Abstract
Current analgesics predominately modulate pain transduction and transmission in neurons and have limited success in controlling disease progression. Accumulating evidence suggests that neuroinflammation, which is characterized by infiltration of immune cells, activation of glial cells and production of inflammatory mediators in the peripheral and central nervous system, has an important role in the induction and maintenance of chronic pain. This review focuses on emerging targets such as chemokines, proteases and the Wnt pathway that promote spinal cord neuroinflammation and chronic pain. It also highlights the anti-inflammatory and pro-resolution lipid mediators that act on immune cells, glial cells and neurons to resolve neuroinflammation, synaptic plasticity and pain. Targeting excessive neuroinflammation could offer new therapeutic opportunities for chronic pain and related neurological and psychiatric disorders.
Chronic pain is a rising health problem that could affect up to 30% adults in the world, but current treatments — such as opioids and non-steroidal anti-inflammatory drugs — are inadequate1. Several different types of pain make up chronic pain, including inflammatory pain following tissue injury (e.g., arthritis) 2, 3, cancer pain 4, 5 and neuropathic pain following nerve injury, spinal cord injury and brain injury (e.g., stroke and trauma) 6–9. Chronic pain is typically characterized by hyperalgesia, which is an increased response to noxious thermal and mechanical stimuli and allodynia in which nociceptive responses occur to normally innocuous stimuli such as light touch (known as mechanical allodynia). Neuropathic pain is also characterized by burning pain, paresthesia (a sensation of tingling, tickling, prickling and pricking) and dysesthesia (an unpleasant, abnormal sense of touch).
It is generally understood that chronic pain results from altered neuronal activity (that is, neuronal plasticity). This altered activity includes the sensitization of peripheral primary sensory neurons in the dorsal root ganglia and trigeminal ganglia 10–12 and the sensitization of central nociceptive neurons in the spinal cord, trigeminal nucleus, brain stem and cortex 13, 14. These actions in the peripheral nervous system (known as peripheral sensitization) and central nervous system (known as central sensitization) mean that an individual has a heightened perception of pain.
Pain is one of the cardinal features of inflammation. It is well established that inflammatory mediators released locally after tissue injury — including classic mediators (e.g., bradykinin, prostaglandins, H+, ATP, nerve growth factor), pro-inflammatory cytokines and chemokines as well as emerging mediators (bacterial N-formylated peptides15 and microRNAs16) — can directly stimulate and cause sensitization of pain-sensing nociceptors located at nerve fibers of primary afferent neurons in peripheral tissues10 (Fig. 1). Therefore, acute inflammation is intimately linked with the development of acute pain.
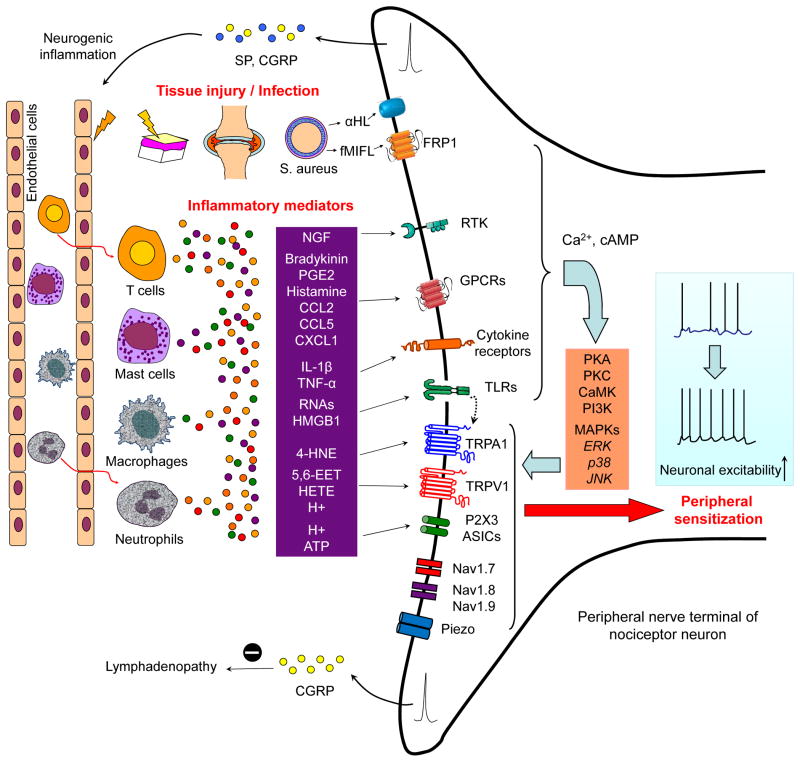
Figure 1. Inflammation elicits pain via inflammatory mediators and peripheral sensitization.
Tissue injury and infection cause inflammation via plasma extravasation and infiltration of immune cells such as macrophages, T cells, and neutrophils into the damaged tissue. The infiltrated immune cells and resident cells including mast cells, macrophages and keratinocytes release several inflammatory mediators, such as bradykinin, prostaglandins, H+, ATP, nerve growth factors (NGF), pro-inflammatory cytokines (TNF-α, IL-1β, IL-6), and proinflammatory chemokines (CCL2, CXCL1, CXCL5). Nociceptor neurons express the receptors for all these inflammatory mediators, which act on their respective receptors on peripheral nociceptor nerve fibers. These receptors include GPCRs, ionotropic receptors, and tyrosine kinase receptors, and their activation results in the generation of second messengers such as Ca2+ and cAMP, which in turn activates several kinases, such as the PKA, PKC, CaMK, PI3K, and MAPKs (ERK, p38, and JNK). Activation of these kinases causes hypersensitivity and hyperexcitability of nociceptor neurons (known as peripheral sensitization), through modulation of key transduction molecules such as transient receptor potential ion channel A1 and V1 (TRPA1 and TRPV1) and Piezo (a stretch-activated ion channel) as well as key conduction molecules such as the sodium channels NaV1.7, NaV1.8 and NaV1.9. Nociceptor neurons also express TLRs (that is, TLR3, TLR4, and TLR7), which can be activated by exogenous ligands (known as pathogen-activated molecular patterns, which include viral and bacterial components) and endogenous ligands (known as danger-activated molecular patterns, such as RNAs). Certain miRNAs (e.g., let-7b) serve as novel pain mediators to activate nociceptors via TLR7 which is coupled with TRPA1 (the coupling is further enhanced when TLR7 is activated by let-7b). Bacterial infection (with Staphylococcus aureus) also directly activates nociceptors and induces neuronal hyperexcitability via releasing bacterial N-formylated peptides (FPs) and the formation of pore-forming toxin α-haemolysin (α-HL). Activation of nociceptors also releases substance P and CGRP which are involved in the generation of neurogenic inflammation. CGRP also negatively regulates lymphadenopathy after inflammation.
Hyperactivity of primary sensory neurons following peripheral inflammation will also increase the release of neurotransmitters (e.g., glutamate) and neuromodulators such as substance P, calcitonin gene-related peptide (CGRP) and brain-derived neurotrophic factor (BDNF) from the central terminals of primary afferents in the spinal cord and trigeminal nucleus, causing hyperactivity of postsynaptic nociceptive neurons, i.e. central sensitization 17. In particular, central sensitization is responsible for the secondary pain outside the initial injury site 17, 18. Activation of NMDA receptors and mitogen activated protein kinases have an important role in central sensitization and pain hypersensitivity 19–21.
While acute inflammation produces transient central sensitization, chronic pain is associated with a long-lasting and even permanent central sensitization that persists after acute inflammation has been resolved 22. For example, Toll-like receptor 4 (TLR4) expressed in the spinal cord was shown to mediate the transition from acute to persistent mechanical hypersensitivity after the resolution of inflammation in a rodent model of arthritis 22. Pain and inflammation can also be dissociated in other conditions, for example periodontal disease (which occurs as a result of chronic inflammation) is not normally associated with pain.
Recent progress indicates that the development of neuroinflammation — inflammation of tissue within the peripheral nervous system (PNS) and central nervous system (CNS) — is responsible for generating and sustaining the sensitization of nociceptive neurons 23, 24 that leads to chronic pain. Therefore, targeting the processes and molecules that are involved in neuroinflammation could lead to better treatments for chronic pain.
Neuroinflammation
As well as having a key role in the development of chronic pain, increasing evidence suggests that neuroinflammation is an underlying cause of several CNS diseases including Alzheimer’s disease, Parkinson’s disease, multiple sclerosis and psychiatric disorders 25. However, there is controversy as to whether neuroinflammation has a detrimental or beneficial role in the pathology of CNS diseases 26, 27, depending on whether proinflammatory mediators (detrimental) versus anti-inflammatory mediators and /or growth factors (beneficial) are produced at different stages of neuroinflammation. Of note, there are clear differences between CNS neuroinflammation in neurodegenerative diseases and that in chronic pain after peripheral injury (Box 1).
Box-1. Neuroinflammation in neurodegenerative diseases and in chronic pain.
There are clear differences between CNS neuroinflammation in neurodegenerative diseases (e.g., Alzheimer’s disease) and that in chronic pain following peripheral injury. Neuroinflammation in neurodegenerative diseases and spinal cord injury is a result of direct damage to the CNS and will cause further neuronal degeneration and cell death (secondary injury) 25. In chronic pain (namely neuropathic and inflammatory pain), neuroinflammation is often the result of a peripheral damage and excessive neuronal activity of primary sensory neurons. Therefore, CNS neuroinflammation after peripheral injury is relatively mild and does not cause marked neuronal loss 161, 162. There are also differences in the role of proinflammtory cytokines in neurodegenerative disease compared to inflammatory pain. Cytokines such as TNF-α and IL-1β cause neurodegeneration and impair memory and synaptic plasticity (such as LTP) in several brain regions (e.g., hippocampus and dentate gyrus) that are associated with brain dysfunction in neurodegenerative disease 163, 164. In contrast, TNF-α and IL-1β serve as neuromodulators in the spinal cord dorsal horn after peripheral injury and induce/enhance synaptic plasticity (e.g., LTP) and inflammatory and neuropathic pain 66, 165, 166. Of interest, neutralization of TNF-α has been shown to inhibit chronic pain in patients with rheumatoid arthritis much faster than it improves the signs of inflammation such as a reduction in joint swelling, probably by inhibiting TNF-α mediated nocicetive neurotransmission (synaptic plasticity) in the spinal cord dorsal horn prior to the improvement of inflammation 167.
Neuroinflammation occurs in the PNS (that is, peripheral nerves and ganglia) and CNS (that is, spinal cord and brain) and is characterized by infiltration of leukocytes and increased production of inflammatory mediators at these sites. The trafficking of different types of leukocytes in the PNS and CNS has distinct temporal profiles; the initial trafficking of neutrophils (hours) is followed by trafficking of macrophages (days) and then infiltration of T cells (days to weeks)28, 29. In particular, neuroinflammation manifests as activation of glial cells, such as Schwann cells in the nerve, satellite glial cells in the ganglia and microglia, and astrocytes and oligodendrocytes in the spinal cord and brain 30. Activation of glial cells leads to the production of glial mediators that can modulate pain sensitivity 31. Of the cells that are resident in the CNS, microglia are probably the first cells to respond (within days) to peripheral nerve damage followed by astrocytes (days to weeks) 32–34. These temporal details are relevant to drug targeting for controlling the initiation and the maintenance of chronic pain, because depending on what stage of chronic pain a drug can target, the cell types and hence mediators will differ. In addition, an increase in the permeability of the BBB and blood-spinal cord barrier (BSCB) — which leads to increased leukocyte invasion to the CNS — is an important feature of the CNS inflammation.
Neuroinflammation is a local inflammation which means that it is more effective at eliciting and sustaining pain than systemic inflammation, yet it is difficult to detect in clinic. For example, fibromyalgia, a chronic muscle pain condition, was previously regarded as an atypical pain, because no obvious pathologies and inflammation could be detected in affected patients. However, a recent study identified neuropathy of small nerve fibres in patients with fibromyalgia 35, which could be a result and also a cause of chronic neuroinflammation. Neuroinflammation appears to be permanent in patients with chronic pain, for example neuroinflammation (measured by glial activation and cytokine expression) was positively associated with neuropathic pain in postmortem spinal cord samples from HIV-infected patients 36. Neuroinflammation in the CNS could also be neurogenic inflammation 37, since it can be triggered by neuronal activities from primary sensory neurons 38, 39 or local neurons in the spinal cord.
There are several excellent reviews on peripheral neuroinflammation and chronic pain 30,40. We focus this review on how central neuroinflammation drives chronic pain (Fig. 2), in part because central inflammation produces more targets to sustain chronic pain. We will outline how the production of inflammatory and glial mediators in the spinal cord modulates synaptic transmission to provide a link between neuroinflammation and chronic pain and highlight emerging targets including chemokines that mediate interactions between neurons and glial cells, lipid mediators that act on neurons and glia to resolve inflammation as well as other emerging targets that modulate neuroinflammation such as proteases and Wnt signalling molecules. In addition, we highlight the advantages and disadvantages of each approach. We focus on these targets because firstly these are relatively new targets in the pain research field and secondly they modulate chronic pain via a unique mechanism, i.e. neuron–glial interactions in the CNS.
