervision from the team psychiatrist and weekly individual supervision from the PI, who reviewed a majority of the audiotaped engagement and brief IPT sessions, providing an opportunity for feedback and minimizing treatment drift.
Data collection and measures
A study interviewer blind to treatment condition conducted the data collection in-person or by phone at baseline, 3-, 6-, 12-, and 18-months post-baseline, a period extending from pregnancy to one-year postpartum. The final 18-month assessment occurred at about one-year postpartum. Participants in usual care and in the intervention received assessments on all of the measures described below and received a $30 gift card or money order for completing each research interview.
Screening
To be enrolled in the study, public health patients were required to show symptoms consistent with the DSM-IV diagnoses of major depression (MDD) on the PHQ-9 or dysthymia on the MINI. Before making likely diagnoses of MDD or dysthymia, the depression care specialist ruled out physical causes of depression, normal bereavement, and a history of a manic episode. The PHQ-9 is a valid and reliable nine item depression questionnaire that has been found to have high sensitivity and specificity, respectively, to the diagnosis of MDD made by structured psychiatric interview in 3000 primary care patients (99%; 91%) and in 3000 Ob/Gyn patients (75%; 88%).39,40 The PHQ-9 is a dual purpose instrument that can be used to provide a provisional diagnosis of MDD and to grade depressive symptom severity via a continuous score. Likely MDD is diagnosed if five or more of the nine depressive symptom criteria have been present “more than half the days” in the past 2 weeks, and one of the symptoms is depressed mood or anhedonia. Sample items include “little interest or pleasure in doing things, “feeling down, depressed, or helpless,” trouble falling asleep or staying asleep or sleeping too much”, and “feeling tired or having little energy.” Per Kroenke and Spitzer's recommendation (2002) 48, we added to the end of the PHQ-9 a global item measuring functional impairment, asking patients who checked off any problems, “How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?” This impairment rating has been shown to correlate strongly with a number of measures on quality of life, functional stability, and health care usage.48 The PHQ-9 has also been found useful in screening for suicidal ideation.86 We had considered using a structured clinical interview, which can take 15-30 minutes of clinical time, to determine MDD. However, the brevity and simplicity of administration of the PHQ-9 (plus impairment), coupled with its construct and criterion validity, made it more feasible and acceptable for assessing likely MDD, particularly in the busy setting of public health centers. Data also show that telephone administration of the PHQ-9 is a reliable procedure for assessing depression.87
The M.I.N.I. 5.0.0 Dysthymia Module41 is a reliable, valid method for lay interviewers to diagnose symptoms consistent with a DSM-IV diagnosis of dysthymia. We chose this instrument because of its excellent construct validity and the feasibility of its administration in a busy public health setting. Validation and reliability studies have been done comparing the M.I.N.I. to the patient version of the Structured Clinical Interview for DSM-IV (SCID) disorders.88 Results of these studies showed that the M.I.N.I. has acceptably high validation and reliability scores, but can be administered in a much shorter period of time than the SCID.41 To meet criteria for likely dysthymia, patients must endorse feeling “sad, low, or depressed over the last 2 years”; not having “a period interrupted by your feeling OK for two months or more”; replying “yes” to having at least 2 problems in areas such as appetite, sleep, fatigue, hopelessness, and self-confidence; and endorsing functional impairment. The MINI also measures lifetime course of depression.
Baseline and follow-up assessments
Demographic data were collected at baseline (age, marital status, race/ethnicity, education, employment status, income level). Assessments included the following measures.
Primary Outcome - Depression severity
The primary outcome, reduction in depression severity, at 3-, 6-, 12-, and 18-month post-baseline time points was assessed by the 20-item SCL-20 depression scale,89 a reliable and valid measure of distress shown to be sensitive to change in large primary care effectiveness studies [Cronbach alpha (α)=0.91].90,91 The SCL-20 was also used to assess treatment response (≥ 50% reduction from baseline) and complete remission of depressive symptoms (SCL-20 score of <0.5).92 The items on the SCL-20 show considerable overlap and excellent convergent validity (r=.90) with the items on the PHQ-9.93
Secondary Outcomes included anxiety comorbidity; personality traits; childhood adversity; functioning assessments, including patient satisfaction with depression care; pregnancy, delivery, and birth outcomes; maternal health service use and estimated costs; quality of depression care process.
Anxiety Comorbidity
The anxiety modules of the PHQ39 were used for assessing panic and generalized anxiety symptoms. The Post-Traumatic Stress Disorder Checklist-Civilian Version (PCL-C) is a 17-item questionnaire that assesses the intrusive, avoidant, and arousal PTSD symptom clusters. Data show a .93 correlation between the total scores on the PCL-C and the clinician-administered PTSD scale.94 PTSD may also delay or diminish, and thus moderate, treatment response for those with MDD. 95,96,97
Personality Traits and Childhood Adversity
The Relationship Quality Questionnaire (RQ)98 assessed the 4 personality attachment styles [i.e., secure, preoccupied (anxious), dismissive (avoidant), or fearful (anxious and avoidant)] categorically and continuously and demonstrates convergent and discriminant validity with other self-report and interview ratings.99 Collaborative care has been shown to be particularly beneficial to patients with avoidant or fearful attachment who often have problems trusting physicians.100 To assess for history of childhood maltreatment, we used the 25-item Childhood Trauma Questionnaire;101 the items have high item-total correlations with each of their respective subscales (physical, emotional, and sexual abuse; physical and emotional neglect).102 Prior childhood adversity has been found to be associated with insecure attachment styles in adults29 and with increased risk for adult depression and PTSD.103,104,105 Childhood trauma has also been observed to delay response to interpersonal psychotherapy for perinatal depression.106
Functioning Assessments
Secondary outcomes included social functioning from the Social and Leisure domain of the Social Adjustment Scale (SAS), which has shown good reliability and validity.107 Perceived stress over the last month was measured by the reliable and valid Perceived Stress Scale.108 For perceived chronic stress over the past 6 months, we used two subscales (i.e., financial and ecological stressors) from the chronic stress scale developed by Norris & Uhl, 1993.109 Exposure to acute and chronic stressors has been found to predict depression severity in socio-economically disadvantaged women.110,111 Postpartum maternal role functioning was assessed by 1) The Inventory of Functional Status after Childbirth (IFSAC)112 consisting of 5 subscales (infant care, household, social/community, occupational, and self-care activities) assessing readiness to assume infant care and resume usual activities; and 2) the 9-item New Baby subscale of the Postpartum Adjustment Questionnaire, measuring how well the mother interacts with the infant in 3 domains (play activity, physical contact, and infant care). It has shown good reliability in studies of postpartum women.113 Patient Satisfaction with Depression Care was assessed via a brief question at 4 follow-ups. Katon and colleagues have found significant intervention versus control differences in many collaborative care studies.31,92,114
Data on Pregnancy, Delivery and Birth Outcomes were obtained from hospital records and recorded systematically with the reliable and valid Peripartum Events Scale (PES).115 The PES quantifies stressful events in the following categories: medical and obstetric risk factors, admission to labor and delivery, labor progress, labor duration, fetal monitoring, delivery method and complications, and infant outcomes (i.e., birthweight, gestational age, APGAR scores, and special care/NICU stay). A coder was trained by the study's OB/Gyn research physician. Reliability was established and the coding was overseen by an OB/Gyn physician.
