Abstract
Limited data exist on the impact of prenatal diagnosis and outcomes of fetal truncus arteriosus (TA). We sought to assess prenatal diagnostic accuracy and prenatal outcomes in fetuses with TA and compare postnatal outcomes in neonates with prenatally and postnatally diagnosed TA. Records were reviewed for patients diagnosed with TA in utero or at ≤60 days of life from 1992 to 2007. Forty-three (32%) of 136 TA patients had prenatal diagnosis. Five patients with TA were prenatally misdiagnosed, and 5 with other congenital heart diseases were misdiagnosed with TA prenatally. Of 28 fetuses diagnosed at <24 weeks gestation, 19 (68%) did not survive to birth because of spontaneous fetal death (n = 2) or because of elective termination (n = 17). Pregnancy termination was not more likely for fetuses with extracardiac anomalies. Of 19 live-born patients with correct prenatal diagnosis of TA, 2 (11%) died before surgery, and 4 (24%) died in the early postoperative period. All patients who died presurgically had been diagnosed prenatally. Overall, early postoperative mortality was 10%. Prenatal diagnosis of TA remains challenging and is associated with a high rate of elective termination. Fetal diagnosis was associated with younger age at repair but was not associated with improved neonatal survival.
Keywords: Fetus, Aortic valve, Pulmonary valve, Tetralogy of Fallot, Pulmonary atresia, Conotruncal anomaly
The impact of prenatal diagnosis on postnatal outcomes has been controversial for patients with critical congenital heart disease (CHD) as well as for those with less critical cardiac lesions. Several studies have shown decreased neonatal morbidity and mortality after prenatal diagnosis, usually of duct-dependent congenital heart defects [1, 3, 10, 14]. Other studies found no benefit of prenatal diagnosis on neonatal outcomes [4, 5, 11]. However, prenatal diagnosis of any CHD has other potential advantages. Early diagnosis gives families time to prepare for having a child with CHD, may provide the opportunity for parents to choose termination of pregnancy, and allows parents and physicians to plan elective delivery at a tertiary care center.
The impact of prenatal diagnosis of truncus arteriosus (TA) is not well characterized. Addition of the outflow view in routine prenatal ultrasound screening has improved fetal detection of conotruncal anomalies [2], but postnatal diagnosis of TA remains common. Published information regarding the accuracy of fetal diagnosis or outcomes in prenatally diagnosed TA patients [6, 13, 15] is sparse, and no previous studies exist that compare patient characteristics and postnatal outcomes between prenatally and postnatally diagnosed TA patients. Current understanding of prognosis is largely founded on studies evaluating neonatal surgical results [8, 9, 12]. The goal of this study was to evaluate prenatal diagnosis of TA-including assessment of diagnostic accuracy, outcomes, and impact of fetal diagnosis on neonatal survival of patients with TA at our institution during a 16-year period.
Methods
Patients
This study included all patients diagnosed with TA in utero or within the first 60 days of life at Children’s Hospital Boston from January 1992 through December 2007. Patients diagnosed at >60 days or those with significant additional cardiac defects (e.g., tricuspid atresia, hypoplastic left heart, etc.) were excluded. Maternal and postnatal medical records were reviewed for maternal age, gestational age at time of diagnosis, extracardiac anomalies, chromosomal abnormalities, echocardiographic findings, and fetal and neonatal clinical courses. When fluorescence in situ hybridization laboratory results were not available to establish 22q11 deletion status, we secondarily searched clinical documents for evidence of genetic testing results. Confirmation of prenatal diagnosis was obtained from postnatal transthoracic echocardiograms in fetuses who survived until birth. This study was approved by the Committee for Clinical Investigation at Children’s Hospital Boston.
Data Analysis
Comparisons between groups (e.g., live-born and non–live-born fetal diagnoses, prenatally and postnatally diagnosed patients, etc) were performed using independent samples Student t test, Wilcoxon rank sum test for continuous data, χ2 analysis, or Fisher’s exact test for catagoric data. Data are presented as means ± SDs or medians (ranges).
