Abstract
Recent epidemiological and clinico-pathological data indicate considerable overlap between cerebrovascular disease (CVD) and Alzheimer’s disease (AD) and suggest additive or synergistic effects of both pathologies on cognitive decline. The most frequent vascular pathologies in the aging brain and in AD are cerebral amyloid angiopathy and small vessel disease. Up to 84% of aged subjects show morphological substrates of CVD in addition to AD pathology. AD brains with minor CVD, similar to pure vascular dementia, show subcortical vascular lesions in about two-thirds, while in mixed type dementia (AD plus vascular dementia), multiple larger infarcts are more frequent. Small infarcts in patients with full-blown AD have no impact on cognitive decline but are overwhelmed by the severity of Alzheimer pathology, while in early stages of AD, cerebrovascular lesions may influence and promote cognitive impairment, lowering the threshold for clinically overt dementia. Further studies are warranted to elucidate the many hitherto unanswered questions regarding the overlap between CVD and AD as well as the impact of both CVD and AD pathologies on the development and progression of dementia.
Electronic supplementary material
The online version of this article (doi:10.1186/s12916-014-0206-2) contains supplementary material, which is available to authorized users.
Keywords: Alzheimer’s disease, Cerebrovascular lesions, Cerebral amyloid angiopathy, Cognitive impairment, Lacunes, Microinfarcts, Small vessel disease, White matter lesions
Introduction
The interaction between cerebrovascular disease (CVD) and Alzheimer’s disease (AD) is a topic of considerable current interest. With age there is an increasing prevalence of coincident AD and CVD that is well recognized. Since 50% to 84% of the brains of persons who die aged 80 to 90+ show appreciable cerebrovascular lesions (CVL) [1], a specific problem is their impact in relation to AD pathology [2]-[8]. CVD frequently occurs in brains of both non-demented elderly and AD patients. The burden of vascular and AD-type pathologies are leading and independent causes of dementia in the elderly [4],[9]-[15], suggesting additive or synergistic effects of both types of lesions on cognitive impairment [2],[3],[5],[9],[16]-[29].
Epidemiological studies have shown that AD and CVD share common risk factors such as hypertension during midlife, diabetes mellitus, smoking, apolipoprotein E (ApoE) ε4 isoforms, hypercholesterolemia, homocysteinemia, and, in particular, age [16],[30]-[34]. Cardiovascular risk factors, e.g., atrial fibrillation and congestive heart failure, have also been linked to the pathogenesis and progression of AD and are among the most important modifiable risk factors for AD [35]-[42]. In the Medical Research Council Cognitive Function and Ageing Study, vascular risk factors were not associated with an increased burden of AD pathology at death in old age, whereas cerebral small vessel disease (SVD) and cardiovascular disease were interrelated [43]. According to other studies, non-stroke cardiovascular disease increases the risk of late-life dementia but it is only a risk factor for AD in carriers of the ApoEε4 allele, while the association between cardiovascular disease and dementia is not explained by genetic or early life environmental factors common to both disorders [44]. AD patients with concomitant CVD were reported to be older and more severely demented, but have less severe AD pathology than patients without CVD [23],[45].
Review
Coincidence between cerebrovascular disease and Alzheimer’s disease
There is a large body of literature regarding coincidence or overlap of CVD and AD and its correlation with dementia [1],[4],[5],[9],[10],[46]-[48]. Of note, this association was recently found to be stronger in cases with lower neurofibrillary tangle pathology (i.e., lower neuritic Braak stages) [5], similar to earlier studies on respective associations with subcortical vascular pathology [6] and general CVD [1]. However, others found an inverse relation between neuritic Braak stage and cerebrovascular pathology in AD [49]. A recent study assessed CVD in 5,715 autopsy cases of the National Alzheimer’s Coordinating Center (NACC) database, and confirmed previous data on the prevalence of CVD in AD and the additive or interactive deleterious effect of both AD and vascular pathologies on cognition [6],[9],[47],[50],[51]. However, the role of combined cerebrovascular pathology and AD in dementia is still under discussion and data obtained from epidemiological and clinico-pathological studies regarding their relation are controversial [13],[17],[22],[23],[52]-[55].
AD has been reported to present frequently together with SVD, microvascular injury, and microscopic CVLs [8],[16],[47],[56]-[60]. SVD-induced ApoE leakage was associated with AD and accumulation of β-amyloid (Aβ) in perivascular astrocytes [61] and transient induction of Aβ deposition [62]. CVD has been shown to induce Aβ deposition, which may by itself cause CVD, in particular micro-vascular degeneration [63]. In addition, aging, per se, has an effect on cerebral arteries in relation to AD since such age related changes may impair the drainage of soluble Aβ out of the brain, which in turn leads to Aβ accumulation in vessel walls and brain parenchyma associated with perturbation of cerebral perfusion and loss of homeostasis of the neuronal environment due to energy failure [64],[65]. It was also suggested that more Aβ accumulates with age in brains of vascular dementia (VaD) subjects compared to elderly without CVD [66].
Activity of smooth muscle actin (SMA) was reduced in the brains of patients with late stage AD, while increased arteriolar SMA expression together with frequent Aβ plaques observed in the brains of non-demented subjects suggests that increased SMA expression might represent a physiological response to neurodegeneration that could prevent or delay the onset of clinical dementia in subjects with cerebral AD neuropathology [67]. Vascular disease is thought by many authors to play a major role in the pathogenesis of AD and some even consider AD as being rather a primarily vascular than a neurodegenerative disorder [22],[68]-[74]. Cerebral hypoperfusion-inducing cortical microinfarcts may further aggravate cognitive decline in AD [75]. However, AD pathology alone more frequently accounts for dementia than both macroscopic and microscopic infarcts [15] and, in late stages of AD, concomitant SVLs do not significantly influence the overall state and progression of cognitive decline [45],[54],[76], the severity and extent of AD pathology overwhelming the rather modest influence of CVD on cognitive impairment [8],[77],[78]. These data add further evidence for AD pathology (mainly neurofibrillary tangles and neuritic plaques) being the main morphological substrate of clinical dementia [51],[79],[80]. On the other hand, CVD has been associated with worse cognitive performance in AD and neuropathological studies report that CVD lowers the threshold for dementia in subjects with a pathological diagnosis of AD [5],[6],[8],[9],[13],[17],[23],[51],[53],[81]-[83]. CVD has been suggested to contribute to AD neuropathological changes including selective brain atrophy and accumulation of abnormal proteins such as Aβ [24],[35],[84],[85]. Moreover, AD pathology and subcortical vascular disease may independently affect cortical atrophy [86].
Vascular pathology in aging and Alzheimer’s disease
The types of vascular pathology in the aged human brain include:
Cerebral amyloid angiopathy (CAA);
Cerebral atherosclerosis, SVD (in most cases caused by hypertension, i.e., hypertensive vasculopathy), or microvascular degeneration (tortuosity, fibro- and lipohyalinosis,);
Blood-brain barrier (BBB) dysfunction causing white matter lesions (WMLs), microinfarctions, lacunes or lacunar infarcts, and microbleeds [17],[87].
All of these pathologies may disrupt the integrity of cerebral vessels and alter brain perfusion leading to neuronal injury and cognitive impairment
CAA results from focal to widespread deposition of Aβ within leptomeningeal and intracortical arteries, arterioles, capillaries, and, rarely, veins causing fibrinoid necrosis, intimal thickening, and microaneurysms. In addition, pericapillary Aβ refers to Aβ depositions in the glia limitans and adjacent neuropil, whereas in capillary CAA Aβ depositions are present in the capillary wall [88]. Sporadic CAA is present in 82% to 98% of AD patients, often associated with ApoE2 and ApoE4 alleles [80], but is also frequently observed in brains of elderly non-demented individuals with an age-related prevalence between 10% and almost 100% [17],[89]. The occipital lobe has been reported to be the site most frequently and severely affected by CAA, followed by either frontal, temporal, or parietal lobes [89],[90]. CAA may cause lobar intracerebral hemorrhages (ICH) and microbleeds [91]; it is indeed considered a risk factor for non-traumatic ICHs in the elderly and is present in up to 20% of all cases with ICH [92]. However, in a large autopsy cohort, the prevalence of ICH was similar in cases with and without CAA (around 5%) [93],[94]. Of note, the majority of cases with CAA-related ICH had hypertension, suggesting that hypertension is an important additional causal factor in CAA-related ICHs [95],[96]. The progression of WMLs in subjects with CAA has been associated with incident lobar ICHs [97]. CAA has been suggested to cause cortical microinfarcts [98],[99], while others did not confirm such an association [100]. Moderate to severe CAA is considered to be an independent risk factor for cognitive impairment [101].
The clinical diagnosis of CAA is based on the assessment of associated CVLs by magnetic resonance imaging (MRI)/cranial computerized tomography (CCT) and clinical data. Correlations of these criteria with post-mortem neuropathological findings indicate that the diagnosis of probable CAA-related hemorrhage can be made intra vitam with high accuracy [102]-[105]. In addition to the presence of superficial siderosis, cerebral microbleeds, cortical microinfarcts, and hypointensities in MRI images [106]-[109], the use of Pittsburgh Compound-B (PiB)-positron emission tomography (PET) is useful in detecting CAA intra vitam[110],[111], and a significant decrease of both Aβ-40 and Aβ-42 in cerebrospinal fluid (CSF) may prove useful in the diagnosis of CAA [112],[113], while in AD, Aβ-42 but not Aβ-40 are significantly decreased [114].
SVD affects small arteries and arterioles and refers to pathological changes similar to atherosclerosis that are termed small vessel arteriosclerosis/atherosclerosis, lipo- or fibrohyalinosis, or hypertensive arteriopathy [115]. They are common in basal ganglia and in the white matter, while small brainstem arteries usually develop arteriosclerosis only in end stages of SVD and cortical vessels usually do not show signs of SVD [116]. In AD neither Aβ load nor metabolic deficit are dependent on the age of disease onset, but patients with late-onset AD show a significantly higher amount of SVD that influences the association between metabolic deficit and clinical symptoms [117]. SVD is a frequent cause of white matter lesions (WMLs; leukoaraiosis) that are increasingly detected by neuroimaging [118]-[121]. Enlarged perivascular spaces in the centrum semiovale are MRI markers indicative of CAA (in the overlying cortex), while those in basal ganglia are usually associated with hypertensive arteriopathy [103],[104]. Deep cerebral microbleeds (CMB) are mainly linked to subcortical SVD, while both subcortical SVD and CAA interact to increase the risk of lobar CMBs [122],[123]. The associated morphological findings include demyelination, axon loss, lacunar infarcts, or enlarged perivascular spaces, most frequently in the frontal, parietal, and occipital white matter [124]. Frontal lobe WMLs have been shown to be associated with neurofibrillary pathology, particularly in the oldest old, while there was no relationship with neocortical Aβ load [125]. Routine histological assessment may underrate mild to moderate subcortical vascular lesions, but MRI imaging of fixed post-mortem brains reliably reflects subcortical vascular pathology of the white matter [126],[127].
BBB dysfunctions related to SVD leading to a leakage of plasma proteins into enlarged perivascular spaces [61],[128] have been described in WMLs and lacunar stroke [129],[130]. These observations point towards SVD-related alterations of the pre-capillary BBB segment which are involved in the pathogenesis of WMLs/lacunar infarcts and associated with vascular lesions in addition to AD-related changes [61],[116]. Thus, chronic plasma protein leakage into the brain and retention of extracellular fluid due to altered perivascular clearance may contribute to the development of WMLs and/or lacunar infarcts [2],[3],[87]. Damage to the vasculature may, in turn, impair the BBB integrity as one mechanism by which WMLs may evolve [124]. Mechanisms leading to BBB leakage in aging brains are complex, including oxidative damage and the activation of proteases, matrix metalloproteinases, and cyclooxygenases [131]. Evidence of early increase of BBB changes and their progression with severity of AD-type pathology suggest that BBB dysfunction contributes to damage in the aging brain [132].