With respect to Child Services and Outcomes. Data on the completeness of the AAP recommended immunization and well-child visit schedules were obtained from mothers' reports of their infants' receipt of well-child care, emergency room and illness care. Mothers also completed the 42-item Brief Infant-Toddler Social and Emotional Assessment (BITSEA), shown to have good reliability in assessing child socio-emotional problems, strengths, and competencies.116
Maternal Health Services
Data on the previous 3- to 6-month use of outpatient medical visits, inpatient hospital services, emergency room visits, counseling, psychotherapy, treatment for alcohol or substance abuse, utilization of medication (name, type, duration), and time costs in accessing and receiving health care were collected via the Cornell Service Index (CSI)117 at baseline and at 3, 6, 12, and 18 months post-baseline. The CSI is a reliable method to assess adult health service use and was successfully used in the cost-effectiveness analysis from IMPACT.118 Although we knew it ideal to use Medicaid claims data, we found this problematic because a substantial minority of study participants go off Medicaid after the first two months postpartum due to their coverage running out and because of limitations in the comprehensiveness of such data. Thus, we decided to rely instead on the CSI self-report measure. We have examined the CSI questions in IMPACT where we also had automated data from many of the 8 sites. In this elderly sample, we found that the estimated rates of utilization based on self-report and our automated data were quite close except for emergency room and mental health use where self-report use tended to be higher.119 In addition, earlier research found high rates of agreement between self-reported antidepressant use and prescription fill data from a pharmacy database.120
Quality Adjusted Life Years
We used the EuroQol121as a measure of study effectiveness in order to capture domains of health and mental health. The EuroQol provides a more general measure of health-related quality of life than depression-free days and includes 5 dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression.
With respect to the Quality of Depression Care Process, adherence to antidepressants and mental health care utilization were assessed31,92,114 by the Cornell Services Index measuring (1) adequate dose and duration of antidepressants defined as the percent of subjects reaching adequate dosage (by AHCPR/newer medication guidelines) and duration (≥90 days) of antidepressants in each 3-or 6-month period, (2) antidepressant medication use and adherence defined as the percent of subjects on any antidepressant and the percent taking antidepressants for ≥25 of the last 30 days assessed at baseline and follow-ups, and (3) psychotherapy use defined as the number of psychotherapy visits in each 3-, 6-, 12-, and 18 -month post-baseline follow-up period and the percent with at least 4 sessions (by a mental health or social work professional) during each follow-up period.
Analyses
We plan bivariate analyses to compare baseline demographic and clinical characteristics of the intervention group and MSS public health care group. In intention-to-treat analyses, we will use generalized estimating equations (GEE) with the appropriate links for the distributions of the dependent variables using baseline, 3-, 6-, 12-, and 18-month follow-up data. Design covariates and potential moderators of treatment effects will include exposure to childhood trauma and likely PTSD co-morbidity with likely MDD. In the mixed-effects models, we will treat time as a categorical variable and examine the fixed effects for time, intervention condition, and their interactions. We will specify the covariance structure within patients using an unstructured model with robust error estimation to account for the within-patient correlation over time. 122 A statistically significant treatment group-by-time interaction will indicate differences in trends over time for the two groups. In the event of a non-significant interaction, the term will be removed and the model re-fit; the main effects of time and treatment group will then be examined. Lastly, using planned post-hoc analyses generated from the GEE analyses, we will assess differences in outcomes by treatment group at each of the follow-ups.
To examine to what extent intervention participants show higher levels of treatment engagement and retention than public health patients receiving MSS services, the primary dependent measures in the analyses are: 1) whether a participant attends an initial treatment session (engagement) and 2) number of depression visits attended at 3- and 6-months post-baseline (retention). We will use logistic regression models to determine whether the intervention patients are more likely to attend an initial session, and Poisson regression models to determine whether the intervention patients attend significantly more treatment sessions over time.
Power
With a sample of women on Medicaid from the public health system, we chose, conservatively, to assume that we would detect a medium effect size of .45 on our primary outcome variables --number of treatment sessions attended, depressive symptoms (SCL-20) and functioning capacity (SAS). Thus, with a moderate effect size of .45, we estimated that we would need a sample of at least 156 to have 80% power to detect a group difference on outcomes. With a sample size of 156, we also estimated that we would have sufficient power to detect effect sizes as small as .26.
We expected that MSS social workers and nurses initially would need to screen an estimated 1530 pregnant public health patients on the PHQ-9. Based on previous studies reporting higher rates of depression in socio-economically disadvantaged women, we expected that 25-30% of those screened (about 459) would receive a PHQ-9 score of ≥10 8,9 indicating likely major depression or subsyndromal depression. Of those who scored ≥ 10 and were referred to MOMCare for further evaluation, we expected that approximately 50-55% (about 229) would show symptoms consistent with a DSM-IV diagnosis of major depression (MDD) and or dysthymia.48 With an expected overall study attrition rate of 20-25%, we planned to end up with an estimated sample size of 229 × .25 or 171 women. Because we found that our overall study attrition rate was much lower − 7%, we decided to stop recruitment with a final sample of 168 depressed, pregnant public health patients, a size which gave us sufficient power to detect group differences on outcomes. See Figure 1 for patient flow chart.
Preliminary Baseline Results
Although all phases of data collection have been completed, for the purpose of this design paper, we present only baseline results. Each of the 10 public health centers referred an average of 10% of women who were enrolled in the MOMCare study (range: 2-18%, depending on size of the population served at each center). One hundred sixty-eight women entered the study and were randomized to the MOMCare intervention (n=83) or to MSS public health care services (n=85). As shown in Tables 3 and 4, the intervention and MSS services groups were well balanced on socio-demographic and clinical variables, except that intervention participants were more likely to be unemployed than MSS participants. On average, the sample was 27.4 years old and at 22.4 weeks gestation, with 41.7% white, 23.2% African American, 22.6% Latina, 7.1%, Asian/Pacific Islander, and 5.4% Native American/Alaskan. Three-quarters were not married; one-fifth had not finished high school; two-thirds were unemployed, over two-fifths were living on $10,000 or less; 13.4% were homeless, over half had experienced a previous postpartum depression; close to three-quarters had an unplanned pregnancy, but two-thirds felt mostly positive about their pregnancy.
Table 3. Baseline Demographic Variables of Study Participants.