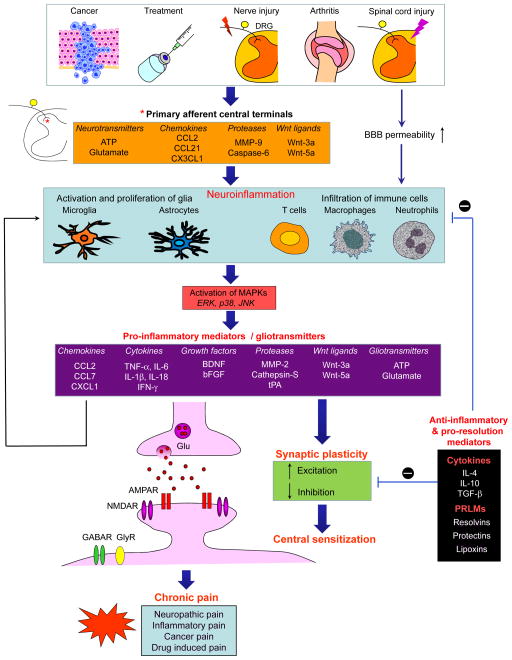
Figure 2. Neuroinflammation in the spinal cord drives chronic pain via neuron–glial interactions and central sensitization.
Chronic pain, such as nerve injury and spinal cord injury-induced neuropathic pain, arthritis-induced inflammatory pain, cancer pain, and drug treatment-induced pain is a result of neuroinflammation in the spinal cord. This neuroinflammation is triggered by activity-dependent release of glial activators (that is, neurotransmitters, chemokines and proteases, and wnt ligands) from the central terminals of primary afferent neurons and/or by disruption of BBB. Neuroinflammation is characterized by the activation of microglia and astrocytes, the infiltration of immune cells to the PNS (e.g., DRG) and CNS (e.g., spinal cord), and the production of inflammatory and glial mediators such as proinflammatory cytokines and chemokines, growth factors and gliotransmitters (glutamate and ATP). These glial mediators can powerfully modulate excitatory and inhibitory synaptic transmission, leading to central sensitization and enhanced chronic pain states. Glial mediators can further act on glial and immune cells to facilitate neuroinflammation via autocrine and paracrine routes. Furthermore, neuroinflammation also generates anti-inflammatory cytokines and pro-resolution lipid mediators (PRLMs) to normalize neuroinflammation, synaptic plasticity and abnormal chronic pain.
Infiltration of immune cells in the CNS
Infiltration of leukocytes such as macrophages and T-cells into the spinal cord is very obvious after direct injury to the spinal cord (such as spinal cord contusion)27. Immune cell infiltration into the CNS after peripheral nerve injury or tissue injury is also evident. Activation of the chemokine receptor CCR2 contributes to the infiltration of bone marrow-derived macrophages into the spinal cord after peripheral nerve injury 41. T-cell infiltration in the spinal cord was also implicated in the development of neuropathic pain after nerve injury, in an age-dependent manner 28. Opening of BSCB has been reported after nerve injury and C-fiber activation in rodents, leading to immune cell infiltration to the spinal cord 42, 43.
Activation of microglia and astrocytes in chronic pain
Due to the presence of larger numbers of residential glial cells compared to leukocytes, residential glial cells are thought to have a more important role in the development of chronic pain. So called “glial activation” is emerging as a key mechanism underlying the genesis of chronic pain 31. Notably, glia have more than one activation states and not so quite even in the physiological “resting” state 44. Thus, it is important to define the specific characteristics of activated glia which can be associated with different activation states of glia (Box-2). Each activation state might have distinct set of characteristics and these characteristics may have different roles in pain sensitization, and therefore, some characteristics/activation states would be more appropriate to target therapeutically than others 31, 45.
Box-2. Distinct characteristics of activated glia.
There are not only non-activated glia (note that even under “resting state” microglia are still doing surveillance job) and activated glia but also more than one type of activated glia with different characteristics which might be associated with different activation states of glia.
Gliosis, glial hypertrophy, or glial reaction is the most investigated characteristic of activated glia and manifests as changes in glial morphology and upregulations of glial markers such as CD11b and Ionized calcium binding adaptor molecule 1 (Iba1) on microglia, and glial fibrillary acidic protein (GFAP) and S100 on astrocytes 168–170. It appears that astrocytic reaction/ hypertrophy in the spinal cord is more general and persistent than microglial reaction/hypertrophy and better correlated with chronic pain states following various painful injuries 31, 33, 171. Notably, microglial reaction in the spinal cord that is induced by nerve injury is age-dependent; neuropathic pain and microglial reaction do not occur in young rats (< 3 weeks old) 172.
Activation of MAPKs is another prominent characteristic of glial activation. ERK1/2, p38, JNK, ERK5 are involved in intracellular signalling in activated glia and in the pathogenesis of chronic pain 173. Strikingly, different MAPKs have distinct activation patterns in spinal glial cells after nerve injury, such as p38 and ERK5 activation in microglia, JNK activation in astrocytes, and the sequential activation of ERK 1/2 in microglia and then in astrocytes 174–176.
Nerve injury also causes upregulation of many receptors and channels in glia in rodent models. Peripheral nerve injury induces the expression of the ATP receptors P2X4, P2X7, P2Y6 and P2Y12 in spinal microglia, which is implicated in the development of neuropathic pain 87, 177–180. Connexin-43 (Cx43) hemichannels, which control ATP release 181, are up-regulated in spinal cord astrocytes after spinal cord injury and are also involved in the development of neuropathic pain 182. Furthermore, the chemokine receptor CX3CR1 is specifically expressed in microglia is upregulated in the spinal cord after nerve injury 183. Neuropathic pain is also associated with downregulation of the glutamate transporters GLT-1 and GLAST in spinal cord astrocytes, which causes a deficit in glutamate clearance from synaptic clefts and extracellular space, leading to enhanced glutamatergic transmission 31, 184.
The most critical characteristic of glial activation for pain regulation is generation of glial mediators, which are act as powerful neuromodulators to regulate excitatory and inhibitory synaptic transmission in the spinal cord 31, 153, 185.
Tumor-necrosis factor-alpha (TNF-α) is one of the most studied and potent inflammatory cytokines and has been shown to be expressed by microglia, astrocytes and primary sensory DRG neurons 46, 47. However, single-cell PCR analysis reveals that although the majority of microglia (90%) and some astrocytes (40%) express TNF-α neurons of spinal cord do not express it 48, suggesting that microglia are the major source of (TNF-α) in the spinal cord. Interleukin-1 beta (IL-1β), another crucial inflammatory cytokine, is expressed by both microglia and astrocytes in the spinal cord 49, 50, whereas IL-18 — which is closely related to IL-1β—is induced in microglia after nerve injury and chronic opioid exposure 51, 52. Chemokines such as CCL2, CXCL1 and CCL7 are produced in spinal cord astrocytes to facilitate neuropathic pain 53–55. BDNF was originally found in DRG neurons and their spinal cord central terminals 56, but is also induced in spinal microglia after nerve injury and following chronic morphine treatment and contributes to neuropathic pain and morphine tolerance 57, 58. Basic fibroblast growth factor (bFGF) is induced in spinal cord astrocytes to sustain neuropathic pain 59. Furthermore, glial cells produce anti-inflammatory cytokines such as IL-4, IL-10, TGF-β and IFN-α to antagonize pain 26, 31, 60, 61, but the cellular localization of these anti-inflammatory cytokines is not well characterized.
Nerve injury also causes proliferation of microglia 62 and astrocytes 63 in the spinal cord, which could contribute to increased production of glial mediators and expression of hyperalgesia and allodynia. Glial mediators are neuromodulators, and as such can powerfully modulate synaptic transmission in the spinal cord at nanomolar concentrations. Of interest, TNF-α;, IL-1β, IL-6 and BDNF modulate both excitatory and inhibitory synaptic transmission 24, 57, 64, 65. In the dorsal horn TNF-α increases glutamate release from terminals of C fibres that express TRPV1, leading to enhanced excitatory synaptic transmission in excitatory interneurons in lamina IIo, which in turn synapse to lamina-I projection neurons to form a pain circuit 66.
BDNF secreted from microglia induces a trans-synaptic reduction in the expression of the potassium–chloride exporter KCC2, leading to a depolarizing shift in the anion reversal potential in projection neurons in lamina I. As a result, GABA produces less inhibition and sometimes even evokes excitation in spinal cord projection neurons 57, 58. Dis-inhibition of GABAergic and glycinergic synaptic transmission in the spinal cord pain circuitry has an important role in generating chronic pain 57, 67. Interestingly, a feed-forward glycinergic circuit in the laminae II-III of the spinal cord was implicated as a new gate control mechanism for pain, and loss of this gate control after nerve injury opens the gate to enable normally innocuous mechanical stimulation to elicit mechanical allodynia, a cardinal feature of neuropathic pain 68. Although many of the above mentioned molecules such as TNF-α, IL-1β, IL-6 and KCC2 are potential targets for pain therapeutics, we will focus this review on the following emerging targets (and see Table-1) that have both pro- and anti-inflammatory actions. We will also discuss new therapeutic strategies for chronic pain management in which the targets with anti-inflammatory actions should be activated / potentiated and the ones with proinflammatory actions should be reduced / blocked.
Table 1.
Emerging pro-inflammatory and anti-inflammatory mediators in rodent models of pain
| Mediator | Pain conditions | Sources | Targets | Roles in pain regulation | Refs |
|---|---|---|---|---|---|
| Pro-inflammatory chemokines, proteases, and Wnt pathway signaling molecule | |||||
| CX3CL1 | Nerve injury, cancer, arthritis | Neurons | CX3CR1 in microglia | Induces activation of microglia and promotes neuropathic pain, cancer pain and inflammatory pain | [72–75] |
| CXCL1 | Nerve injury | Astrocytes | CXCR2 in neurons | Maintains central sensitization and neuropathic pain | [55] |
| CCL2 | Nerve injury | Neurons Astrocytes |
CCR2 in microglia CCR2 in neurons |
Induces activation of microglia and neuropathic pain Maintains central sensitization and neuropathic pain |
[33,78] [54,80] |
| CCL21 | Nerve injury, spinal cord injury | Neurons | CXCR3 in microglia | Induces activation of microglia and neuropathic pain | [85,86] |
| CCL7 | Nerve injury | Astrocytes | CCR2 in microglia | Maintains activation of microglia and neuropathic pain | [53] |
| MMP9 | Nerve injury | DRG neurons | IL-1β signaling | Induces activation of microglia and neuropathic pain | [138] |
| MMP2 | Nerve injury | Astrocytes satellite cells | IL-1β signaling | Maintains astrocyte and ERK activation and neuropathic pain | [138] |
| Cathepsin S | Nerve injury | Microglia | Neuronal CX3CL1 | Promotes activation of microglia and neuropathic pain | [73, 147] |
| Caspase 6 | Tissue injury | DRG neurons | TNF-α in microglia | Induces microglia activation and inflammatory pain | [48] |
| Wnt3a | Nerve injury cancer, EAE | Neurons Astrocytes |
Frizzled/β-catenin | Enhances glial activation, cancer pain and neuropathic pain Induces neural and synaptic plasticity |
[148, 150] |
| Anti-inflammatory pro-resolution lipid mediators (PRLMs) | |||||
| PD1 | Nerve injury Arthritis |
Immune cells and glial cells? | GPCRS in neurons, immune cells, and glia | Inhibits TRPV1 and TNF-α signalling Prevents glial activation and neuropathic pain Reduces established inflammatory pain and neuropathic pain |
[66,98] |
| RvE1 | Nerve injury Arthritis |
Immune cells and glial cells? | ChemR23 in neurons, immune cells, and glia | Inhibit TRPV1, ERK, and TNF-α signaling Reduces inflammation and microglia activation, reduces inflammatory pain and neuropathic pain |
[99, 121] |
| RvD1 | Arthritis | Immune cells and glial cells? | GRP32 and ALXR in neurons and glia | Inhibits TRPA1, TRPV3 and TRPV4 | [99, 123, 124, 130] |
| RvD2 | Arthritis | Immune cells and glial cells? | GPCRs in neurons and immune cells and glia | InhibitsTRPA1 and TRPV1 and reduces synaptic plasticity; Inhibits inflammatory pain | [123] |
| Lipoxins | Arthritis | Immune cells and glial cells? | ALXR in astrocytes | Inhibit JNK activation in astrocytes; Reduce inflammatory pain | [3] |
Chemokines: mediators of neuron–glial interactions
It is generally believed that neuroinflammation modulates chronic pain by promoting signaling interactions between neurons and glial cells 31, 45, 69, 70. In particular, chemokines are well positioned to mediate these interactions, because the chemokines and their receptors are differentially expressed in neurons and glial cells. Chemokines-mediated neuron-glial interactions have two fold. First, neurons express chemokines and glial cells express the respective receptors of these chemokines. Second, glial cells express chemokines and neurons express their respective receptors 23. The role of chemokines in the regulation of peripheral leukocyte migration and activation, cell adhesion and T cell activation, as well as in the induction of peripheral sensitization is well established 40, 71. Here we focus on the role of chemokines within the CNS in the processing of chronic pain and provide an update on recent progress in this research area. Specifically, we discuss several pairs of chemokines and chemokine receptors in modulating signalling from neurons and glia and from glia to neurons in the spinal cord and how this signalling is involved in the persistence of chronic pain.
CX3CL1 and CX3CR1 mediate neuron–microglia interactions
CX3CL1 (also named fractalkine) is the only member of CX3C subfamily and has two distinct molecular forms: a membrane-bound form which promotes cell adhesion and a soluble form with chemotactic properties. CX3CL1 is constitutively expressed in DRG and spinal cord neurons 72, 73. Following nerve injury in a rodent model or treatment of DRG neurons with the protease cathepsin S, CX3CL1 is cleaved and secreted from DRG neurons (including their central terminals) and spinal neurons.73. It then binds to CX3CR1, the only receptor of CX3CL1, and importantly, CX3CR1 is specifically expressed in microglia and upregulated in chronic pain conditions 72, 74. Neuropathic pain is reduced by spinal administration of a CX3CR1 neutralizing antibody in rats and is abrogated in Cx3cr1 knockout mice 73–75. Mechanistically, CX3CL1 was shown to activate p38 MAPK in spinal microglia 74.