Atherosclerosis is a very common vessel disorder in elderly individuals, frequently affecting large- to medium-sized arteries of the entire cardiovascular system (large-vessel disease; LVD). With respect to the cerebrum, it mainly affects the circle of Willis and the carotid arteries, in particular at the level of the carotic bifurcation. It causes narrowing of the arteries’ lumina, thereby reducing the blood blow for the supported region, while rupture of atherosclerotic plaques often leads to thrombosis that results in either occlusion of the vessel or thromboembolisms. Depending on the size of the embolus, it may cause lesions that range from “silent” infarcts or microinfarcts to large cerebral infarcts with overt clinical symptoms. “Silent” lacunar infarcts are frequently detected by MRI or CCT and are not accompanied by any overt clinical symptoms, but double the risk of subsequent stroke and dementia [133]. They have been shown to be associated with atrophy in multiple subcortical structures, ventricular enlargement, and widespread cortical thinning, supporting the assumption of a vascular contribution to neurodegeneration and cognitive impairment [134]. As opposed to large and lacunar infarcts, cortical microinfarcts (CMI) are usually not visible at gross neuropathological examination. Due to the location of the underlying vessel disorder, multiple cortical CMIs are often associated with CAA, whereas subcortical microinfarcts are mainly linked to SVD or atherosclerosis-related embolism [135]. A systemic review of CMIs reported frequencies of 43% in patients with AD and 24% in non-demented older adults [136], while a 7-Tesla MRI study revealed CMI occurrence in 55% of early AD and 45% of non-demented age-matched controls [137].
Widespread CAA and SVD have been suggested to contribute to neurodegeneration in AD [116]. Moreover, atherosclerosis in the circle of Willis has been specifically linked to AD [138]-[140], and the presence of large-vessel CVD was strongly associated with an increased frequency of neuritic plaques, suggesting a common etiology or a reciprocal regulation for atherosclerosis and AD [138],[141]. Others, however, saw no direct association between large-vessel cerebral atherosclerosis and AD pathology [142], suggesting that atherosclerosis of the intracranial vessels is an independent and important risk factor for dementia due to potentially reversible pathways unrelated to AD pathology and stroke [143]. The pathophysiology of VaD has been critically reviewed recently [48],[144]-[146].
Topographical distribution of cerebrovascular lesions
In AD brains with minor CVD the majority of CVLs are lacunar infarcts in basal ganglia and white matter, and multiple micro-infarcts. This pattern of topographical distribution of CVLs is very similar to the one seen in “pure” vascular dementia (VaD without AD pathology beyond age-related lesions), where around 68% are lacunar infarcts in subcortical brain areas or strategic infarcts involving the thalamus or hippocampus, whereas only 32.5% were multiple large cortico-subcortical infarcts (Table 1). By contrast, mixed dementia (AD + severe CVD), according to our experience, is more frequently characterized by large or lobar infarcts, and multiple cortico-subcortical lesions (56.6%) than small subcortical lacunar infarcts, micro-infarcts, or strategic infarcts (43.4%, Table 2), suggesting different pathogenic mechanisms between these types of disorders [2],[3]. In both pure VaD and AD + minor CVD, microangiopathy (SVD) appears more important than in mixed dementia. The type and average prevalence of CVLs in AD, VaD, mixed dementia, and aged controls is shown in Table 3[147]. The combination of two or more pathological processes may influence the severity of cognitive deficits, unmasking preclinical dementia due to mild AD lesions, while small CVLs alone, seen in 10% to 50% of aged cognitively unimpaired controls, are not likely to account for a single cause of dementia.
Table 1.
Types and location of cerebrovascular lesions in vascular dementia (total 188)
| Multiple infarcts (61 = 32.5%) | |
| MCA bilateral | 4 |
| MCA left/right | 9 |
| MCA bilat. + PCAS/PCAD | 2/1 |
| MCA bilat. + PCA bilat. | 2 |
| MCAS + PCAS | 4 |
| MCAD + PCAD | 4 |
| PCA bilateral | 3 |
| PCA left/right | 5/7 |
| ACAS + MCAS | 2 |
| ACAD | 1 |
| Multiple cortico-subcortico bilateral | 12 |
| Multiple cortico-subcortico left hem. | 2 |
| SAE (subcortical) (108 = 57.4%) | |
| Basal ganglia | 21 |
| Basal ganglia + white matter | 31 |
| Basal ganglia + thalamus (+white matter) | 33 |
| Basal ganglia brainstem (+thalamus) | 23 |
| SID/strategic infarcts (19 = 10.1%) | |
| Thalamus bilateral | 9 |
| Thalamus left | 2 |
| Thalamus + hippocampus | 8 |
Table 2.
Types and location of cerebrovascular lesions in mixed dementia (n = 83)
| 1) AD + Multiple infarcts (47 = 56.6%) | |
| MCA bilateral | 7 |
| MCA left | 6 |
| MCA right (+ lacunes basal ganglia) | 3/1 |
| MCA + ACA bilat. | 1 |
| MCA + PCA left | 2 |
| MCA + PCA right | 1 |
| MCA + PCA left/right | 3/3 |
| MCA bilat. +PCAD | 1 |
| PCA bilateral | 2 |
| Multiple cort. and subcort. bilateral | 13 |
| Multiple left hemisphere | 4 |
| 2) AD + SAE (subcortical) (33 = 39.8%) | |
| Lacunes basal ganglia | 15 |
| Lacunes basal ganglia + white matter | 8 |
| Lacunes basal ganglia + thalamus | 10 |
| 3) AD + SID/strategic infarcts (3 = 3.6%) | |
| Thalamus bilateral | 2 |
| Thalamus + hippocampus | 1 |
Table 3.
Common lesions in AD, VaD, MIX, and aged controls (from[130])
| Pathological feature | AD [%] | VaD [%] | MIX [%] | Aged controls [%] |
|---|---|---|---|---|
| Cerebral amyloid angiopathy | 98 | 30 | ~90 | 23-45 |
| Small vessel disease/MVD | ~50 | >50 | >50 | ~20 |
| Total infarctions | 10-20 | 100 | 30-40 | >10 |
| Microinfarcts/lacunes | 30-46 | 70 | 60-70 | 17-21 |
| Intracerebral hemorrhage | 10-15 | 15 | 10 | 1-2 |
| White matter pathology | 40 | 80 | 70-80 | <20 |
| Loss of cholinergic markers | 75 | 40 | ~70 | |
| CVD/atherosclerosis | 45-60 | 60 | ~60 | 30-53 |
Abbreviations: AD, Alzheimer’s disease; CVD, Cerebrovascular disease; MIX, mixed type dementia (AD plus vascular dementia); MVD, Microvascular disease; VaD, Vascular dementia.
Cerebrovascular and Alzheimer’s disease pathology in demented and non-demented elderly
In a series of 300 autopsy cases of AD, Kalaria and Ballard [148] reported 98% CAA, 100% microvascular degeneration, 31% infarcts of all sizes, and 7% intracerebral hemorrhage, while Olichney [149], in a cohort of 248 autopsy cases of AD, revealed a total of 48% CVLs, with 31% microinfarcts, 12.5% large infarcts, and 13.5% hemorrhages. Comparing 173 autopsy-proven AD cases and 130 age-matched controls, CVL were significantly less frequent in controls (42.4%) as compared to AD (56.4%, P <0.05), and CAA was seen in 97.2% of AD cases, out of which 26% showed severe degrees [150]. In a population-based study of 419 demented persons, with neuropathological data available in 89 (21%), the neuropathological diagnoses were AD (51%), VaD (13%), combined AD + VaD (12%), and others (24%). Criteria for pure VaD using imaging results (Mayo Clinic criteria) showed 75% sensitivity and 81% specificity [151]. In a UK population-based autopsy study on elderly subjects (n =209, 48% demented), neuropathological evidence of CVD was found in 78% and of AD in 70%. The proportion of multiple CVL was higher in the demented group, while only 21% of clinically-demented patients showed “pure” AD pathology at post-mortem, indicating that most patients had mixed disease [152]. In a retrospective series of 730 autopsy cases of AD and 535 age-matched controls, using a four-grade scale for the severity of CVLs, the total prevalence of CVD in AD was significantly higher than in controls (31.6% vs. 23.4%) [153]. In a population based longitudinal study of over-80-year-old brain donors from Cambridge, UK, 53% of subjects presented with clinical dementia. In those cases, neuropathological findings were consistent with AD in 67% and with pure VaD in 4%, while 22% showed mixed pathologies and 1% dementia with Lewy bodies. AD and CVD frequently co-existed in the very old [154]. Among 190 older autopsy cases, 68% had CVLs, vascular score was associated with dementia (OR, 1.6), AD (OR, 1.5), and VaD (OR, 2.0). Leukoencephalopathy, large infarcts, and higher vascular burden were associated with clinical dementia [18]. Analysis of 4,629 cases of the NACC database with autopsy-confirmed neurodegenerative AD classified 79.7% as having CVD [37].
In a recent study from the Oxford Project to Investigate Memory and Ageing, assessment of the severity of SVD in 161 cases of autopsy-confirmed AD gave no relationship between the SVD score and cognitive scores acquired in the last two years of life nor to blood pressure at entry; further, SVD scores were significantly lower when compared with a cohort of cases with only CVD [8]. Assessment of 175 autopsy cases in the Baltimore Longitudinal Study of Aging cohort found no relationship between the degree of atherosclerosis in the aorta, heart, and intracranial vessels and the degree of AD pathology, while the presence of intracranial atherosclerosis significantly increased the odds of dementia, independent of cerebral infarction [143].
A recent study from the NACC selected 835 subjects that represent the AD continuum. While the cause of mild to moderate dementia remained uncertain in 14% of the patients, plaques and tangles independently predicted cognitive dysfunction, as did severe SVD, CAA, and hippocampal sclerosis. Thus, concomitant CVD strongly correlated with cognitive impairment in this sample selected to represent the AD pathology continuum, confirming the uncertainty of AD clinico-pathological correlations based only on neurofibrillary tangles and Aβ-plaques [155]. Assessment of 856 participants of two longitudinal clinico-pathological studies (Rush Memory and Aging Project and Religious Orders Study, autopsy rate 80%, mean age at death 88.2 ± 6.5 years) showed that global AD pathology, Aβ-plaques, neurofibrillary tangles, macroscopic infarcts, and neocortical Lewy bodies were associated with faster rates of decline and explained 22%, 6%, 34%, 2%, and 8% of the variation in decline, respectively. However, much of the variation in cognitive decline remains unexplained, suggesting that other important determinants of cognitive decline remain to be identified [156].
In a consecutive autopsy series of 494 cases (257 autopsy-proven AD, mean age 83.1 ± 8.4 years and 237 age-matched non-demented controls), 42.7% of the AD brains, all showing advanced AD pathology, were free of essential vascular pathology except for minor to moderate CAA (50%) and without CVLs, compared to 66.8% in age-matched controls, all showing low Braak stages (P <0.01). Prevalence of CAA in AD was 94.1% (45% severe degrees) as compared to 33.3% in controls. The severity of CAA was significantly higher in AD brains with CVLs compared to controls with similar vascular lesions [157]. Minor and moderate vascular pathology in AD were about twice as frequent as in controls (26.2% vs. 12.2% and 20.9% vs. 11.3%; P <0.01). On the other hand, severe vascular pathology did not significantly differ between both groups (10.2% vs. 12.2%). Retrospective examination of the prevalence of CVD in a consecutive autopsy series of 621 autopsy-proven AD cases and 486 age-matched controls, using a four-degree scale for cerebrovascular pathology, showed a generally higher prevalence of CVLs in AD (67.8%) than in controls (29.4%); severe CVLs (old/recent infarcts and hemorrhages) were more frequent in AD (23.6%) than in controls (5.4%). Likewise, the prevalence of cortico-subcortical infarcts and subcortical vascular lesions was higher in AD (41.2%) compared to controls (11.6%) [157]. Both the incidence and severity of CVLs increased with higher neuritic Braak stages as was reported in a previous study [12]. In elderly subjects with and without dementia, the prevalence of “pure” VaD (without other cerebral pathologies) ranged from 5% to 78% and in the oldest old group from 4.5% to 46.8% [47], while the majority (24% to 93%) showed mixed pathologies [158],[159]. In the age group 70 to 90+, the prevalence of VaD increased from 13% to 44.8%, compared to AD (23.6% to 57%) and mixed dementia (2% to 86%) [47]. In contrast to AD and mixed dementia, the prevalence of pure VaD decreased after 80 years of age [145],[158].
