Abstract
Objective
To investigate the feasibility of game-based robotic training of the ankle in children with cerebral palsy (CP).
Design
Case study, 12 weeks intervention, with no follow-up.
Setting
University research laboratory.
Participants
A referred sample of 3 children with cerebral palsy, age 7 to 12, all male were enrolled. Three completed the intervention.
Interventions
Participants trained on the RA CP system for 36 rehabilitation sessions (12 weeks, 3 times/week), playing two custom virtual reality games. The games were played while participants were seated, and trained one ankle at-a-time for strength, motor control, and coordination.
Main Outcome Measures
The primary study outcome measures were for impairment (DF/PF torques, DF initial contact angle and gait speed), function (GMFM) and quality of life (Peds QL). Secondary outcome measures relate to game performance (game scores as reflective of ankle motor control and endurance).
Results
Gait function improved substantially in ankle kinematics, speed and endurance. Overall function (GMFM) indicated improvements that were typical of other ankle strength training programs. Quality of life increased beyond what would be considered a minimal clinical important difference. Game performance improved in both games during the intervention.
Conclusions
This feasibility study supports the assumption that game-based robotic training of the ankle benefits gait in children with CP. Game technology is appropriate for the age group and was well accepted by the participants. Additional studies are needed however, to quantify the level of benefit and compare the approach presented here to traditional methods of therapy.
Keywords: ankle, cerebral palsy, gait, robotics, video games
Cerebral palsy (CP) is a non-progressive disorder with impaired motor function secondary to injury of the immature brain [1]. Its incidence is 2-3 per 1,000 live births [2], making cerebral palsy the most prevalent physical disability originating in childhood. While initially only the central nervous system (CNS) is damaged in CP, damage is eventually seen peripherally with growth and development of the child. The lack of selective muscle control, primitive reflex patterns for ambulation, and deficient equilibrium [3], among other manifestations of CP result in poor gait, diminished function and reduced quality of life.
A primary impairment in children with CP is muscle weakness [4, 5], with the ankle dorsiflexors and plantarflexors being weaker by about 30 to 35% compared to children without disability. No cure exists at this time for CP, but many treatments are used to improve gait and function. These include tendon lengthening [6], transfers, releases, selective dorsal rhizotomy [7], Botulinum toxin injections [8], Baclofen, stretching, casting, orthotics and robotic rehabilitation [9, 10, 11 ]. Recent results indicate that increases in ankle or knee strength after training can improve gait and function in children with CP [12, 13].
Virtual reality (VR) is known for its engaging, highly motivating and rich feedback on performance characteristics when used in therapy [14-16]. The first virtual rehabilitation system developed for the ankle was the RA [17], consisting of a small Stewart platform-type parallel pneumatic robot, combined with custom rehabilitation videogames written in WorldToolKit [18]. This earlier system was used successfully by patients chronic post-stroke and by those with musculoskeletal deficits [19, 20]. This work was followed by a controlled study on patients with chronic stroke, in which robotic rehabilitation integrating the RA custom rehabilitation games, was shown to be clinically more beneficial than robotic rehabilitation on the same RA in the absence of these video games [21].
More recently, researchers at Northeastern University developed NUVABAT (Northeastern U Virtual Ankle and Balance Trainer) [Ding et al. 2010]. This 2 DOF ankle co-robot is designed to provide passive resistance to one ankle, while the patient is either sitting or standing. Similar to the RA, this co-robot uses VR games, however no clinical data on patients is yet available. Deng an colleagues [2011] report on a randomized controlled study of ankle dorsiflexion (DF) training under home tele-rehabilitation of patients chronic post-stroke. Using a sensing orthosis and web camera, the patients had to either track complex wave curves displayed on the screen by moving their ankle, or do simple ankle movements. The participants in the complex tracking movement group had significantly larger DF gains vs. that of the simple movement group.
The purpose of the feasibility study described here was to determine if a revised RA robot (the RA CP) could improve ankle strength, motor control, gait, function, and quality of life in children with CP while playing custom VR games.
I. METHODS
A. Participants
Three children with CP participated in this investigation (see Table 1 for vital statistics). The children were enrolled in age-appropriate classes in regular public schools. They ambulated independently, two wearing shoe inserts, and one othotics. Parents reported they had difficulty walking in the community and often tripped and fell. Participants and their parents/legal guardians provided written informed consent/assent consistent with a study protocol approved by the institutional review boards of both ... University and .... University. Any therapy the participants were receiving before beginning the current study was continued during the experimental intervention.
TABLE I.