Thus, CX3CL1 and CX3CR1 are involved in neuron–microglia interactions in the spinal cord to promote chronic pain. In addition to the neutralizing antibody mentioned above, a hCX3CL1 analogue (named F1) was identified as the first CX3CR1 antagonist that could potently inhibit macrophage accumulation in a murine model of periodontitis 76. The analgesic efficacy of this antagonist needs to be tested in animal models.
CCL2 and CCR2 mediate neuron–microglia and astrocyte–neuron interactions
CCL2 (also known as monocytes chemoattractant protein 1 (MCP-1)) is one of 28 members of CC subfamily of chemokines. CCL2 recognizes several receptors including CCR1, CCR2 and CCR4, but CCR2 is the preferred receptor with higher affinity for CCL2 23, 40. CCL2 neutralization, CCR2 antagonists or deletion of Ccr2 each reduces neuropathic pain in rodents 41, 54, 77, 78. Early studies suggested that CCL2 and CCR2 are involved in signalling interactions between primary sensory neurons and microglia in the spinal cord in neuropathic pain, based on the following evidence: First, nerve injury causes upregulation of CCL2 in DRG nociceptor neurons29. Second, high intensity stimulation of the dorsal root (which contains efferent fibers of DRG neurons) induces CCL2 release from spinal cord slices taken from animal models of neuropathic pain 69. Third, Ccr2 knockout mice have reduced levels of neuropathic pain and spinal microgliosis 41, 45, 78. However, morphological evidence for CCR2 expression in spinal microglia is insufficient 77, although CCR2 was shown to be upregulated in microglia in the rostral ventromedial medulla (an area of the brainstem involved in pain modulation) following spinal nerve ligation in rats 79.
Recent studies (since 2009) suggest that CCL2 and CCR2 also mediate astrocyte–neuron signalling in the spinal cord during neuropathic pain. First, nerve injury in mice induces expression of CCL2 astrocytes in the spinal cord and trigeminal nucleus and also upregulates CCR2 in spinal cord neurons 54, 80. Second, incubation of spinal cord slices with CCL2 very rapidly (within minutes) increases excitatory synaptic transmission, NMDA currents and ERK activation in dorsal horn neurons 54. Third, transgenic mice over-expressing CCL2 in astrocytes are hypersensitive to pain 81. Thus, CCL2 also severs as a neuromodulator in the spinal cord. It is reasonable to postulate that CCL2- and CCR2-mediated neuron–microglia interactions (which activate microglia in the early phase of nerve injury) are involved in the induction of neuropathic pain and CCL2- and CCR2-mediated astrocyte–neuron signalling (which is delayed and sustained) is involved in the maintenance of neuropathic pain.
CXCL1 and CXCR2 mediate astrocyte-neuron interaction
CXCL1 (also known as a keratinocyte-derived chemokine) belongs to the CXC family of chemokines. CXCL1 in rodents has similar biological roles as interleukin-8 in humans. Spinal nerve ligation in mice induces a persistent (> 3 weeks) increase in CXCL1 expression in spinal cord astrocytes; this increase can also be recapitulated by application of TNF-α in astrocyte cultures 55. CXCL1 is also selectively expressed in hypertrophic astrocytes from active multiple sclerosis lesions taken from patients 82, indicating a possible involvement of astrocytic CXCL1 in the pathogenesis of multiple sclerosis. CXCR2, the major receptor of CXCL1 40, is upregulated in dorsal horn neurons after nerve injury. Behavioral studies showed that intrathecal injection of a CXCL1 neutralizing antibody or the CXCR2 antagonist SB225002 attenuated mechanical allodynia and heat hyperalgesia that were induced by spinal nerve ligation in mice. Moreover, intraspinal delivery of CXCL1 shRNA via lentivirus produced similar effects 55.
These data suggest that CXCL1 and CXCR2 signalling, which mediates astrocyte–neuron interactions, has an important role in the maintenance of neuropathic pain. In addition, CXCL1 may also be involved in other types of cell–cell signalling, since it is transiently induced in DRG neurons after nerve injury (which can be involved in neuron-microglial signaling as CCL2) 83. After spinal cord injury, spinal cord astrocytes also express CXCL1, which promotes the entry of leukocytes to the site of injury 84.
Other chemokines involved in pain modulation
Expression of CCL21 in neurons after spinal cord or nerve injury in rodents was implicated in microglial activation in the thalamus and spinal cord 85, 86. Injection of recombinant CCL21 into the ventral posterolateral nucleus of the thalamus transiently activated microglia and induced pain-related behaviors in rats, and the effects could be blocked by the non-selective microglial inhibitor minoncycline 85. Another study showed that the development of allodynia was blocked in mice deficient in CCL21 or by intrathecal administration of a CCL21-blocking antibody to wildtype mice. Furthermore, nerve injury-induced upregulation of P2X4 receptors in microglia, which is essential for the development of neuropathic pain in rats 87, was also abolished in CCL21 deficient mice 86.
In mice, nerve injury also induces a long-lasting upregulation of CCL7 in spinal cord astrocytes to sustain neuropathic pain, and intrathecal administration of a CCL7 neutralizing antibody suppressed nerve injury-induced spinal microglia activation and neuropathic pain-like behaviour53. CXCL12 (also named stromal derived factor-1 (SDF1)), and its receptor CXCR4 are involved in neuron–glial signalling in DRGs and HIV-associated peripheral neuropathy: in rats the pain hypersensitivity produced by an antiviral drug was inhibited by treatment with the CXCR4 antagonist AMD3100 (also named plerixafor) 88. However, CXCL12/CXCR4-mediated neuron–glial interactions mediated by CXCL12 and CXCR4 in the spinal cord remain to be investigated. In addition, partial sciatic nerve injury induces a drastic up-regulation of CCL3 (also called macrophage inflammatory protein-1alpha, MIP-1α) in macrophages and Schwann cells of the injured sciatic nerve, and nerve injury-induced thermal hyperalgesia in mice was prevented by perineural treatment with siRNA against the CCL3 receptor CCR5 89. Nerve injury causes persistent spinal upregulations of CCL3 and CCR5, and furthermore, spinal and oral administration of the CCR5 antagonist maraviroc alleviated neuropathic pain in rodents 90.
Benefits and limitations of targeting chemokine signaling
Although two chemokine receptor inhibitors are approved for clinical use, the CCR5 antagonist maraviroc for the treatment of HIV-1 infection and the anti-cancer CXCR4 antagonist plerixafor 91, many chemokine receptor inhibitors have failed to show efficacy in clinical trials. Given the effectiveness of intrathecal and oral maraviroc in a rodent model of neuropathic pain 90, it will be interesting to test this drug in human pain conditions in the future. CCR2 is probably the most studied chemokine receptor in pain research 40, 77, 92. AZD2423, which is a highly selective antagonist for CCR2, induced robust analgesia in two rodent models of neuropathic pain and a model of joint destruction pain (http://www.ncats.nih.gov/files/AZD2423.pdf). However, AZD2423 did not show significant effects in a trial of posttraumatic neuralgia, despite a there being trend towards a reduction in some sensory components of pain such as paroxysmal pain and paresthesia and dysesthesia 93. This low efficacy may arise from species selectivity (rodents versus humans), pharmacokinetic properties and/or drug metabolism, and redundancy in the chemokine network, as one chemokine often has more than one receptor. Given the important role of central chemokine signalling in chronic pain 23, the low efficacy of the CCR2 antagonist AZD2423 in a pain trial 93 may also be a result of poor CNS actions. To potentially increase the efficacy of chemokine antagonism it might be beneficial to simultaneously target several chemokine receptors. Indeed the dual CCR2/CCR5 peptide antagonist RAP-103 (which was orally active) effectively reduced neuropathic pain and inhibit CCR2- and CCR5-mediated monocyte chemotaxis and inflammation in rodents 94.
Several CXCR2 antagonists have been tested in inflammation models in humans 95–97. Administration of AZD-8309, a pyrimidine-based CXCR2 antagonist, reduced neutrophil recruitment and leukotriene B4 levels by 50% in a human airway inflammation model induced by lipopolysaccharide, without causing systemic inflammation 95. SB-656933, a selective and reversible CXCR2 antagonist, dose-dependently inhibited neutrophil activation and reduced ozone-induced airway inflammation following oral administration96. SCH527123, another selective anatagonist of CXCR2, also attenuated of ozone-induced airway neutrophil activation in healthy subjects 97. Further preclinical studies are warranted to test these novel CXCR2 antagonists in animal models of inflammatory and neuropathic pain. Given that CXCL1 and CXCR2 signalling has a critical role in the maintenance of chronic pain 55, CXCR2 inhibitors or antagonists that are CNS permeable could be promising for pain management.
Emerging targets: pro-resolution lipid mediators
Targeting lipid mediators that promote the resolution of inflammation could be another way of combating neuroinflammation. Notably, such lipid mediators such as resolvins and protectins not only act on immune cells and glial cells but also act on neurons and have neuroprotective actions 98–100 (Table-1). Although the omega-3 unsaturated fatty acids docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), which are metabolized to produce resolvins and protectins [figure 3], have several benefits including pain relief, when used experimentally, the analgesic efficacy and potency of resolvins and protectins, are much higher 101. Resolvins, such as resolvin D1 (RvD1), resolvin D2 (RvD2), and resolvin E1 (RvE1), and protectin D1 represent a class of pro-resolution lipid mediators (PRLMs) 102 (Fig. 3). Resolvins were originally isolated from inflammatory exudates that were involved in inflammation resolution in rodents and humans 102, 103 and have potent anti-inflammatory and pro-resolution actions in several rodent models of inflammation, such as colitis 104, pneumonia and acute lung injury 105, and kidney ischemia 106. Protectin D1 is also termed neuroprotectin D1 107–109, because it protects against experimental brain damage, oxidative-stress in retinal pigment epithelial cells, and accumulation of beta amyloid peptides in cultured human brain cells 108, 110, 111. The complete stereochemistry of protecitin D1 and 10,17-docosatriene structure were confirmed by total organic synthesis 112. Notably the enzymes responsible for the synthesis of resolvins and protectins such as lipoxygenase-5 and lipoxygenase-12 (LOX-5/12) and cyclooxygenase-2 (COX-2) can be induced at the acute or resolution phases of inflammation113. Thus, whether consumed (digested) fish oil (which comprises of DHA and EPA) can be converted to resolvins and protectins rely on the activities of these enzymes 101.
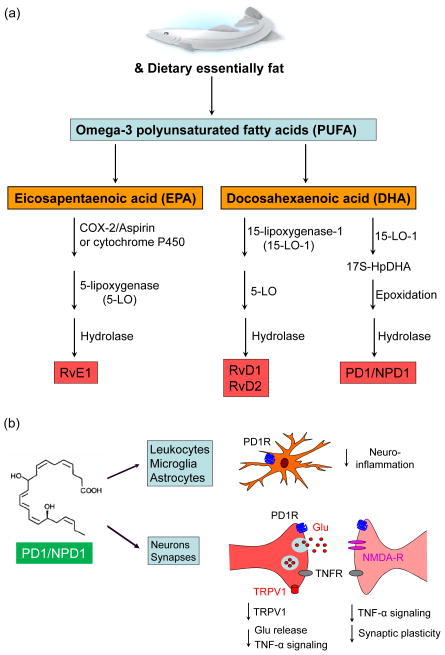
Figure 3. Biosynthetic pathways of PRLMs resolvins and protectin and mechanisms of actions of protectin D1.
(a) Omega-3 polyunsaturated fatty acids (DHA and EPA) are derived from dietary essentially fat which is enriched in fish oil. Resolvins (RvD1, RvD2) and protectin D1 (PD1, also known as neuroprotectin D1) are derived from DHA, whereas RvE1 is derived from EPA. Distinct synthetic enzymes, including COX-2, cytochrome P450, and 5- and 15-lipoxygenase (5-LOX and 12-LOX) are responsible for the biosynthesis of the PRLMs. (b) Structure and mechanisms of actions of PD1. Note that PD1 acts on immune and glial cells to control neuroinflammation as well as on neurons and synapses to normalize synaptic and neuronal plasticity.
The biological actions of these lipid mediators are mediated by GPCRs. For example, ChemR23 was identified as RvE1 receptor 114, whereas GPR32 and ALX were identified as receptors for RvD1115. However, specific GPCRs for RvD2 and protectin D1 are still under investigation. In next series of paragraphs, we will discuss the actions of revolvins and protectin D1 in rodents and their translational potentials.
Inhibition of inflammatory pain
Peripheral (intraplantar) injection of RvD1 and RvE1 effectively prevented inflammatory pain and also reduced inflammation-induce paw edema and expression of proinflammatory cytokines and chemokines (TNF-α, IL-1β, IL-6, CCL2) in mice 99. Moreover, spinal administration of RvE1 very rapidly (<15 min) inhibited persistent inflammatory pain, at effective doses that were around 100 times lower than that of morphine 99. RvE1 and protectin D1 are powerful inhibitors of TNF-α signalling: hyperalgesia evoked by spinal TNF-α can be blocked by intrathecal administration of RvE1 or protectin D1 66, 99, further suggesting the importance of PRLMs in modulating CNS functions.