Results
Prenatal Diagnosis
One hundred forty-one patients were diagnosed with TA from 1992 to 2007. Forty-three (30%) had prenatal diagnosis of TA, and 5 others (4%) had a prenatal diagnoses of tetralogy of Fallot with pulmonary atresia (TOF-PA) or double-outlet right ventricle (DORV), but postnatally they were found to have TA. There was no gradual trend in the frequency of prenatal detection during the study period (Fig. 1). However, patients diagnosed after 2004 were more likely to be diagnosed prenatally (14 of 23 [16%]) than patients diagnosed in 2004 or before (34 of 118 [29%], P = 0.003). In the 43 patients with prenatal diagnosis of TA, referral for fetal echocardiogram was made due to suspicion of cardiac anomaly on obstetric screening ultrasound in 41 (95%) patients, maternal diabetes and fetal rib abnormality in 1 patient, and early rupture of membranes in 1 twin gestation.
Figure 1.
Number of new fetal and neonatal diagnoses of TA from 1992 to 2007 at Children’s Hospital Boston
Prenatal Diagnostic Accuracy
Five (21%) of the 24 patients with prenatal diagnosis of TA who survived to birth were found to have TOF-PA on postnatal echocardiogram. Uncertainty between the diagnoses of TA versus TOF-PA was documented in 4 of these patients, 2 of whom were diagnosed with TOF-PA on >1 fetal echocardiogram, but diagnosis of TA was thought to be most likely on the last fetal echocardiogram before birth. Five additional patients in our study had prenatal diagnoses of TOFPA or DORV but were found to have TA postnatally.
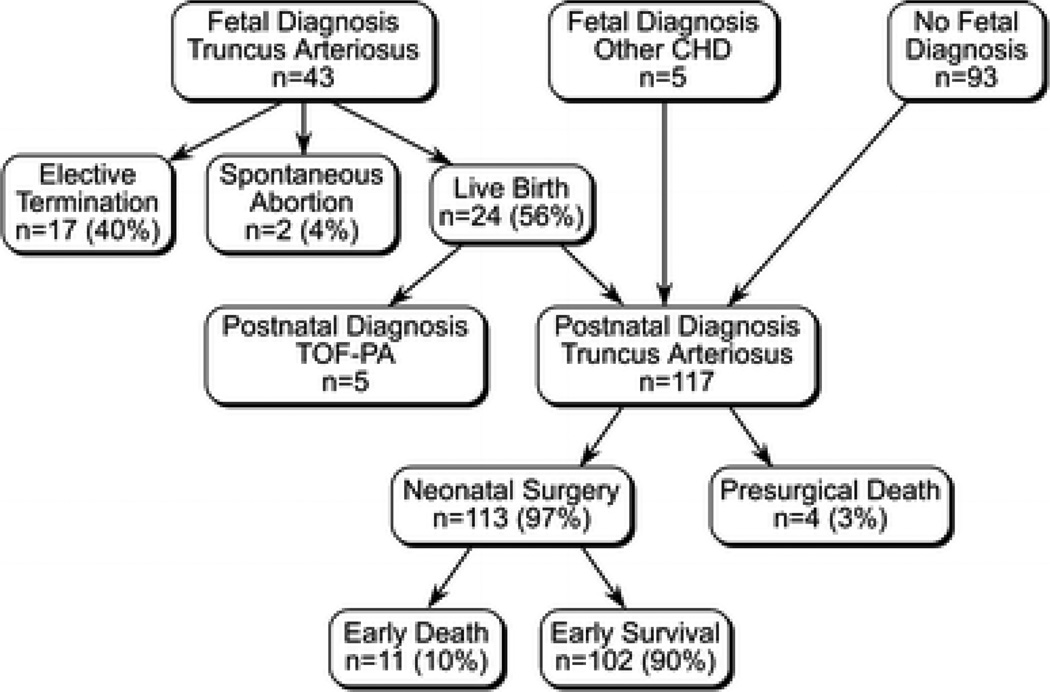
Prenatal Outcomes
Two (5%) of the 43 fetuses with prenatal diagnosis of TA dies spontaneously in utero (Fig. 2); these were the only 2 fetuses who had more than moderate truncal valve regurgitation described on the first fetal echocardiogram. Seventeen (40%) of 43 families elected to terminate pregnancy. No trend in