| Variable | Total Sample | MSS Public Health Care | MOMCARE | Statistical p Value |
|---|---|---|---|---|
|
| ||||
| (N = 168) | (N = 85) | (N = 83) | ||
|
| ||||
| Age – M (SD) | 27.4 (6.1) | 27.2 (5.7) | 27.7 (6.5) | .59 |
| Range (18-44 years old) | ||||
|
| ||||
| Race - % (N) | ||||
| White | 41.7 (70) | 41.2 (35) | 42.2 (35) | |
| African American | 23.2 (39) | 24.7 (21) | 21.7 (18) | |
| Latina | 22.6 (38) | 22.4 (19) | 22.9 (19) | .82 |
| Asian/Pacific Islander | 7.1 (12) | 8.2 (7) | 6.0 (5) | |
| Native American /Alaskan | 5.4 (9) | 3.5 (3) | 7.2 (6) | |
|
| ||||
| Non-White - % (N) – | 58.3 (98) | 58.8 (50) | 57.8 (48) | 1.00 |
|
| ||||
| Marital Status - %(N) | ||||
| Married | 28.6 (48) | 22.4 (19) | 34.9 (29) | |
| Living with a partner | 33.3 (56) | 31.8 (27) | 34.9 (29) | |
| Partner (not living with) | 13.1 (22) | 12.9 (11) | 13.3 (11) | .08 |
| Living without a partner | 25.0 (42) | 32.9 (28) | 16.9 (14) | |
|
| ||||
| Living alone - % (N) | 17.9 (30) | 22.4 (19) | 13.3 (11) | .16 |
|
| ||||
| Education - % (N) | ||||
| Less than high school | 22.0 (37) | 22.4 (19) | 21.7 (18) | |
| High School degree/GED | 20.8 (35) | 18.8 (16) | 22.9 (19) | .93 |
| Some college/vocational | 46.5 (78) | 48.2 (41) | 44.6 (37) | |
| College grade or higher | 10.7 (18) | 10.6 (9) | 10.8 (9) | |
|
| ||||
| Employment - % (N) | ||||
| Full-time | 15.2 (25) | 21.7 (18) | 8.6 (7) | .02 |
| Part-time | 19.5 (32) | 22.9 (19) | 16.0 (13) | |
| Unemployed | 65.3 (107) | 55.4 (46) | 75.3 (61) | |
|
| ||||
| Income | ||||
| 10K or below - % (N) | 42.1 (69) | 41.2 (35) | 43.0 (34) | .88 |
|
| ||||
| Homelessness - % (N) | 13.4 (22) | 15.7 (13) | 11.0 (9) | .49 |
|
| ||||
| Past Pregnancy - % | 71.4 (120) | 75.3 (64) | 67.5 (56) | .31 |
|
| ||||
| Postpartum depression - % (N) for past pregnancies | 53.0 (62) | 47.6 (30) | 59.3 (32) | .26 |
|
| ||||
| Gestational Age – M (SD) | 22.4 (6.1) | 22.5 (6.0) | 22.4 (6.3) | .94 |
|
| ||||
| Unplanned Pregnancy- % (N) | 72.0 (118) | 78.3 (65) | 65.4 (53) | .08 |
|
| ||||
| Quite a bit or Very Positive about Pregnancy - % (N) | 62.6 (102) | 62.7 (52) | 62.5 (50) | 1.00 |
Table 4. Baseline Clinical, Childhood Trauma, and Personality Variables for Study Participants.
| Variable | Total Sample | MSS Public Health Care | MOMCARE | Statistical p Value |
|---|---|---|---|---|
|
| ||||
| (N = 168) | (N = 85) | (N = 83) | ||
|
| ||||
| Likely Depressive Disorders - % (N) | ||||
| PHQ Major Depression | 96.4 (162) | 98.8 (84) | 94.0 (78) | .11 |
| Dysthymia from MINI | 24.4 (41) | 25.9 (22) | 22.9 (19) | .72 |
| Depression and Dysthymia | 21.4 (36) | 24.7 (21) | 18.1 (15) | .35 |
|
| ||||
| # Previous Depressive Episodes | ||||
| Any prior episode - % (N) | 80.4 (135) | 83.5 (71) | 77.1 (64) | .34 |
| Too many to count/always - % (N) | 48.2 (81) | 44.7 (38) | 51.8 (43) | .44 |
| Average # of episodes for those reporting at least 1– M (SD) | 5.6 (5.5) | 5.1 (4.2) | 6.5 (7.1) | .37 |
|
| ||||
| Likely Anxiety Disorders - % (N) | ||||
| Panic Disorder | 21.3 (35) | 19.3 (16) | 23.5 (19) | .57 |
| GAD or other anxiety | 52.4 (86) | 50.6 (42) | 54.3 (44) | .64 |
| PTSD | 64.6 (106) | 69.9 (58) | 59.3 (48) | .19 |
| At least one anxiety disorder | 75.6 (127) | 76.5 (65) | 74.7 (62) | .86 |
|
| ||||
| Baseline Functioning | ||||
| aSCL Depression Score -M (SD) | 1.8 (.6) | 1.8 (.6) | 1.8 (.6) | .56 |
| bPTSD Severity Score- Sum (SD) | 48.8 (11.3) | 49.2 (10.8) | 48.4 (11.9) | .67 |
| cPerceived Stress - Sum (SD) | 25.3 (5.2) | 26.0 (5.0) | 24.7 (5.3) | .12 |
| dChronic Stress - Sum (SD) | 20.2 (8.4) | 19.5 98.6) | 21.0 (8.2) | .26 |
| -> Financial | 10.1 (3.8) | 10.1 (4.2) | 10.1 (3.5) | .99 |
| -> Ecological: Discrimination/ Poor Neighborhood/Crime | 10.2 (6.6) | 9.4 (6.2) | 10.9 (7.0) | .15 |
| eSocial Functioning - M (SD) | 2.9 (.58) | 2.9 (.60) | 2.8 (.55) | .17 |
|
| ||||
| Moderate to Severe Childhood Trauma - % (N) | ||||
| Emotional Abuse | 31.7 (52) | 39.8 (33) | 23.5 (19) | .03 |
| Physical Abuse | 15.2 (25) | 16.9 (14) | 13.6 (11) | .68 |
| Sexual Abuse | 15.5 (25) | 18.3 (15) | 12.7 (10) | .39 |
| Emotional Neglect | 37.8 (62) | 37.3 (31) | 38.3 (31) | 1.00 |
| Physical Neglect | 15.2 (25) | 18.1 (15) | 12.3 (10) | .39 |
| At least one type of trauma | 51.8 (87) | 55.3 (47) | 48.2 (40) | .44 |
|
| ||||
| Attachment orientation - % (N) | ||||
| Secure | 16.5 (27) | 19.3 (16) | 13.6 (11) | |
| Preoccupied/Anxious | 25.0 (41) | 22.9 (19) | 27.2 (22) | .76 |
| Dismissing/Self-reliant | 11.5 (19) | 10.8 (9) | 12.3 (10) | |
| Fearful | 47.0 (77) | 47.0 (39) | 46.9 (38) | |
A SCL-20 score of ≥ 0.5 indicates possible depression. Possible scores range from 0-4, with higher scores indicating more symptoms.
PCL scores range from 17 -85, with higher scores indicating more symptoms.
Perceived Stress scores range from 10-50, with higher scores indication higher levels of acute stress.
Chronic stress scores range from 12 (none)-60 (high); financial stress scores from 4-20; ecological stress scores from 8-40.
Social/leisure domain on the Social Adjustment Scale. Possible scores range from 1-5, with higher scores indicating greater impairment.
Almost all participants had likely major depression, with one-quarter experiencing likely dysthymia and one-fifth experiencing double depression. Eighty-percent reported a previous depressive episode, with an average number of 5.6 episodes. Over half of the sample met criteria for likely generalized anxiety disorder (GAD), almost two-thirds met criteria for likely post-traumatic stress disorder (PTSD), and three-quarters had at least one current anxiety disorder. Participants reported moderate to severe levels of depression severity, PTSD severity, perceived stress, chronic stress, and impairment in social functioning. Over half of the sample reported at least one type of childhood abuse and neglect and four-fifths reported an insecure attachment orientation, with close to half endorsing fearful attachment.