Protection of neuropathic pain and neuropathy
Neuropathic pain is often resistant to the treatments that are effective for inflammatory pain, such as opioids and NSAIDS 116–118. Strikingly, peri-surgical treatment with PD1 completely prevented mechanical allodynia (Fig. 4a) in a mouse model of neuropathic pain 98, whereas RvE1 and glia-derived neurotrophic factor (GDNF) only transiently prevented this type of pain 98, 119–121. Moreover, post-treatment of protectin D1 via spinal intrathecal route, 2 weeks after nerve injury, also reversed nerve injury-induced mechanical allodynia for several hours (Fig 4b,c) and did not induce antinoiciceptive tolerance 98. Notably, much higher doses of gabapentin – which is widely used to treat neuropathic pain - were needed to suppress mechanical allodynia (Fig 4c). Interestingly, protectin D1 pre-treatment suppressed the expression of activating transcription factor-3 (ATF-3) associated with axonal injury 122 (that is, neuropathy) in DRG neurons 98, showing that protectin D1 further protects primary sensory neurons against nerve injury-induced neuropathy.
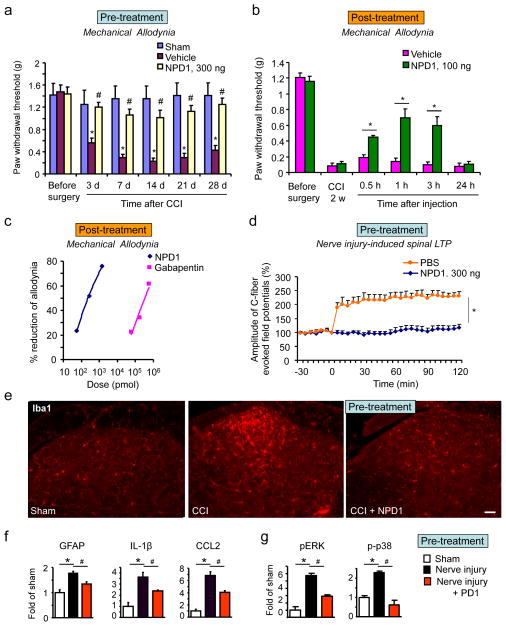
Figure 4. Protectin D1 protects neuropathic pain and prevents nerve injury-induced spinal LTP and neuroinflammation in mice.
(a) Local peri-surgical pretreatment with NPD1 (300 ng per mouse, via peri-sciatic administration) prevents mechanical allodynia induced by chronic constriction injury (CCI). *P<0.05, compared to sham control, #P<0.05, compared to corresponding vehicle (that is, phosphate buffered saline solution, PBS) control.
(b) Intrathecal injection of NPD1 (100 ng per mouse) 2 weeks after nerve injury reduces CCI-induced mechanical allodynia. *P<0.05, compared to corresponding vehicle (that is, PBS) control.
(c) Dose-dependent inhibition of CCI-induced mechanical allodynia by NPD1 (20–500 ng per mouse administered intrthecially, which approximately equals 0.06–1.4 nmol) and gabapentin (i.t., 10–100 μg ≈ 58.4–584.1 nmol). Mechanical allodynia was tested 3 h after the drug injection. Note that the effective doses of gabapentin are much higher than that of NPD1.
(d) NPD1 (300 ng) reduces LTP in the spinal cord that is induced by nerve injury; *P<0.05 versus PBS.
(e) Iba1 (microglial marker) immunostaining in the dorsal horns of sham control and CCI mice (1 week) with pretreatment of PBS or NPD1. Nerve injury causes upregulation of Iba1 in the dorsal horn of mice; this can be reduced by pretreatment with NPD1 but not PBS. Scale, 50 μm.
(f, g) Peri-surgical treatment with NPD1 prevents nerve injury-induced spinal cord neuroinflammation (as measured by the expression of GFAP, IL-1β, and CCL2 mRNAs and phosphorylation of p38/ERK (p-p38/pERK, g) in the dorsal horn. *P<0.05, #P<0.05. Data are mean ± SEM. Modified from the paper of Xu et al. (2013, Annals of Neurology) with permission from the press.
Regulation of synaptic plasticity and neuroinflammation
Given the importance of synaptic plasticity in the induction and maintenance of chronic pain 17, compounds that block synaptic plasticity in the spinal cord have the potential to be powerful analgesics. One of the most effective mechanisms for the PRLMs to resolve pain is through modulation of spinal cord synaptic plasticity 98. RvE1, RvD2, and protectin D1 do not alter excitatory synaptic transmission in ex-vivo spinal neurons of spinal cord slices under normal (that is, non-painful) conditions 66, 99, 123, but reversed the increases in excitatory synaptic transmission that were induced by inflammation, nerve injury, or TNF-α treatment 66, 98, 99, 123. Future studies to investigate whether these PRLMs also modulate inhibitory synaptic transmission are warranted. It is noteworthy that spinal administration of PD1 and RvD2 reversed long-term potentiation in the spinal cord — a form of synaptic plasticity that has been linked to the development of pain — in vivo 66, 123. Furthermore, peri-surgical treatment with protectin D1 at the injury site controlled nerve injury-induced neuroinflammation in the CNS (Fig. 4e–g) and PNS 98. Other PRLMs such as resolvins also inhibit neuroinglammation in rodent models: RvE1 inhibited neuropathic pain and microglial activation 121 and RvD1 inhibited arthritic pain and the expression of NF-κB and COX-2 in DRG and spinal cord of rats 124.
Modulation of TRP channels
Transient receptor potential ion channels such as TRPV1, TRPA1 TRPV4 are expressed by nociceptor neurons and are involved in peripheral sensitization and the pathogenesis of chronic pain 125–127. Lipid mediators can act as endogenous ligands to activate or inhibit TRP channels 128, 129. For example, in native DRG neurons protectin D1 potently inhibits TPRV1 (IC50 = 0.4 nM), through actions that are mediated by Gi/o-coupled GPCRs 66. Of interest, resolvins differently modulate TRP channels: RvD1 only inhibits TRPA1, and RvE1 only inhibits TRPV1, but RvD2 inhibits both TRPA1 and TRPV1 in DRG neurons 123. RvD1 also inhibits TRPV3 and TRPV4 in heterologous cells 130. Thus, PRLMs are potent endogenous inhibitors of TRP channels. Of interest, the RvE1 receptor ChemR23 is heavily colocalized with TRPV1 in DRG neurons 99. TRP channels serve as key signal transduction integrators for several inflammatory mediators, and hyperactivity of TRPA1 and TRPV1 is a hallmarks of peripheral sensitization 125. So, it is likely that PRLMs resolve peripheral sensitization in part by normalizing the tissue injury-induced hyperactivity of TRP channels, without blocking basic functions of these channels.
Benefits and limitations of PRLMs as drug targets
As described above, PRLMs have several actions that could be beneficial for treating inflammatory and postoperative pain associated with arthritis, lower back injury and surgery, as well as neuropathic pain associated with nerve injury. In addition to resolvins and protectin, the lipoxins, which are PRLMs that are derived from arachidonic acid, reduce inflammatory pain in rats 3. Maresin (macrophage mediator in resolving inflammation), derived from DHA, was also shown to prevent chemotherapy-induced neuropathic pain in mice 131. The most striking benefits of these PRLMs are high potency, a wide safety window and multiple mechanisms of actions. These actions include the control of inflammation in peripheral tissues, control of neuroinflammation in the PNS and CNS, resolution of synaptic plasticity in the CNS, and modulation of TRP channel activities.
Current treatments for inflammatory and neuropathic pain are limited by well-known side effects. Opioids produce respiratory depression and sedation after acute treatment and also cause addiction, tolerance and hyperalgesia after chronic treatment. COX-2 inhibitors are limited by cardiovascular defects after long-term treatment and TNF-α–targeted treatment may cause infection through immune suppression101. Neuropathic pain treatments such as gabapentin and pregabalin (lyrica) are only effective in a portion of patients and cause dizziness, drowsiness, and nausea 132. To overcome the disadvantages of the current pain medicine, the endogenous PRLMs or their analogues could be developed for treating inflammatory pain133. Notably, the incidence of developing chronic neuropathic pain after major surgeries, such as amputation, thoracotomy and breast surgeries, is very high 116, despite aggressive preventive efforts 134. Given the remarkable efficacy of protectin D1 in preventing nerve injury-induced neuropathic pain 98, protectin D1 and their mimetics could be useful for the prevention of surgery-induced neuropathic pain. Since post-treatment of protectin D1 via repeated injections does not cause analgesic tolerance and side effects under such low dose (Fig. 4)98, protectin D1 and its analogs might also be used to treat chronic neuropathic pain after diabetic neuropathy 98 and perhaps viral infection or chemotherapy, but further testing in animal models is needed.
PRLMs also have limitations as new therapeutics. It is well known that endogenous local acting lipid mediators are metabolically unstable in vivo. For example, RvE1 reduces CFA-induced heat hyperalgesia for less than 2 hours. However, a modified form of RvE1 (19-pf-RvE1), which is metabolically stable and resistant to local rapid metabolic inactivation is able to reduce heat hyperalgesia for more than 6 hours 99. Hence, development of more stable forms of PRLMs (through chemical modification to enhance their half-lives in body fluids), or improved delivery methods for unstable PRLMs (e.g., using nanoparticles for sustained release of PRLMs) should prolong and enhance the analgesic effects of resolvins. The receptors for some PRLMs, such as ChemR23 for RvE1 and ALX for RvD1 and LXA4 are widely expressed in neurons, glia, and immune cells 3, 99–101, which may explain the broad beneficial actions of PRLMs. However, the receptors for the other PRLMs (e.g., PD1 and RvD2) and the detailed signalling mechanisms of how PRLMs resolve pain remain unclear. The identification of novel receptors (which are presumably GPCRs) and a better understanding of their signalling mechanisms will be crucial for the future development of small-molecule agonists for activating PRLMs receptors and signalling pathways.
An alternative strategy is to boost the production of endogenous PRLMs from a healthy diet that is high in Omega-3 fatty acids and low Omega-6 fatty acids. Effective conversion of dietary DHA and EPA to PRLMs may be responsible for dietary control of chronic headache 135. Notably, aspirin initiates the biosynthetic pathway of RvE1 via acetylating COX-2, which may explain the beneficial effects of low-dose aspirin in inflammation-associated chronic diseases 136, 137. It will be of great interest to test whether diet control together with low-dose aspirin is a safe and low-cost treatment for certain types of chronic pain.
Other emerging targets that modulate neuroinflammation
Proteases
Increasing evidence suggests that proteases such as matrix metalloproteases (MMPs) 138, cathepsin S 73, 139, and caspases 48 are involved in pain sensitization by regulating neuroinflammation in the CNS. The MMP family has over 26 family members and the gelatinases MMP-9 and MMP-2 are among the most studied family members. Nerve injury induces a transient upregulation of MMP-9 in DRG neurons in a mouse model, which is required for the induction — but not the maintenance of— neuropathic pain, by inducing spinal cord microglial activation138. The maintenance of murine neuropathic pain is dependent upon the delayed but persistent upregulation of MMP-2 in DRG satellite cells and spinal cord astrocytes 138. MMP-9 is both sufficient and required for eliciting persistent mechanical allodynia via IL-1β signaling in mice 138. Moreover, there is evidence that MMP levels are altered in human pain states, since there is an upregulation of MMP-2 levels in the cerebrospinal fluid of elderly patients with chronic osteoarthritis pain 140.
Thus, inhibition of MMP-9 inhibition could be used to prevent neuropathic pain after major surgeries (for example amputationand thoracotomy), spinal cord injury and brain trauma. MMP-2 inhibition could have the potential to treat established neuropathic pain after diabetes, viral infection, and chemotherapy. A dual inhibitor of MMP-9 and MMP-2 may help to treat neuropathic pain at different phases. Specific targeting of MMP-9 and/or MMP-2 can be achieved with small molecule inhibitors, monoclonal antibodies and administration of endogenous inhibitors such as TIMP-1 and TIMP-2 (tissue inhibitor of MMPs)138. Indeed, small molecule inhibitors of MMP-9 (termed MMP-9 inhibitor I) and MMP-2 (termed MMP-2 inhibitor III) as well as TIMP-1 and TIMP-2 are effective in reducing murine neuropathic pain 138. The peripheral inflammation-induced thermal and tactile hypersensitivity was also attenuated by intrathecal pretreatment with either an MMP-3 inhibitor N-Isobutyl-N-(4-methoxyphenylsulfonyl)glycyl hydroxamic acid (NNGH), or a broad spectrum MMP inhibitor (GM6001) 141. However, MMPs also have normal physiological functions, and a broad inhibition of MMPs or long-term treatment of MMP-2 and/or 9 inhibitor may cause undesirable side effects. For example, treatment with MMP inhibitors in rodents at 7 days after stroke was shown to suppress neurovascular remodeling and increase ischemic brain injury at 14 days 142. Previous clinical trials with MMP inhibitors for cancer were disappointing, because of a lack of efficacy 143 and toxicity 144, but new inhibitors are emerging 145. Two new selective and orally active MMP inhibitors, 1-{[4-(4-chlorophenoxy)-3,5-difluorophenyl]sulfonyl}-N-hydroxy-4-(morpholin-4-ylcarbonyl)piperazine-2-carboxamide (XL081) and bis-4-[4-(chloro-phenoxy)-3,5-difluoro-benzenesulfonyl]-3-hydroxycarbamoyl-piperazine-1-carboxylic acid 2-methoxy-ethyl ester, magnesium salt (XL784, with IC50 values of 1–2 nM for MMP-2 and 20 nM for MMP-9) were shown to delay the progression of hypertension and diabetic nephropathy following chronic administration in rats 146.