PARTICIPANTS CHARACTERISTICS PRE-INTERVENTION. © WASHINGTON UNIVERSITY IN ST. LOUIS AND RUTGERS UNIVERSITY TELE-REHABILITATION INSTITUTE. REPRINTED BY PERMISSION.
| Case | Age | Race | Gender | Height (cm) | Mass (kg) | Ambulation |
|---|---|---|---|---|---|---|
| 1 | 7 yr. | White | Male | 122 | 21.4 | Independent Shoe insoles |
| 2 | 11 yr. | White | Male | 134 | 27.3 | Independent Orthotics |
| 3 | 12 yr. | African American | Male | 148 | 55.9 | Independent Shoe insoles |
B. Data collection instruments
Clinical evaluation sessions occurred pre- and post-intervention, with 5 clinical outcome measures collected by a senior physical therapist (..) who is a co-author of this article. The standardized outcome measures used were: 1) ankle strength [22], 2) Gross Motor Function Measure (GMFM) [23], 3) maximum ankle dorsiflexion at initial contact during gait [24], 4) gait speed [24], and 5) quality of life using the Pediatric Quality of Life Inventory (PedsQL) [25, 26].
Ankle strength was assessed with a Kincom dynamometer (Chattanooga Group, Inc., Chattanooga, TN, Model, 125E+) [27]. Maximum concentric torque values were recorded for each ankle in dorsiflexion (Max DF) and plantarflexion (Max PF) over a full range of motion at 90°/s. A gait analysis video motion capture system (Motion Analysis Corp, Santa Rosa, CA, Model, Eagle Camera) [28] was used to determine gait speed and ankle dorsiflexion angle at initial contact (DF@IC).
The Gross Motor Function Measure (GMFM) is a standard criterion-referenced test designed to assess change in gross motor function in children with CP [29]. The 88 items of the test assess activities in five dimensions: 1) lying and rolling, 2) sitting, 3) crawling and kneeling, 4) standing, and 5) walking, running and jumping. Each item is scored using a 4-point Likert scale (0=does not initiate; 1=initiates; 2=partially completes; 3=completes). A child's totals from each category are divided by the total possible points for that category, to produce a category percentage score (maximum being 100%). These percentages can be used individually or can be averaged to yield an overall score. The percentage for the walk-run-jump and the standing components of GMFM were used as outcome measures in this study.
PedsQL measure was used to assess the quality of life of the participants based on child and parent self-reports [13]. The PedsQL includes 23 items that measure the physical, emotional, social and school functioning of children and adolescents, with an excellent reported reliability (0.88 child, 0.90 parent report). The measure has been shown to be valid distinguishing between healthy children and children with acute and chronic health conditions. The threshold for clinical significance (minimal improvement) is 4.5 points for the parent report and 4.4 points for the child report.
The experimental system used in training included a PC workstation running the two custom rehabilitation games. It stored game performance data transparently and uploaded it on a remote clinical server. Thus in addition to the primary outcome measures listed above, secondary (computer measured) outcomes relate to game performance, in terms of game scores. The scores reflect ankle control and endurance capability, and were measured separately for each ankle, when used to play the games described below.
C. Intervention
1) Experimental system
The RA CP system used in the intervention is shown in Figure 1. It consisted of a small prototype robot on which the patient placed the foot to be trained, a multi-core PC workstation which received data from the robot, and used those data to alter the state of virtual reality simulations, a custom controller box interface between the PC and the robot [30], and an air compressor (not shown).
Fig. 1.
The Rutgers Ankle CP: a) system installed at the clinical site; b) foot adapter. © Rutgers University Tele-Rehabilitation Institute and Washington University in St. Louis. Reprinted by permission.
The RA CP had a pneumatic Stewart platform parallel configuration, capable of measuring all six degrees of freedom of the foot, as well as providing controlled resistive forces and torques. The top platform of the robot had a custom ankle angle adapter and a snowboard foot binding which allowed attachment of the patient's foot to the top platform of the robot (Figure 1b). The adapter was designed at Washington University in St. Louis, to permit a more comfortable seating of the participant while playing the games. The adapter kept the patient's foot at 45° to 90° relative to the top platform. It should be noted that while the robot had the capability to train for ankle eversion and inversion also, for simplicity, it was decided not to include that in the protocol.
The custom controller box was a complete redesign of the older RA controller [19], creating a more powerful reaction force, more accurate kinematics, and reducing air consumption. It incorporated an Intel dual core processor with microcontrollers to drive the air servo-valves at a control loop frequency of 200 Hz. The controller software was developed in Java running on a Linux OS. The communication between the robot controller box and the PC was done over a serial line. Further technical details on the experimental system can be found in [31, 32].
2) Rehabilitation games
The therapy was in the form of engaging games that needed to respond promptly to the patient's ankle movements. The system software components running on the PC workstation were the Scheduler, the session Baseline, the Airplane and Breakout 3D games. The software was developed in Java and Java3D API [33], running on a Windows XP operating system.
The Scheduler module allowed the therapist to define the game sequence and difficulty progression for each participant and each ankle. This was done by setting the number of games in a session, their order, difficulty parameters for each game, the total session time and rest period duration between games.
Each session started with a baseline which measured the ankle mobility for the current rehabilitation session based on two parameters: dorsiflexion and plantarflexion movement. The ankle excursion in plantarflexion and dorsiflexion were then used to automatically adapt the games to each participant, for each training session. This adaptation mapped the physical movement of the ankle to the movement of the avatar it controlled, such that the avatar could travel the full extent of the virtual scene, even for small the physical movements.