Cerebrovascular lesions are found in the majority of late-onset AD and only in half of early-onset AD cases [160]. There are considerable differences in the pathological burden in relation to age of onset of dementia, suggesting that late onset is associated with increased vascular pathology and lower AD burden [161],[162]. However, in a 90+ study, there was extensive overlap in pathology among those with and without dementia; 22% of demented subjects did not have significant pathology to account for their cognitive impairment [163]. A specific caveat in this respect is the effect of sample selection in incident-bases dementia autopsy series [164]. Community samples tend to show greater degrees of cerebrovascular pathology as compared to hospital based samples; and the prevalence of mixed AD/CVD was higher in the community-based RUSH Memory and Aging Project (44%) than in the RUSH Religious Order Study (28%). Therefore, the type of study sample may strongly bias results and should be mentioned as a possible contribution to variability of findings.
Many studies emphasized multiple confounding pathologies in non-demented elderly subjects, in particular CVLs, e.g., small or large cerebral infarcts, lacunes, and WMLs, in up to 10% [10],[165]-[167]. Among 418 non-demented participants of the Religious Order Study (mean age 88.5 ± 5.3 years), 35% showed macroscopic brain infarcts and 14.8% arteriosclerosis, while only 37.5% were free of any CVD [168]. Various degrees of CAA have been found in up to 75% of cognitively normal seniors [167]. Among 100 non-demented elderly, mild, moderate, and severe intracranial atherosclerosis was present in 31%, 17%, and 6% of subjects, respectively. A lacunar state in basal ganglia and/or white matter was observed in 73%, hippocampal sclerosis in 3%, and mixed cerebral pathologies in 6%, whereas only 9% were free of CVLs [169]. A recent cross-sectional study in a community-based sample of 72 cognitively normal older individuals (mean age 74.9 ± 5.7 years) confirmed that a substantial number harbor neurodegeneration without Aβ burden, but association of neurodegenerative lesions with CVD can emerge through non-Aβ pathways within regions most affected by AD [170].
Pathogenic factors
Microvascular changes in the aged brain and in AD induce impairment of cerebral perfusion, in particular decrease of regional blood flow, reduction of glucose transport and utilization, loss of vascular innervation with special impact on the cholinergic and transmitter deficits in AD [171], impairment of neurovascular regulation, ultrastructural changes in capillaries and basement membranes due to deposition of Aβ, with breakdown of the BBB and impairment of amyloid clearance. The pathogenic chain of these and other deleterious effects, in a vicious circle, finally produces either structural cerebral disintegration (lacunes, infarcts, WMLs) with compromised neuronal metabolism, mitochondrial deficiency, oxidative stress, protein degradation, failure promoting cytoskeletal lesions with deposition of Aβ, and formation of neuritic lesions (e.g., neurofibrillary tangles). These factors induce brain atrophy with cognitive and memory impairment (Figure 1) [147], although the complex cascade of these and other noxious factors needs further elucidation.
Figure 1.
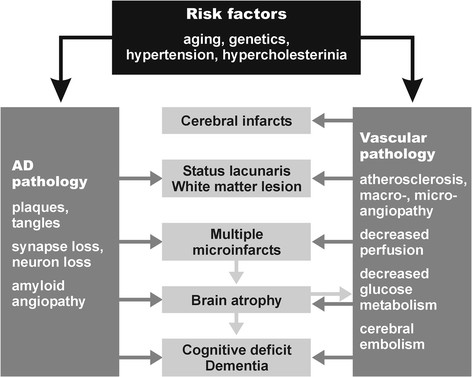
Pathogenic factors for the development of mixed dementia. Modified from [147].
The role of vascular pathology as a factor contributing to AD is a topic of current interest, with a wide overlap between both disorders. Both hypertension and CAA are associated with an increased prevalence of CVLs [157], and both human and experimental studies in transgenic mice overexpressing amyloid precursor protein suggest that cerebrovascular effects of Aβ render the aged brain more vulnerable to ischemic injury [172]. Both atherosclerosis and CAA cause changes in microvasculature auto-regulation and thus may lead to myelin loss, frequently seen in aged and diseased brains, suggesting shared risk factors for all pathological changes seen in AD and CVD. WMLs may be caused by both CVD (hypoperfusion) and AD (retrograde degeneration), they progress with age, and they are a considerable risk factor for cognitive impairment [120],[173],[174]. They impair frontal functions regardless of their location [175],[176] and increase the risk of dementia, particularly in patients with lacunar infarcts [177],[178], causing functional network disruption in cognitively-impaired individuals compared with age-matched healthy elderly controls [179],[180]. Although WMLs and lacunes may be independently associated with cognitive dysfunction [181],[182], WMLs in AD are significantly correlated to cortical and medial temporal lobe atrophy [181]-[183], and, thus, are assumed to contribute to cognitive decline [184]. Together with cortical microinfarcts, WMLs may contribute to the progression of cognitive impairment, but do not necessarily interact with AD pathology to increase the likelihood of dementia beyond their additive effect [20]. Further, the neuropathological evaluation of focal and white matter gliosis may have no clinical validity [185].
Conclusions
CVD has been suggested to be an important cause of cognitive impairment in the elderly, both by itself or as a catalyst for the conversion of low-grade AD to overt dementia [186]. Hence, the combination of both AD and vascular or other pathological processes, as seen in many elderly persons, may coexist in the earlier stages of cognitive decline and may influence its progression and severity, thus representing a major diagnostic challenge not only for clinicians but also for neuropathologists. Despite multiple attempts, there is still a lack of consensus regarding the optimal means of incorporating vascular disease into clinical and neuropathological classification schemes for dementias. Therefore, an integrating rather than a strictly taxonomic approach (instead of discriminating AD, VaD, and other diseases) to elucidate specific pathophysiological mechanisms that contribute to dementia phenotypes and neuropathological causes has been proposed [37].
To improve the diagnostic specificity on the interaction between AD and CVD pathologies, a multivariable and multimodality algorithm is required. While structural MRI results have limited security and specificity, a number of in vivo studies using functional MRI [187] and amyloid and tau PET (e.g., PiB, florbetabin, flutemetamole, etc.) [188]-[190] will enable the identification of AD and CVD patients in clinical and research settings. However, recent evidence comparing PiB-PET with post-mortem or biopsy results raised doubts about this method as representative of Aβ loads in the living brain [191],[192] and PiB-positivity was observed in 55% of non-demented subjects over 80 [193]. The recent development of in vivo amyloid imaging enables further pathological breakdown of SVD into pure forms and mixed dementia based on the absence or presence of amyloid pathology in the brain [194]. Modern CSF biomarkers may support a direct relationship between SVD and AD pathology [195], although in the Alzheimer Disease Neuroimaging Initiative that is focused on AD, no interactions were noted between vascular risk factors and AD biomarkers [26]. Therefore, differentiation of mixed AD/CVD with CSF biomarkers may be difficult. Converging evidence from autopsy, amyloid PET, functional MRI, and CSF biomarker studies indicate that AD and CVD exert additive rather than interactive adverse effects on cognitive health, but interaction between various vascular factors and amyloidosis/tauopathy still remain unresolved. Further studies to more accurately elucidate the impact of vascular disease and AD-related brain pathology are an important challenge for neuroscience as such studies could serve as a basis for the development of efficient therapies against age associated dementias.
Authors’ contributions
KAJ drafted the manuscript and JA critically revised the manuscript. Both authors read and approved the final manuscript.
Acknowledgements
JA is funded by the Dunhill Medical Trust (R173/1110) and by the National Institute for Health Research (NIHR) Biomedical Research Centre for Ageing and Age-related disease and the Biomedical Research Unit for Lewy Body Dementia based at Newcastle upon Tyne Hospitals NHS Foundation Trust and Newcastle University (R:CH/ML/0712). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. Tissue for original work by JA cited in this review was provided by the Newcastle Brain Tissue Resource, which is funded in part by a grant from the UK Medical Research Council (G0400074) and by Brains for Dementia Research, a joint venture between Alzheimer’s Society and Alzheimer’s Research UK.
Abbreviations
- Aβ
β-amyloid
- AD
Alzheimer’s disease
- ApoE
Apolipoprotein E
- BBB
Blood-brain barrier
- CAA
Cerebral amyloid angiopathy
- CCT
Cranial computerized tomography
- CMB
Cerebral microbleed
- CMI
Cortical microinfarcts
- CSF
Cerebrospinal fluid
- CVD
cerebrovascular disease
- CVL
Cerebrovascular lesions
- ICH
Intracerebral hemorrhages
- LVD
Large-vessel disease
- MRI
Magnetic resonance imaging
- NACC
National Alzheimer’s Coordinating Center
- PiB
Pittsburgh compound-B
- PET
Positron emission tomography
- SMA
Smooth muscle actin
- SVD
Small vessel disease
- VaD
Vascular dementia
- WML
White matter lesions
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Contributor Information
Johannes Attems, Email: j.attems@ncl.ac.uk.
Kurt A Jellinger, Email: kurt.jellinger@univie.ac.at.