frequency of termination was found during the study period. Of the 28 fetuses diagnosed at <24 weeks of gestation, 68% (n = 19) did not continue to term either because of spontaneous fetal death (n = 2) or elective termination (n = 17). No prenatal deaths occurred in patients diagnosed >24 weeks gestation. Twenty-four (56%) of 43 fetuses with prenatal diagnosis of TA survived to birth; 15 were born at ≥36 weeks gestation, 7 were born at 30 to 35 weeks gestation, and 2 were born at <30 weeks gestation. There was no difference in frequency of extracardiac anomalies between live-born fetuses and those who did not survive to birth (Table 1).
Figure 2.
Flow chart depicting diagnosis and outcome of patients diagnosed with TA in the fetal or neonatal period
Table 1.
Characteristics of fetuses diagnosed with truncus arteriosus that were and were not live born
| Variable | Live born | Not live born | P |
|---|---|---|---|
| All fetusesa | 24 | 19 | |
| Maternal age (±SD) at diagnosis (y) | 30.0 ± 4.9 | 31.4 ±4.1 | 0.36 |
| Gestational age (±SD) at diagnosis (wk) | 25.9±5.7 | 20.5±1.8 | <0.001 |
| Extracardiac anomalies (%) | 8 (33) | 6 (32) | 0.9 |
| Twin gestation (%) | 3 (13) | 2 (11) | 0.84 |
| Truncal regurgitation greater than mild (%) | 1 (4) | 2 (11) | 0.42 |
| Truncus stenosis greater than mild (%) | 2 (8) | 4 (21) | 0.23 |
Includes all fetuses with prenatal diagnosis
Postnatal Diagnosis
From 1992 to 2007, 93 patients with TA were first diagnosed in the postnatal period. Extracardiac anomalies were present in 32% (6/19) of patients prenatally diagnosed and only 15% (14/93) of patients postnatally diagnosed (P = 0.08), which suggests a trend toward statistical significance (Table 2). There were no statistically significant differences in cardiac anatomy or truncal valve dysfunction found between prenatally diagnosed live-born patients and patients diagnosed postnatally.
Table 2.