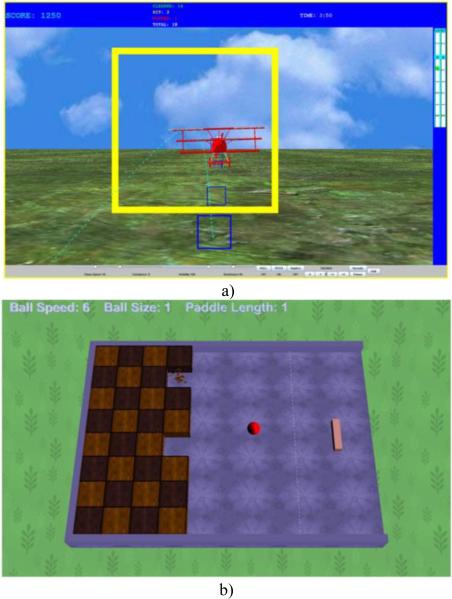
In the Airplane exercise (Figure 2a) the participant piloted a virtual airplane avatar through a series of target frames colored yellow. The position of the frames followed an unpredictable curved path with hills and valleys, which required repeated plantarflexions and dorsiflexions of the ankle. At the beginning of the exercise the therapist chose the airplane velocity, the degree of air turbulence, the scene visibility, and the exercise time. Longer exercises required more ankle endurance, while faster planes required better motor control to succeed in passing through the target frames. Visibility was controlled such that fog reduced the visual flow, and turbulence (during simulated storms) created disturbances (vibrations) that the participant had to overcome to pass through the targets. This was meant to be an interactive way to improve ankle control. The game score was based on the number of frames passed (100 points for a clear pass though, −25 points for the plane hitting the frame with a wingtip, and −75 points for a total miss, when passing outside the frame). Target accuracy was recorded as the number of targets correctly cleared, targets hit and targets completely missed.
Fig. 2.
Game starting screens: a) Airplane game, b) Breakout 3D game in the configuration used to train the right ankle. © Rutgers University Tele-Rehabilitation Institute. Reprinted by permission.
The Breakout 3D exercise (Figure 2b) is a modified version of the well-known Breakout arcade game [34]. The participants controlled a paddle avatar to rebound balls towards a wall of bricks, which were destroyed when the balls made contact with the wall. Unlike the arcade version of the game, only one brick could be destroyed for each rebound from the paddle, so to maximize the necessary ankle movements needed to destroy all the bricks. The difficulty of the game was dependent on the speed of the ball, the size of the paddle, and the number of bricks in the wall. Faster balls and smaller paddles required higher eye-foot coordination, and more bricks corresponded to higher number of repetitions. The score was incremented by 1 for each brick destroyed, and the number of balls lost (when missed by the paddle and leaving the virtual table) was counted and saved as a performance parameter. Unlike the Airplane game which had one configuration irrespective of which ankle was trained, the location of the brick changed. When training the right ankle the game presented the brick wall to the left of the screen, and vice versa for the left ankle. Accuracy was recorded as success rate in the percentage of bricks removed from the wall in a set amount of time, and the number of balls used to do so.
3) Training sessions
The participants warmed up at the start of each session with a 2-minute walk. Next, they were seated comfortably on a rehabilitation chair, secured in place using a pelvic strap and a mid-thigh strap on the exercising extremity. The knee joint was positioned at approximately 90° of flexion and the active ankle range of motion limits in dorsiflexion and plantarflexion were established. The participants then exercised on the RA CP by playing alternating Airplane and Breakout 3D games displayed on the PC screen. A single game lasted approximately 5 minutes, with each game alternating two times per side (left ankle and right ankle) for a total training time of at least 20 minutes/ankle, or 40 minutes/session.
Training difficulty was progressed such that in the first session the Airplane game was played at 100% visibility, 0% turbulence and 25% of maximum airplane speed. Once the participants missed 0 targets and hit less than 3 targets per game, the airplane speed was increased. By the final session the participants were training at 0% visibility (only the proximal target was visible on a dark and stormy sky), 75% turbulence and 100% speed.
For the first session of the Breakout 3D game, the ball speed was slowest (level 1), the paddle longest (level 1) and there were fewest bricks to destroy (level 1). By the final session, the participants were training with the ball highest speed (level 6), a shorter paddle (level 2) and had more bricks to destroy (level 2). The robot resistance level was kept fixed for the duration of training. Participants trained for 36 sessions (three times per week for 12 weeks). Any session missed during the 12 week training were made up at the end of the 12 weeks.
II RESULTS
A. Clinical Outcomes
Strength increases were seen in 5 out of 6 possible cases for maximum DF and PF torques (Table 2). All children increased in PF strength with an overall average of 0.15 Nm/kg. The largest increase occurred in Participant 1 (0.19 Nm/kg) and the smallest occurred in Participant 2 (0.09 Nm/kg). Participant 1 had the largest increase in DF strength (0.26 Nm/kg) followed by Participant 3 (0.12 Nm/kg). Participant 2 had a decrease in DF strength (−0.12 Nm/kg). The average change for DF strength indicated an increase of 0.06 Nm/kg.