References
- 1.Petrovitch H, Ross GW, Steinhorn SC, Abbott RD, Markesberry W, Davis DG, Nelson J, Hardman J, Masaki KH, Vogt MR, Launer LJ, White LR. AD lesions and infarcts in demented and no-demented Japanese-American men. Ann Neurol. 2005;57:98–103. doi: 10.1002/ana.20318. [DOI] [PubMed] [Google Scholar]
- 2.Jellinger KA. The enigma of vascular cognitive disorder and vascular dementia. Acta Neuropathol. 2007;113:349–388. doi: 10.1007/s00401-006-0185-2. [DOI] [PubMed] [Google Scholar]
- 3.Jellinger KA. The enigma of mixed dementia. Alzheimers Dement. 2007;3:40–53. doi: 10.1016/j.jalz.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Schneider JA, Arvanitakis Z, Bang W, Bennett DA. Mixed brain pathologies account for most dementia cases in community-dwelling older persons. Neurology. 2007;69:2197–2204. doi: 10.1212/01.wnl.0000271090.28148.24. [DOI] [PubMed] [Google Scholar]
- 5.Toledo JB, Arnold SE, Raible K, Brettschneider J, Xie SX, Grossman M, Monsell SE, Kukull WA, Trojanowski JQ. Contribution of cerebrovascular disease in autopsy confirmed neurodegenerative disease cases in the National Alzheimer’s Coordinating Centre. Brain. 2013;136:2697–2706. doi: 10.1093/brain/awt188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chui HC, Zarow C, Mack WJ, Ellis WG, Zheng L, Jagust WJ, Mungas D, Reed BR, Kramer JH, Decarli CC, Weiner MW, Vinters HV. Cognitive impact of subcortical vascular and Alzheimer’s disease pathology. Ann Neurol. 2006;60:677–687. doi: 10.1002/ana.21009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giannakopoulos P, Gold G, Kovari E, von Gunten A, Imhof A, Bouras C, Hof PR. Assessing the cognitive impact of Alzheimer disease pathology and vascular burden in the aging brain: the Geneva experience. Acta Neuropathol. 2007;113:1–12. doi: 10.1007/s00401-006-0144-y. [DOI] [PubMed] [Google Scholar]
- 8.Esiri MM, Joachim C, Sloan C, Christie S, Agacinski G, Bridges LR, Wilcock GK, Smith AD. Cerebral subcortical small vessel disease in subjects with pathologically confirmed Alzheimer disease: a clinicopathologic study in the Oxford Project to Investigate Memory and Ageing (OPTIMA) Alzheimer Dis Assoc Disord. 2014;28:30–35. doi: 10.1097/WAD.0b013e31829b72f1. [DOI] [PubMed] [Google Scholar]
- 9.Snowdon DA, Greiner LH, Mortimer JA, Riley KP, Greiner PA, Markesbery WR. Brain infarction and the clinical expression of Alzheimer disease. Nun Study JAMA. 1997;277:813–817. [PubMed] [Google Scholar]
- 10.Schneider JA, Aggarwal NT, Barnes L, Boyle P, Bennett DA. The neuropathology of older persons with and without dementia from community versus clinic cohorts. J Alzheimers Dis. 2009;18:691–701. doi: 10.3233/JAD-2009-1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider JA, Wilson RS, Cochran EJ, Bienias JL, Arnold SE, Evans DA, Bennett DA. Relation of cerebral infarctions to dementia and cognitive function in older persons. Neurology. 2003;60:1082–1088. doi: 10.1212/01.WNL.0000055863.87435.B2. [DOI] [PubMed] [Google Scholar]
- 12.Jellinger KA. Prevalence and impact of cerebrovascular lesions in Alzheimer and Lewy body diseases. Neurodegener Dis. 2010;7:112–115. doi: 10.1159/000285518. [DOI] [PubMed] [Google Scholar]
- 13.Esiri MM, Nagy Z, Smith MZ, Barnetson L, Smith AD. Cerebrovascular disease and threshold for dementia in the early stages of Alzheimer’s disease. Lancet. 1999;354:919–920. doi: 10.1016/S0140-6736(99)02355-7. [DOI] [PubMed] [Google Scholar]
- 14.Sonnen JA, Larson EB, Crane PK, Haneuse S, Li G, Schellenberg GD, Craft S, Leverenz JB, Montine TJ. Pathological correlates of dementia in a longitudinal, population-based sample of aging. Ann Neurol. 2007;62:406–413. doi: 10.1002/ana.21208. [DOI] [PubMed] [Google Scholar]
- 15.Troncoso JC, Zonderman AB, Resnick SM, Crain B, Pletnikova O, O’Brien RJ. Effect of infarcts on dementia in the Baltimore longitudinal study of aging. Ann Neurol. 2008;64:168–176. doi: 10.1002/ana.21413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, Launer LJ, Laurent S, Lopez OL, Nyenhuis D, Petersen RC, Schneider JA, Tzourio C, Arnett DK, Bennett DA, Chui HC, Higashida RT, Lindquist R, Nilsson PM, Roman GC, Sellke FW, Seshadri S. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2672–2713. doi: 10.1161/STR.0b013e3182299496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jellinger KA. Alzheimer disease and cerebrovascular pathology: an update. J Neural Transm. 2002;109:813–836. doi: 10.1007/s007020200068. [DOI] [PubMed] [Google Scholar]
- 18.Strozyk D, Dickson DW, Lipton RB, Katz M, Derby CA, Lee S, Wang C, Verghese J. Contribution of vascular pathology to the clinical expression of dementia. Neurobiol Aging. 2010;31:1710–1720. doi: 10.1016/j.neurobiolaging.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Launer LJ, Petrovitch H, Ross GW, Markesbery W, White LR. AD brain pathology: vascular origins? Results from the HAAS autopsy study. Neurobiol Aging. 2008;29:1587–1590. doi: 10.1016/j.neurobiolaging.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Costanza A, Xekardaki A, Kovari E, Gold G, Bouras C, Giannakopoulos P. Microvascular burden and Alzheimer-type lesions across the age spectrum. J Alzheimers Dis. 2012;32:643–652. doi: 10.3233/JAD-2012-120835. [DOI] [PubMed] [Google Scholar]
- 21.Esiri MM, Chance SA. Cognitive reserve, cortical plasticity and resistance to Alzheimer’s disease. Alzheimers Res Ther. 2012;4:7. doi: 10.1186/alzrt105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalaria RN. The role of cerebral ischemia in Alzheimer’s disease. Neurobiol Aging. 2000;21:321–330. doi: 10.1016/S0197-4580(00)00125-1. [DOI] [PubMed] [Google Scholar]
- 23.Zekry D, Duyckaerts C, Moulias R, Belmin J, Geoffre C, Herrmann F, Hauw JJ. Degenerative and vascular lesions of the brain have synergistic effects in dementia of the elderly. Acta Neuropathol (Berl) 2002;103:481–487. doi: 10.1007/s00401-001-0493-5. [DOI] [PubMed] [Google Scholar]
- 24.Kalaria RN. Risk factors and neurodegenerative mechanisms in stroke related dementia. Panminerva Med. 2012;54:139–148. [PubMed] [Google Scholar]
- 25.Bennett DA, Wilson RS, Boyle PA, Buchman AS, Schneider JA. Relation of neuropathology to cognition in persons without cognitive impairment. Ann Neurol. 2012;72:599–609. doi: 10.1002/ana.23654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lo RY, Jagust WJ. Vascular burden and Alzheimer disease pathologic progression. Neurology. 2012;79:1349–1355. doi: 10.1212/WNL.0b013e31826c1b9d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Brien TJ, Wadley V, Nicholas AP, Stover NP, Watts R, Griffith HR. The contribution of executive control on verbal-learning impairment in patients with Parkinson’s disease with dementia and Alzheimer’s disease. Arch Clin Neuropsychol. 2009;24:237–244. doi: 10.1093/arclin/acp029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snyder HM, Corriveau RA, Craft S, Faber JE, Greenberg S, Knopman D, Lamb BT, Montine TJ, Nedergaard M, Schaffer CB, Schneider JA, Wellington C, Wilcock DM, Zipfel GJ, Zlokovic B, Bain LS, Bosetti F, Galis ZS, Koroshetz W, Carrillo MC: Vascular contributions to cognitive impairment and dementia including Alzheimer’s disease.Alzheimers Dement 2015. In press.. [DOI] [PMC free article] [PubMed]
- 29.Stephan BC, Matthews FE, Ma B, Muniz G, Hunter S, Davis D, McKeith IG, Foster G, Ince PG, Brayne C. Alzheimer and vascular neuropathological changes associated with different cognitive States in a non-demented sample. J Alzheimers Dis. 2012;29:309–318. doi: 10.3233/JAD-2011-110518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Casserly I, Topol E. Convergence of atherosclerosis and Alzheimer’s disease: inflammation, cholesterol, and misfolded proteins. Lancet. 2004;363:1139–1146. doi: 10.1016/S0140-6736(04)15900-X. [DOI] [PubMed] [Google Scholar]
- 31.Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jellinger KA. Morphologic diagnosis of “vascular dementia” - a critical update. J Neurol Sci. 2008;270:1–12. doi: 10.1016/j.jns.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 33.Meng X-F, Yu J-T, Wang H-F, Tan M-S, Wang C, Tan C-C, Tan L: Midlife vascular risk factors and the risk of Alzheimer's disease: a systematic review and meta-analysis.J Alzheimers Dis 2014. in print: doi:10.3233/JAD-140954.. [DOI] [PubMed]
- 34.Elias MF, Sullivan LM, D’Agostino RB, Elias PK, Jacques PF, Selhub J, Seshadri S, Au R, Beiser A, Wolf PA. Homocysteine and cognitive performance in the Framingham offspring study: age is important. Am J Epidemiol. 2005;162:644–653. doi: 10.1093/aje/kwi259. [DOI] [PubMed] [Google Scholar]
- 35.Toledo JB, Toledo E, Weiner MW, Jack CR, Jr, Jagust W, Lee VM, Shaw LM, Trojanowski JQ. Cardiovascular risk factors, cortisol, and amyloid-beta deposition in Alzheimer’s Disease Neuroimaging Initiative. Alzheimers Dement. 2012;8:483–489. doi: 10.1016/j.jalz.2011.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Polidori MC, Pientka L, Mecocci P. A review of the major vascular risk factors related to Alzheimer’s disease. J Alzheimers Dis. 2012;32:521–530. doi: 10.3233/JAD-2012-120871. [DOI] [PubMed] [Google Scholar]
- 37.Kling MA, Trojanowski JQ, Wolk DA, Lee VM, Arnold SE. Vascular disease and dementias: paradigm shifts to drive research in new directions. Alzheimers Dement. 2013;9:76–92. doi: 10.1016/j.jalz.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ahtiluoto S, Polvikoski T, Peltonen M, Solomon A, Tuomilehto J, Winblad B, Sulkava R, Kivipelto M. Diabetes, Alzheimer disease, and vascular dementia: a population-based neuropathologic study. Neurology. 2010;75:1195–1202. doi: 10.1212/WNL.0b013e3181f4d7f8. [DOI] [PubMed] [Google Scholar]
- 39.Helzner EP, Luchsinger JA, Scarmeas N, Cosentino S, Brickman AM, Glymour MM, Stern Y. Contribution of vascular risk factors to the progression in Alzheimer disease. Arch Neurol. 2009;66:343–348. doi: 10.1001/archneur.66.3.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kivipelto M, Ngandu T, Laatikainen T, Winblad B, Soininen H, Tuomilehto J. Risk score for the prediction of dementia risk in 20 years among middle aged people: a longitudinal, population-based study. Lancet Neurol. 2006;5:735–741. doi: 10.1016/S1474-4422(06)70537-3. [DOI] [PubMed] [Google Scholar]
- 41.Mielke MM, Rosenberg PB, Tschanz J, Cook L, Corcoran C, Hayden KM, Norton M, Rabins PV, Green RC, Welsh-Bohmer KA, Breitner JC, Munger R, Lyketsos CG. Vascular factors predict rate of progression in Alzheimer disease. Neurology. 2007;69:1850–1858. doi: 10.1212/01.wnl.0000279520.59792.fe. [DOI] [PubMed] [Google Scholar]