Postnatal characteristics of prenatally and postnatally diagnosed truncus arteriosus
| Variable | Total | Correct prenatal diagnosisa |
Postnatal diagnosisb |
P c |
|---|---|---|---|---|
| Total no. of patients | 112 | 19 | 93 | |
| Extracardiac abnormalities (%) | 20 (18) | 6 (32) | 14 (15) | 0.08 |
| Truncal regurgitation greater than mild (%) | 19 (17) | 1 (5) | 18 (19) | 0.12 |
| Truncal stenosis greater than mild (%) | 13 (12) | 3 (16) | 10 (11) | 0.46 |
| Right aortic arch (%) | 34 (30) | 7 (37) | 27 (29) | 0.50 |
| Interrupted aortic arch (%) | 18 (16) | 2 (11) | 16 (17) | 0.73 |
| Discontinuous pulmonary arteries (%) | 6 (5) | 3 (16) | 3 (3) | 0.06 |
| Abnormal coronary pattern (%) | 32 (29) | 6 (32) | 26 (28) | 0.75 |
| Median age (range) at first postnatal echocardiogram (d) | 6 (1–59) | 1 (1–2) | 7 (1–59) | <0.001 |
| Death without surgery (%) | 2 (2) | 2 (11) | 0 (0) | 0.002 |
| Median age (range) at surgery (d) | 10 (1–79) | 6 (1–27) | 12 (2–79) | 0.006 |
| Mean weight (range) at surgery (kg) | 3.0 (1.1–.2) | 3.0 (1.1–3.9) | 3.0 (1.5–5.2) | 0.44 |
| Median length (range) of hospital stay (d)d | 15 (4–156) | 19 (8–102) | 15 (4–156) | 0.39 |
| Early postoperative deathd,e (%) | 11 (10) | 4 (24) | 7 (8) | 0.07 |
| Neonatal death at <60 d (%) | 13 (12) | 6 (32) | 7 (8) | 0.003 |
Includes all TA patients with correct prenatal diagnosis of TA. Imaging data are from the first postnatal echocardiogram
Includes all patients with first diagnosis of TA in the neonatal period. Excludes patients with prenatal misdiagnosis of other CHD
Prenatal versus postnatal diagnosis
Excludes presurgical deaths
Less than/equal to 30 days after surgery. Reported percentage is of total patients undergoing surgical repair
Neonatal Course
Four patients with prenatal identification of CHD died in the newborn period without attempted surgical repair. Two of these patients were diagnosed with TA correctly in utero, and 2 were diagnosed prenatally with pulmonary atresia or TOF and were postnatally found to have TA. One of these patients was born at 29 weeks gestation and died secondary to necrotizing enterocolitis and sepsis. The other 3 patients had severe extracardiac abnormalities, which were the primary cause of death soon after birth, and 2 of these were also born very prematurely. There were no presurgical deaths among patients first diagnosed neonatally.
A total of 113 patients with TA underwent surgical repair. Twenty of these patients had prenatal diagnosis of CHD, 17 of which had a correct prenatal diagnosis of TA. The 93 postnatally diagnosed patients underwent surgical repair at a median age of 12 days (range 2 to 79), which is significantly older than prenatally diagnosed patients who underwent surgical repair at a median age of 6 days (range 1 to 27, P = 0.006). There was no difference in length of hospital stay between prenatally diagnosed and postnatally diagnosed cohorts.
Although patients with prenatal diagnosis underwent repair at an earlier age than postnatally diagnosed TA patients, they actually had a greater early postoperative mortality overall. Four (24%) of the 17 prenatally diagnosed patients who underwent surgery had early postoperative death (≤30 days after surgery) compared with 7 (8%) of the 93 patients first diagnosed postnatally (P = 0.07). We found no differences in early postoperative survival between patients with and without associated cardiac anomalies (e.g., interrupted aortic arch, discontinuous pulmonary arteries, coronary arteries, truncal valve dysfunction) or those with and without extracardiac abnormalities.
22q11 Deletion
Because this was a retrospective study during a period of 16 years, 22q11 status was not able to be identified for all patients and therefore was not used in outcome analysis. Seventeen (71%) of the 24 prenatally diagnosed patients with TA who were liveborn had fluorescence in situ hybridization results available in our laboratory database or detailed in clinical documentation, and 5 (29%) of these 17 were positive for 22q11 deletion. Of the 93 patients first diagnosed postnatally, 51 (55%) patients had documented genetic testing results, and 27 (53%) of these were positive for 22q11 deletion.
Discussion
Prenatal Diagnosis
Prenatal diagnosis of CHD has a number of potential benefits. It may decrease neonatal morbidity and mortality by providing the opportunity for a controlled elective delivery at an institution with specialized perinatal care and a cardiac surgical program. In addition, early diagnosis allows parents time to prepare themselves, research treatment options, obtain more in-depth evaluation for other fetal anomalies, and determine whether to continue the pregnancy.