TABLE II.
CLINICAL OUTCOMES FOR STRENGTH, GAIT, GROSS MOTOR FUNCTION AND QUALITY OF LIFE FOR THREE CHILDREN WITH CEREBRAL PALSY, BEFORE AND AFTER TRAINING ON THE RUTGERS ANKLE CP SYSTEM. GMFM - GROSS MOTOR FUNCTION MEASURE, PEDSQL - PEDIATRIC QUALITY OF LIFE INVENTORY. PRE – PRE INTERVENTION, POST-POST INTERVENTION. © WASHINGTON UNIVERSITY IN ST. LOUIS AND RUTGERS UNIVERSITY TELE -REHABILITATION INSTITUTE. REPRINTED BY PERMISSION.
| Strength | Gait | GMFM | PedsQL | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case | Max DF (Nm/Kg) | Max PF (Nm/Kg) | DF@IC (°) | * | Speed (cm/s) | ** | walk/run/jump (%) | Standing(%) | Child (%) | Parent (%) | ||||||||
| Pre- | Post- | Pre- | Post- | Pre- | Post- | Norm | Pre- | Post- | Norm | Pre- | Post- | Pre | Post- | Pre- | Post- | Pre- | Post- | |
| 1 | 0.27 | 0.53 | 2.39 | 2.58 | −4 | 5 | −2 (3) | 98.7 | 120.0 | 116 (9) | 94.4 | 98.6 | 100 | 97.4 | 85.7 | 91.4 | 79.3 | 85.0 |
| 2 | 0.50 | 0.38 | 1.72 | 1.81 | 1.5 | 4 | −2(3) | 40.5 | 53.4 | 116 (9) | 63.9 | 66.7 | 74.4 | 79.5 | 60.0 | 65.0 | 39.3 | 39.3 |
| 3 | 0.24 | 0.36 | 1.33 | 1.49 | −4.0 | −3.5 | −2(3) | 100. | 99.0 | 116 (9) | 80.6 | 79.2 | 71.8 | 79.5 | 83.6 | 81.4 | 73.6 | 75.0 |
[24]
[51]
Dorsi-flexion angle at initial contact during gait indicated a change from 4° of PF to 5° of DF for Participant 1 (Table 2). There was little change in the other two participants. Gait speed improved on average by 11.06 cm/s, with Participants 1 and 2 improving in the gait speed, while Participant 3 speed remaining essentially the same (a reduction of 1 cm/s after training).
The walk/run/jump subset of GMFM improved in Participants 1 and 2 and had a reduction of less than 1 % for Participant 3. The GMFM Standing had a reduction of 2.6% for Participant 1, however it improved for Participants 2 and 3 by 5.1% and 7.7%, respectively.
B. Quality of life outcomes
The Pediatric Quality of Life self report for child improved on average by 2.8%. Based on the instrument's 4.5 points threshold for minimal clinical important difference reported in literature [25], the improvement in the participant's quality of life had clinical significance for Participants 1 and 2 (5.7% and 5% respectively). Participant 3 had a reduction of 2.2%, which is not clinically significant. Parent PedsQL report showed an improvement averaging 2.4%, with a clinically significat increase only for Participants 1 (5.7%).
C. Game performance
1) Airplane Game
All participants improved in Airplane game score (Figure 3) over the course of therapy. They were able to clear the targets despite an increase of 200% (Participant 1) to 400% (Participants 2 and 3) in airplane speed. Since the number of targets to clear depended on the airplane speed, there is an observed proportionality between game score and airplane speed. However, there are also portions where there was an improvement in score when the airplane speed was kept constant over a number of sessions. This is reflective of improved motor control and ankle speed of DF/PF movement. Furthermore, there was a progressive increase in the number of targets cleared, from 40 to 160 per game. This is indicative of increased ankle endurance and number of repetitions (discussed later in this section).
Fig. 3.
Participants performance in the Airplane game: a) Participant 1; b) Participant 2); c) Participant 3. © Rutgers University Tele-Rehabilitation Institute. Reprinted by permission.
2) Breakout 3D Game
All participants improved in the Breakout 3D game scores as well. The game score being directly proportional with the number of bricks destroyed means that they improved their motor control by bouncing balls of increasing velocity, and with smaller paddle avatars. One can argue that the number of bricks destroyed was due to increased ball velocities (participant got to destroy more bricks before the game timed out). However, there were session sequences where the ball speed was kept unchanged from session to session, but the score the number of bricks destroyed continued to improve (higher scores).
3) Number of repetitions
The number of repetitions (defined as the movement from neutral to max DF and back or from neutral to max PF and back) increased. Counting only the targets cleared and considering there was one repetition per target, the number of repetitions per ankle increased from 40 to 150-160 for every Airplane game played. This 400% increase in number of repetitions resulted in a minimum of 300 repetitions per ankle per session playing this game.