The lysosomal cysteine protease cathepsin S has an important role in regulating neuron–microglial interactions in the spinal cord in neuropathic pain. After nerve injury cathepsin S is upregulated in spinal microglia and contributes to the maintenance of neuropathic pain via cleavage of the transmembrane chemokine from the surface of DRG and spinal cord neurons. Activity-dependent secretion of soluble CX3CL1 then activates microglia activation in the spinal cord 73, 147. Intrathecal injection of cathepsin S inhibitor morpholinurea-leucine-homophenylalanine-vinyl phenyl sulfone reduced neuropathic pain in a mouse model 73. A recent study shows that caspase-6 also regulates neuron–microglial signaling and activity-dependent central sensitization in the spinal cord 48. Following tissue injury and nociceptive activity, release of caspase 6 from the central axonal terminals in superficial dorsal horn causes TNF-α secretion from microglia to drive inflammatory pain 48. Intrathecal injection of caspase 6 inhibitor Z-V-E(OMe)-I-D(OMe)-FMK reduced murine inflammatory pain 48. Thus, targeting cathepsin S and caspase 6 via identifying small-molecule inhibitors in the CNS may open a new avenue for developing pain therapeutics.
Wnt signalling
New evidence suggests that the Wnt signalling pathway regulates neuroinflammation to promote chronic pain 148. Wnts are a family of secreted signalling molecules that regulate several cellular processes including proliferation, differentiation and migration during the development of the nervous system. Wnt ligands bind frizzled receptors and coreceptors and signal through canonical β-catenin-dependent pathways and noncanonical β-catenin–independent pathways. Dysregulation of Wnt signalling is implicated in various neurological diseases 149. Recent studies have demonstrated a critical role of Wnt signalling in the pathogenesis of neuropathic pain and cancer pain in rodents 148, 149. Nerve injury and bone cancer caused rapid and long-lasting upregulation of Wnts (e.g., Wnt3a, a prototypical Wnt ligand for the canonical pathway), as well as activation of Wnt/frizzled/β-catenin signalling – not only in primary sensory and spinal dorsal horn neurons but also in spinal astrocytes 148. Spinal injection of inhibitors of Wnt signalling pathways into rodents (e.g., Wnt production inhibitor IWP-2 and Wnt scavenger Fz-8/Fc) attenuated the development and maintenance of neuropathic and cancer pain and further blocked nerve injury-induced neuroinflammation (as measured by the expression of Iba1 (ionized calcium-binding adapter molecule 1), GFAP (glial fibrillary acidic protein), IL-18 and TNF-α) in the spinal cord through the β-catenin pathway 148.
Wnt signalling has also been implicated in the development of neuropathic pain after multiple sclerosis. Wnt3a and β-catenin are up-regulated in the spinal cord dorsal horn of mice with experimental autoimmune encephalomyelitis (EAE); inhibition of Wnt5a (using Box-5) and β-catenin (using indomethacin) attenuated mechanical allodynia in mice with EAE 150. Moreover, Wnt ligands and downstream effector proteins are also upregulated in the spinal cord dorsal horn of patients with HIV who developed pain but not in those who did not develop pain 151. Wnt signalling may also directly regulate synaptic plasticity 152 in chronic pain.
Phase I/II trials of inhibitors that target targeting Wnt ligand secretion or recognition or downstream β-catenin function for cancer treatment have been initiated (NCT01345201, NCT01608867, NCT01606579, NCT01302405, and NCT01351103). The major limitation of these inhibitors is side effects, since in addition to cancer cells, other cells that have a high-turnover rate also heavily rely on the Wnt pathway for growth. However, if these inhibitors are proven to be safe they could be potentially used to treat chronic pain, and would be particularly attractive for treating cancer pain, in which both pain and tumour growth can be targeted by the same molecule.
Concluding remarks
Current analgesics focus on reducing pain transduction and transmission in neurons, which explains their limited success in controlling disease progression 31, 153. Mounting evidence suggests that neuroinflammation, as characterized by activation of glial cells, infiltration of leukocytes and the production of inflammatory mediators, has a critical role in the pathogenesis of chronic pain. Chronic pain is regarded as a consequence of “gliopathy”, i.e. dysfunction of glial cells 31. Neuroinflammation drives chronic pain via neuron–glial and neuron–immune cell interactions. We have reviewed the evidence that chemokines (CXCL1, CCL2, and CX3CL1), proteases (MMP-9, cathepsin S and caspase-6), and the Wnt signalling pathway contribute to neuroinflammation and chronic pain sensitization by regulating neuron–glial or glia–neuronal interactions in the spinal cord. Thus, inhibitors of these emerging targets will open new avenues for the development of pain therapeutics.
In the past decade, the development of novel pain therapeutics has been disappointing 154. The failures could be results of complexity of chronic pain mechanisms (peripheral and central, neuronal and non-neuronal), a translational gap from animals to humans (it is a problem to solely rely on evoked reflex behavior for pain measurement in animal models) 155, 156 and inadequate engagement of the claimed drug targets. A recent analysis of 44 Phase II trial decisions shows that the failures are not only caused by lack of efficacy but also, in a large number of cases (43%), by the fact that the mechanisms of action of drugs cannot be adequately tested at appropriate sites 157. Given the fact that chronic pain is operated by distinct mechanisms at different phases, alternative strategies should also be considered for treating pain at early and late phases.
It has to be kept in mind that blocking the proinflammatory signalling of chemokines and proteases can also detrimental effects as well as beneficial effects. Inhibiting the immune response following bacterial or viral infections can be dangerous. Blocking proinflammatory signalling (e.g., MMP-9) in the late recovery phase of brain injury was shown to impair the resolution of neuroinflammation 142. Acute neuroinflammation not only produces proinflammatory mediators but also recruits anti-inflammatory M2 macrophages 27 and generates anti-inflammatory and pro-resolution mediators for the resolution of neuroinflammation and pain (Fig. 2). The PRLMs resolvins, protectins, and lipoxins possess potent anti-inflammatory and anti-nociceptive actions by acting on neurons, immune cells, and glial cells. Notably, these PRLMs are not immune suppressants, and rather they protect against bacterial and viral infection 158, 159. Conceptually, PRLMs are different from classic analgesics, as they do not alter basal pain perception but normalize abnormal pain 101. Although PRLMs have several beneficial actions through multiple mechanisms of actions, their pharmacological properties as drugs need to be improved. One of the most effective treatments for these PRLMs (e.g., PD1/NPD1) is to prevent surgery or trauma-induced chronic pain. Alternative strategies are to develop small molecule agonists to stimulate their receptors and down-stream signal transduction and also boost endogenous production of these powerful lipid mediators through diet control together with low-dose aspirin.
Neuroinflammaiton is not only a driving force for chronic pain, but also implicated in the majority of neurological, psychiatric and neurodevelopmental diseases 25, 160. Given that chronic pain is a comorbidity of many of these diseases, targeting excessive neuroinflammation in the PNS and CNS, without impairing the beneficial function of neuroinflammation, will help to alleviate chronic pain and also control the progression of the underlying diseases.
Glossary
- Mechanical allodynia
a painful response to normally innocuous mechanical stimulation. It is also regarded as a cardinal feature of chronic pain
- Dorsal root ganglion (DRG)
a sensory ganglion of the dorsal root that lies alongside the spinal cord. It is the location of cell bodies of primary sensory neurons including nociceptive and touch neurons that innervate differ body parts
- Trigeminal ganglia
a sensory ganglion of the trigeminal nerve. It is the location of cell bodies of primary sensory neurons including nociceptive and touch neurons that innervate orofacial area
- Primary afferents
afferent fibers of primary sensory neurons that carry sensory information from the periphery to the central nervous system
- Trigeminal nucleus
the sensory nucleus that is located in the brain stem and the trigeminal nucleus caudalis in the medulla is an equivalent of the spinal cord to receive sensory input from the trigeminal system
- Inflammation
a biological response of vascular tissue to harmful stimuli, such as tissue injury, infection, or irritants. The classical signs of acute inflammation are pain, heat, redness, swelling, and loss of function. Acute inflammation is protective and promotes healing process
- Neuroinflammation
local inflammation in the peripheral and central nervous system, which is more efficient to drive chronic pain than systemic inflammation
- Glial mediators
secreted molecules produced by glial cells, including small molecules (e.g., glutamate, ATP, nitric oxide) and large molecule (e.g., proinflammatory cytokines/chemokines and growth factors). They can act as neuromodulators and powerfully modulate nociceptor excitability and nociceptive synaptic transmission
- Mitogen-activated protein kinases (MAPKs)
MAPK family consists of ERK1/2 (extracellular signal–regulated kinase 1/2), p38, JNK (c-Jun N-terminal kinase), and ERK5 and is activated by phosphorylation. MAPKs play important roles in intracellular signalling in neurons and glia and genesis of pain hypersensitivity
- Neurogenic inflammation
inflammation triggered by the activation of primary afferent neurons and subsequent local release of inflammatory mediators such as substance P and calcitonin gene-related peptide. Neurogenic inflammation is responsible for the pathogenesis of migraine
- Chemokines
a family of secreted molecules as small cytokines. They can be classified into 4 subfamilies: C family, CC family, CXC family and CX3C family. There are about 50 chemokines and all exert their functions by activating GPCRs
- Primary sensory neurons
sensory neurons with their cell bodies located in dorsal root and trigeminal ganglia. Their peripheral terminals innervate skin and muscle and their central axons terminate in the spinal cord and trigeminal nucleus
- C fibres
unmyelinated afferent fibres with small diameter and low conduction velocity. They are present in the nerves of somatic sensory system and carry sensory information of pain from the periphery to the central nervous system. They can be activated by capsaicin, an ingredient that gives chili peppers a hot sensation
- Glial activation
transcriptional/translational changes (gene expression), post-translation changes (phosphorylation), morphological changes, and proliferation of glial cells in the PNS and CNS. Glial activation has been strongly implicated in the development and maintenance of chronic pain. Notably, glial cells have different activation states
- Anion reversal potential
the membrane potential at which there is no net flow of that particular anion ion (Cl−) from one side of the membrane to the other. After nerve injury, a decrease in Cl− anion reversal potential (a shift to less negative potentials) reduces glycine/GABAA receptor-mediated hyperpolarization, leading to the genesis of neuropathic pain
- Gate control mechanism
Originally proposed by Ronald Melzack and Patrick Wall during the early 1960s, gate control theory suggests that the spinal cord dorsal horn contains a neural circuit with excitatory and inhibitory modulation that serves as a gate that either allows or blocks pain signals to the brain
- Spinal nerve ligation
a nerve injury condition that can cause long-lasting neuropathic pain in rodents. The spinal nerve ligation model of neuropathic pain is also called Chung model
- Satellite cells
Glial cells that surround neurons in the dorsal root and trigeminal ganglia. Like astrocytes, these cells express glial fibrillary acidic (GFAP) protein and contribute to the pathogenesis of pain
Biography
Dr. Ru-Rong Ji is a Professor at Duke University Medical Center. His research focuses on molecular and cellular mechanisms of persistent pain and development of novel pain therapeutics. Dr. Zhen-Zhong Xu is an Assistant Professor at Duke University Medical Center. He studies how lipid mediators control pain. Dr. Yong-Jing Gao is a Professor of Nantong University in China. She studies how chemokines and astrocytes regulate chronic pain.
Contributor Information
Zhen-Zhong Xu, Email: zhen.xu@duke.edu.
Yong-Jing Gao, Email: gaoyongjing@ntu.edu.cn.