- 42.Qiu C, Xu W, Winblad B, Fratiglioni L. Vascular risk profiles for dementia and Alzheimer’s disease in very old people: a population-based longitudinal study. J Alzheimers Dis. 2010;20:293–300. doi: 10.3233/JAD-2010-1361. [DOI] [PubMed] [Google Scholar]
- 43.Richardson K, Stephan BC, Ince PG, Brayne C, Matthews FE, Esiri MM. The neuropathology of vascular disease in the Medical Research Council Cognitive Function and Ageing Study (MRC CFAS) Curr Alzheimer Res. 2012;9:687–696. doi: 10.2174/156720512801322654. [DOI] [PubMed] [Google Scholar]
- 44.Eriksson UK, Bennet AM, Gatz M, Dickman PW, Pedersen NL. Nonstroke cardiovascular disease and risk of Alzheimer disease and dementia. Alzheimer Dis Assoc Disord. 2010;24:213–219. doi: 10.1097/WAD.0b013e3181d1b99b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jellinger KA. Small concomitant cerebrovascular lesions are not important for cognitive decline in severe Alzheimer disease. Arch Neurol. 2001;58:520–521. doi: 10.1001/archneur.58.3.520. [DOI] [PubMed] [Google Scholar]
- 46.Mungas D, Jagust WJ, Reed BR, Kramer JH, Weiner MW, Schuff N, Norman D, Mack WJ, Willis L, Chui HC. MRI predictors of cognition in subcortical ischemic vascular disease and Alzheimer’s disease. Neurology. 2001;57:2229–2235. doi: 10.1212/WNL.57.12.2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jellinger KA, Attems J. Prevalence and pathology of vascular dementia in the oldest-old. J Alzheimers Dis. 2010;21:1283–1293. doi: 10.3233/jad-2010-100603. [DOI] [PubMed] [Google Scholar]
- 48.Rincon F, Wright CB. Current pathophysiological concepts in cerebral small vessel disease. Front Aging Neurosci. 2014;6:24. doi: 10.3389/fnagi.2014.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Goulding JM, Signorini DF, Chatterjee S, Nicoll JA, Stewart J, Morris R, Lammie GA. Inverse relation between Braak stage and cerebrovascular pathology in Alzheimer predominant dementia. J Neurol Neurosurg Psychiatry. 1999;67:654–657. doi: 10.1136/jnnp.67.5.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arvanitakis Z, Leurgans SE, Barnes LL, Bennett DA, Schneider JA. Microinfarct pathology, dementia, and cognitive systems. Stroke. 2011;42:722–727. doi: 10.1161/STROKEAHA.110.595082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bennett DA, Wilson RS, Arvanitakis Z, Boyle PA, de Toledo-Morrell L, Schneider JA. Selected findings from the religious orders study and rush memory and aging project. J Alzheimers Dis. 2013;33:S397–S403. doi: 10.3233/JAD-2012-129007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Crystal H, Dickson D. Cerebral infarcts in patients with autopsy proven Alzheimer’s disease. Neurobiol Aging. 2002;23:207. [Google Scholar]
- 53.Esiri MM, Wilcock GK, Morris JH. Neuropathological assessment of the lesions of significance in vascular dementia. J Neurol Neurosurg Psychiatry. 1997;63:749–753. doi: 10.1136/jnnp.63.6.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee JH, Olichney JM, Hansen LA, Hofstetter CR, Thal LJ. Small concomitant vascular lesions do not influence rates of cognitive decline in patients with Alzheimer disease. Arch Neurol. 2000;57:1474–1479. doi: 10.1001/archneur.57.10.1474. [DOI] [PubMed] [Google Scholar]
- 55.Smallwood A, Oulhaj A, Joachim C, Christie S, Sloan C, Smith AD, Esiri M. Cerebral subcortical small vessel disease and its relation to cognition in elderly subjects: a pathological study in the Oxford Project to Investigate Memory and Ageing (OPTIMA) cohort. Neuropathol Appl Neurobiol. 2012;38:337–343. doi: 10.1111/j.1365-2990.2011.01221.x. [DOI] [PubMed] [Google Scholar]
- 56.Kalaria RN. Advances in molecular genetics and pathology of cerebrovascular disorders. Trends Neurosci. 2001;24:392–400. doi: 10.1016/S0166-2236(00)01836-1. [DOI] [PubMed] [Google Scholar]
- 57.Zipser BD, Johanson CE, Gonzalez L, Berzin TM, Tavares R, Hulette CM, Vitek MP, Hovanesian V, Stopa EG. Microvascular injury and blood-brain barrier leakage in Alzheimer’s disease. Neurobiol Aging. 2007;28:977–986. doi: 10.1016/j.neurobiolaging.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 58.Nagata K, Takano D, Yamazaki T, Maeda T, Satoh Y, Nakase T, Ikeda Y. Cerebrovascular lesions in elderly Japanese patients with Alzheimer’s disease. J Neurol Sci. 2012;322:87–91. doi: 10.1016/j.jns.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 59.Launer LJ, Hughes TM, White LR. Microinfarcts, brain atrophy, and cognitive function: the Honolulu Asia Aging Study Autopsy Study. Ann Neurol. 2011;70:774–780. doi: 10.1002/ana.22520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sinka L, Kovari E, Gold G, Hof PR, Herrmann FR, Bouras C, Giannakopoulos P. Small vascular and Alzheimer disease-related pathologic determinants of dementia in the oldest-old. J Neuropathol Exp Neurol. 2010;69:1247–1255. doi: 10.1097/NEN.0b013e3181ffc3b9. [DOI] [PubMed] [Google Scholar]
- 61.Utter S, Tamboli IY, Walter J, Upadhaya AR, Birkenmeier G, Pietrzik CU, Ghebremedhin E, Thal DR. Cerebral small vessel disease-induced apolipoprotein E leakage is associated with Alzheimer disease and the accumulation of amyloid beta-protein in perivascular astrocytes. J Neuropathol Exp Neurol. 2008;67:842–856. doi: 10.1097/NEN.0b013e3181836a71. [DOI] [PubMed] [Google Scholar]
- 62.Garcia-Alloza M, Gregory J, Kuchibhotla KV, Fine S, Wei Y, Ayata C, Frosch MP, Greenberg SM, Bacskai BJ. Cerebrovascular lesions induce transient beta-amyloid deposition. Brain. 2011;134:3697–3707. doi: 10.1093/brain/awr300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee CW, Shih YH, Kuo YM. Cerebrovascular pathology and amyloid plaque formation in Alzheimer’s disease. Curr Alzheimer Res. 2013;11:4–10. doi: 10.2174/1567205010666131119234308. [DOI] [PubMed] [Google Scholar]
- 64.Hawkes CA, Sullivan PM, Hands S, Weller RO, Nicoll JA, Carare RO. Disruption of arterial perivascular drainage of amyloid-beta from the brains of mice expressing the human APOE epsilon4 allele. PLoS One. 2012;7:e41636. doi: 10.1371/journal.pone.0041636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hawkes CA, Carare RO, Weller RO. Amyloid and tau in the brain in sporadic Alzheimer’s disease: defining the chicken and the egg. Acta Neuropathol. 2014;127:617–618. doi: 10.1007/s00401-014-1243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lewis H, Beher D, Cookson N, Oakley A, Piggott M, Morris CM, Jaros E, Perry R, Ince P, Kenny RA, Ballard CG, Shearman MS, Kalaria RN. Quantification of Alzheimer pathology in ageing and dementia: age-related accumulation of amyloid-beta(42) peptide in vascular dementia. Neuropathol Appl Neurobiol. 2006;32:103–118. doi: 10.1111/j.1365-2990.2006.00696.x. [DOI] [PubMed] [Google Scholar]
- 67.Hulette CM, Ervin JF, Edmonds Y, Antoine S, Stewart N, Szymanski MH, Hayden KM, Pieper CF, Burke JR, Welsh-Bohmer KA. Cerebrovascular smooth muscle actin is increased in nondemented subjects with frequent senile plaques at autopsy: implications for the pathogenesis of Alzheimer disease. J Neuropathol Exp Neurol. 2009;68:417–424. doi: 10.1097/NEN.0b013e31819e6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.de la Torre JC. Alzheimer disease as a vascular disorder: nosological evidence. Stroke. 2002;33:1152–1162. doi: 10.1161/01.STR.0000014421.15948.67. [DOI] [PubMed] [Google Scholar]
- 69.Shi J, Perry G, Smith MA, Friedland RP. Vascular abnormalities: the insidious pathogenesis of Alzheimer’s disease. Neurobiol Aging. 2000;21:357–361. doi: 10.1016/S0197-4580(00)00119-6. [DOI] [PubMed] [Google Scholar]
- 70.de la Torre JC, Stefano GB. Evidence that Alzheimer’s disease is a microvascular disorder: the role of constitutive nitric oxide. Brain Res Brain Res Rev. 2000;34:119–136. doi: 10.1016/S0165-0173(00)00043-6. [DOI] [PubMed] [Google Scholar]
- 71.Kudo T, Imaizumi K, Tanimukai H, Katayama T, Sato N, Nakamura Y, Tanaka T, Kashiwagi Y, Jinno Y, Tohyama M, Takeda M. Are cerebrovascular factors involved in Alzheimer’s disease? Neurobiol Aging. 2000;21:215–224. doi: 10.1016/S0197-4580(00)00129-9. [DOI] [PubMed] [Google Scholar]
- 72.Schmidt R, Schmidt H, Fazekas F. Vascular risk factors in dementia. J Neurol. 2000;247:81–87. doi: 10.1007/s004150050021. [DOI] [PubMed] [Google Scholar]
- 73.Farkas E, Luiten PG. Cerebral microvascular pathology in aging and Alzheimer’s disease. Prog Neurobiol. 2001;64:575–611. doi: 10.1016/S0301-0082(00)00068-X. [DOI] [PubMed] [Google Scholar]
- 74.Brown WR, Moody DM, Challa VR, Thore CR. Cerebrovascular pathology in Alzheimer disease. In: Vellas B, Fitten LJ, Winblad B, Feldman H, Grundman M, Giacobini E, editors. Research and Practice in Alzheimer’s Disease. Springer, Paris, New York: Serdi Publications; 2001. pp. 76–81. [Google Scholar]
- 75.Miklossy J. Cerebral hypoperfusion induces cortical watershed microinfarcts which may further aggravate cognitive decline in Alzheimer’s disease. Neurol Res. 2003;25:605–610. doi: 10.1179/016164103101202048. [DOI] [PubMed] [Google Scholar]
- 76.Bennett DA, Schneider JA, Bienias JL, Evans DA, Wilson RS. Mild cognitive impairment is related to Alzheimer disease pathology and cerebral infarctions. Neurology. 2005;64:834–841. doi: 10.1212/01.WNL.0000152982.47274.9E. [DOI] [PubMed] [Google Scholar]
- 77.Gold G, Giannakopoulos P, Herrmann FR, Bouras C, Kovari E. Identification of Alzheimer and vascular lesion thresholds for mixed dementia. Brain. 2007;130:2830–2836. doi: 10.1093/brain/awm228. [DOI] [PubMed] [Google Scholar]
- 78.Zekry D, Duyckaerts C, Belmin J, Geoffre C, Herrmann F, Moulias R, Hauw JJ. The vascular lesions in vascular and mixed dementia: the weight of functional neuroanatomy. Neurobiol Aging. 2003;24:213–219. doi: 10.1016/S0197-4580(02)00066-0. [DOI] [PubMed] [Google Scholar]
- 79.Nelson PT, Jicha GA, Schmitt FA, Liu H, Davis DG, Mendiondo MS, Abner EL, Markesbery WR. Clinicopathologic correlations in a large Alzheimer disease center autopsy cohort: neuritic plaques and neurofibrillary tangles “do count” when staging disease severity. J Neuropathol Exp Neurol. 2007;66:1136–1146. doi: 10.1097/nen.0b013e31815c5efb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nelson PT, Pious NM, Jicha GA, Wilcock DM, Fardo DW, Estus S, Rebeck GW. APOE-epsilon2 and APOE-epsilon4 correlate with increased amyloid accumulation in cerebral vasculature. J Neuropathol Exp Neurol. 2013;72:708–715. doi: 10.1097/NEN.0b013e31829a25b9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Iadecola C. The overlap between neurodegenerative and vascular factors in the pathogenesis of dementia. Acta Neuropathol. 2010;120:287–296. doi: 10.1007/s00401-010-0718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Heyman A, Fillenbaum G, Welsh-Bohmer K, Gearing M, Mirra SS, Mohs RC, Peterson BL, Pieper CF. Cerebral infarcts in patients with autopsy-proven Alzheimer’s disease, CERAD, Part XVIII. Neurology. 1998;51:159–162. doi: 10.1212/WNL.51.1.159. [DOI] [PubMed] [Google Scholar]