In addition, considering that major depression and PTSD most likely represent a joint psychiatric vulnerability with regard to trauma exposure95,102,123 and that PTSD and exposure to childhood trauma may delay or diminish treatment response for those with major depression,95,96,97,106 we planned to examine the impact of childhood trauma exposure and comorbid PTSD on treatment outcomes for our depressed participants. Table 5 shows baseline differences on demographic and clinical variables for the participants in the subgroup with MDD/Dysthymia alone and for those in the subgroup with MDD/Dysthymia and PTSD. Participants in the latter subgroup were more likely to be unemployed, and to have experienced a previous depressive episode, GAD, or another anxiety disorder in addition to PTSD. Not surprisingly, those with MDD/Dysthymia and PTSD, relative to their peers with depression alone, showed significantly higher scores on depression severity, PTSD severity, perceived stress, chronic stress, and impaired social functioning and more emotional abuse, emotional neglect, and physical neglect in childhood. They also reported a significantly more fearful attachment orientation relative to those with depression alone. This set of associations suggests that those with likely MDD and PTSD and those with likely MDD alone may represent different populations. Because of this constellation of multiple risk factors shown by the depressed participants with PTSD, we expected that their depression would be more difficult-to-treat.124,125
Table 5. Baseline Demographic, clinical, and childhood trauma variables for depressed participants with and without PTSD.
| Variable | Total Sample | MDD/Dysthymia NO PTSD | MDD/Dysthymia and PTSD | Statistical p Value |
|---|---|---|---|---|
|
| ||||
| (N = 164) | (N = 58) | (N = 106) | ||
|
| ||||
| Treatment Group - % (N) | ||||
| MOMCare | 49.4 (81) | 43.0 (25) | 45.3 (48) | .19 |
| Maternity Support Services Public Health Care | 50.6 (83) | 57.0 (33) | 54.7 (58) | |
|
| ||||
| Employment - % (N) | ||||
| Full-Time | 15.2 (25) | 13.8 (8) | 16.0 (17) | .02 |
| Part-Time | 19.5 (32) | 31.0 (18) | 13.2 (14) | |
| Unemployed | 65.2 (107) | 55.2 (32) | 70.8 (75) | |
|
| ||||
| Likely Depressive Disorders - % (N) | ||||
| PHQ Major Depression (MDD) | 96.3 (158) | 96.6 (56) | 96.2 (102) | .74 |
| Dysthymia from MINI | 23.8 (39) | 20.7 (12) | 25.5 (27) | .57 |
| MDD and Dysthymia | 20.7 (34) | 19.0 (11) | 21.7 (23) | .84 |
|
| ||||
| # Previous Depressive Episodes | ||||
| Any prior episode - % (N) | 82.3 (135) | 67.2 (39) | 90.6 (96) | .0001 |
| Too many to count or always - % (N) | 49.4 (81) | 29.3 (17) | 60.4 (64) | .0001 |
| Average # of episodes for those listing at least one – M (SD) | 5.6 (5.5) | 6.0 (5.6) | 5.4 (5.6) | .68 |
|
| ||||
| Likely Anxiety Disorders - % (N) | ||||
| Panic Disorder | 21.3 (35) | 15.5 (9) | 24.5 (26) | .23 |
| GAD or other anxiety | 52.4 (86) | 29.3 (17) | 65.1 (89) | .0001 |
| At least one anxiety disorder in addition to PTSD | 77.4 (127) | 36.2 (21) | 100.0 (106) | .0001 |
|
| ||||
| Baseline Functioning | ||||
| SCL Depression Score - M (SD) | 1.8 (.6) | 1.4 (.5) | 2.0 (.5) | .0001 |
| PTSD Severity Score - Sum (SD) | 48.8 (11.3) | 38.3 (6.7) | 54.6 (9.0) | .0001 |
| Perceived Stress - Sum (SD) | 25.3 (5.1) | 23.0 (4.8) | 26.6 (4.9) | .0001 |
| Chronic Stress – Sum (SD) | 20.2 (8.4) | 17.8 (7.5) | 21.6 (8.6) | .006 |
| → Financial | 10.1 (3.8) | 9.2 (3.9) | 10.6 (3.8) | .03 |
| → Ecological: Poor Neighborhood | 10.2 (6.6) | 8.6 (5.6) | 11.0 (7.0) | .03 |
| Social Functioning - M (SD) | 2.9 (.58) | 2.8 (.60) | 2.9 (.55) | .03 |
|
| ||||
| Moderate-Severe Childhood Trauma - % (N) | ||||
| Emotional Abuse | 31.7 (52) | 20.7 (12) | 37.7 (40) | .04 |
| Physical Abuse | 15.2 (25) | 8.6 (5) | 18.9 (20) | .11 |
| Sexual Abuse | 15.5 (25) | 12.3 (7) | 17.3 (18) | .50 |
| Emotional Neglect | 37.8 (62) | 25.9 (15) | 44.3 (47) | .03 |
| Physical Neglect | 15.2 (25) | 5.2 (3) | 20.8 (22) | .01 |
| At least one type of trauma | 53.0 (87) | 41.4 (24) | 59.4 (63) | .03 |
|
| ||||
| Attachment Orientation - % (N) | ||||
| Secure | 16.5 (27) | 19.0 (11) | 15.1 (16) | |
| Preoccupied/Anxious | 25.0 (41) | 36.2 (21) | 18.9 (20) | .02 |
| Dismissing/Extremely Self-reliant | 11.6 (19) | 13.8 (8) | 10.4 (11) | |
| Fearful | 46.9 (77) | 31.0 (18) | 55.7 (59) | |
A SCL-20 score of ≥ 0.5 indicates possible depression. Possible scores range from 0 to 4, with higher scores indicating more symptoms.
PCL scores range from 17 to 85, with higher scores indicating more symptoms.
Perceived Stress scores range from 10to 50, with higher scores indication higher levels of acute stress.
Chronic stress scores range from 12 (none) to 60 (high); financial stress scores from 4 to 20; ecological stress scores from 8 to 40.
Social/leisure domain on the Social Adjustment Scale. Possible scores range from 1 to 5, with higher scores indicating more impairment.
Preliminary evaluations of the MOMCare study from MSS public health providers showed high levels of satisfaction with the services provided to intervention participants. MSS social workers and nurses reported appreciating that MOMCare depression care specialists (DCSs) did “such a great job of staying in touch with us and clients” and their “giving updates on how clients are doing, as well as letting us know outcomes of referrals they made.” These providers commented that “it was great to know that [their] client was connected to the intervention and getting the extra support she needed” or that “it was really nice to be able to just walk down the hall and introduce the client” to the MOMCare DCS. When the MOMCare study stopped taking referrals, providers remarked that “Oh, this client would've been perfect for MOMCare. I wish this program was still going.” Overall, women who received the intervention were highly satisfied with the care they received for mood problems or stress. For example, when asked at the end of each treatment session what they liked or did not like, intervention participants made positive remarks, such as, “You help me plan what I'm going to do;” “I don't feel so alone;” “You help me see I am making progress;” “It helps just to talk and get my feelings out;” and “You have confidence in me.”
Discussion
Notwithstanding improvements in perinatal depression screening starting in 2006, the leadership of Maternity Support Services (MSS) of the public health system in Seattle and King County recognized that only a minority of depressed, pregnant women sought or actually received evidence-based psychotherapy or pharmacotherapy in the community. Thus, MSS administrators and staff were very supportive of examining the effectiveness of the MOMCare study on site with their public health patients. The study addressed an important question, “Does the MOMCare collaborative care intervention confer advantages to socio-economically disadvantaged, pregnant women greater than those that accrue from the MSS public health care services in treating depression in this population?” The primary aim of the MOMCare study was to test a health services model of care that was designed to address patient, provider, and system-level barriers to care and to enhance exposure of depressed, low-income, pregnant women to evidence-based models of depression care compared to MSS public health care. This research represented an important, incremental extension of previous work because it involved testing a collaborative care model in a different service environment than that of previous studies 30,31,32 – the public health system of Seattle-King County in Washington State..
