Abstract
Background
Restoring orbital volume in large blowout fractures is still a technically challenge to the orbital surgeon. In this study, we restored the orbital wall using the combination of transorbital and transnasal approach with additional supports from the paranasal sinuses, and we compared the surgical outcome to that of a conventional transorbital method.
Methods
A retrospective review of all patients with pure unilateral blowout fractures between March 2007 and March 2013 was conducted. 150 patients were classified into two groups according to the surgical method: conventional transorbital method (group A, 75 patients, control group), and the combination of transorbital and transnasal approach with additional supports from the paranasal sinuses (group B, 75 patients, experimental group). Each group was subdivided depending on fracture location: group I (inferior wall), group IM (inferomedial wall), and group M (medial wall). The surgical results were assessed by the Hertel scale and a comparison of preoperative and postoperative orbital volume ratio (OVR) values.
Results
In the volumetric analysis, the OVR decreased more by the experimental groups than each corresponding control groups (P<0.05). Upon ophthalmic examination, neither the differences among the groups in the perioperative Hertel scale nor the preoperative and postoperative Hertel scales were statistically significant (P>0.05).
Conclusions
Our surgical results suggest that orbital volume was more effectively restored by the combination of transorbital and transnasal approach with additional supports from the paranasal sinuses than the conventional method, regardless of the type of fracture.
Keywords: Orbital fractures, Enophthalmos, Paranasal sinuses
INTRODUCTION
Orbital blowout fractures, which are frequently encountered in maxillofacial trauma, can cause a wide range of functional impairments and aesthetic deformities. To reconstruct orbital fractures, the surgeon should carefully reposition the orbital contents and the cavity walls back into their proper position while restoring both the orbital volume and shape [1]. Compared to isolated medial or inferior blowout fracture, surgical treatment of a large blowout fracture presents a particular challenge for the orbital surgeon because of the structural complexity and extensive tissue injury. Although various methods and ideas have been reported for improving the surgical outcomes, none has been found to consistently produce good outcomes.
The transorbital approaches, including the subciliary and transconjunctival approaches, are the conventional methods for providing a wide view of the orbital wall and sufficient exposure for implant placement [2]. However, several disadvantages are associated with these conventional approaches including incomplete restoration of the herniated orbital tissues. Implant displacement or reherniation of orbital contents occasionally produced unfavorable outcomes. Recently, the approach through the ethmoid or maxillary sinuses with an endoscope has been developed and proposed as an alternative to the transorbital approach. Endoscopic transnasal approaches provide a clear view of the orbital wall from the paranasal sinuses and could be useful for achieving accurate reduction [2,3]. However, placing a large implant on the orbital side has been difficult through this endoscope approach [4]. Therefore, a few surgeons have experimented with a combination of these two approaches to compensate for the weakness of each approach alone [2,4].
In this study, we restored the orbital wall to its prior position in pure blowout fractures using a combination of transorbital and transnasal approach from the maxillary or ethmoid sinuses. The restored orbit could be confirmed with the transorbital view, and an implant over the bony defect could easily be placed subperiosteally. Additionally, we supported the restored orbital wall with transnasal packing using Nasopore and/or inflation of a Foley catheter. We report here our surgical method and comparison of its outcome to that of the conventional transorbital method for orbital blowout fractures according to the fracture location.
METHODS
Subjects
The medical records of patients who underwent surgical reconstruction of pure unilateral blowout fractures between March 2007 and March 2013 were reviewed retrospectively. Patients with any of the following criteria were excluded: patients aged under 18, orbital rim fracture, any history of facial fractures, bilateral orbital fracture, or diseases which alter the orbital shape. This study was approved by the institutional review board. All of 150 patients were treated with either conventional transorbital method (group A, 75 patients, control group) or the combination approach with paranasal support (group B, 75 patients, experimental group). Each group was subdivided into 3 groups depending on the fracture location: group I (inferior wall), group IM (inferomedial wall), and group M (medial wall). Data was collected sequentially until there were 25 patients in each subgroup. There were 123 males and 27 females, aged 19 to 61, with a mean of 32.6 years (group A, 34.7 vs. group B, 30.1). The average of surgical timing was 8.04 days after injury (range, 1-19 days; group A, 7.36 days vs. group B, 8.72 days). The most common cause was assault trauma (82 cases), followed by slipping (31 cases), traffic accidents (27 cases), and falling (10 cases). The indications for surgical treatment were 1) limitation of extraocular movement, 2) radiographic evidence of extensive fracture (fracture size >2 cm2 on CT scans), or 3) enophthalmos (>2 mm).