Although it is encouraging that the frequency of in utero diagnosis of CHD is increasing, 68% of all TA patients diagnosed during our study period were not recognized to have significant CHD before birth. Prenatally diagnosed patients were more likely to have extracardiac anomalies, which seems logical because fetuses diagnosed with an extracardiac anomaly may undergo more rigorous cardiac evaluation and thus be more likely to have a CHD identified prenatally. No structural or hemodynamic features of TA were associated with increased likelihood of prenatal diagnosis.
Accuracy of Prenatal Diagnosis of TA
When a pulmonary valve and right ventricular outflow tract cannot be identified on fetal echocardiogram, differentiation between TA and other congenital heart defects with semilunar valve atresia can be difficult. Several other lesions, including TOF-PA and aortic atresia with ventricular septal defect, involve a single large semilunar valve and a ventricular septal defect. In TA, the pulmonary arteries arise before the take-off of the first brachiocephalic vessel, and the flow in the pulmonary arteries is pulsatile. Based on our clinical experience, patients with TOF-PA are more likely to have continuous flow in the pulmonary arteries because these vessels are supplied either by aortopulmonary collateral arteries or a ductus arteriosus, which arises distal to the first brachiocephalic vessel. In aortic atresia with ventricular septal defect, retrograde flow in the hypoplastic aortic arch is supplied by the ductal arch.
Duke et al. found that 2 of 16 patients (13%) with firm prenatal diagnosis of TA were misdiagnosed, whereas Volpe et al. reported inaccurate prenatal diagnosis of TA in 1 of 24 patients (4%) [6, 15]. Although 5 patients in our study were misdiagnosed with TA on the last prenatal echocardiogram, only 1 of these patients was considered to have certain diagnosis of TA (1 of 24 [4%]). Although definitive diagnosis in utero is desirable, the ambiguity that sometimes exists may not have an important postnatal clinical impact as long as prompt neonatal evaluation is performed. In most cases of fetal misdiagnosis in our study, diagnostic uncertainty was acknowledged at the time of prenatal evaluation. All possible diagnoses were discussed with the family, and appropriate counseling was provided to include all potential diagnoses. In addition, once families receive the diagnosis of any significant CHD, they may still benefit from this prenatal information regarding the various aspects we described earlier.
Fetal Survival
Prenatal diagnosis allows for more informed choices about management of pregnancy and better understanding of the in utero natural history of the disease. Only two fetuses in our cohort had more than moderate truncal regurgitation on first fetal echocardiogram, and these were the only two fetuses that died spontaneously in utero. This suggests that a critical degree of truncal regurgitation is not tolerated in utero and is a significant risk factor for fetal death. It also highlights the importance of informing families that fetal death can occur despite parental wishes to carry a child to term.
Despite improvements in postnatal management and surgical outcomes during the last 2 decades, the rate of termination of fetuses with TA remains high. Previously published studies have found that 24% to 34.8% of prenatally diagnosed TA patients are electively terminated [6, 15], so our 40% elective termination frequency is higher than previously reported. Even more striking is that among fetuses diagnosed >24 weeks gestation in our study, 61% of families elected to terminate pregnancy. Because of the fact that we are a regional referral center, our frequency of pregnancy termination may be an underestimate because some families receive diagnostic information from their obstetrician or local cardiologist and may elect to terminate pregnancy without referral for specialized cardiac evaluation. This high frequency of elective termination may result in substantially decreased incidence of TA at birth. However, because this is not a true population-based study, we cannot determine the actual effect of elective termination on incidence of neonatal TA. We anticipated that termination of pregnancy would be more common for fetuses with noncardiac anomalies, but we did not find this to be the case.