For the Breakout 3D game, a repetition corresponded to a ball bounce, since the game allowed only one brick to be destroyed for every bounce off the paddle avatar. The children had an increase in number of cube destroyed from 32 to 50. This corresponds to a minimum of 64 to 100 repetitions playing the Breakout 3D game for every session and every ankle (not counting missed balls). Adding these repetitions to those playing the Airplane game, the participants executed about 400 repetitions per ankle per session at the end of therapy.
4) Technology acceptance
The training sessions required direct supervision from a therapist for setup and progression of each game depending on the child's performance. The patients were motivated to exercise for the required duration and there was good compliance with the protocol. Once maximum game difficulty was attained, the patients wanted to be challenged more and expressed a desire for new games. In general, and based on prior research [35], it is believed that lengthy game-based interventions of pediatric populations need to constantly introduce new games, so to maintain participant's motivation. Children as young as 4-6 years old may be able to perform these tasks. They need to be able to follow commands such as “push down on your toes to make the plane move down so it can go through a target.”
III DISCUSSION
Virtual reality game therapy for the lower extremity has been facilitated by the introduction of the Wii Balance Board (WBB). It was found to have concurrent validity for the (much more expensive) force plates used to measure the center of pressure while the patient is standing [Clark 2010]. The WBB low cost, good sensitivity to body posture and available games makes it ideal for balance rehabilitation, A control study on adults with acquired brain injury playing custom VR games while standing on the board showed that their standing balance was substantially improved [Gil-Gomez 2011]. However, the WBB would not have been useful in the present study which targeted gate.
The first paediatric trial aimed to determine the feasibility of robotic-assisted treadmill training in children with central gait impairment was done on the pediatric Lokomat (Hocoma AG, Switzerland) – a two-leg driven orthotic exoskeleton adjustable to the anatomy of a patient [11]. Nine out-patients trained for an average of 12 sessions of about 29 minutes each, practicing walking on a treadmill while partially un-weighted. Patients’ gait improved significantly with the mean gait speed increasing 0.22 m/s (from 0.87m/s to 1.09m/s). This is a larger improvement than that obtained with our system, which trained one ankle at-a-time. It is possible that the larger effect in the Lokomat study was due in part to the bilateral training which the Lokomat allows, thus providing a more ecological therapy than that possible on the RA CP. A more recent study on the Lokomat showed that pediatric patient motivation was maintained by the introduction of virtual reality game-like environments [36]. This is similar to our finding that game play-based rehabilitation benefitted from the motivational aspect of virtual reality.
Researchers at the Rehabilitation Institute of Chicago [37] developed a novel portable robot with which they trained 12 children with CP during 18 sessions (3 sessions/wk for 6 wk). Each session consisted of 20 minutes of passive stretching done by the robot, followed by 30 minutes of active movement training and ended with 10 minutes of passive stretching. Results showed significant improvements in passive and active ranges of motion, selective motor control and mobility functions. Ankle DF strength increased 1.7 Nm (from a mean of 2.9 Nm, before to 4.6 Nm after training). This represents a larger gain than obtained with the RA CP, which had a small resistance setting due to controller box malfunction.
The average increase in strength of the plantarflexors (0.38 Nm/kg) in our study was close to those previously recorded for trained plantarflexor muscles (0.4 Nm/kg) in children training for the same amount of time on a Kincom dynamometer [24]. However Participant 2 had a PF strength increase of 0.82 Nm/kg, double that reported for the Kincom. The average increase in strength of the dorsiflexors (0.23 Nm/kg) was slightly larger than those previously recorded for trained dorsiflexor muscles (0.22 Nm/kg) in children training on the Kincom dynamometer [13].
Baran [38] studied the effects of gait training with visual and auditory feedback cues on the walking abilities of patients with gait disorders due to cerebral palsy. Visual and auditory feedback cues were generated by a wearable accelerometry-driven device. On a group of 20 randomly selected patients with CP who trained with visual or auditory feedback cues there was a 21% to 25% improvement in walking speed. This relates to our study which provided visual and auditory cues as part of the games. Interestingly, while our participants trained in sitting, this transferred to gait speed improvements. There was substantial increase of 21 cm/s in gait speed for Participant 1, and 12.9 cm/s for Participant 2, while Participant 2 was slower by 1 cm/sec post-training.
Treatment effects on gait of children with CP were studied on an experimental group of 21 children who each received EMG biofeedback training plus conventional exercise program [39]. The control group consisted of 15 children who each received conventional exercise therapy only. Results showed there was an improvement in the experimental group active dorsiflexion range of motion of 8° when the knee was kept in flexion. Our participants also trained with the knee flexed. Their ankle kinematics indicated good progress for angle at initial contact in Participants 1 (9°) and 2 (2.5 °), with no progress for Participant 3.