Reference List
- 1.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an Internet-based survey. J Pain. 2010;11:1230–1239. doi: 10.1016/j.jpain.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Stein C, Millan MJ, Herz A. Unilateral inflammation of the hindpaw in rats as a model of prolonged noxious stimulation: alterations in behavior and nociceptive thresholds. Pharmacol Biochem Behav. 1988;31:455–51. doi: 10.1016/0091-3057(88)90372-3. [DOI] [PubMed] [Google Scholar]
- 3.Svensson CI, Zattoni M, Serhan CN. Lipoxins and aspirin-triggered lipoxin inhibit inflammatory pain processing. J Exp Med. 2007;204:245–252. doi: 10.1084/jem.20061826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Honore P, et al. Murine models of inflammatory, neuropathic and cancer pain each generates a unique set of neurochemical changes in the spinal cord and sensory neurons. Neuroscience. 2000;98:585–598. doi: 10.1016/s0306-4522(00)00110-x. [DOI] [PubMed] [Google Scholar]
- 5.Xu Q, et al. Peripheral TGF-beta1 signaling is a critical event in bone cancer-induced hyperalgesia in rodents. J Neurosci. 2013;33:19099–19111. doi: 10.1523/JNEUROSCI.4852-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Decosterd I, Woolf CJ. Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain. 2000;87:149–158. doi: 10.1016/S0304-3959(00)00276-1. [DOI] [PubMed] [Google Scholar]
- 7.Costigan M, Scholz J, Woolf CJ. Neuropathic pain: a maladaptive response of the nervous system to damage. Annu Rev Neurosci. 2009;32:1–32. doi: 10.1146/annurev.neuro.051508.135531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain. 1988;33:87–107. doi: 10.1016/0304-3959(88)90209-6. [DOI] [PubMed] [Google Scholar]
- 9.Kim SH, Chung JM. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 1992;50:355–363. doi: 10.1016/0304-3959(92)90041-9. [DOI] [PubMed] [Google Scholar]
- 10.Basbaum AI, Bautista DM, Scherrer G, Julius D. Cellular and molecular mechanisms of pain. Cell. 2009;139:267–284. doi: 10.1016/j.cell.2009.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gold MS, Levine JD, Correa AM. Modulation of TTX-R INa by PKC and PKA and their role in PGE2-induced sensitization of rat sensory neurons in vitro. J Neurosci. 1998;18:10345–10355. doi: 10.1523/JNEUROSCI.18-24-10345.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aley KO, Levine JD. Role of protein kinase A in the maintenance of inflammatory pain. J Neurosci. 1999;19:2181–2186. doi: 10.1523/JNEUROSCI.19-06-02181.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature. 1983;306:686–688. doi: 10.1038/306686a0. [DOI] [PubMed] [Google Scholar]
- 14.Ossipov MH, Dussor GO, Porreca F. Central modulation of pain. J Clin Invest. 2010;120:3779–3787. doi: 10.1172/JCI43766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chiu IM, et al. Bacteria activate sensory neurons that modulate pain and inflammation. Nature. 2013;501:52–57. doi: 10.1038/nature12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park CK, et al. Extracellular MicroRNAs Activate Nociceptor Neurons to Elicit Pain via TLR7 and TRPA1. Neuron. 2014;82:47–54. doi: 10.1016/j.neuron.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woolf CJ, Salter MW. Neuronal plasticity: increasing the gain in pain. Science. 2000;288:1765–1769. doi: 10.1126/science.288.5472.1765. [DOI] [PubMed] [Google Scholar]
- 18.Hylden JL, Nahin RL, Traub RJ, Dubner R. Expansion of receptive fields of spinal lamina I projection neurons in rats with unilateral adjuvant-induced inflammation: the contribution of dorsal horn mechanisms. Pain. 1989;37:229–243. doi: 10.1016/0304-3959(89)90135-8. [DOI] [PubMed] [Google Scholar]
- 19.Ji RR, Baba H, Brenner GJ, Woolf CJ. Nociceptive-specific activation of ERK in spinal neurons contributes to pain hypersensitivity. Nat Neurosci. 1999;2:1114–1119. doi: 10.1038/16040. [DOI] [PubMed] [Google Scholar]
- 20.Liu XJ, et al. Treatment of inflammatory and neuropathic pain by uncoupling Src from the NMDA receptor complex. Nat Med. 2008;14:1325–1332. doi: 10.1038/nm.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karim F, Wang CC, Gereau RW. Metabotropic glutamate receptor subtypes 1 and 5 are activators of extracellular signal-regulated kinase signaling required for inflammatory pain in mice. J Neurosci. 2001;21:3771–3779. doi: 10.1523/JNEUROSCI.21-11-03771.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Christianson CA, et al. Spinal TLR4 mediates the transition to a persistent mechanical hypersensitivity after the resolution of inflammation in serum-transferred arthritis. Pain. 2011;152:2881–2891. doi: 10.1016/j.pain.2011.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao YJ, Ji RR. Chemokines, neuronal-glial interactions, and central processing of neuropathic pain. Pharmacol Ther. 2010;126:56–68. doi: 10.1016/j.pharmthera.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kawasaki Y, Zhang L, Cheng JK, Ji RR. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci. 2008;28:5189–5194. doi: 10.1523/JNEUROSCI.3338-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rivest S. Regulation of innate immune responses in the brain. Nat Rev Immunol. 2009;9:429–439. doi: 10.1038/nri2565. [DOI] [PubMed] [Google Scholar]
- 26.Grace PM, Hutchinson MR, Maier SF, Watkins LR. Pathological pain and the neuroimmune interface. Nat Rev Immunol. 2014 doi: 10.1038/nri3621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kigerl KA, et al. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J Neurosci. 2009;29:13435–13444. doi: 10.1523/JNEUROSCI.3257-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Costigan M, et al. T-cell infiltration and signaling in the adult dorsal spinal cord is a major contributor to neuropathic pain-like hypersensitivity. J Neurosci. 2009;29:14415–14422. doi: 10.1523/JNEUROSCI.4569-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Old EA, et al. Monocytes expressing CX3CR1 orchestrate the development of vincristine-induced pain. J Clin Invest. 2014;124:2023–2036. doi: 10.1172/JCI71389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ellis A, Bennett DL. Neuroinflammation and the generation of neuropathic pain. Br J Anaesth. 2013;111:26–37. doi: 10.1093/bja/aet128. [DOI] [PubMed] [Google Scholar]
- 31.Ji RR, Berta T, Nedergaard M. Glia and pain: Is chronic pain a gliopathy? Pain. 2013;154(Suppl 1):S10–28. doi: 10.1016/j.pain.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Raghavendra V, Tanga F, DeLeo JA. Inhibition of microglial activation attenuates the development but not existing hypersensitivity in a rat model of neuropathy. J Pharmacol Exp Ther. 2003;306:624–630. doi: 10.1124/jpet.103.052407. [DOI] [PubMed] [Google Scholar]
- 33.Zhang J, De Koninck Y. Spatial and temporal relationship between monocyte chemoattractant protein-1 expression and spinal glial activation following peripheral nerve injury. J Neurochem. 2006;97:772–783. doi: 10.1111/j.1471-4159.2006.03746.x. [DOI] [PubMed] [Google Scholar]
- 34.Katsura H, et al. Activation of Src-family kinases in spinal microglia contributes to mechanical hypersensitivity after nerve injury. J Neurosci. 2006;26:8680–8690. doi: 10.1523/JNEUROSCI.1771-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uceyler N, et al. Small fibre pathology in patients with fibromyalgia syndrome. Brain. 2013;136:1857–1867. doi: 10.1093/brain/awt053. [DOI] [PubMed] [Google Scholar]
- 36.Shi Y, Gelman BB, Lisinicchia JG, Tang SJ. Chronic-pain-associated astrocytic reaction in the spinal cord dorsal horn of human immunodeficiency virus-infected patients. J Neurosci. 2012;32:10833–10840. doi: 10.1523/JNEUROSCI.5628-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xanthos DN, Sandkuhler J. Neurogenic neuroinflammation: inflammatory CNS reactions in response to neuronal activity. Nat Rev Neurosci. 2014;15:43–53. doi: 10.1038/nrn3617. [DOI] [PubMed] [Google Scholar]
- 38.Hathway GJ, Vega-Avelaira D, Moss A, Ingram R, Fitzgerald M. Brief, low frequency stimulation of rat peripheral C-fibres evokes prolonged microglial-induced central sensitization in adults but not in neonates. Pain. 2009;144:110–118. doi: 10.1016/j.pain.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wen YR, et al. Nerve conduction blockade in the sciatic nerve prevents but does not reverse the activation of p38 mitogen-activated protein kinase in spinal microglia in the rat spared nerve injury model. Anesthesiology. 2007;107:312–321. doi: 10.1097/01.anes.0000270759.11086.e7. [DOI] [PubMed] [Google Scholar]
- 40.White FA, Bhangoo SK, Miller RJ. Chemokines: integrators of pain and inflammation. Nat Rev Drug Discov. 2005;4:834–844. doi: 10.1038/nrd1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang J, et al. Expression of CCR2 in both resident and bone marrow-derived microglia plays a critical role in neuropathic pain. J Neurosci. 2007;27:12396–12406. doi: 10.1523/JNEUROSCI.3016-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Echeverry S, Shi XQ, Rivest S, Zhang J. Peripheral nerve injury alters blood-spinal cord barrier functional and molecular integrity through a selective inflammatory pathway. J Neurosci. 2011;31:10819–10828. doi: 10.1523/JNEUROSCI.1642-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beggs S, Liu XJ, Kwan C, Salter MW. Peripheral nerve injury and TRPV1-expressing primary afferent C-fibers cause opening of the blood-brain barrier. Mol Pain. 2010;6:74. doi: 10.1186/1744-8069-6-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nimmerjahn A, Kirchhoff F, Helmchen F. Resting microglial cells are highly dynamic surveillants of brain parenchyma in vivo. Science. 2005;308:1314–1318. doi: 10.1126/science.1110647. [DOI] [PubMed] [Google Scholar]
- 45.McMahon SB, Malcangio M. Current challenges in glia-pain biology. Neuron. 2009;64:46–54. doi: 10.1016/j.neuron.2009.09.033. [DOI] [PubMed] [Google Scholar]
- 46.Schafers M, Geis C, Svensson CI, Luo ZD, Sommer C. Selective increase of tumour necrosis factor-alpha in injured and spared myelinated primary afferents after chronic constrictive injury of rat sciatic nerve. Eur J Neurosci. 2003;17:791–804. doi: 10.1046/j.1460-9568.2003.02504.x. [DOI] [PubMed] [Google Scholar]
- 47.Xu JT, Xin WJ, Zang Y, Wu CY, Liu XG. The role of tumor necrosis factor-alpha in the neuropathic pain induced by Lumbar 5 ventral root transection in rat. Pain. 2006;123:306–321. doi: 10.1016/j.pain.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 48.Berta T, et al. Extracellular caspase-6 drives murine inflammatory pain via microglial TNF-alpha secretion. J Clin Invest. 2014;124:1173–1186. doi: 10.1172/JCI72230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang RX, et al. Spinal glial activation in a new rat model of bone cancer pain produced by prostate cancer cell inoculation of the tibia. Pain. 2005;118:125–136. doi: 10.1016/j.pain.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 50.Clark AK, et al. P2X7-dependent release of interleukin-1beta and nociception in the spinal cord following lipopolysaccharide. J Neurosci. 2010;30:573–582. doi: 10.1523/JNEUROSCI.3295-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Miyoshi K, Obata K, Kondo T, Okamura H, Noguchi K. Interleukin-18-mediated microglia/astrocyte interaction in the spinal cord enhances neuropathic pain processing after nerve injury. J Neurosci. 2008;28:12775–12787. doi: 10.1523/JNEUROSCI.3512-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen ML, et al. Role of P2X7 Receptor-Mediated IL-18/IL-18R Signaling in Morphine Tolerance: Multiple Glial-Neuronal Dialogues in the Rat Spinal Cord. J Pain. 2012;13:945–958. doi: 10.1016/j.jpain.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 53.Imai S, et al. Epigenetic transcriptional activation of monocyte chemotactic protein 3 contributes to long-lasting neuropathic pain. Brain. 2013;136:828–843. doi: 10.1093/brain/aws330. [DOI] [PubMed] [Google Scholar]
- 54.Gao YJ, et al. JNK-induced MCP-1 production in spinal cord astrocytes contributes to central sensitization and neuropathic pain. J Neurosci. 2009;29:4096–4108. doi: 10.1523/JNEUROSCI.3623-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang ZJ, Cao DL, Zhang X, Ji RR, Gao YJ. Chemokine contribution to neuropathic pain: respective induction of CXCL1 and CXCR2 in spinal cord astrocytes and neurons. Pain. 2013;154:2185–2197. doi: 10.1016/j.pain.2013.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lever IJ, et al. Brain-derived neurotrophic factor is released in the dorsal horn by distinctive patterns of afferent fiber stimulation. J Neurosci. 2001;21:4469–4477. doi: 10.1523/JNEUROSCI.21-12-04469.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Coull JA, et al. BDNF from microglia causes the shift in neuronal anion gradient underlying neuropathic pain. Nature. 2005;438:1017–1021. doi: 10.1038/nature04223. [DOI] [PubMed] [Google Scholar]
- 58.Ferrini F, et al. Morphine hyperalgesia gated through microglia-mediated disruption of neuronal Cl(-) homeostasis. Nat Neurosc. 2013;16:183–192. doi: 10.1038/nn.3295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Madiai F, et al. Upregulation of FGF-2 in reactive spinal cord astrocytes following unilateral lumbar spinal nerve ligation. Exp Brain Res. 2003;148:366–376. doi: 10.1007/s00221-002-1286-3. [DOI] [PubMed] [Google Scholar]