- 83.Riekse RG, Leverenz JB, McCormick W, Bowen JD, Teri L, Nochlin D, Simpson K, Eugenio C, Larson EB, Tsuang D. Effect of vascular lesions on cognition in Alzheimer’s disease: a community-based study. J Am Geriatr Soc. 2004;52:1442–1448. doi: 10.1111/j.1532-5415.2004.52405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zlokovic BV. Neurovascular mechanisms of Alzheimer’s neurodegeneration. Trends Neurosci. 2005;28:202–208. doi: 10.1016/j.tins.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 85.Zlokovic BV. Neurovascular pathways to neurodegeneration in Alzheimer’s disease and other disorders. Nat Rev Neurosci. 2011;12:723–738. doi: 10.1038/nrn3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Du AT, Schuff N, Chao LL, Kornak J, Ezekiel F, Jagust WJ, Kramer JH, Reed BR, Miller BL, Norman D, Chui HC, Weiner MW. White matter lesions are associated with cortical atrophy more than entorhinal and hippocampal atrophy. Neurobiol Aging. 2005;26:553–559. doi: 10.1016/j.neurobiolaging.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 87.Grinberg LT, Thal DR. Vascular pathology in the aged human brain. Acta Neuropathol. 2010;119:277–290. doi: 10.1007/s00401-010-0652-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Attems J, Yamaguchi H, Saido TC, Thal DR. Capillary CAA and perivascular Abeta-deposition: two distinct features of Alzheimer’s disease pathology. J Neurol Sci. 2010;299:155–162. doi: 10.1016/j.jns.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 89.Attems J, Jellinger K, Thal DR, Van Nostrand W. Review: sporadic cerebral amyloid angiopathy. Neuropathol Appl Neurobiol. 2011;37:75–93. doi: 10.1111/j.1365-2990.2010.01137.x. [DOI] [PubMed] [Google Scholar]
- 90.Attems J, Jellinger KA, Lintner F. Alzheimer’s disease pathology influences severity and topographical distribution of cerebral amyloid angiopathy. Acta Neuropathol (Berl) 2005;110:222–231. doi: 10.1007/s00401-005-1064-y. [DOI] [PubMed] [Google Scholar]
- 91.Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, Launer LJ, Van Buchem MA, Breteler MM. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009;8:165–174. doi: 10.1016/S1474-4422(09)70013-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Pezzini A, Del Zotto E, Volonghi I, Giossi A, Costa P, Padovani A. Cerebral amyloid angiopathy: a common cause of cerebral hemorrhage. Curr Med Chem. 2009;16:2498–2513. doi: 10.2174/092986709788682047. [DOI] [PubMed] [Google Scholar]
- 93.Jellinger KA, Lauda F, Attems J. Sporadic cerebral amyloid angiopathy is not a frequent cause of spontaneous brain hemorrhage. Eur J Neurol. 2007;14:923–928. doi: 10.1111/j.1468-1331.2007.01880.x. [DOI] [PubMed] [Google Scholar]
- 94.Attems J, Lauda F, Jellinger KA. Unexpectedly low prevalence of intracerebral hemorrhages in sporadic cerebral amyloid angiopathy: an autopsy study. J Neurol. 2008;255:70–76. doi: 10.1007/s00415-008-0674-4. [DOI] [PubMed] [Google Scholar]
- 95.Arima H, Tzourio C, Anderson C, Woodward M, Bousser MG, MacMahon S, Neal B, Chalmers J. Effects of perindopril-based lowering of blood pressure on intracerebral hemorrhage related to amyloid angiopathy: the PROGRESS trial. Stroke. 2010;41:394–396. doi: 10.1161/STROKEAHA.109.563932. [DOI] [PubMed] [Google Scholar]
- 96.Gregoire SM, Charidimou A, Gadapa N, Dolan E, Antoun N, Peeters A, Vandermeeren Y, Laloux P, Baron JC, Jager HR, Werring DJ. Acute ischaemic brain lesions in intracerebral haemorrhage: multicentre cross-sectional magnetic resonance imaging study. Brain. 2011;134:2376–2386. doi: 10.1093/brain/awr172. [DOI] [PubMed] [Google Scholar]
- 97.Chen YW, Gurol ME, Rosand J, Viswanathan A, Rakich SM, Groover TR, Greenberg SM, Smith EE. Progression of white matter lesions and hemorrhages in cerebral amyloid angiopathy. Neurology. 2006;67:83–87. doi: 10.1212/01.wnl.0000223613.57229.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Okamoto Y, Ihara M, Fujita Y, Ito H, Takahashi R, Tomimoto H. Cortical microinfarcts in Alzheimer’s disease and subcortical vascular dementia. Neuroreport. 2009;20:990–996. doi: 10.1097/WNR.0b013e32832d2e6a. [DOI] [PubMed] [Google Scholar]
- 99.Soontornniyomkij V, Lynch MD, Mermash S, Pomakian J, Badkoobehi H, Clare R, Vinters HV. Cerebral microinfarcts associated with severe cerebral beta-amyloid angiopathy. Brain Pathol. 2010;20:459–467. doi: 10.1111/j.1750-3639.2009.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kovari E, Herrmann FR, Hof PR, Bouras C. The relationship between cerebral amyloid angiopathy and cortical microinfarcts in brain ageing and Alzheimer’s disease. Neuropathol Appl Neurobiol. 2013;39:498–509. doi: 10.1111/nan.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Matthews FE, Jagger C, Miller LL, Brayne C. Education differences in life expectancy with cognitive impairment. J Gerontol A Biol Sci Med Sci. 2009;64:125–131. doi: 10.1093/gerona/gln003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Charidimou A, Peeters AP, Jager R, Fox Z, Vandermeeren Y, Laloux P, Baron JC, Werring DJ. Cortical superficial siderosis and intracerebral hemorrhage risk in cerebral amyloid angiopathy. Neurology. 2013;81:1666–1673. doi: 10.1212/01.wnl.0000435298.80023.7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Charidimou A, Jager RH, Fox Z, Peeters A, Vandermeeren Y, Laloux P, Baron JC, Werring DJ. Prevalence and mechanisms of cortical superficial siderosis in cerebral amyloid angiopathy. Neurology. 2013;81:626–632. doi: 10.1212/WNL.0b013e3182a08f2c. [DOI] [PubMed] [Google Scholar]
- 104.Charidimou A, Meegahage R, Fox Z, Peeters A, Vandermeeren Y, Laloux P, Baron JC, Jager HR, Werring DJ. Enlarged perivascular spaces as a marker of underlying arteriopathy in intracerebral haemorrhage: a multicentre MRI cohort study. J Neurol Neurosurg Psychiatry. 2013;84:624–629. doi: 10.1136/jnnp-2012-304434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Knudsen KA, Rosand J, Karluk D, Greenberg SM. Clinical diagnosis of cerebral amyloid angiopathy: validation of the Boston criteria. Neurology. 2001;56:537–539. doi: 10.1212/WNL.56.4.537. [DOI] [PubMed] [Google Scholar]
- 106.Gurol ME, Greenberg SM. A physiologic biomarker for cerebral amyloid angiopathy. Neurology. 2013;81:1650–1651. doi: 10.1212/01.wnl.0000435303.10519.15. [DOI] [PubMed] [Google Scholar]
- 107.Linn J, Halpin A, Demaerel P, Ruhland J, Giese AD, Dichgans M, van Buchem MA, Bruckmann H, Greenberg SM. Prevalence of superficial siderosis in patients with cerebral amyloid angiopathy. Neurology. 2010;74:1346–1350. doi: 10.1212/WNL.0b013e3181dad605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Schrag M, McAuley G, Pomakian J, Jiffry A, Tung S, Mueller C, Vinters HV, Haacke EM, Holshouser B, Kido D, Kirsch WM. Correlation of hypointensities in susceptibility-weighted images to tissue histology in dementia patients with cerebral amyloid angiopathy: a postmortem MRI study. Acta Neuropathol. 2010;119:291–302. doi: 10.1007/s00401-009-0615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Viswanathan A, Greenberg SM. Cerebral amyloid angiopathy in the elderly. Ann Neurol. 2011;70:871–880. doi: 10.1002/ana.22516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Johnson KA, Gregas M, Becker JA, Kinnecom C, Salat DH, Moran EK, Smith EE, Rosand J, Rentz DM, Klunk WE, Mathis CA, Price JC, Dekosky ST, Fischman AJ, Greenberg SM. Imaging of amyloid burden and distribution in cerebral amyloid angiopathy. Ann Neurol. 2007;62:229–234. doi: 10.1002/ana.21164. [DOI] [PubMed] [Google Scholar]
- 111.Greenberg SM, Grabowski T, Gurol ME, Skehan ME, Nandigam RN, Becker JA, Garcia-Alloza M, Prada C, Frosch MP, Rosand J, Viswanathan A, Smith EE, Johnson KA. Detection of isolated cerebrovascular beta-amyloid with Pittsburgh compound B. Ann Neurol. 2008;64:587–591. doi: 10.1002/ana.21528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Renard D, Castelnovo G, Wacongne A, Le Floch A, Thouvenot E, Mas J, Gabelle A, Labauge P, Lehmann S. Interest of CSF biomarker analysis in possible cerebral amyloid angiopathy cases defined by the modified Boston criteria. J Neurol. 2012;259:2429–2433. doi: 10.1007/s00415-012-6520-8. [DOI] [PubMed] [Google Scholar]
- 113.Verbeek MM, Kremer BP, Rikkert MO, Van Domburg PH, Skehan ME, Greenberg SM. Cerebrospinal fluid amyloid beta(40) is decreased in cerebral amyloid angiopathy. Ann Neurol. 2009;66:245–249. doi: 10.1002/ana.21694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.de Jong D, Kremer BP, Olde Rikkert MG, Verbeek MM. Current state and future directions of neurochemical biomarkers for Alzheimer’s disease. Clin Chem Lab Med. 2007;45:1421–1434. doi: 10.1515/CCLM.2007.320. [DOI] [PubMed] [Google Scholar]
- 115.Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9:689–701. doi: 10.1016/S1474-4422(10)70104-6. [DOI] [PubMed] [Google Scholar]
- 116.Thal DR, Ghebremedhin E, Orantes M, Wiestler OD. Vascular pathology in Alzheimer disease: correlation of cerebral amyloid angiopathy and arteriosclerosis/lipohyalinosis with cognitive decline. J Neuropathol Exp Neurol. 2003;62:1287–1301. doi: 10.1093/jnen/62.12.1287. [DOI] [PubMed] [Google Scholar]
- 117.Ortner M, Kurz A, Alexopoulos P, Auer F, Diehl-Schmid J, Drzezga A, Forster S, Forstl H, Perneczky R, Sorg C, Yousefi BH, Grimmer T: Small vessel disease, but neither amyloid load nor metabolic deficit, is dependent on age at onset in Alzheimer’s Disease.Biol Psychiatry 2014. In press.. [DOI] [PubMed]
- 118.Doubal FN, MacLullich AM, Ferguson KJ, Dennis MS, Wardlaw JM. Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke. 2010;41:450–454. doi: 10.1161/STROKEAHA.109.564914. [DOI] [PubMed] [Google Scholar]
- 119.Duering M, Csanadi E, Gesierich B, Jouvent E, Herve D, Seiler S, Belaroussi B, Ropele S, Schmidt R, Chabriat H, Dichgans M. Incident lacunes preferentially localize to the edge of white matter hyperintensities: insights into the pathophysiology of cerebral small vessel disease. Brain. 2013;136:2717–2726. doi: 10.1093/brain/awt184. [DOI] [PubMed] [Google Scholar]
- 120.Schmidt R, Schmidt H, Haybaeck J, Loitfelder M, Weis S, Cavalieri M, Seiler S, Enzinger C, Ropele S, Erkinjuntti T, Pantoni L, Scheltens P, Fazekas F, Jellinger K. Heterogeneity in age-related white matter changes. Acta Neuropathol. 2011;122:171–185. doi: 10.1007/s00401-011-0851-x. [DOI] [PubMed] [Google Scholar]