Given the critical importance of treating antenatal depression to prevent postpartum depression and its probable adverse consequences for maternal and child health and mental health,3,4,5,6 the MOMCare study may prove to be an effective and cost-effective strategy for treating maternal depression during the perinatal period in socio-economically disadvantaged, vulnerable women. The integration of public health services, prenatal medical care, and behavioral health care is sorely needed both to relieve the suffering of low-income mothers with untreated depression (and their children and families) and to lower costs. If the MOMCare intervention proves cost-effective for pregnant women with likely MDD, and especially those with comorbid PTSD, the net benefits may facilitate further integration of mental health care into Maternity Support Services in Seattle-King County public health by means of Medicaid expansion and the Affordable Care Act.
A frequent criticism of clinical trials research is that clinical complexity, represented by childhood vulnerabilities and psychiatric comorbidity, is not taken into account. We therefore aimed to examine potential moderators of depression treatment response - specifically, exposure to childhood trauma and comorbid PTSD. Prior childhood adversity has been found to be associated with increased risk for adult depression and PTSD.103,104,105 Childhood trauma also predicts a 12-fold risk of having PTSD in pregnancy and is associated with a comorbidity of PTSD and depression during pregnancy. 126 PTSD has been found to affect from 8% - 33% of pregnant and parenting women,95,127 and, if comorbid with antenatal depression, appears to be associated with a 4-fold increased risk of preterm birth.128
With respect to mental health services research, childhood trauma has been observed to delay response to interpersonal psychotherapy for perinatal depression.106 PTSD also may delay or diminish treatment response for those with major depression. 95,96,97 Exploring the impact of childhood trauma and comorbid PTSD on perinatal depression care in low-income and minority women is of substantial public health significance and may inform depression screening and treatment. Implications for current clinical practice and service delivery in public health Maternity Support Services (MSS) may involve adding a childhood trauma questionnaire and a PTSD screening tool to the depression screening on the PHQ-9 that is already taking place at the intake interview. A stepped care, collaborative care treatment model for antenatal depression could be developed in the Seattle-King County public health system, as well as other local and state public health systems, whereby those high-risk pregnant women with likely MDD and PTSD would receive a more sustained, intensive intervention, similar to the one provided by the MOMCare intervention. Potential sustainability of the MOMCare intervention within a public health system requires further study.
Acknowledgments
This research was funded by NIMH MH 084897(Principal Investigator: Grote).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T, Gartlehner G, et al. Evidence Report/Technology Assessment No 119 AHRQ Publication 05-E006-2. Rockville, MD: Agency for Healthcare Research and Quality; 2005. Perinatal depression: prevalence, screening accuracy, and screening outcomes. Available from: http://archive.ahrq.gov/downloads/pub/evidence/pdf/peridepr/peridep.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Hara M, Swain A. Rates and risk of postpartum depression: a meta-analysis. Int Rev Psychiatr. 1996;8:37–54. [Google Scholar]
- 3.Grote NK, Bridge J, Gavin AF, Melville JL, Iyengar S, Katon WJ. A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiat. 2010;67(10):1012–24. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar R, Robson M. A prospective study of emotional disorders in childbearing women. Brit J Psychiat. 1984;144:35–47. doi: 10.1192/bjp.144.1.35. [DOI] [PubMed] [Google Scholar]
- 5.Moore G, Cohn J, Campbell S. Infant affective responses to mother's still face at 6 months differentially predict externalizing and internalizing behaviors at 18 months. Dev Psychol. 2001;37:706–14. [PubMed] [Google Scholar]
- 6.Murray L, Cooper P. The role of infant and maternal factors in postpartum depression, mother-infant interactions, and infant outcome. In: Murray L, Cooper P, editors. Postpartum depression and child development. New York: Guilford; 1997. pp. 111–35. [Google Scholar]
- 7.Gotlib I, Whiffen V, Wallace P, Mount J. Prospective investigation of postpartum depression: factors involved in onset and recovery. J Abnorm Psychol. 1991;100:122–32. doi: 10.1037//0021-843x.100.2.122. [DOI] [PubMed] [Google Scholar]
- 8.Hobfoll S, Ritter C, Lavin J, Hulszier M, Cameron R. Depression prevalence and incidence among inner-city pregnant and postpartum women. J Consult Clin Psych. 1995;63:445–53. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- 9.Scholle SH, Hasket RF, Hanusa BH, Pincus HA, Kupfer DJ. Addressing depression in obstetrics/gynecology practice. Gen Hosp Psychiat. 2003;25:83–90. doi: 10.1016/s0163-8343(03)00006-9. [DOI] [PubMed] [Google Scholar]
- 10.Miranda J, Chung J, Green B, Krupnick J, Siddique J, Revicki D, Belin T. Treating depression in predominantly low-income young minority women: a randomized controlled trial. J Amer Med Assoc. 2003;290:57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 11.Azocar F, Miranda J, Dwyer E. Treatment of depression in disadvantaged women. Women Ther. 1996;18:91–105. [Google Scholar]
- 12.Grote NK, Zuckoff A, Swartz HA, Bledsoe SE, Geibel SL. Engaging women who are depressed and economically disadvantaged in mental health treatment. Soc Work. 2007;52(4):295–308. doi: 10.1093/sw/52.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Arch Gen Psychiat. 2005;62(6):629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 14.Katon WJ. The Institute of Medicine “Chasm” report: implications for depression collaborative care models. Gen Hosp Psychiat. 2003;25:222–9. doi: 10.1016/s0163-8343(03)00064-1. [DOI] [PubMed] [Google Scholar]
- 15.Snowden LR. Barriers to effective mental health services for African Americans. Ment Health Serv Res. 2001;3:181–7. doi: 10.1023/a:1013172913880. [DOI] [PubMed] [Google Scholar]
- 16.Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21stcentury. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 17.Berwick D. A user's manual for the IOM's “Quality Chasm” Report. Health Affair. 2001;21:80–90. doi: 10.1377/hlthaff.21.3.80. [DOI] [PubMed] [Google Scholar]
- 18.Wagner E, Austin B, Von Korff M. Organizing care for patients with chronic illness. Millbank Q. 1996;74:511–43. [PubMed] [Google Scholar]
- 19.McGlynn E, Norquist G, Wells K, Sullivan G, Liberman R. Quality-of-care in mental health: responding to the challenge. Inquiry. 1988;25:157–70. [PubMed] [Google Scholar]
- 20.Armstrong H, Ishike D, Heiman J, Mundt J, Womack W. Service utilization by black and white clientele in an urban community mental health center: revised assessment of an old problem. Community Ment Hlt J. 1984;20:269–81. doi: 10.1007/BF00757076. [DOI] [PubMed] [Google Scholar]