- 60.Milligan ED, et al. Intrathecal polymer-based interleukin-10 gene delivery for neuropathic pain. Neuron Glia Biol. 2006;2:293–308. doi: 10.1017/S1740925X07000488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sloane EM, et al. Long-term control of neuropathic pain in a non-viral gene therapy paradigm. Gene Ther. 2009;16:470–475. doi: 10.1038/gt.2009.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Echeverry S, Shi XQ, Zhang J. Characterization of cell proliferation in rat spinal cord following peripheral nerve injury and the relationship with neuropathic pain. Pain. 2008;135:37–47. doi: 10.1016/j.pain.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 63.Tsuda M, et al. JAK-STAT3 pathway regulates spinal astrocyte proliferation and neuropathic pain maintenance in rats. Brain. 2011;134:1127–1139. doi: 10.1093/brain/awr025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang H, Nei H, Dougherty PM. A p38 mitogen-activated protein kinase-dependent mechanism of disinhibition in spinal synaptic transmission induced by tumor necrosis factor-alpha. J Neurosci. 2010;30:12844–12855. doi: 10.1523/JNEUROSCI.2437-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Garraway SM, Petruska JC, Mendell LM. BDNF sensitizes the response of lamina II neurons to high threshold primary afferent inputs. Eur J Neurosci. 2003;18:2467–2476. doi: 10.1046/j.1460-9568.2003.02982.x. [DOI] [PubMed] [Google Scholar]
- 66.Park CK, et al. Resolving TRPV1- and TNF-α-mediated spinal cord synaptic plasticity and inflammatory pain with neuroprotectin D1. J Neurosci. 2011;31:15072–15085. doi: 10.1523/JNEUROSCI.2443-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zeilhofer HU, Benke D, Yevenes GE. Chronic pain states: pharmacological strategies to restore diminished inhibitory spinal pain control. Annu Rev Pharmacol Toxicol. 2012;52:111–133. doi: 10.1146/annurev-pharmtox-010611-134636. [DOI] [PubMed] [Google Scholar]
- 68.Lu Y, et al. A feed-forward spinal cord glycinergic neural circuit gates mechanical allodynia. J Clin Invest. 2013;123:4050–4062. doi: 10.1172/JCI70026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guo W, et al. Glial-cytokine-neuronal interactions underlying the mechanisms of persistent pain. J Neurosci. 2007;27:6006–6018. doi: 10.1523/JNEUROSCI.0176-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Calvo M, et al. Neuregulin-ErbB signaling promotes microglial proliferation and chemotaxis contributing to microgliosis and pain after peripheral nerve injury. J Neurosci. 2010;30:5437–5450. doi: 10.1523/JNEUROSCI.5169-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Oh SB, et al. Chemokines and glycoprotein120 produce pain hypersensitivity by directly exciting primary nociceptive neurons. J Neurosci. 2001;21:5027–5035. doi: 10.1523/JNEUROSCI.21-14-05027.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Verge GM, et al. Fractalkine (CX3CL1) and fractalkine receptor (CX3CR1) distribution in spinal cord and dorsal root ganglia under basal and neuropathic pain conditions. Eur J Neurosci. 2004;20:1150–1160. doi: 10.1111/j.1460-9568.2004.03593.x. [DOI] [PubMed] [Google Scholar]
- 73.Clark AK, et al. Inhibition of spinal microglial cathepsin S for the reversal of neuropathic pain. Proc Natl Acad Sci U S A. 2007;104:10655–10660. doi: 10.1073/pnas.0610811104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhuang ZY, et al. Role of the CX3CR1/p38 MAPK pathway in spinal microglia for the development of neuropathic pain following nerve injury-induced cleavage of fractalkine. Brain Behav Immun. 2007;21:642–651. doi: 10.1016/j.bbi.2006.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Milligan ED, et al. Evidence that exogenous and endogenous fractalkine can induce spinal nociceptive facilitation in rats. Eur J Neurosci. 2004;20:2294–2302. doi: 10.1111/j.1460-9568.2004.03709.x. [DOI] [PubMed] [Google Scholar]
- 76.Dorgham K, et al. An engineered CX3CR1 antagonist endowed with anti-inflammatory activity. J Leukoc Biol. 2009;86:903–911. doi: 10.1189/jlb.0308158. [DOI] [PubMed] [Google Scholar]
- 77.Abbadie C, et al. Impaired neuropathic pain responses in mice lacking the chemokine receptor CCR2. Proc Natl Acad Sci U S A. 2003;100:7947–7952. doi: 10.1073/pnas.1331358100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Thacker MA, et al. CCL2 is a key mediator of microglia activation in neuropathic pain states. Eur J Pain. 2009;13:263–272. doi: 10.1016/j.ejpain.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 79.Guo W, Wang H, Zou S, Dubner R, Ren K. Chemokine signaling involving chemokine (C-C motif) ligand 2 plays a role in descending pain facilitation. Neurosci Bull. 2012;28:193–207. doi: 10.1007/s12264-012-1218-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang ZJ, et al. Chemokine CCL2 and its receptor CCR2 in the medullary dorsal horn are involved in trigeminal neuropathic pain. J Neuroinflammation. 2012;9:136. doi: 10.1186/1742-2094-9-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Menetski J, et al. Mice overexpressing chemokine ligand 2 (CCL2) in astrocytes display enhanced nociceptive responses. Neuroscience. 2007;149:706–714. doi: 10.1016/j.neuroscience.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 82.Omari KM, John G, Lango R, Raine CS. Role for CXCR2 and CXCL1 on glia in multiple sclerosis. Glia. 2006;53:24–31. doi: 10.1002/glia.20246. [DOI] [PubMed] [Google Scholar]
- 83.Li H, Xie W, Strong JA, Zhang JM. Systemic antiinflammatory corticosteroid reduces mechanical pain behavior, sympathetic sprouting, and elevation of proinflammatory cytokines in a rat model of neuropathic pain. Anesthesiology. 2007;107:469–477. doi: 10.1097/01.anes.0000278907.37774.8d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pineau I, Sun L, Bastien D, Lacroix S. Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain Behav Immun. 2010;24:540–553. doi: 10.1016/j.bbi.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 85.Zhao P, Waxman SG, Hains BC. Modulation of thalamic nociceptive processing after spinal cord injury through remote activation of thalamic microglia by cysteine cysteine chemokine ligand 21. J Neurosci. 2007;27:8893–8902. doi: 10.1523/JNEUROSCI.2209-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Biber K, et al. Neuronal CCL21 up-regulates microglia P2X4 expression and initiates neuropathic pain development. EMBO J. 2011;30:1864–1873. doi: 10.1038/emboj.2011.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tsuda M, et al. P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature. 2003;424:778–783. doi: 10.1038/nature01786. [DOI] [PubMed] [Google Scholar]
- 88.Bhangoo SK, et al. CXCR4 chemokine receptor signaling mediates pain hypersensitivity in association with antiretroviral toxic neuropathy. Brain Behav Immun. 2007;21:581–591. doi: 10.1016/j.bbi.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kiguchi N, Maeda T, Kobayashi Y, Fukazawa Y, Kishioka S. Macrophage inflammatory protein-1alpha mediates the development of neuropathic pain following peripheral nerve injury through interleukin-1beta up-regulation. Pain. 2010;149:305–315. doi: 10.1016/j.pain.2010.02.025. [DOI] [PubMed] [Google Scholar]
- 90.Matsushita K, et al. Chemokine (C-C motif) Receptor 5 Is an Important Pathological Regulator in the Development and Maintenance of Neuropathic Pain. Anesthesiology. 2014 doi: 10.1097/ALN.0000000000000190. [DOI] [PubMed] [Google Scholar]
- 91.Weitzenfeld P, Ben-Baruch A. The chemokine system, and its CCR5 and CXCR4 receptors, as potential targets for personalized therapy in cancer. Cancer Lett. 2013 doi: 10.1016/j.canlet.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 92.White FA, et al. Excitatory monocyte chemoattractant protein-1 signaling is up-regulated in sensory neurons after chronic compression of the dorsal root ganglion. Proc Natl Acad Sci U S A. 2005;102:14092–14097. doi: 10.1073/pnas.0503496102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kalliomaki J, et al. A randomized, double-blind, placebo-controlled trial of a chemokine receptor 2 (CCR2) antagonist in posttraumatic neuralgia. Pain. 2013;154:761–767. doi: 10.1016/j.pain.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 94.Padi SS, et al. Attenuation of rodent neuropathic pain by an orally active peptide, RAP-103, which potently blocks. Pain. 2012;153:95–106. doi: 10.1016/j.pain.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 95.Virtala R, Ekman AK, Jansson L, Westin U, Cardell LO. Airway inflammation evaluated in a human nasal lipopolysaccharide challenge model by investigating the effect of a CXCR2 inhibitor. Clin Exp Allergy. 2012;42:590–596. doi: 10.1111/j.1365-2222.2011.03921.x. [DOI] [PubMed] [Google Scholar]
- 96.Lazaar AL, et al. SB-656933, a novel CXCR2 selective antagonist, inhibits ex vivo neutrophil activation and ozone-induced airway inflammation in humans. Br J Clin Pharmacol. 2011;72:282–293. doi: 10.1111/j.1365-2125.2011.03968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Holz O, et al. SCH527123, a novel CXCR2 antagonist, inhibits ozone-induced neutrophilia in healthy subjects. Eur Respir J. 2010;35:564–570. doi: 10.1183/09031936.00048509. [DOI] [PubMed] [Google Scholar]
- 98.Xu ZZ, et al. Neuroprotectin/Protectin D1 protects neuropathic pain in mice after nerve trauma. Ann Neurol. 2013;74:490–495. doi: 10.1002/ana.23928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Xu ZZ, et al. Resolvins RvE1 and RvD1 attenuate inflammatory pain via central and peripheral actions. Nat Med. 2010;16:592–7. doi: 10.1038/nm.2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Connor KM, et al. Increased dietary intake of omega-3-polyunsaturated fatty acids reduces pathological retinal angiogenesis. Nat Med. 2007;13:868–873. doi: 10.1038/nm1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ji RR, Xu ZZ, Strichartz G, Serhan CN. Emerging roles of resolvins in the resolution of inflammation and pain. Trends Neurosci. 2011;34:599–609. doi: 10.1016/j.tins.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Serhan CN, et al. Resolvins: a family of bioactive products of omega-3 fatty acid transformation circuits initiated by aspirin treatment that counter proinflammation signals. J Exp Med. 2002;196:1025–1037. doi: 10.1084/jem.20020760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hong S, Gronert K, Devchand PR, Moussignac RL, Serhan CN. Novel docosatrienes and 17S-resolvins generated from docosahexaenoic acid in murine brain, human blood, and glial cells. Autacoids in anti-inflammation. J Biol Chem. 2003;278:14677–14687. doi: 10.1074/jbc.M300218200. [DOI] [PubMed] [Google Scholar]
- 104.Arita M, et al. Resolvin E1, an endogenous lipid mediator derived from omega-3 eicosapentaenoic acid, protects against 2,4,6-trinitrobenzene sulfonic acid-induced colitis. Proc Natl Acad Sci U S A. 2005;102:7671–7676. doi: 10.1073/pnas.0409271102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Seki H, et al. The anti-inflammatory and proresolving mediator resolvin E1 protects mice from bacterial pneumonia and acute lung injury. J Immunol. 2010;184:836–843. doi: 10.4049/jimmunol.0901809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Duffield JS, et al. Resolvin D series and protectin D1 mitigate acute kidney injury. J Immunol. 2006;177:5902–5911. doi: 10.4049/jimmunol.177.9.5902. [DOI] [PubMed] [Google Scholar]
- 107.Mukherjee PK, Marcheselli VL, Serhan CN, Bazan NG. Neuroprotectin D1: a docosahexaenoic acid-derived docosatriene protects human retinal pigment epithelial cells from oxidative stress. Proc Natl Acad Sci U S A. 2004;101:8491–8496. doi: 10.1073/pnas.0402531101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lukiw WJ, et al. A role for docosahexaenoic acid-derived neuroprotectin D1 in neural cell survival and Alzheimer disease. J Clin Invest. 2005;115:2774–2783. doi: 10.1172/JCI25420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bazan NG. Neuroprotectin D1-mediated anti-inflammatory and survival signaling in stroke, retinal degenerations, and Alzheimer’s disease. J Lipid Res. 2009;50 (Suppl):S400–S405. doi: 10.1194/jlr.R800068-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bazan NG, Calandria JM, Serhan CN. Rescue and repair during photoreceptor cell renewal mediated by docosahexaenoic acid-derived neuroprotectin D1. J Lipid Res. 2010;51:2018–2031. doi: 10.1194/jlr.R001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Palacios-Pelaez R, Lukiw WJ, Bazan NG. Omega-3 essential fatty acids modulate initiation and progression of neurodegenerative disease. Mol Neurobiol. 2010;41:367–374. doi: 10.1007/s12035-010-8139-z. [DOI] [PubMed] [Google Scholar]
- 112.Serhan CN, et al. Anti-inflammatory actions of neuroprotectin D1/protectin D1 and its natural stereoisomers: assignments of dihydroxy-containing docosatrienes. J Immunol. 2006;176:1848–1859. doi: 10.4049/jimmunol.176.3.1848. [DOI] [PubMed] [Google Scholar]
- 113.Samad TA, et al. Interleukin-1beta-mediated induction of Cox-2 in the CNS contributes to inflammatory pain hypersensitivity. Nature. 2001;410:471–475. doi: 10.1038/35068566. [DOI] [PubMed] [Google Scholar]
- 114.Arita M, et al. Resolvin E1 selectively interacts with leukotriene B4 receptor BLT1 and ChemR23 to regulate inflammation. J Immunol. 2007;178:3912–3917. doi: 10.4049/jimmunol.178.6.3912. [DOI] [PubMed] [Google Scholar]
- 115.Krishnamoorthy S, et al. Resolvin D1 binds human phagocytes with evidence for proresolving receptors. Proc Natl Acad Sci U S A. 2010;107:1660–1665. doi: 10.1073/pnas.0907342107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–1625. doi: 10.1016/S0140-6736(06)68700-X. [DOI] [PubMed] [Google Scholar]