Another study by our group [40] showed that a supported speed treadmill training exercise program for children with CP was not better than a program of exercise on spasticity, strength, motor control, gait spatiotemporal parameters, gross motor skills, and physical function in a sample of 26 children with spastic diplegia. In our study Participants 1 and 2 had a 4 point, and 3 point, respective improvement in the GMFM. This was about the same as that previously reported in children training for the same amount of time on a Kincom dynamometer [13].
The game performance results support the current theory about brain neuroplasticity indicating that hundreds of repetitions are required to bring about a change in a movement pattern [41]. It has been reported that only 10-40 repetitions are being performed during a typical therapy session in a clinic, far less than the needed hundreds [Lang et al., 2007]. Prescribing home therapy can augment the therapy performed in the clinic and boost the number of repetitions. Instead of non-motivational typical movement therapy, virtual reality game play is an engaging way to mediate the needed number of repetitions needed to induce neuro-plasticity. Our study gradated the number of repetitions per ankle, up to about 400 repetitions per ankle per session and well in line with current theory, with positive outcomes.
IV CONCLUSSIONS
The RA CP was used to train the ankle strength and function in three boys with CP during a 12 weeks (36 sessions) intervention. Assessments for impairment, function and quality of life were taken before and after training, with no follow up. Results indicated varying degrees of improvement in ankle strength, gait kinematics and speed. Overall function (GMFM) indicated improvements that were typical of other ankle strength training programs. Quality of life increased in some participants. Improvements measured by clinical evaluations mapped to improved game performance. The RA CP system induced up to 400 repetitions for every ankle and session of game play. This amount is viewed as needed to induce neural plasticity. While these results are only for three participants, they are encouraging and indicative of improvement in ankle function and quality of life of children with CP. The procedure followed in this study is a first step in the suggested clinical trial procedure [(Robey & Schultz, 1998; Rodriguez & Rothi, 2008; Rothi, 2006; Onken, Blaine, & Battjes, 1997]. The study is a proof of concept in which investigators used sensitive measures to determine if there is a treatment effect. Further research with a larger number of participants is needed.
Study limitations
The main limitations of this study were the small number of subjects, lack of follow up and lack of a control group. Another limitation is that the therapist performing the clinical evaluations was not blinded to the training protocol.
Suppliers’ List.
Dell Precision 690 Dell Marketing LP, Higher Education Sales, 1 Dell Way Round Rock, TX 78682.
Eagle Digital Real Time System. Motion Analysis Co, 3617 Westwind Boulevard, Santa Rosa, CA USA 95403.
Java3D API; Java SE Desktop Technologies, Sun Microsystems, Inc, 4150 Network Circle, Santa Clara, CA 95054.
The PaedsQL™ Measurement Model for the Pediatric Quality of Life Inventory. Mapi Research Institute, 27 rue de la Villette, 69003 Lyon, France. http://www.pedsql.org/
System 3 Chair, Biodex Medical Systems Inc, 20 Ramsay Rd, Shirley, NY 11967-0702.
World Toolkit software; SENSE8 Product Line http://www.sense8.com.
Fig. 4.
Participants performance in the Breakout 3D game: a) Participant 1; b) Participant 2); c) Participant 3. © Rutgers University Tele-Rehabilitation Institute. Reprinted by permission.
List of abbreviations
- API
Application Programmer's Interface
- CNS
central nervous system
- CP
cerebral palsy
- DF
dorsiflexion
- GMFM
Gross Motor Function Measure
- IC
Initial Contact
- OS
Operating System
- PC
Personal Computer
- PedsQL
pediatric quality of life
- PF
plantarflexion
- RA
blinded
- RACP
blinded
- VR
virtual reality
- WBB
Wii Balance Board
Contributor Information
Grigore C. Burdea, Tele-Rehabilitation Institute, Rutgers University, Piscataway, NJ 08854 USA.
Daniel Cioi, Department of Electrical and Computer Engineering, Rutgers University, Piscataway, NJ 08854 USA.
Angad Kale, Department of Electrical and Computer Engineering, Rutgers University, Piscataway, NJ 08854 USA.