Neonatal Outcome
One of the most important potential benefits of prenatal diagnosis of CHD is improved neonatal outcome. This benefit is most likely to be seen with duct-dependent congenital cardiac lesions because normal ductal closure causes undiagnosed neonates to become acidotic and critically ill before cardiac evaluation is initiated. TA is not a duct-dependent lesion unless there is an associated interrupted aortic arch, so it is not expected that prenatal diagnosis would significantly impact either patient condition in the immediate postnatal period or longer-term neonatal outcomes. In fact, all four presurgical deaths in our study occurred in patients who were prenatally identified as having significant CHD. One major reason for this finding is that three of these patients also had severe extracardiac abnormalities, which were the primary cause of death or provoked redirection of care after birth.
In this series, neonates with fetal diagnosis underwent surgical repair at a younger age compared with patients without prenatal diagnosis. However, this did not result in shorter hospital stays for prenatally diagnosed patients, and these neonates actually had increased presurgical and postsurgical death. One explanation could be that prenatally diagnosed neonates tended to have extracardiac abnormalities, which can add complications to postnatal management and lengthen hospital stay. Another contributing factor could be underascertainment of postnatally diagnosed patients because patients who died before transfer to our institution for surgery would not be included in this series. However, this is probably not a large factor because TA is not a ductdependent lesion. The only statistically significant difference we found between these two cohorts that might have impacted postsurgical mortality is age at surgical repair.
It is worth noting that the overall postoperative mortality for TA was 10% in our series. There were no major differences in survival related to anatomic or functional abnormalities, including interrupted aortic arch, discontinuous pulmonary arteries, coronary artery anomalies, or truncal valve regurgitation, which were previously found to be important predictors of outcome, [7, 12].
Limitations
The major limitation of this study is that it is a retrospective institutional review rather than a population-based study. Fetal patients are often evaluated and then the parents counseled by an obstetrician and/or cardiologist at another institution before referral to our tertiary care center. Similarly, there may be ascertainment bias with respect to postnatally diagnosed patients because patients with TA who died in the community without surgery, and possibly without diagnosis of CHD, would not appear in our cohort. The high frequency of termination in this population confounds analysis of the accuracy of prenatal diagnosis because it does not allow postnatal confirmation of diagnosis for a large number of patients. Because this was a retrospective study during a long time period, 22q11 deletion status was not able to be identified for all patients. Because of this, it was not possible to perform comprehensive analysis to determine the importance of this genetic abnormality on outcome.
In conclusion, prenatal diagnosis of TA remains challenging and is associated with a high rate of elective termination. Although fetal diagnosis was associated with younger age at repair, it was not associated with shorter hospital stay or improved neonatal survival.
Acknowledgments
This work was supported by the National Institutes of Health under award number: T32HL007572. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This study was supported by contributions from the Kenrose Kitchen Table Foundation.
Contributor Information
Tara M. Swanson, Email: tara.swanson@alum.dartmouth.org.
Doff B. McElhinney, Email: doff.mcelhinney@cardio.chboston.org.