- 21.Diamond R, Factor R. Treatment-resistant patients of treatment-resistant systems? Hosp Community Psych. 1994;45:197. doi: 10.1176/ps.45.3.197. [DOI] [PubMed] [Google Scholar]
- 22.Maynard C, Ehreth J, Cox G, Peterson P, McGann M. Racial differences in the utilization of public mental health services in Washington State. Adm Policy Mental Hlth. 1997;24:411–24. doi: 10.1007/BF02042723. [DOI] [PubMed] [Google Scholar]
- 23.Brown C, Abe-Kim J, Barrio C. Depression in ethnically diverse women: Implications for treatment in primary care settings. Prof Psychol-Res Pr. 2003;34:10–9. [Google Scholar]
- 24.Hall GC. Psychotherapy research with ethnic minorities: Empirical, ethical, and conceptual issues. J Consult Clin Psych. 2001;69:502–10. doi: 10.1037//0022-006x.69.3.502. [DOI] [PubMed] [Google Scholar]
- 25.McKay M, McCadam K, Gonzales J. Addressing the barriers to mental health services for inner city children and their caretakers. Community Ment Hlt J. 1996;32:353–61. doi: 10.1007/BF02249453. [DOI] [PubMed] [Google Scholar]
- 26.Corrigan PW. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614–25. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- 27.Mickelson K, Kessler R, Shaver P. Adult attachment in a nationally representative sample. J Pers Soc Psychol. 1997;73:1092–106. doi: 10.1037//0022-3514.73.5.1092. [DOI] [PubMed] [Google Scholar]
- 28.Bifulco A, Kwon J, Jacobs C, Moran PM, Bunn A, Beer N. Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Soc Psych Psych Epid. 2006;41:796–805. doi: 10.1007/s00127-006-0101-z. [DOI] [PubMed] [Google Scholar]
- 29.Ciechanowski P, Katon W, Russo J, Walker EA. The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. Am J Psychiat. 2001;158:29–35. doi: 10.1176/appi.ajp.158.1.29. [DOI] [PubMed] [Google Scholar]
- 30.Katon W, Von Korff M, Lin E, Walker E, Simon G, Bush T, et al. Collaborative management to achieve treatment guidelines: Impact on depression in primary care. J Amer Med Assoc. 1995;273:1026–31. [PubMed] [Google Scholar]
- 31.Katon W, Robinson P, Von Korff M, Lin E, Bush T, Ludman E, et al. A multifaceted intervention to improve treatment of depression in primary care. Arch Gen Psychiat. 1996;53:924–32. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- 32.Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiat. 1999;56:1109–15. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 33.Katon W, Rutter C, Ludman EJ, Von Korff M, Lin E, Simon G, et al. A randomized trial of relapse prevention of depression in primary care. Arch Gen Psychiat. 2001;58:241–7. doi: 10.1001/archpsyc.58.3.241. [DOI] [PubMed] [Google Scholar]
- 34.Katon W, von Korff M, Ciechanowski P, Russo J, Lin E, Simon G, et al. Behavioral and clinical factors associated with depression among persons with diabetes. Diabetes Care. 2004;27:914–20. doi: 10.2337/diacare.27.4.914. [DOI] [PubMed] [Google Scholar]
- 35.Katon W. Clinical and health services relationship between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–26. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 36.Institute of Medicine (IOM) Fetal alcohol syndrome: diagnosis, epidemiology, prevention, and treatment. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 37.Cowan C, Cowan P. When partners become parents: the big life change for couples. Mahwah, NJ: Lawrence Erlbaum Associates, Inc; 2000. [Google Scholar]
- 38.Grote NK, Swartz HA, Geibel S, Zuckoff A, Houck P, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiat Serv. 2009;60:295–308. doi: 10.1176/appi.ps.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spitzer R, Kroenke K, Williams J. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. J Amer Med Assoc. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 40.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 41.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller EC, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatricinterview for DSM-IV and ICD-10. J Clin Psychiat. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 42.Friedman RA. Social impairment in dysthymia. Psychiat Annals. 1993;23:632–7. [Google Scholar]
- 43.Markowitz JC. Psychotherapy of dysthymia. Am J Psychiatry. 1994;151:1114–21. doi: 10.1176/ajp.151.8.1114. [DOI] [PubMed] [Google Scholar]
- 44.Markowitz JC. Interpersonal psychotherapy for dysthymic disorder. Washington, D.C.: American Psychiatric Press; 1998. [Google Scholar]
- 45.Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry. 2003;160(3):555–62. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- 46.Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–17. [Google Scholar]
- 47.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–15. [PubMed] [Google Scholar]
- 48.Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:1–7. [Google Scholar]
- 49.Hobfoll S, Ritter C, Lavin J, Hulszier M, Cameron R. Depression prevalence and incidence among inner-city pregnant and postpartum women. Consult Clin Psychol. 1995;63:445–453. doi: 10.1037//0022-006x.63.3.445. [DOI] [PubMed] [Google Scholar]
- 50.Scholle SH, Hasket RF, Hanusa BH, Pincus HA, Kupfer DJ. Addressing depression in obstetrics/gynecology practice. General Hospital Psychiatr. 2003;25:83–90. doi: 10.1016/s0163-8343(03)00006-9. [DOI] [PubMed] [Google Scholar]
- 51.Spinelli MG, Endicott J, Leon AC, Goetz RR, Kalish R, Brustman LE, et al. A controlled clinical trial of interpersonal psychotherapy for depressed pregnant women at 3 New York City sites. J Clin Psychiat. 2013;74:393–9. doi: 10.4088/JCP.12m07909. [DOI] [PubMed] [Google Scholar]
- 52.Katon W, Ludman E, Simon G. The depression helpbook. Boulder: Bull Publishing Co; 2002. [Google Scholar]
- 53.Swartz H, Zuckoff A, Grote NK, Frank E, Spielvogle H, Bledsoe SE, et al. Engaging depressed patients in psychotherapy: integrating techniques from motivational interviewing and ethnographic interviewing to improve treatment participation. Prof Psychol-Res Pr. 2007;38:430–9. [Google Scholar]
- 54.Schensul SL, Schensul JJ, LeCompte MD. Essential ethnographic methods: observations, interviews, and questionnaires Ethnographer's toolkit 2. Walnut Creek, CA: Alta Mira Press; 1999. [Google Scholar]
- 55.Miller WR, Rollnick S. Motivational interviewing: preparing people for change. 2nd. New York: Guilford Press; 2002. [Google Scholar]
- 56.Weissman M, Klerman G, Prusoff B, Sholomskas D, Padian N. Depressed outpatients: results after one year of treatment with drugs and/or interpersonal psychotherapy. Arch Gen Psychiat. 1981;38:51–5. doi: 10.1001/archpsyc.1981.01780260053005. [DOI] [PubMed] [Google Scholar]
- 57.Weissman MM, Prusoff BA, Demascio A, Neu C, Goklaney M, Klerman GL. The efficacy of drugs and psychotherapy in the treatment of acute depressive episodes. Am J Psychiatry. 1979;136:555–8. [PubMed] [Google Scholar]
- 58.Klerman G, Weissman M. Interpersonal psychotherapy (IPT) and drugs in the treatment of depression. Pharmacopsychiatry. 1987;20:3–7. doi: 10.1055/s-2007-1017067. [DOI] [PubMed] [Google Scholar]
- 59.Kupfer DJ, Frank E, Perel JM, Cornes C, Mallinger AG, Thase ME, et al. Five-year outcomes for maintenance therapies in recurrent depression. Arch Gen Psychiat. 49:769–73. doi: 10.1001/archpsyc.1992.01820100013002. [DOI] [PubMed] [Google Scholar]