Ophthalmic examination
All of the surgical candidates underwent ophthalmic examinations for diplopia and extraocular muscle movement before surgery. A Hertel exophthalmometer (Inami Inc., Tokyo, Japan) was used to measure the degree of enophthalmos by measuring from the lateral orbital rim to the apex of the cornea. The Hertel scale was defined as the difference in the globe position between the two eyes. A single surgeon measured the scale three times in each patient and the average value was calculated to minimize the error. Preoperative values were obtained one day before surgery to minimize the influence of periorbital edema. The patients visited the outpatient clinic at one week, 1 month, 6 months, and 1 year after surgery. Postoperative Hertel measurements were delayed for 1 year after surgery to allow the processes of atrophy and scarring of the orbital soft tissue to complete by themselves.
CT scans and orbital volume measurements
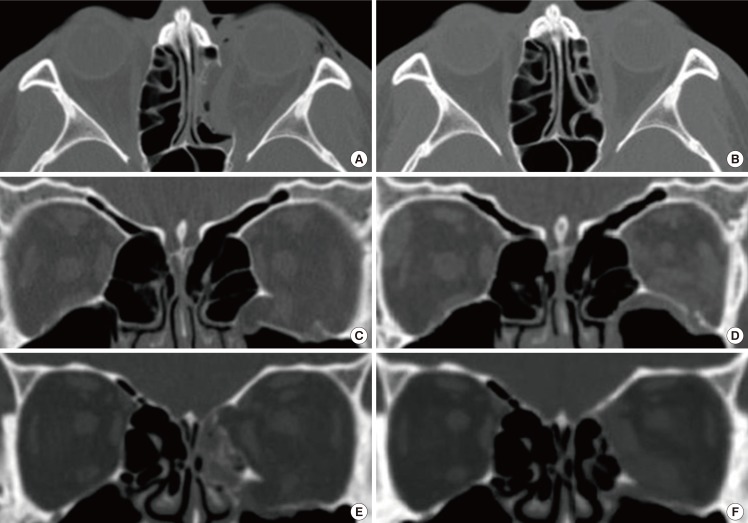
Three-dimensional CT images (GE Lightspeed VCT, GE Healthcare, Milwaukee, WI, USA), were obtained in continuous 2.5-mm-thick axial and coronal slices. In all cases, the patients underwent CT scans within 1 week after injury and at 6 months after surgical treatment (Fig. 1). Boundary of the orbital content including the implant was traced on each image with the Rapidia Image Postprocessing System (Infinitt Co., Ltd., Seoul, Korea). The volume of orbital cavity was calculated by multiplying the orbital area by the thickness of each scan slice; the sum of volumes from the scan slices were used to compute the volume occupied by the measured structure in each orbit. The volume of the orbit on unaffected side was used as a control to eliminate the individual orbital volume differences. The orbital volume ratio (OVR) was obtained with dividing the volume of the traumatized orbit by that of the control side.
Fig. 1.
Computed tomography (CT) scan images of orbital wall restoring surgery
The fractured orbital walls were restored with the combined transorbital and transnasal approaches with additional paranasal sinuses supporting method. (A) Preoperative and (B) postoperative CT scan image of medial orbital wall fracture. (C) Preoperative and (D) postoperative CT scan image of inferior orbital wall fracture. (E) Preoperative and (F) postoperative CT scan image of inferomedial orbital wall fracture.
The postoperative OVR was measured in the same manner.