References
- 1.Bonnet D, Coltri A, Butera G, Fermont L, Le BJ, Kachaner J, et al. Detection of transposition of the great arteries in fetuses reduces neonatal morbidity and mortality. Circulation. 1999;99:916–918. doi: 10.1161/01.cir.99.7.916. [DOI] [PubMed] [Google Scholar]
- 2.Carvalho JS, Mavrides E, Shinebourne EA, Campbell S, Thilaganathan B. Improving the effectiveness of routine prenatal screening for major congenital heart defects. Heart. 2002;88:387–391. doi: 10.1136/heart.88.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang AC, Huhta JC, Yoon GY, Wood DC, Tulzer G, Cohen A, et al. Diagnosis, transport, and outcome in fetuses with left ventricular outflow tract obstruction. J Thorac Cardiovasc Surg. 1991;102:841–848. [PubMed] [Google Scholar]
- 4.Cohen MS, Schultz AH, Tian ZY, Donaghue DD, Weinberg PM, Gaynor JW, et al. Heterotaxy syndrome with functional single ventricle: does prenatal diagnosis improve survival? Ann Thorac Surg. 2006;82:1629–1636. doi: 10.1016/j.athoracsur.2006.05.039. [DOI] [PubMed] [Google Scholar]
- 5.Daubeney PE, Sharland GK, Cook AC, Keeton BR, Anderson RH, Webber SA. Pulmonary atresia with intact ventricular septum: impact of fetal echocardiography on incidence at birth and postnatal outcome UK and Eire Collaborative Study of Pulmonary Atresia with Intact Ventricular Septum. Circulation. 1998;98:562–566. doi: 10.1161/01.cir.98.6.562. [DOI] [PubMed] [Google Scholar]
- 6.Duke C, Sharland GK, Jones AM, Simpson JM. Echocardiographic features and outcome of truncus arteriosus diagnosed during fetal life. Am J Cardiol. 2001;88:1379–1384. doi: 10.1016/s0002-9149(01)02117-8. [DOI] [PubMed] [Google Scholar]
- 7.Hanley FL, Heinemann MK, Jonas RA, Mayer JE, Jr, Cook NR, Wessel DL, et al. Repair of truncus arteriosus in the neonate. J Thorac Cardiovasc Surg. 1993;105:1047–1056. [PubMed] [Google Scholar]
- 8.Imamura M, Drummond-Webb JJ, Sarris GE, Mee RB. Improving early and intermediate results of truncus arteriosus repair: a new technique of truncal valve repair. Ann Thorac Surg. 1999;67:1142–1146. doi: 10.1016/s0003-4975(99)00061-2. [DOI] [PubMed] [Google Scholar]
- 9.Kalavrouziotis G, Purohit M, Ciotti G, Corno AF, Pozzi M. Truncus arteriosus communis: early and midterm results of early primary repair. Ann Thorac Surg. 2006;82:2200–2206. doi: 10.1016/j.athoracsur.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Mahle WT, Clancy RR, McGaurn SP, Goin JE, Clark BJ. Impact of prenatal diagnosis on survival and early neurologic morbidity in neonates with the hypoplastic left heart syndrome. Pediatrics. 2001;107:1277–1282. doi: 10.1542/peds.107.6.1277. [DOI] [PubMed] [Google Scholar]
- 11.McElhinney DB, Salvin JW, Colan SD, Thiagarajan R, Crawford EC, Marcus EN, et al. Improving outcomes in fetuses and neonates with congenital displacement (Ebstein’s malformation) or dysplasia of the tricuspid valve. Am J Cardiol. 2005;96:582–586. doi: 10.1016/j.amjcard.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 12.Thompson LD, McElhinney DB, Reddy M, Petrossian E, Silverman NH, Hanley FL. Neonatal repair of truncus arteriosus: continuing improvement in outcomes. Ann Thorac Surg. 2001;72:391–395. doi: 10.1016/s0003-4975(01)02796-5. [DOI] [PubMed] [Google Scholar]
- 13.Tometzki AJ, Suda K, Kohl T, Kovalchin JP, Silverman NH. Accuracy of prenatal echocardiographic diagnosis and prognosis of fetuses with conotruncal anomalies. J Am Coll Cardiol. 1999;33:1696–1701. doi: 10.1016/s0735-1097(99)00049-2. [DOI] [PubMed] [Google Scholar]
- 14.Tworetzky W, McElhinney DB, Reddy VM, Brook MM, Hanley FL, Silverman NH. Improved surgical outcome after fetal diagnosis of hypoplastic left heart syndrome. Circulation. 2001;103:1269–1273. doi: 10.1161/01.cir.103.9.1269. [DOI] [PubMed] [Google Scholar]
- 15.Volpe P, Paladini D, Marasini M, Buonadonna AL, Russo MG, Caruso G, et al. Common arterial trunk in the fetus: characteristics, associations, and outcome in a multicentre series of 23 cases. Heart. 2003;89:1437–1441. doi: 10.1136/heart.89.12.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]