- 60.Frank E, Kupfer DJ, Cornes C, Morri S. Maintenance interpersonal psychotherapy for recurrent depression. In: Klerman G, Weissman MM, editors. New applications of interpersonal psychotherapy. Washington, DC: American Psychiatric Press; 1993. [Google Scholar]
- 61.O'Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch Gen Psychiat. 2000;57:1039–45. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- 62.Schulberg HC, Block MR, Madonia MJ. Treating major depression in primary care practice: eighth-month clinical outcomes. Arch Gen Psychiat. 1996;53:913–9. doi: 10.1001/archpsyc.1996.01830100061008. [DOI] [PubMed] [Google Scholar]
- 63.Swartz HA, Frank E, Shear MK, Thase ME, Fleming MA, Scott J. A pilot study of brief interpersonal psychotherapy for depression among women. Psychiat Serv. 2004;55:448–50. doi: 10.1176/appi.ps.55.4.448. [DOI] [PubMed] [Google Scholar]
- 64.Grote NK, Bledsoe SE, Swartz HA, Frank E. Feasibility of providing culturally relevant, brief interpersonal psychotherapy for antenatal depression in an obstetrics clinic: a pilot study. Res Social Work Prac. 2004;14:397–407. [Google Scholar]
- 65.Grote NK, Swartz HA, Zuckoff A. Enhancing interpersonal psychotherapy for mother and expectant mothers on low incomes: additions and adaptations. J Contemp Psychother. 2008;38:23–33. doi: 10.1007/s10879-007-9065-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jacobson NS, Martell CR, Dimidjian S. Behavioral activation treatment for depression: returning to contextual roots. Clin Psychol-Sci Pr. 2001;8:255–70. [Google Scholar]
- 67.Lewinsohn PM. A behavioral approach to depression. In: Friedman RJ, Katz M, editors. The psychology of depression: contemporary theory and research. Oxford, England: Wiley; 1974. pp. 157–78. [Google Scholar]
- 68.Beck J. Cognitive therapy: basics and beyond. New York: Guilford Press; 1995. [Google Scholar]
- 69.Grote NK, Swartz HA, Bledsoe SE, Frank E. Culturally relevant psychotherapy for perinatal depression in low-income ob/gyn patients. Clin Soc Work J. 2004;32:327–47. [Google Scholar]
- 70.Belle D. Poverty and women's mental health. Am Psychol. 1990;45:385–9. [Google Scholar]
- 71.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. J Amer Med Assoc. 2005;292:935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 72.Conner KO, Grote NK. A model for evaluating the cultural relevance of empirically-supported mental health interventions. Fam Soc. 2008;89:587–95. doi: 10.1606/1044-3894.3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chabrol H, Teissedre F, Armitage J, Danel M, Walburg V. Acceptability of psychotherapy and antidepressants for postnatal depression among newly delivered mothers. J Reprod Infant Psych. 2004;22:5–12. [Google Scholar]
- 74.Pearlstein TB, Zlotnick C, Battle CL, Stuart S, O'Hara MW, Price AB, et al. Patient choice of treatment for postpartum depression: a pilot study. Arch Women Ment Hlth. 2006;9:303–8. doi: 10.1007/s00737-006-0145-9. [DOI] [PubMed] [Google Scholar]
- 75.Goodman S, Dimidjian S, Williams KG. Pregnant African American women's attitudes toward perinatal depression prevention. Cultural Diversity and Ethnic Minority Psychology. 2013;19:50–7. doi: 10.1037/a0030565. [DOI] [PubMed] [Google Scholar]
- 76.Cooper WO, Willy ME, Pont SJ, Ray WA. Increasing use of antidepressants in pregnancy. Am J Obstet Gynecol. 2007;196:544.e1–5. doi: 10.1016/j.ajog.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 77.Dietz PM, Williams S, Callaghan W, Bachman D, Whitlock E, Hornbrook M. Clinically identified maternal depression before, during, and after pregnancies ending in live births. Am J Psychiat. 2007;164:1515–20. doi: 10.1176/appi.ajp.2007.06111893. [DOI] [PubMed] [Google Scholar]
- 78.American Academy of Obstetricians and Gynecologists. ACOG Practice Bulletin No 92: use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008;111:1000–20. [Google Scholar]
- 79.Wisner K, Gelenberg AJ, Leonard H, Zarin D, Frank E. Pharmacologic treatment of depression during pregnancy. J Amer Med Assoc. 1999;282:1264–9. doi: 10.1001/jama.282.13.1264. [DOI] [PubMed] [Google Scholar]
- 80.Hallberg P, Sjoblom V. The use of selective serotonin reuptake inhibitors during pregnancy and breast-feeding: a review and clinical aspects. J Clin Psychopharm. 2005;25:59–73. doi: 10.1097/01.jcp.0000150228.61501.e4. [DOI] [PubMed] [Google Scholar]
- 81.Weissman AM, Levy BT, Hartz AJ, Bentler S, Donohue M, Ellingrod VL, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiat. 2004;61:1066–78. doi: 10.1176/appi.ajp.161.6.1066. [DOI] [PubMed] [Google Scholar]
- 82.Wisner KL, Zarin DA, Holmboe ES, Appelbaum PS, Gelenberg AJ, Leonard HL, et al. Risk-benefit decision-making for treatment of depression during pregnancy. Am J Psychiat. 2000;157:1933–40. doi: 10.1176/appi.ajp.157.12.1933. [DOI] [PubMed] [Google Scholar]
- 83.ACOG Practice Bulletin: Clinical Management Guidelines for Obstetricians-Gynecologists, Number 87 Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2007;110:1179–98. doi: 10.1097/01.AOG.0000291559.02462.7f. [DOI] [PubMed] [Google Scholar]
- 84.Cohen LS, Altshuler LL, Harlow BL, Nonacs R, Newport DJ, Viquera AC, et al. Relapse of major depression during pregnancy in women who maintain or discontinue antidepressant treatment. J Amer Med Assoc. 2006;295:499–507. doi: 10.1001/jama.295.5.499. [DOI] [PubMed] [Google Scholar]
- 85.Kupfer D. Long-term treatment of depression. J Clin Psychiat. 1991;52:28–34. [PubMed] [Google Scholar]
- 86.Unützer J, Tang L, Oishi S, Katon W, Williams JW, Jr, Hunkeler E, et al. Reducing suicidal ideation in depressed older primary care patients. Amer Geriatr Soc. 2006;54:1550–6. doi: 10.1111/j.1532-5415.2006.00882.x. [DOI] [PubMed] [Google Scholar]
- 87.Pinto-Meza A, Serrano-Blanco A, Penarrubia MT, Blanco E, Haro JM. Assessing depression in primary care with the PHQ-9: can it be carried out over the telephone? J Gen Intern Med. 2005;20:738–42. doi: 10.1111/j.1525-1497.2005.0144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 89.Derogatis L. SCL-90-R Administration, Scoring and Procedures Manual II for the Revised Version. Towson, MD: Clinical Psychometric Research; 1983. [Google Scholar]
- 90.Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines: impact on depression in primary care. J Amer Med Assoc. 2005;273:1026–31. [PubMed] [Google Scholar]
- 91.Katon W, Robinson P, Von Korff M, Lin E, Bush T, Ludman E, et al. A multifaceted intervention to improve treatment of depression in primary care. Arch Gen Psychiat. 1996;53:924–32. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- 92.Unutzer J, Katon W, Callahan CM, Williams JW, Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. J Amer Med Assoc. 2002;288:2836–45. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 93.Fann JR, Bombardier CH, Dikmen S, Esselman P, Warms CA, Pelzer E, et al. Validity of the Patient Health Questionnaire-9 in assessing depression following traumatic brain injury. J Head Trauma Rehabil. 2005;20:501–11. doi: 10.1097/00001199-200511000-00003. [DOI] [PubMed] [Google Scholar]