Surgical techniques
Conventional transorbital method (group A, control group)
Under general anesthesia, a forced duction test was first performed to evaluate the passive mobility of the globe. An incision 3 mm below the lower eyelid tarsal plate was made from the precaruncular area to the lateral orbital fissure. A plane of dissection was then created and followed over the orbital septum to the inferior orbital rim. The incision was extended laterally with canthotomy. After the orbital septum was separated from the inferior orbital rim, the dissection proceeded through the subperiosteal space until the fracture on the inferior and/or medial orbital wall was exposed. The herniated orbital soft tissue was repositioned back into the orbit, and the bony defect in the inferior and/or medial orbital wall was covered with a porous polyethylene implant such as Synpor (Synthes Inc., West Chester, PA, USA) or Medpor (Porex Surgical Inc., Newnan, GA, USA). After the fractured wall was substituted with the implant, the periosteum and the conjunctival incision were sutured in a standard fashion.
Combination of transorbital and transnasal approach with additional supports from the maxillary or ethmoid sinuses (group B, experimental group)
Under general anesthesia, a standard transconjunctival incision to expose the fractured area was performed in the same manner as above. The fractured wall and the herniated orbital contents were identified from the orbital side. After the nasal cavity was decongested with epinephrine pledgets, 2% lidocaine with 1:100,000 epinephrine was injected into the anterior root of the middle turbinate and the uncinate process.
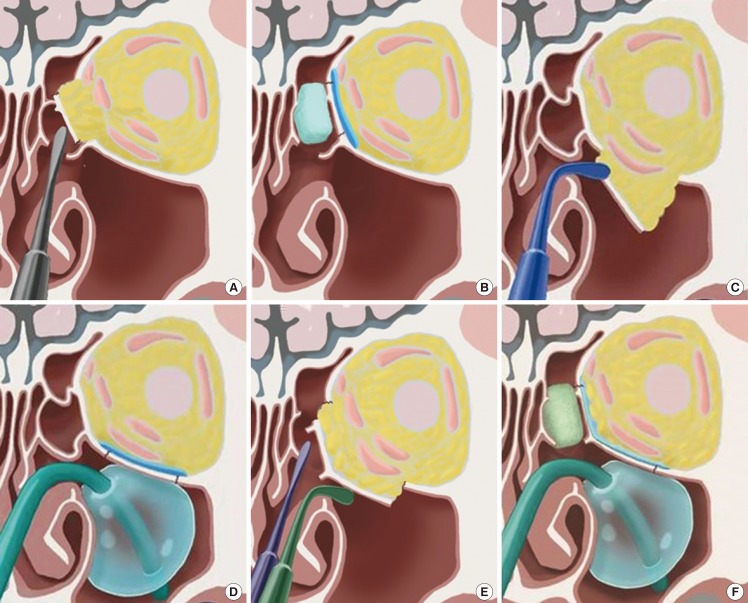
In medial orbital wall fracture
If the medial wall of the orbit was broken, a straight Freer elevator was inserted into the middle nasal meatus and passed gently through the fractured ethmoidal air cells to reach the medial side of the orbital wall fracture without ethmoidectomy (Fig. 2). The prolapsed orbital contents were freed from the entrapment through orbital approach, and the bone fragments were gently mobilized with Freer elevator from the ethmoidal sinuses under direct vision from the transorbital approach. To support the restored orbital wall, Nasopore (Polyganics B.V., Groningen, Netherlands) was placed in the ethmoid sinus through transnasal approach to the medial side of the reconstructed orbit.
Fig. 2.
Illustrations of orbital wall restoring surgery
The fractured orbital wall was restored with a straight and/or curved Freer elevator and maintained with supporting structures on the paranasal sinuses through the transnasal approach. (A) An illustration of the restoration of the fractured medial orbital wall with a straight Freer elevator transnasally, and (B) an illustration of the support with Nasopore for the medial side. (C) An illustration of restoration of the fractured inferior orbital wall with a curved Freer elevator transnasally, and (D) an illustration of the support with a ballooned Foley catheter for the inferior side. (E) An illustration of restoration of the fractured medial and inferior side orbital wall with a straight and curved Freer elevator transnasally, and (F) an illustration of the support with Nasopore for the medial side and ballooned Foley catheter for the inferior side in an inferomedial orbital wall fracture.