- 121.Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, Lindley RI, O’Brien JT, Barkhof F, Benavente OR, Black SE, Brayne C, Breteler M, Chabriat H, Decarli C, de Leeuw FE, Doubal F, Duering M, Fox NC, Greenberg S, Hachinski V, Kilimann I, Mok V, Oostenbrugge R, Pantoni L, Speck O, Stephan BC, Teipel S, Viswanathan A, Werring D, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013;12:822–838. doi: 10.1016/S1474-4422(13)70124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cordonnier C, van der Flier WM. Brain microbleeds and Alzheimer’s disease: innocent observation or key player? Brain. 2011;134:335–344. doi: 10.1093/brain/awq321. [DOI] [PubMed] [Google Scholar]
- 123.Park JH, Seo SW, Kim C, Kim GH, Noh HJ, Kim ST, Kwak KC, Yoon U, Lee JM, Lee JW, Shin JS, Kim CH, Noh Y, Cho H, Kim HJ, Yoon CW, Oh SJ, Kim JS, Choe YS, Lee KH, Lee JH, Ewers M, Weiner MW, Werring DJ, Na DL. Pathogenesis of cerebral microbleeds: In vivo imaging of amyloid and subcortical ischemic small vessel disease in 226 individuals with cognitive impairment. Ann Neurol. 2013;73:584–593. doi: 10.1002/ana.23845. [DOI] [PubMed] [Google Scholar]
- 124.Young VG, Halliday GM, Kril JJ. Neuropathologic correlates of white matter hyperintensities. Neurology. 2008;71:804–811. doi: 10.1212/01.wnl.0000319691.50117.54. [DOI] [PubMed] [Google Scholar]
- 125.Polvikoski TM, van Straaten EC, Barkhof F, Sulkava R, Aronen HJ, Niinisto L, Oinas M, Scheltens P, Erkinjuntti T, Kalaria RN. Frontal lobe white matter hyperintensities and neurofibrillary pathology in the oldest old. Neurology. 2010;75:2071–2078. doi: 10.1212/WNL.0b013e318200d6f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.McAleese KE, Firbank M, Hunter D, Sun L, Hall R, Neal JW, Mann DM, Esiri M, Jellinger KA, O’Brien JT, Attems J. Magnetic resonance imaging of fixed post mortem brains reliably reflects subcortical vascular pathology of frontal, parietal and occipital white matter. Neuropathol Appl Neurobiol. 2013;39:485–497. doi: 10.1111/j.1365-2990.2012.01310.x. [DOI] [PubMed] [Google Scholar]
- 127.Piguet O, Double KL, Kril JJ, Harasty J, Macdonald V, McRitchie DA, Halliday GM. White matter loss in healthy ageing: a postmortem analysis. Neurobiol Aging. 2009;30:1288–1295. doi: 10.1016/j.neurobiolaging.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 128.Bell RD, Zlokovic BV. Neurovascular mechanisms and blood-brain barrier disorder in Alzheimer’s disease. Acta Neuropathol. 2009;118:103–113. doi: 10.1007/s00401-009-0522-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Topakian R, Barrick TR, Howe FA, Markus HS. Blood-brain barrier permeability is increased in normal-appearing white matter in patients with lacunar stroke and leucoaraiosis. J Neurol Neurosurg Psychiatry. 2010;81:192–197. doi: 10.1136/jnnp.2009.172072. [DOI] [PubMed] [Google Scholar]
- 130.Wardlaw JM, Doubal F, Armitage P, Chappell F, Carpenter T, Munoz Maniega S, Farrall A, Sudlow C, Dennis M, Dhillon B. Lacunar stroke is associated with diffuse blood-brain barrier dysfunction. Ann Neurol. 2009;65:194–202. doi: 10.1002/ana.21549. [DOI] [PubMed] [Google Scholar]
- 131.Rosenberg GA. Neurological diseases in relation to the blood-brain barrier. J Cereb Blood Flow Metab. 2012;32:1139–1151. doi: 10.1038/jcbfm.2011.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Viggars AP, Wharton SB, Simpson JE, Matthews FE, Brayne C, Savva GM, Garwood C, Drew D, Shaw PJ, Ince PG. Alterations in the blood brain barrier in ageing cerebral cortex in relationship to Alzheimer-type pathology: a study in the MRC-CFAS population neuropathology cohort. Neurosci Lett. 2011;505:25–30. doi: 10.1016/j.neulet.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 133.Vermeer SE, Longstreth WT, Jr, Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–619. doi: 10.1016/S1474-4422(07)70170-9. [DOI] [PubMed] [Google Scholar]
- 134.Thong JY, Hilal S, Wang Y, Soon HW, Dong Y, Collinson SL, Anh TT, Ikram MK, Wong TY, Venketasubramanian N, Chen C, Qiu A. Association of silent lacunar infarct with brain atrophy and cognitive impairment. J Neurol Neurosurg Psychiatry. 2013;84:1219–1225. doi: 10.1136/jnnp-2013-305310. [DOI] [PubMed] [Google Scholar]
- 135.Thal DR, Griffin WS, de Vos RA, Ghebremedhin E. Cerebral amyloid angiopathy and its relationship to Alzheimer’s disease. Acta Neuropathol. 2008;115:599–609. doi: 10.1007/s00401-008-0366-2. [DOI] [PubMed] [Google Scholar]
- 136.Brundel M, de Bresser J, van Dillen JJ, Kappelle LJ, Biessels GJ. Cerebral microinfarcts: a systematic review of neuropathological studies. J Cereb Blood Flow Metab. 2012;32:425–436. doi: 10.1038/jcbfm.2011.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.van Veluw SJ, Heringa SM, Kuijf HJ, Koek HL, Luijten PR, Biessels GJ. Cerebral cortical microinfarcts at 7 Tesla MRI in patients with early Alzheimer’s disease. J Alzheimers Dis. 2013;39:163–167. doi: 10.3233/JAD-131040. [DOI] [PubMed] [Google Scholar]
- 138.Yarchoan M, Xie SX, Kling MA, Toledo JB, Wolk DA, Lee EB, Van Deerlin V, Lee VM, Trojanowski JQ, Arnold SE. Cerebrovascular atherosclerosis correlates with Alzheimer pathology in neurodegenerative dementias. Brain. 2012;135:3749–3756. doi: 10.1093/brain/aws271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Beach TG, Wilson JR, Sue LI, Newell A, Poston M, Cisneros R, Pandya Y, Esh C, Connor DJ, Sabbagh M, Walker DG, Roher AE. Circle of Willis atherosclerosis: association with Alzheimer’s disease, neuritic plaques and neurofibrillary tangles. Acta Neuropathol. 2007;113:13–21. doi: 10.1007/s00401-006-0136-y. [DOI] [PubMed] [Google Scholar]
- 140.Roher AE, Tyas SL, Maarouf CL, Daugs ID, Kokjohn TA, Emmerling MR, Garami Z, Belohlavek M, Sabbagh MN, Sue LI, Beach TG. Intracranial atherosclerosis as a contributing factor to Alzheimer’s disease dementia. Alzheimers Dement. 2011;7:436–444. doi: 10.1016/j.jalz.2010.08.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Honig LS, Kukull W, Mayeux R. Atherosclerosis and AD: analysis of data from the US National Alzheimer’s Coordinating Center. Neurology. 2005;64:494–500. doi: 10.1212/01.WNL.0000150886.50187.30. [DOI] [PubMed] [Google Scholar]
- 142.Luoto TM, Haikonen S, Haapasalo H, Goebeler S, Huhtala H, Erkinjuntti T, Karhunen PJ. Large vessel cerebral atherosclerosis is not in direct association with neuropathological lesions of Alzheimer’s disease. Eur Neurol. 2009;62:93–98. doi: 10.1159/000222779. [DOI] [PubMed] [Google Scholar]
- 143.Dolan H, Crain B, Troncoso J, Resnick SM, Zonderman AB, O’Brien RJ. Atherosclerosis, dementia, and Alzheimer’s disease in the BLSA cohort. Ann Neurol. 2010;68:231–240. doi: 10.1002/ana.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Iadecola C. The pathobiology of vascular dementia. Neuron. 2013;80:844–866. doi: 10.1016/j.neuron.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Jellinger KA. Challenges in the neuropathological diagnosis of dementias. Int J Neuropathol. 2013;1:8–52. [Google Scholar]
- 146.Jellinger KA: Pathogenesis and treatment of vascular cognitive impairment.Neurodeg Dis Management 2014. In press.. [DOI] [PubMed]
- 147.Jellinger KA, Attems J. Neuropathological evaluation of mixed dementia. J Neurol Sci. 2007;257:80–87. doi: 10.1016/j.jns.2007.01.045. [DOI] [PubMed] [Google Scholar]
- 148.Kalaria RN, Ballard C. Overlap between pathology of Alzheimer disease and vascular dementia. Alzheimer Dis Assoc Disord. 1999;13:S115–S123. doi: 10.1097/00002093-199912003-00017. [DOI] [PubMed] [Google Scholar]
- 149.Olichney JM, Ellis RJ, Katzman R, Sabbagh MN, Hansen L. Types of cerebrovascular lesions associated with severe cerebral amyloid angiopathy in Alzheimer’s disease. Ann N Y Acad Sci. 1997;826:493–497. doi: 10.1111/j.1749-6632.1997.tb48511.x. [DOI] [PubMed] [Google Scholar]
- 150.Jellinger KA, Attems J. Incidence of cerebrovascular lesions in Alzheimer’s disease: a postmortem study. Acta Neuropathol. 2003;105:14–17. doi: 10.1007/s00401-002-0634-5. [DOI] [PubMed] [Google Scholar]
- 151.Knopman DS, Parisi JE, Boeve BF, Cha RH, Apaydin H, Salviati A, Edland SD, Rocca WA. Vascular dementia in a population-based autopsy study. Arch Neurol. 2003;60:569–575. doi: 10.1001/archneur.60.4.569. [DOI] [PubMed] [Google Scholar]
- 152.Fernando MS, Ince PG. Vascular pathologies and cognition in a population-based cohort of elderly people. J Neurol Sci. 2004;226:13–17. doi: 10.1016/j.jns.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 153.Jellinger KA, Mitter-Ferstl E. The impact of cerebrovascular lesions in Alzheimer disease. A comparative autopsy study. J Neurol. 2003;250:1050–1055. doi: 10.1007/s00415-003-0142-0. [DOI] [PubMed] [Google Scholar]
- 154.Brayne C, Richardson K, Matthews FE, Fleming J, Hunter S, Xuereb JH, Paykel E, Mukaetova-Ladinska EB, Huppert FA, O’Sullivan A, Dening T. Neuropathological correlates of dementia in over-80-year-old brain donors from the population-based Cambridge City over-75 s Cohort (CC75C) Study. J Alzheimers Dis. 2009;18:645–658. doi: 10.3233/JAD-2009-1182. [DOI] [PubMed] [Google Scholar]
- 155.Serrano-Pozo A, Qian J, Monsell SE, Frosch MP, Betensky RA, Hyman BT. Examination of the clinicopathologic continuum of Alzheimer disease in the autopsy cohort of the national Alzheimer coordinating center. J Neuropathol Exp Neurol. 2013;72:1182–1192. doi: 10.1097/NEN.0000000000000016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Boyle PA, Wilson RS, Yu L, Barr AM, Honer WG, Schneider JA, Bennett DA. Much of late life cognitive decline is not due to common neurodegenerative pathologies. Ann Neurol. 2013;74:478–489. doi: 10.1002/ana.23964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Jellinger KA, Attems J. Prevalence and pathogenic role of cerebrovascular lesions in Alzheimer’s disease. J Neurol Sci. 2005;229-230:37–41. doi: 10.1016/j.jns.2004.11.018. [DOI] [PubMed] [Google Scholar]
- 158.Jellinger KA. Pathology and pathogenesis of vascular cognitive impairment - a critical update. Front Aging Neurosci. 2013;5:17. doi: 10.3389/fnagi.2013.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Kovacs GG, Milenkovic I, Wohrer A, Hoftberger R, Gelpi E, Haberler C, Honigschnabl S, Reiner-Concin A, Heinzl H, Jungwirth S, Krampla W, Fischer P, Budka H. Non-Alzheimer neurodegenerative pathologies and their combinations are more frequent than commonly believed in the elderly brain: a community-based autopsy series. Acta Neuropathol. 2013;126:365–384. doi: 10.1007/s00401-013-1157-y. [DOI] [PubMed] [Google Scholar]