- 94.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Beh Res Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 95.Green BL, Krupnick J, Chung J, Siddique J, Krause ED, Revicki D, et al. Impact of PTSD comorbidity on the one-year outcomes in a depression trial. J Clin Psychol. 2006;62:815–35. doi: 10.1002/jclp.20279. [DOI] [PubMed] [Google Scholar]
- 96.Hegel MT, Unutzer J, Tang L, Arean PA, Katon W, Noe PH, et al. Impact of comorbid panic and posttraumatic stress disorder on outcomes of collaborative care for late-life depression in primary care. Am J Geriat Psychiat. 2005;13:48–58. doi: 10.1176/appi.ajgp.13.1.48. [DOI] [PubMed] [Google Scholar]
- 97.Holtzheimer PE, 3rd, Russo J, Zatzick D, Bundy C, Roy-Byrne PP. The impact of comorbid posttraumatic stress disorder on shortterm clinical outcome in hospitalized patients with depression. Am J Psychiat. 2005;162:970–6. doi: 10.1176/appi.ajp.162.5.970. [DOI] [PubMed] [Google Scholar]
- 98.Griffin D, Bartholomew K. The metaphysics of measurement: the case of adult attachment. Adv Pers Relationship. 1994;5:17–52. [Google Scholar]
- 99.Scharfe J, Bartholomew K. Reliability and stability of adult attachment patterns. Pers Relationship. 1994;1:23–43. [Google Scholar]
- 100.Ciechanowski PS, Russo JE, Katon WJ, Korff MV, Simon GE, Lin EH, et al. The association of patient relationship style and outcomes in collaborative care treatment for depression in patients with diabetes. Med Care. 2006;44:283–91. doi: 10.1097/01.mlr.0000199695.03840.0d. [DOI] [PubMed] [Google Scholar]
- 101.Bernstein D, Fink L. Childhood trauma questionnaire: a retrospective self-report. San Antonio, TX: The Psychological Corporation; 1988. [Google Scholar]
- 102.Walker E, Gelfand A, Katon W, Koss MP, Von Korff M, Bernstein D, et al. Adult health status of women with histories of childhood abuse and neglect. Am J Med. 1999;107:332–9. doi: 10.1016/s0002-9343(99)00235-1. [DOI] [PubMed] [Google Scholar]
- 103.Widom CS. Posttraumatic stress disorder in abused and neglected children grown up. Am J Psychiat. 1999;156:1223–9. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- 104.Scott KM, Smith DR, Ellis PM. Prospectively ascertained child maltreatment and its association with the DSM-IV mental disorders in young adults. Arch Gen Psychiat. 2010;67:712–9. doi: 10.1001/archgenpsychiatry.2010.71. [DOI] [PubMed] [Google Scholar]
- 105.Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiat. 1999;156:902–7. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- 106.Grote NK, Spieker SJ, Lohr MJ, Geibel SL, Swartz HA, Frank E, et al. Impact of childhood trauma on the outcomes of a perinatal depression trial. Depress Anxiety. 2012;29:563–73. doi: 10.1002/da.21929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiat. 1976;33:1111–5. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 108.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 109.Norris FH, Uhl GA. Chronic stress as a mediator of acute stress: the case of Hurricane Hugo. J Appl Soc Psychol. 1993;23:1263–84. [Google Scholar]
- 110.Grote NK, Bledsoe SE, Larkin J, Brown C. Depression in African American and White women with low-incomes: the role of chronic stress. Soc Work Public Health. 2007;23:59–88. doi: 10.1080/19371910802148511. [DOI] [PubMed] [Google Scholar]
- 111.Grote NK, Bledsoe SE, Larkin J, Lemay E, Brown C. Stress frequency and depression in African American and White women with low-incomes: the protective effects of optimism and perceived control. Soc Work Res. 2007;31:19–33. [Google Scholar]
- 112.Fawcett J, Tulman L, Myers ST. Development of the inventory of functional status after childbirth. J Nurse-Midwifery. 1988;33:252–60. doi: 10.1016/0091-2182(88)90080-8. [DOI] [PubMed] [Google Scholar]
- 113.O'Hara M, Hoffman J, Phillips L, Wright E. Adjustment in postpartum women: the Postpartum Adjustment Questionnaire. Psychol Assessment. 1992;4:160–9. [Google Scholar]
- 114.Katon W, Von Korff M, Lin E, Simon G, Walker E, Unutzer J, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiat. 1999;56:1109–15. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 115.O'Hara MW, Varner MW, Johnson SR. Assessing stressful life events associated with childbearing: the Peripartum Events Scale. J Reprod Infant Psyc. 1986;4:85–98. [Google Scholar]
- 116.Briggs-Gowan MJ, Carter AS. Preliminary acceptability and psychometrics of the infant-toddler social and emotional assessment (ITSEA): A new adult-report questionnaire. Infant Ment Health J. 2000;19:422–45. [Google Scholar]
- 117.Sirey JA, Meyers BS, Teresi JA, Bruce ML, Ramirez M, Raue PJ, et al. The Cornell Service Index as a measure of health service use. Psychiat Serv. 2005;56:1564–9. doi: 10.1176/appi.ps.56.12.1564. [DOI] [PubMed] [Google Scholar]
- 118.Katon WJ, Schoenbaum M, Fan MY, Callahan CM, Williams J, Hunkeler E, et al. Cost-effectiveness of improving primary care treatment of late-life depression. Arch Gen Psychiat. 2005;62:1313–20. doi: 10.1001/archpsyc.62.12.1313. [DOI] [PubMed] [Google Scholar]
- 119.Unutzer, Katon unpublished report [Google Scholar]
- 120.Saunders K, Simon G, Bush T, Grothaus L. Assessing feasibility of using computerized pharmacy refill data to monitor antidepressant treatment on a population basis: A comparison of automated and self-report data. J Clin Epidemiol. 1998;51:883–90. doi: 10.1016/s0895-4356(98)00053-5. [DOI] [PubMed] [Google Scholar]
- 121.EuroQoL Group. EuroQoL - a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 122.Littell RC, Milliken GA, Stroup WW, Wolfinger R. SAS system for mixed models. Cary, NC: SAS Publications; 1996. [Google Scholar]
- 123.Silverstein M, Feinberg E, Sauder S, Egbert L, Stein R. Comorbid post-traumatic stress symptoms in an urban population of mothers screening positive for depression. Arch Pediatr Adolesc Med. 2010;164:778–9. doi: 10.1001/archpediatrics.2010.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Grote NK, Frank E. Difficult-to-treat depression: the role of contexts and co-morbidities. Biol Psychiat. 2003;53:660–70. doi: 10.1016/s0006-3223(03)00006-4. [DOI] [PubMed] [Google Scholar]
- 125.Kaplan MJ, Klinetob NA. Childhood emotional trauma and chronic post-traumatic stress disorder in adult outpatients with treatment-resistant depression. J Nerv Ment Dis. 2000;188:596–601. doi: 10.1097/00005053-200009000-00006. [DOI] [PubMed] [Google Scholar]
- 126.Seng JS, Low LK, Sperlich M, Ronis DL, Muzik M, Liberson I. Trauma history and risk for PTSD among nulliparous women in maternity care. Obstet Gynecol. 2009;114:839–47. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberson I. Childhood abuse history, post-traumatic stress disorder, postpartum mental health, and bonding: A prospective cohort study. J Midwifery Women's Health. 2013;58:57–68. doi: 10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2014.558. published online June 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zuckoff AM, Swartz HA, Grote NK. MI as prelude to psychotherapy of depression. In: Arkowitz H, Westra H, Miller WR, Rollnick S, editors. Motivational interviewing in the treatment of psychological problems. New York: Guilford; 2008. [Google Scholar]