In inferior orbital wall fracture
In cases of inferior orbital wall fracture, a curved Freer elevator was introduced to the maxillary sinus through the maxillary ostium to mobilize the inferior aspect of the fracture (Fig. 2). To support the restored orbital floor, the balloon of a 16 Fr. Foley catheter (Sewoon Medical Co., Ltd., Seoul, Korea) was held in curved mosquito forceps, passed through the nostril, and inserted into the maxillary ostium (Fig. 2). After the Foley catheter was inserted, a volume of physiologic saline solution appropriate for each patient, ranging from 12-15 mL, was injected into the balloon until the orbital floor was anatomically restored with the view from the orbit. Care was taken not to entrap the orbital contents, and not to overinflate the balloon. The tube of the Foley catheter was fixed on the cheek. The balloon support was kept in position for 7-8 days.
In inferomedial orbital wall fracture
If fractures had occurred in the medial and inferior wall simultaneously, restoration of the fractured orbit was achieved by using straight and curved Freer elevator consecutively. When the inferomedial strut located near maxillary ostium was collapsed in the inferomedial blowout fractures, it was easily restored with the straight Freer elevator from the transnasal approach.
The placement of the implant
After bony restoration and support procedure, a porous polyethylene implant was shaped to the right size to bridge the defect, and it was adapted to the orbital wall without fixation in all cases. A forced duction test was carried out to ensure free movement without entrapment.
Statistical analysis
A Wilcoxon signed-rank test was used to analyze the perioperative difference of OVR and Hertel scale of two surgical methods in three types of fracture. A Mann-Whitney test was used to compare the measurements of the OVR and Hertel scale between group A and B in three types of orbital fracture. A P-value <0.05 was considered to indicate significance. All of the analyses were performed using SPSS ver. 20.0 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
Ophthalmic examinations
During the study period, 150 patients with pure unilateral blowout fractures underwent orbital reconstruction. Before surgery, 54 of the patients had diplopia (group A, 23 patients vs. group B, 31 patients) and 25 patients had limited extraocular movement (group A, 12 patients vs. group B, 13 patients). Within 1 year after surgery, all of the patients had recovered completely from ocular dysfunctions such as diplopia and extraocular movement limitation. Changes in the Hertel scale within the surgical method group were non-significant in all types of fracture (Table 1). Each preoperative and postoperative value did not differ significantly between the two surgical method groups (P>0.05). Likewise, the difference of the improvement of Hertel scale was non-significant between two surgical method groups (P>0.05) (Table 1).
Table 1.
Hertel scale (mm) in blowout fractures
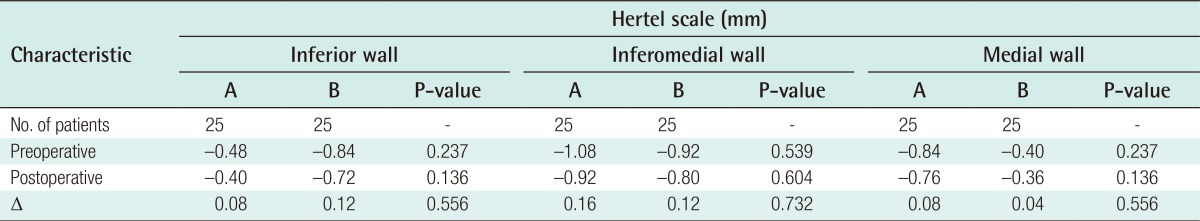
A, control group, conventional transorbital method; B, experimental group, combination of transorbital and transnasal approach with additional supports from the maxillary or ethmoid sinuses; Δ, the difference of perioperative value (postoperative value-preoperative value).
CT scans and orbital volume measurements
The preoperative difference in the OVR between the two surgical groups was found to be statistically no significant in all types of fracture (Table 2). The mean preoperative OVR of group I (109.74% in group A, 110.61% in group B) was significantly higher than that of group M (106.74% in group A, 107.40% in group B). The preoperative OVR in group IM (115.92% in group A, 114.72% in group B) was the highest among the three groups, and its difference was statistically significant.
Table 2.