William E. Janes, Human Performance Laboratory, Washington University in St. Louis, St. Louis, MO 63130 USA
Sandy A. Ross, Human Performance Laboratory, Washington University in St. Louis, St. Louis, MO 63130 USA
Jack R. Engsberg, Human Performance Laboratory, Washington University in St. Louis, St. Louis, MO 63130 USA
REFERENCES
- 1.Ingram TTS. A Historical Review of the Definition of Cerebral Palsy. In: Stanley FAE, editor. The Epidemiology of the Cerebral Palsies. Lippincott Co; Philadelphis, PA.: 1984. pp. 1–11. [Google Scholar]
- 2.Rosen MG, Dickinson JC. The incidence of cerebral palsy. Am J Obstet. Gynecol. 1992;167:417–423. doi: 10.1016/s0002-9378(11)91422-7. [DOI] [PubMed] [Google Scholar]
- 3.Gage JR. Gait Analysis in Cerebral Palsy. Mac Keith Press; NY.: 1991. [Google Scholar]
- 4.Damiano DL, Vaughan C, Abel MF. Muscle response to heavy resistance exercise in children with spastic cerebral palsy. Dev Med Child Neurol. 1995;37:731–739. doi: 10.1111/j.1469-8749.1995.tb15019.x. [DOI] [PubMed] [Google Scholar]
- 5.1998 ...... Maximum .... J Applied Biomechanics. [Google Scholar]
- 6.Ganjwala D. Multilevel orthopedic surgery for crouch gait in cerebral palsy: An evaluation using functional mobility and energy cost. Indian J Orthop. 2011 Jul;45(4):314–9. doi: 10.4103/0019-5413.82334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tedroff K, Löwing K, Jacobson DN, Åström E. Does loss of spasticity matter? A 10-year follow-up after selective dorsal rhizotomy in cerebral palsy. Dev Med Child Neurol. 2011 Aug;53(8):724–9. doi: 10.1111/j.1469-8749.2011.03969.x. doi: 10.1111/j.1469-8749.2011.03969.x. Epub 2011 May 18. [DOI] [PubMed] [Google Scholar]
- 8.Friedman BC, Goldman RD. Use of botulinum toxin A in management of children with cerebral palsy. Can Fam Physician. 2011 Sep;57(9):1006–73. [PMC free article] [PubMed] [Google Scholar]
- 9.Smania N, Gandolfi M, Marconi V, Calanca A, et al. Applicability of a new robotic walking aid in a patient with cerebral palsy. Eur J Phys Rehabil Med. 2011 May 23; [PubMed] [Google Scholar]
- 10.Roy A, Krebs HI, Williams DJ, Bever CT, et al. Robot-Aided Neurorehabilitation: A Novel Robot for Ankle Rehabilitation. IEEE Trans Robotics. 2009;25(3):569–582. [Google Scholar]
- 11.Meyer-Heim A, Borggraefe I, Ammann-Reiffer C, Berweck S, et al. Feasibility of robotic assisted locomotor training in children with central gait impairment. Developmental Medicine & Child Neurology. 2007;49:900–906. doi: 10.1111/j.1469-8749.2007.00900.x. [DOI] [PubMed] [Google Scholar]
- 12.Dodd KJ, Taylor NF, Graham HK. A randomized clinical trial of strength training in young people with cerebral palsy. Dev Med Child Neuro. 2003;45:652–657. doi: 10.1017/s0012162203001221. [DOI] [PubMed] [Google Scholar]
- 13.Pediat Phys Ther. 2006 ....... Ankle .... [Google Scholar]
- 14.Hodges L, Anderson P, Burdea G, Hoffman H, et al. Treating Psychological and Physical Disorders with VR. IEEE Computer Graphics Applications. 2001 Nov-Dec;:25–33. [Google Scholar]
- 15.J Methods Information Medicine. 2003 ..... Keynote Address: .... [Google Scholar]
- 16.Rizzo A, Kim GJ. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence. 2005;14(2):119–146. [Google Scholar]
- 17.Proc ASME Haptics Symposium. 1999 ....... The ..... Interface. [Google Scholar]
- 18.Engineering Animation Inc . WorldToolKit Reference Manual Release 9. Mill Valley CA: 1999. www.cs.princeton.edu/courses/archive/spr01/cs598b/papers/wtkr9.pdf. [Google Scholar]
- 19.Proc Virtual Reality. 2000 ...... Orthopedic .... Interface. [Google Scholar]
- 20.MIT Press; 2001. ...... Post-Stroke ...... .... Presence. [Google Scholar]
- 21.Mirelman A, Bonato P, Deutsch JE. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke. 2009 Jan;40(1):169–74. doi: 10.1161/STROKEAHA.108.516328. [DOI] [PubMed] [Google Scholar]
- 22.Dev Med Child Neurol. 2000 ....... Ankle ..... cerebral palsy. [Google Scholar]
- 23.J Applied Biomechanics. 2008 ....... A measure ....... cerebral palsy. [Google Scholar]
- 24.J Neurosurgery. 2006 ..... The efficacy ..... cerebral palsy. [Google Scholar]
- 25.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3(6):329–341. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 26.Varni JW. The PaedsQL™ Measurement Model for the Pediatric Quality of Life Inventory. 2011 doi: 10.1097/00005650-199902000-00003. http://www.pedsql.org/ [DOI] [PubMed]
- 27.National Health and Nutrition Examination Survey Muscle Strength Procedures Manual. 2011 http://www.cdc.gov/nchs/data/nhanes/nhanes_01_02/muscle_strength_year_3.pdf.
- 28.Motion Analysis Co. Eagle Digital Real Time System. 2011 http://www.motionanalysis.com/html/movement/eagle.html.
- 29.Thompson P, Beath T, Bell J, Jacobson G, et al. Test-retest reliability of the 10-metre fast walk and 6 minute walk test in ambulatory school-aged children with cerebral palsy. Dev Med and Child Neurol. 2008;50:370–376. doi: 10.1111/j.1469-8749.2008.02048.x. [DOI] [PubMed] [Google Scholar]
- 30.... Advanced ... ‘RA CP’ Controller Interface, ..... Master of Science. ... University. December .....