- 160.Carotenuto A, Rea R, Colucci L, Ziello AR, Molino I, Carpi S, Traini E, Amenta F, Fasanaro AM. Late and early onset dementia: what is the role of vascular factors? A retrospective study. J Neurol Sci. 2012;322:170–175. doi: 10.1016/j.jns.2012.07.066. [DOI] [PubMed] [Google Scholar]
- 161.White L, Small BJ, Petrovitch H, Ross GW, Masaki K, Abbott RD, Hardman J, Davis D, Nelson J, Markesbery W. Recent clinical-pathologic research on the causes of dementia in late life: update from the Honolulu-Asia Aging Study. J Geriatr Psychiatry Neurol. 2005;18:224–227. doi: 10.1177/0891988705281872. [DOI] [PubMed] [Google Scholar]
- 162.White L. Brain lesions at autopsy in older Japanese-American men as related to cognitive impairment and dementia in the final years of life: a summary report from the Honolulu-Asia Aging Study. J Alzheimers Dis. 2009;18:713–725. doi: 10.3233/JAD-2009-1178. [DOI] [PubMed] [Google Scholar]
- 163.Corrada MM, Berlau DJ, Kawas CH. A population-based clinicopathological study in the oldest-old: the 90+ study. Curr Alzheimer Res. 2012;9:709–717. doi: 10.2174/156720512801322537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Tsuang D, Simpson KL, Li G, Barnhart RL, Edland SD, Bowen J, McCormick W, Teri L, Nochlin D, Larson EB, Thompson ML, Leverenz JB. Evaluation of selection bias in an incident-based dementia autopsy case series. Alzheimer Dis Assoc Disord. 2005;19:67–73. doi: 10.1097/01.wad.0000165507.67993.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Knopman DS, Parisi JE, Salviati A, Floriach-Robert M, Boeve BF, Ivnik RJ, Smith GE, Dickson DW, Johnson KA, Petersen LE, McDonald WC, Braak H, Petersen RC. Neuropathology of cognitively normal elderly. J Neuropathol Exp Neurol. 2003;62:1087–1095. doi: 10.1093/jnen/62.11.1087. [DOI] [PubMed] [Google Scholar]
- 166.Davis DG, Schmitt FA, Wekstein DR, Markesbery WR. Alzheimer neuropathologic alterations in aged cognitively normal subjects. J Neuropathol Exp Neurol. 1999;58:376–388. doi: 10.1097/00005072-199904000-00008. [DOI] [PubMed] [Google Scholar]
- 167.Jentoft M, Parisi J, Dickson D, Johnson K, Boeve B, Knopman D, Petersen R. Neuropathologic findings in 32 nondemented elderly subjects (abs.) J Neuropathol Exp Neurol. 2011;70:531. [Google Scholar]
- 168.Buchman AS, Leurgans SE, Nag S, Bennett DA, Schneider JA. Cerebrovascular disease pathology and Parkinsonian signs in old age. Stroke. 2011;42:3183–3189. doi: 10.1161/STROKEAHA.111.623462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Jellinger KA, Attems J. Neuropathology and general autopsy findings in nondemented aged subjects. Clin Neuropathol. 2012;31:87–98. doi: 10.5414/NP300418. [DOI] [PubMed] [Google Scholar]
- 170.Wirth M, Villeneuve S, Haase CM, Madison CM, Oh H, Landau SM, Rabinovici GD, Jagust WJ. Associations between Alzheimer disease biomarkers, neurodegeneration, and cognition in cognitively normal older people. JAMA Neurol. 2013;70:1512–1519. doi: 10.1001/jamaneurol.2013.4013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Roman GC, Kalaria RN. Vascular determinants of cholinergic deficits in Alzheimer disease and vascular dementia. Neurobiol Aging. 2006;27:1769–1785. doi: 10.1016/j.neurobiolaging.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 172.Garde E, Lykke Mortensen E, Rostrup E, Paulson OB. Decline in intelligence is associated with progression in white matter hyperintensity volume. J Neurol Neurosurg Psychiatry. 2005;76:1289–1291. doi: 10.1136/jnnp.2004.055905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Artero S, Tiemeier H, Prins ND, Sabatier R, Breteler MM, Ritchie K. Neuroanatomical localisation and clinical correlates of white matter lesions in the elderly. J Neurol Neurosurg Psychiatry. 2004;75:1304–1308. doi: 10.1136/jnnp.2003.023713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ihara M, Polvikoski TM, Hall R, Slade JY, Perry RH, Oakley AE, Englund E, O’Brien JT, Ince PG, Kalaria RN. Quantification of myelin loss in frontal lobe white matter in vascular dementia, Alzheimer’s disease, and dementia with Lewy bodies. Acta Neuropathol. 2010;119:579–589. doi: 10.1007/s00401-009-0635-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Tullberg M, Fletcher E, DeCarli C, Mungas D, Reed BR, Harvey DJ, Weiner MW, Chui HC, Jagust WJ. White matter lesions impair frontal lobe function regardless of their location. Neurology. 2004;63:246–253. doi: 10.1212/01.WNL.0000130530.55104.B5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Malykhin N, Vahidy S, Michielse S, Coupland N, Camicioli R, Seres P, Carter R. Structural organization of the prefrontal white matter pathways in the adult and aging brain measured by diffusion tensor imaging. Brain Struct Funct. 2011;216:417–431. doi: 10.1007/s00429-011-0321-1. [DOI] [PubMed] [Google Scholar]
- 177.Reed BR, Eberling JL, Mungas D, Weiner M, Kramer JH, Jagust WJ. Effects of white matter lesions and lacunes on cortical function. Arch Neurol. 2004;61:1545–1550. doi: 10.1001/archneur.61.10.1545. [DOI] [PubMed] [Google Scholar]
- 178.Wen HM, Mok VC, Fan YH, Lam WW, Tang WK, Wong A, Huang RX, Wong KS. Effect of white matter changes on cognitive impairment in patients with lacunar infarcts. Stroke. 2004;35:1826–1830. doi: 10.1161/01.STR.0000133686.29320.58. [DOI] [PubMed] [Google Scholar]
- 179.Pievani M, de Haan W, Wu T, Seeley WW, Frisoni GB. Functional network disruption in the degenerative dementias. Lancet Neurol. 2011;10:829–843. doi: 10.1016/S1474-4422(11)70158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.De Vogelaere F, Santens P, Achten E, Boon P, Vingerhoets G. Altered default-mode network activation in mild cognitive impairment compared with healthy aging. Neuroradiology. 2012;54:1195–1206. doi: 10.1007/s00234-012-1036-6. [DOI] [PubMed] [Google Scholar]
- 181.van der Flier WM, van Straaten EC, Barkhof F, Verdelho A, Madureira S, Pantoni L, Inzitari D, Erkinjuntti T, Crisby M, Waldemar G, Schmidt R, Fazekas F, Scheltens P. Small vessel disease and general cognitive function in nondisabled elderly: the LADIS study. Stroke. 2005;36:2116–2120. doi: 10.1161/01.STR.0000179092.59909.42. [DOI] [PubMed] [Google Scholar]
- 182.van der Flier WM, van Straaten EC, Barkhof F, Ferro JM, Pantoni L, Basile AM, Inzitari D, Erkinjuntti T, Wahlund LO, Rostrup E, Schmidt R, Fazekas F, Scheltens P. Medial temporal lobe atrophy and white matter hyperintensities are associated with mild cognitive deficits in non-disabled elderly people: the LADIS study. J Neurol Neurosurg Psychiatry. 2005;76:1497–1500. doi: 10.1136/jnnp.2005.064998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Capizzano AA, Acion L, Bekinschtein T, Furman M, Gomila H, Martinez A, Mizrahi R, Starkstein SE. White matter hyperintensities are significantly associated with cortical atrophy in Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2004;75:822–827. doi: 10.1136/jnnp.2003.019273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Schmidt R, Ropele S, Ferro J, Madureira S, Verdelho A, Petrovic K, Gouw A, van der Flier WM, Enzinger C, Pantoni L, Inzitari D, Erkinjuntti T, Scheltens P, Wahlund LO, Waldemar G, Rostrup E, Wallin A, Barkhof F, Fazekas F. Diffusion-weighted imaging and cognition in the leukoariosis and disability in the elderly study. Stroke. 2010;41:e402–e408. doi: 10.1161/STROKEAHA.109.576629. [DOI] [PubMed] [Google Scholar]
- 185.Kövari E, Gold G, Herrmann FR, Canuto A, Hof PR, Michel JP, Bouras C, Giannakopoulos P. Cortical microinfarcts and demyelination significantly affect cognition in brain aging. Stroke. 2004;35:410–414. doi: 10.1161/01.STR.0000110791.51378.4E. [DOI] [PubMed] [Google Scholar]
- 186.Kalaria RN, Kenny RA, Ballard CG, Perry R, Ince P, Polvikoski T. Towards defining the neuropathological substrates of vascular dementia. J Neurol Sci. 2004;226:75–80. doi: 10.1016/j.jns.2004.09.019. [DOI] [PubMed] [Google Scholar]
- 187.Burhan AM, Bartha R, Bocti C, Borrie M, Laforce R, Rosa-Neto P, Soucy JP. Role of emerging neuroimaging modalities in patients with cognitive impairment: a review from the Canadian Consensus Conference on the Diagnosis and Treatment of Dementia 2012. Alzheimers Res Ther. 2013;5:S4. doi: 10.1186/alzrt200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kantarci K. Molecular imaging of Alzheimer disease pathology. AJNR Am J Neuroradiol. 2014;35:S12–S17. doi: 10.3174/ajnr.A3847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Landau SM, Thomas BA, Thurfjell L, Schmidt M, Margolin R, Mintun M, Pontecorvo M, Baker SL, Jagust WJ. Amyloid PET imaging in Alzheimer’s disease: a comparison of three radiotracers. Eur J Nucl Med Mol Imaging. 2014;41:1398–1407. doi: 10.1007/s00259-014-2753-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Villemagne VL, Furumoto S, Fodero-Tavoletti MT, Mulligan RS, Hodges J, Harada R, Yates P, Piguet O, Pejoska S, Dore V, Yanai K, Masters CL, Kudo Y, Rowe CC, Okamura N. In vivo evaluation of a novel tau imaging tracer for Alzheimer’s disease. Eur J Nucl Med Mol Imaging. 2014;41:816–826. doi: 10.1007/s00259-013-2681-7. [DOI] [PubMed] [Google Scholar]
- 191.Jack CR, Jr, Barrio JR, Kepe V. Cerebral amyloid PET imaging in Alzheimer’s disease. Acta Neuropathol. 2013;126:643–657. doi: 10.1007/s00401-013-1185-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Kepe V, Moghbel MC, Langstrom B, Zaidi H, Vinters HV, Huang SC, Satyamurthy N, Doudet D, Mishani E, Cohen RM, Hoilund-Carlsen PF, Alavi A, Barrio JR. Amyloid-beta positron emission tomography imaging probes: a critical review. J Alzheimers Dis. 2013;36:613–631. doi: 10.3233/JAD-130485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Mathis CA, Kuller LH, Klunk WE, Snitz BE, Price JC, Weissfeld LA, Rosario BL, Lopresti BJ, Saxton JA, Aizenstein HJ, McDade EM, Kamboh MI, DeKosky ST, Lopez OL. In vivo assessment of amyloid-beta deposition in nondemented very elderly subjects. Ann Neurol. 2013;73:751–761. doi: 10.1002/ana.23797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Roh JH, Lee JH. Recent updates on subcortical ischemic vascular dementia. J Stroke. 2014;16:18–26. doi: 10.5853/jos.2014.16.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Kester MI, Goos JD, Teunissen CE, Benedictus MR, Bouwman FH, Wattjes MP, Barkhof F, Scheltens P, van der Flier WM. Associations between cerebral small-vessel disease and Alzheimer disease pathology as measured by cerebrospinal fluid biomarkers. JAMA Neurol. 2014;71:855–862. doi: 10.1001/jamaneurol.2014.754. [DOI] [PubMed] [Google Scholar]