Orbital volume ratio (%) in blowout fracturesular
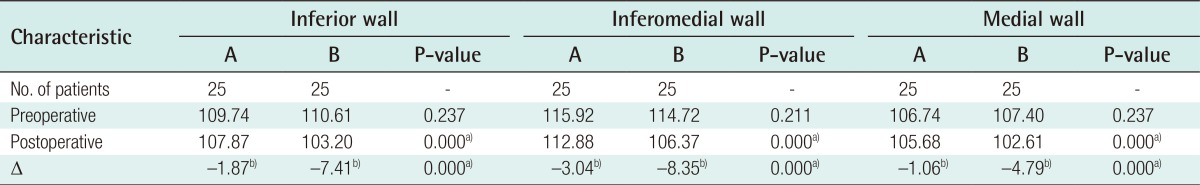
A, control group, conventional transorbital method; B, experimental group, combination of transorbital and transnasal approach with additional supports from the maxillary or ethmoid sinuses; Δ, the difference of perioperative value (postoperative value-preoperative value).
a)Significant difference, P<0.05, Mann-Whitney test; b)Significant difference, P<0.05, Wilcoxon signed rank test.
The postoperative CT scan taken 6 months after surgery showed a significantly decreased OVR in both group A and B, regardless of the type of fracture (P<0.05) (Table 2); among them, the OVR was more significantly decreased in group B than group A in all three locations (7.41% vs. 1.87% in group I, 8.35% vs. 3.04% in group IM, and 4.79 vs. 1.06% in group M) (P<0.05) (Table 2).
DISCUSSION
Blowout fractures are comprised of the fracture defects in deep located bony orbit and the reconstruction of those complicated area remains as a challenge to orbital surgeons. Therefore, there are several different attempts with different approaches to treat the fractures. The conventional reconstruction of orbital wall fractures has been achieved with transorbital approaches, but a technique using an endoscope through ethmoid or maxillary sinus has been developed recently [2,4]. However, it is difficult to insert a large synthetic implant successfully through those endoscopic approaches alone, due to the incomplete exposure of the entire fracture from the sinus as well as the limited space to introducing the implant to the orbital side [3].
The dual approach used in this study has the advantages of each procedure in retrieving the orbital contents and restoring the original shape of the wall. A transconjunctival approach provides sufficient space for the insertion of a properly sized implant, while a transnasal approach can minimize traction injury when restoring the herniated soft tissue back into the orbit from the sinus (Fig. 2). To prevent undesired outcomes such as enophthalmos, it is important to restore the fractured orbital wall precisely in its original shape and to maintain the surgical result throughout the healing process. Most synthetic materials are sufficient to maintain their shape or position in an isolated small orbital wall fracture, but it is difficult in practice to span the wide defect in a large or combined fracture, especially in an inferomedial orbital wall fracture lacking an external bony support. Unlike other facial bone fractures, it is impossible to fixate the fracture rigidly in orbital wall injury due to the thinness of the fractured orbital wall and the shortage of soft tissue supplying blood circulation. Furthermore, a thin flexible implant covering the wide fracture gap tend to be displaced back into the paranasal sinuses, which would result in the unnoticed postoperative reherniation of the orbital tissue [5]. Therefore, if the bony defect was treated with an implant without bone restoration, it would increase the risk of delayed implant malposition and take a long time for the fracture healing that is induced by the osteoinduction of the synthetic implant.
With a dual approach, we were able to mobilize the fractured orbital wall back to its original position through transnasal manipulation as the sinus mucosa was attached. Therefore, it was expected it to heal primarily in relatively a shorter period of time, as an autologous muco-osteal flap underneath the implant. The porous polyethylene implant was placed in opposition to the intraorbital pressure from the orbital side and the Nasopore and a Foley catheter were used to support the restored orbital wall from the extraorbital sinus side. With these supports from the both side of the fracture, we could maintain the contact with porous implant with the restored bone and facilitate the orbital tissue ingrowth during the early bone healing. In addition, we could decrease the load to the orbital implant and use relatively smaller implant to bridging the entire fracture defect. Once bony continuity has been achieved, the protection of orbital pressure is no longer required and the risk of delayed implant displacement or reherniation is eliminated.