- 31.Proc. Int. Conf. 2011:654–659. ...... Ankle Control .... the RA CP - .... Digital ... [Google Scholar]
- 32...... The RA CP ... design. IEEE ...... submitted.
- 33.Sun Microsystems Java 3D API Tutorial. 2000 http://java.sun.com/developer/onlineTraining/java3d/
- 34.Atari Inc. Breakout Operations, Maintenance, Service Manual. 1976 http://www.cityofberwyn.com/manuals/Breakout.pdf.
- 35.IEEE Trans. 2010 ...., et al. Feasibility ..... .... .... cerebral palsy. [Google Scholar]
- 36.Brűtsch K, Koenig A, Zimmerli L, et al. Virtual Reality for Enhancement of Robot- Assisted Gait Training in Children with Neurological Gait Disorders. J Rehabil Med. 2011;43(6):493–499. doi: 10.2340/16501977-0802. [DOI] [PubMed] [Google Scholar]
- 37.Wu YN, Hwang M, Ren Y, Gaebler-Spira DJ, et al. Combined passive stretching and active movement rehabilitation of lower-limb impairments in children with cerebral palsy using a portable robot. Neurorehabil Neural Repair. 2011 May;25(4):378–85. doi: 10.1177/1545968310388666. Epub 2011 Feb 22. [DOI] [PubMed] [Google Scholar]
- 38.Baram Y, Lenger R. Gait improvement in patients with cerebral palsy by visual and auditory feedback. Proc. Virtual Rehabilitation International Conf. 2009:146–149. [Google Scholar]
- 39.Dursun E, Dursun N, Alican D. Effects of biofeedback treatment on gait in children with cerebral palsy. Disability and Rehabilitation. 2004;26(2):116–120. doi: 10.1080/09638280310001629679. [DOI] [PubMed] [Google Scholar]
- 40.Johnston TE, Watson KE, Ross SA, et al. Effects of a supported speed treadmill training exercise program on impairment and function for children with cerebral palsy. Dev Med Child Neurol. 2011 Aug;53(8):742–750. doi: 10.1111/j.1469-8749.2011.03990.x. [DOI] [PubMed] [Google Scholar]
- 41.Nudo RJ. Remodeling of cortical motor representations after stroke: implications for recovery from brain damage. Mol Psychiatry. 1997 May;2(3):188–91. doi: 10.1038/sj.mp.4000188. [DOI] [PubMed] [Google Scholar]
- Ding Y, Sivak M, Weinberg B, et al. NUVABAT: Northeastern University Virtual Ankle and Balance Trainer. Proc. IEEE Haptics Symposium. 2010:509–514. http://ieeexplore.ieee.org/xpl/freeabs_all.jsp?arnumber=5444608.
- Lang CE, MacDonald JR, Gnip C. Counting repetitions: An observational study of outpatient therapy for people with hemiparesis post-stroke. Journal of Neurologic Physical Therapy. 2007;31:3–10. doi: 10.1097/01.npt.0000260568.31746.34. [DOI] [PubMed] [Google Scholar]
- Onken LS, Blaine JD, Battjes R. Behavioral therapy research: A conceptualization of a process. In: Henngler SW, Amentos R, editors. Innovative approaches from difficult to treat populations. American Psychiatric Press; Washington, DC: 1997. pp. 477–485. [Google Scholar]
- Robey RR, Schultz MC. A model for conducting clinical-outcome research: An adaptation of the standard protocol for use in aphasiology. Aphasiology. 1998;12:787–810. [Google Scholar]
- Rodriguez AD, Rothi LJ. Principles in conducting rehabilitation research. In: Stuff DT, Gordon W, Robertson I, editors. Cognitive neurorehabilitation, evidence and applications. 2nd ed. Cambridge University Press; New York, NY: 2008. pp. 79–90. [Google Scholar]
- Rothi LJ. Cognitive rehabilitation: The role of theoretical rationales and respect for the maturational process needed for our evidence. Journal of Head Trauma Rehabilitation. 2006;21:194–197. doi: 10.1097/00001199-200603000-00011. [DOI] [PubMed] [Google Scholar]
- Clark RA, Bryant AL, Pua Y, McCrory P, Bennell K, Hunt M. Validity and Reliability of the Nintendo Wii Balance Board for assessment of standing posture. Gait & Posture. 2010;31:307–310. doi: 10.1016/j.gaitpost.2009.11.012. [DOI] [PubMed] [Google Scholar]
- Gil-Gómez JA, Lloréns R, Alcañiz M, Colomer C. Effectiveness of a Wii balance board- based system (eBaViR) for balance rehabilitation: a pilot randomized clinical trial in patients with acquired brain injury. Journal of Neuroengineering and Rehabilitation. 2011;8:30. doi: 10.1186/1743-0003-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]