Case Notes
A 29-year-old woman came to the outpatient clinic with complaints of chronic pelvic pain and dyspareunia. Her physical examination was normal. Her blood work and laboratory investigations were within normal range. Ultrasonography revealed a cystic mass posterior to vagina and uterus. Computed tomography (CT scan) showed an oblong structure with fluid density contents (Fig. 1). Patient had a magnetic resonance imaging (MRI) scan which revealed a large 10 × 9 × 4 cm cystic structure posterior to the uterus, originating along the posterior vaginal wall, representing Gartner duct cyst (Fig. 2a, b). The cyst was excised, and benignity of the lesion was confirmed by a histologic study. The diagnosis was consistent with Gartner duct cyst.
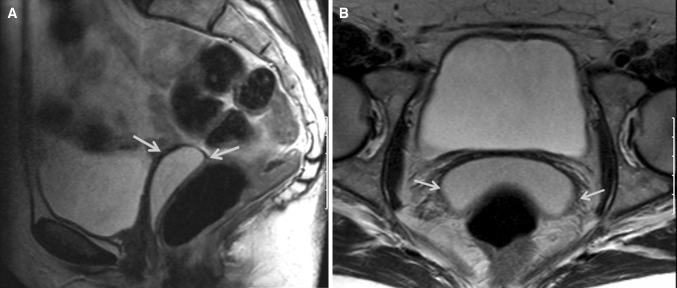
Fig. 1.
Sagittal image from a CT scan of the pelvis shows an oblong structure with fluid density contents
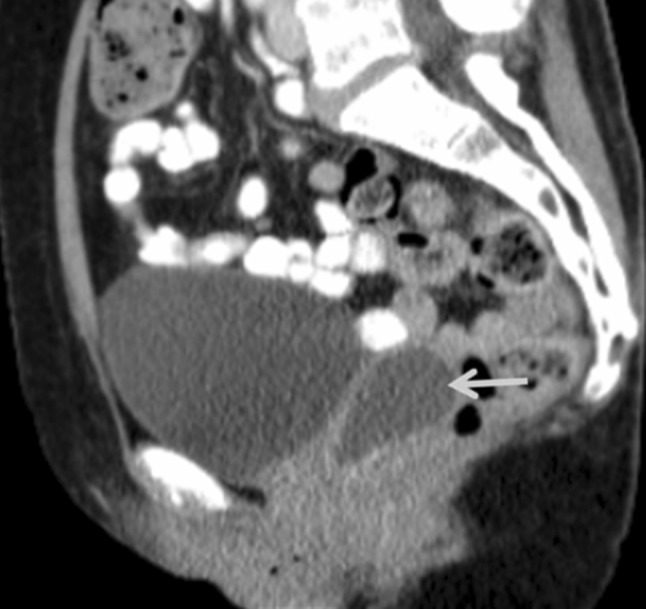
Fig. 2.
a, b Axial- and sagittal T2-weighted images reveal a cystic structure posterior to the uterus, originating along the posterior vaginal wall, representing a Gartner duct cyst
Discussion
Gartner ducts develop from the vestigial remnants of the mesonephric duct or wolffian ducts. Mullerian and mesonephric duct derivatives tend to be located along the anterolateral aspect of vagina but can be found almost at any location within the vaginal walls. Gartner duct cyst can be associated with anomalies of the metanephric urinary system. Case reports of ectopic ureter, unilateral renal aplasia, and hypoplasia have been reported with Gartner duct cyst. Histologically, mesonephric duct cysts are lined by low columnar or cuboidal, non-mucinous, non-ciliated epithelium. Gartner duct cyst can be differentiated from mullerian cysts by the presence of basement membrane and smooth muscle layer. However, a clear difference can be made only by histochemical staining [1].
Gartner duct cysts are usually small and clinically silent but sometimes can be large enough to produce symptoms, and imaging studies become necessary to make a differential diagnosis. Bartholin cyst, urethral diverticulum and cystocele are the common differential diagnoses. Urethral diverticulum is commonly found on the anterior vaginal wall along the distal two-thirds of vagina. These diverticula are usually confined to the urethral walls. Bartholin cysts typically range from 1 to 4 cm in diameter; majority of the cysts are non-tender cystic masses and occur commonly in the posterolateral portion of the lower vagina. Ductal obstruction due to inspissated mucus or previous infection is a prerequisite for Bartholin cyst formation. Ultrasound and CT scan can show cystic mass, while MRI imaging is the best diagnostic modality, which allows better tissue characterization and defines the extent and site of origin of the pelvic mass with concomitant urethral anomalies [2].
Excision of large Gartner duct cyst is indicated. One case report of malignant transformation of Gartner duct cyst is also reported [3]. Conservative treatment with cyst aspiration and 5 % tetracycline injection has been reported to be successful in a series of 15 patients [4], but no long-term follow-up or other reports of this treatment are available. Our patient underwent excision of the cyst transvaginaly. At her annual follow-up visit, she was doing well with no further complaints.
Acknowledgments
Conflict of interest
None.
References
- 1.Eilber KS, Raz S. Benign cystic lesions of the vagina: a literature review. J Urol. 2003;170:717–722. doi: 10.1097/01.ju.0000062543.99821.a2. [DOI] [PubMed] [Google Scholar]
- 2.Hagspiel KD. Giant Gartner duct cyst: magnetic resonance imaging findings. Abdom Imaging. 1995;20:566–568. doi: 10.1007/BF01256713. [DOI] [PubMed] [Google Scholar]
- 3.Bats AS, Metzger U, Le Frere-Belda MA, et al. Malignant transformation of Gartner cyst. Int J Gynecol Cancer. 2009;19:1655–1657. doi: 10.1111/IGC.0b013e3181a844f2. [DOI] [PubMed] [Google Scholar]
- 4.Abd-Rabbo MS, Atta MA. Aspiration and tetracycline sclerotherapy: a novel method for management of vaginal and vulval Gartner cysts. Int J Gynaecol Obstet. 1991;35:235. doi: 10.1016/0020-7292(91)90292-D. [DOI] [PubMed] [Google Scholar]