We used CT volume measurements and Hertel exophthalmometer to evaluate surgical outcomes in this study. The Hertel exophthalmometer is commonly used to measure enophthalmos, which is an indicator of the results of reconstructive surgery in blowout fractures. However, some researchers have objected to the use of the Hertel scale based on its low reliability and poor repeatability [6,7]. Furthermore, a globe depression could not be measured accurately in orbital fracture patients who had surgery within 7-10 days after the injury due to periorbital edema.
In the cases we examined, there were no significant changes in the Hertel scale, but the postoperative OVR decreased significantly in all groups (Tables 1, 2). The OVRs decreased after surgery more significantly in experimental group than control group and there was no patient whose OVR was under 100% postoperatively. As the postoperative enophthalmos is strongly related to the orbital volume [8], we expect our orbital wall restoring method to be effective in preventing late enophthalmos. Among three types of fracture, the preoperative orbit volume was most severely expanded in inferomedial wall fracture and least in medial wall fracture, which was statistically significant. As the risk of enophthalmos was expected to be higher in a severely expanded orbit, the orbital wall restoring surgery would be more required in inferomedial orbital wall fracture (Table 2).
Although our results indicate a perioperative OVR to be significantly decreased in experimental group, it is not established yet that the OVR can be a quantitative surgical guideline in blowout fracture surgery [6]. It is recommended that investigations with larger samples sizes be performed for more precise comparison between the two surgical methods.
In conclusion, our surgical results from 150 patients with pure unilateral blowout fractures suggest that the combination of transorbital and transnasal approach with additional supports from the maxillary or ethmoid sinuses was more effective in restoring the orbital volume than the conventional transorbital method, regardless of the type of fracture.
Footnotes
No potential conflict of interest relevant to this article was reported.
This article was presented in part at the 4th Research and Reconstructive Forum on April 3, 2014, in Busan, Korea.
References
- 1.Rodriguez ED, Dorafshar AH, Manson PN. Facial fractures. In: Neligan PC, editor. Plastic surgery: volume 3. Philadelphia: Elsevier Saunders; 2013. pp. 53–57. [Google Scholar]
- 2.Kakibuchi M, Fukazawa K, Fukuda K, et al. Combination of transconjunctival and endonasal-transantral approach in the repair of blowout fractures involving the orbital floor. Br J Plast Surg. 2004;57:37–44. doi: 10.1016/j.bjps.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Farwell DG, Strong EB. Endoscopic repair of orbital floor fractures. Facial Plast Surg Clin North Am. 2006;14:11–16. doi: 10.1016/j.fsc.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Shi W, Jia R, Li Z, et al. Combination of transorbital and endoscopic transnasal approaches to repair orbital medial wall and floor fractures. J Craniofac Surg. 2012;23:71–74. doi: 10.1097/SCS.0b013e318240c88e. [DOI] [PubMed] [Google Scholar]
- 5.Cho RI, Davies BW. Combined orbital floor and medial wall fractures involving the inferomedial strut: repair technique and case series using preshaped porous polyethylene/titanium implants. Craniomaxillofac Trauma Reconstr. 2013;6:161–170. doi: 10.1055/s-0033-1343785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oh SA, Aum JH, Kang DH, et al. Change of the orbital volume ratio in pure blow-out fractures depending on fracture location. J Craniofac Surg. 2013;24:1083–1087. doi: 10.1097/SCS.0b013e31828b6c2d. [DOI] [PubMed] [Google Scholar]
- 7.Musch DC, Frueh BR, Landis JR. The reliability of Hertel exophthalmometry. Observer variation between physician and lay readers. Ophthalmology. 1985;92:1177–1180. doi: 10.1016/s0161-6420(85)33880-0. [DOI] [PubMed] [Google Scholar]
- 8.Andrades P, Hernandez D, Falguera MI, et al. Degrees of tolerance in post-traumatic orbital volume correction: the role of prefabricated mesh. J Oral Maxillofac Surg. 2009;67:2404–2411. doi: 10.1016/j.joms.2008.11.024. [DOI] [PubMed] [Google Scholar]