- 117.Bian D, Nichols ML, Ossipov MH, Lai J, Porreca F. Characterization of the antiallodynic efficacy of morphine in a model of neuropathic pain in rats. Neuroreport. 1995;6:1981–1984. doi: 10.1097/00001756-199510010-00007. [DOI] [PubMed] [Google Scholar]
- 118.Kohno T, et al. Peripheral axonal injury results in reduced mu opioid receptor pre- and post-synaptic action in the spinal cord. Pain. 2005;117:77–87. doi: 10.1016/j.pain.2005.05.035. [DOI] [PubMed] [Google Scholar]
- 119.Boucher TJ, et al. Potent analgesic effects of GDNF in neuropathic pain states. Science. 2000;290:124–127. doi: 10.1126/science.290.5489.124. [DOI] [PubMed] [Google Scholar]
- 120.Gardell LR, et al. Multiple actions of systemic artemin in experimental neuropathy. Nat Med. 2003;9:1383–1389. doi: 10.1038/nm944. [DOI] [PubMed] [Google Scholar]
- 121.Xu ZZ, Berta T, Ji RR. Resolvin E1 inhibits neuropathic pain and spinal cord microglial activation following peripheral nerve injury. J Neuroimmune Pharmacol. 2013;8:37–41. doi: 10.1007/s11481-012-9394-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tsujino H, et al. Activating transcription factor 3 (ATF3) induction by axotomy in sensory and motoneurons: A novel neuronal marker of nerve injury. Mol Cell Neurosci. 2000;15:170–182. doi: 10.1006/mcne.1999.0814. [DOI] [PubMed] [Google Scholar]
- 123.Park CK, et al. Resolvin d2 is a potent endogenous inhibitor for transient receptor potential subtype v1/a1, inflammatory pain, and spinal cord synaptic plasticity in mice: distinct roles of resolvin d1, d2, and e1. J Neurosci. 2011;31:18433–18438. doi: 10.1523/JNEUROSCI.4192-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lima-Garcia JF, et al. The precursor of resolvin D series and aspirin-triggered resolvin D1 display anti-hyperalgesic properties in adjuvant-induced arthritis in rats. Br J Pharmacol. 2011;164:278–293. doi: 10.1111/j.1476-5381.2011.01345.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Patapoutian A, Tate S, Woolf CJ. Transient receptor potential channels: targeting pain at the source. Nat Rev Drug Discov. 2009;8:55–68. doi: 10.1038/nrd2757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Caterina MJ, et al. Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science. 2000;288:306–313. doi: 10.1126/science.288.5464.306. [DOI] [PubMed] [Google Scholar]
- 127.Chen Y, et al. Temporomandibular joint pain: a critical role for Trpv4 in the trigeminal ganglion. Pain. 2013;154:1295–1304. doi: 10.1016/j.pain.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Patwardhan AM, et al. Heat generates oxidized linoleic acid metabolites that activate TRPV1 and produce pain in rodents. J Clin Invest. 2010;120:1617–1626. doi: 10.1172/JCI41678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sisignano M, Bennett DL, Geisslinger G, Scholich K. TRP-channels as key integrators of lipid pathways in nociceptive neurons. Prog Lipid Res. 2013;53C:93–107. doi: 10.1016/j.plipres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 130.Bang S, et al. Resolvin D1 attenuates activation of sensory transient receptor potential channels leading to multiple anti-nociception. Br J Pharmacol. 2010;161:707–720. doi: 10.1111/j.1476-5381.2010.00909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Serhan CN, et al. Macrophage proresolving mediator maresin 1 stimulates tissue regeneration and controls pain. FASEB J. 2012;26:1755–1765. doi: 10.1096/fj.11-201442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Finnerup NB, Sindrup SH, Jensen TS. The evidence for pharmacological treatment of neuropathic pain. Pain. 2010;150:573–581. doi: 10.1016/j.pain.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 133.Sommer C, Birklein F. Fighting off pain with resolvins. Nat Med. 2010;16:518–520. doi: 10.1038/nm0510-518. [DOI] [PubMed] [Google Scholar]
- 134.Nikolajsen L, Ilkjaer S, Christensen JH, Kroner K, Jensen TS. Randomised trial of epidural bupivacaine and morphine in prevention of stump and phantom pain in lower-limb amputation. Lancet. 1997;350:1353–1357. doi: 10.1016/S0140-6736(97)06315-0. [DOI] [PubMed] [Google Scholar]
- 135.Ramsden CE, et al. Targeted alteration of dietary n-3 and n-6 fatty acids for the treatment of chronic headaches: a randomized trial. Pain. 2013;154:2441–2451. doi: 10.1016/j.pain.2013.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Chiang N, Bermudez EA, Ridker PM, Hurwitz S, Serhan CN. Aspirin triggers antiinflammatory 15-epi-lipoxin A4 and inhibits thromboxane in a randomized human trial. Proc Natl Acad Sci U S A. 2004;101:15178–15183. doi: 10.1073/pnas.0405445101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Morris T, et al. Effects of low-dose aspirin on acute inflammatory responses in humans. J Immunol. 2009;183:2089–2096. doi: 10.4049/jimmunol.0900477. [DOI] [PubMed] [Google Scholar]
- 138.Kawasaki Y, et al. Distinct roles of matrix metalloproteases in the early- and late-phase development of neuropathic pain. Nat Med. 2008;14:331–336. doi: 10.1038/nm1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Clark AK, Malcangio M. Microglial signalling mechanisms: Cathepsin S and Fractalkine. Exp Neurol. 2012;234:283–292. doi: 10.1016/j.expneurol.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 140.Guo SL, et al. Cystatin C in Cerebrospinal Fluid is Upregulated in Elderly Patients With Chronic Osteoarthritis Pain and Modulated Through Matrix Metalloproteinase 9-Specific Pathway. Clin J Pain. 2013;30:331–339. doi: 10.1097/AJP.0b013e31829ca60b. [DOI] [PubMed] [Google Scholar]
- 141.Christianson CA, et al. Spinal matrix metalloproteinase 3 mediates inflammatory hyperalgesia via a tumor necrosis factor-dependent mechanism. Neuroscience. 2012;200:199–210. doi: 10.1016/j.neuroscience.2011.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhao BQ, et al. Role of matrix metalloproteinases in delayed cortical responses after stroke. Nat Med. 2006;12:441–445. doi: 10.1038/nm1387. [DOI] [PubMed] [Google Scholar]
- 143.Bissett D, et al. Phase III study of matrix metalloproteinase inhibitor prinomastat in non-small-cell lung cancer. J Clin Oncol. 2005;23:842–849. doi: 10.1200/JCO.2005.03.170. [DOI] [PubMed] [Google Scholar]
- 144.Miller KD, et al. A randomized phase II feasibility trial of BMS-275291 in patients with early stage breast cancer. Clin Cancer Res. 2004;10:1971–1975. doi: 10.1158/1078-0432.ccr-03-0968. [DOI] [PubMed] [Google Scholar]
- 145.Hu J, Van den Steen PE, Sang QX, Opdenakker G. Matrix metalloproteinase inhibitors as therapy for inflammatory and vascular diseases. Nat Rev Drug Discov. 2007;6:480–498. doi: 10.1038/nrd2308. [DOI] [PubMed] [Google Scholar]
- 146.Williams JM, et al. Evaluation of metalloprotease inhibitors on hypertension and diabetic nephropathy. Am J Physiol Renal Physiol. 2011;300:F983–F998. doi: 10.1152/ajprenal.00262.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Clark AK, Yip PK, Malcangio M. The liberation of fractalkine in the dorsal horn requires microglial cathepsin S. J Neurosci. 2009;29:6945–6954. doi: 10.1523/JNEUROSCI.0828-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhang YK, et al. WNT signaling underlies the pathogenesis of neuropathic pain in rodents. J Clin Invest. 2013;123:2268–2286. doi: 10.1172/JCI65364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Tang SJ. Synaptic Activity-Regulated Wnt Signaling in Synaptic Plasticity, Glial Function and Chronic Pain. CNS Neurol Disord Drug Targets. 2013 doi: 10.2174/1871527312666131223114457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Yuan S, Shi Y, Tang SJ. Wnt signaling in the pathogenesis of multiple sclerosis-associated chronic pain. J Neuroimmune Pharmacol. 2012;7:904–913. doi: 10.1007/s11481-012-9370-3. [DOI] [PubMed] [Google Scholar]
- 151.Shi Y, Shu J, Gelman BB, Lisinicchia JG, Tang SJ. Wnt signaling in the pathogenesis of human HIV-associated pain syndromes. J Neuroimmune Pharmacol. 2013;8:956–964. doi: 10.1007/s11481-013-9474-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chen J, Park CS, Tang SJ. Activity-dependent synaptic Wnt release regulates hippocampal long term potentiation. J Biol Chem. 2006;281:11910–11916. doi: 10.1074/jbc.M511920200. [DOI] [PubMed] [Google Scholar]
- 153.Watkins LR, Maier SF. Glia: a novel drug discovery target for clinical pain. Nat Rev Drug Discov. 2003;2:973–985. doi: 10.1038/nrd1251. [DOI] [PubMed] [Google Scholar]
- 154.Woolf CJ. Overcoming obstacles to developing new analgesics. Nat Med. 2010;16:1241–1247. doi: 10.1038/nm.2230. [DOI] [PubMed] [Google Scholar]
- 155.Mogil JS. Animal models of pain: progress and challenges. Nat Rev Neurosci. 2009;10:283–294. doi: 10.1038/nrn2606. [DOI] [PubMed] [Google Scholar]
- 156.King T, et al. Unmasking the tonic-aversive state in neuropathic pain. Nat Neurosci. 2009;12:1364–1366. doi: 10.1038/nn.2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Morgan P, et al. Can the flow of medicines be improved? Fundamental pharmacokinetic and pharmacological principles toward improving Phase II survival. Drug Discov Today. 2012;17:419–424. doi: 10.1016/j.drudis.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 158.Chiang N, et al. Infection regulates pro-resolving mediators that lower antibiotic requirements. Nature. 2012;484:524–528. doi: 10.1038/nature11042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Morita M, et al. The lipid mediator protectin d1 inhibits influenza virus replication and improves severe influenza. Cell. 2013;153:112–125. doi: 10.1016/j.cell.2013.02.027. [DOI] [PubMed] [Google Scholar]
- 160.Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol. 2005;57:67–81. doi: 10.1002/ana.20315. [DOI] [PubMed] [Google Scholar]
- 161.Polgar E, Gray S, Riddell JS, Todd AJ. Lack of evidence for significant neuronal loss in laminae I-III of the spinal dorsal horn of the rat in the chronic constriction injury model. Pain. 2004;111:144–150. doi: 10.1016/j.pain.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 162.Scholz J, et al. Blocking caspase activity prevents transsynaptic neuronal apoptosis and the loss of inhibition in lamina II of the dorsal horn after peripheral nerve injury. J Neurosci. 2005;25:7317–7323. doi: 10.1523/JNEUROSCI.1526-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Vereker E, O’Donnell E, Lynch MA. The inhibitory effect of interleukin-1beta on long-term potentiation is coupled with increased activity of stress-activated protein kinases. J Neurosci. 2000;20:6811–6819. doi: 10.1523/JNEUROSCI.20-18-06811.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ren WJ, et al. Peripheral nerve injury leads to working memory deficits and dysfunction of the hippocampus by upregulation of TNF-alpha in rodents. Neuropsychopharmacology. 2011;36:979–992. doi: 10.1038/npp.2010.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Liu YL, et al. Tumor necrosis factor-alpha induces long-term potentiation of C-fiber evoked field potentials in spinal dorsal horn in rats with nerve injury: the role of NF-kappa B, JNK and p38 MAPK. Neuropharmacology. 2007;52:708–715. doi: 10.1016/j.neuropharm.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 166.Choi JI, Svensson CI, Koehrn FJ, Bhuskute A, Sorkin LS. Peripheral inflammation induces tumor necrosis factor dependent AMPA receptor trafficking and Akt phosphorylation in spinal cord in addition to pain behavior. Pain. 2010;149:243–253. doi: 10.1016/j.pain.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Hess A, et al. Blockade of TNF-alpha rapidly inhibits pain responses in the central nervous system. Proc Natl Acad Sci U S A. 2011;108:3731–3736. doi: 10.1073/pnas.1011774108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Calvo M, Bennett DL. The mechanisms of microgliosis and pain following peripheral nerve injury. Exp Neurol. 2012;234:271–282. doi: 10.1016/j.expneurol.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 169.Garrison CJ, Dougherty PM, Kajander KC, Carlton SM. Staining of glial fibrillary acidic protein (GFAP) in lumbar spinal cord increases following a sciatic nerve constriction injury. Brain Res. 1991;565:1–7. doi: 10.1016/0006-8993(91)91729-k. [DOI] [PubMed] [Google Scholar]
- 170.Raghavendra V, Tanga FY, DeLeo JA. Complete Freunds adjuvant-induced peripheral inflammation evokes glial activation and proinflammatory cytokine expression in the CNS. Eur J Neurosci. 2004;20:467–473. doi: 10.1111/j.1460-9568.2004.03514.x. [DOI] [PubMed] [Google Scholar]
- 171.Colburn RW, et al. Dissociation of microglial activation and neuropathic pain behaviors following peripheral nerve injury in the rat. J Neuroimmunol. 1997;79:163–175. doi: 10.1016/s0165-5728(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 172.Moss A, et al. Spinal microglia and neuropathic pain in young rats. Pain. 2007;128:215–224. doi: 10.1016/j.pain.2006.09.018. [DOI] [PubMed] [Google Scholar]
- 173.Ji RR, Gereau RW, Malcangio M, Strichartz GR. MAP kinase and pain. Brain Res Rev. 2009;60:135–148. doi: 10.1016/j.brainresrev.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zhuang ZY, Gerner P, Woolf CJ, Ji RR. ERK is sequentially activated in neurons, microglia, and astrocytes by spinal nerve ligation and contributes to mechanical allodynia in this neuropathic pain model. Pain. 2005;114:149–159. doi: 10.1016/j.pain.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 175.Zhuang ZY, et al. A peptide c-Jun N-terminal kinase (JNK) inhibitor blocks mechanical allodynia after spinal nerve ligation: respective roles of JNK activation in primary sensory neurons and spinal astrocytes for neuropathic pain development and maintenance. J Neurosci. 2006;26:3551–3560. doi: 10.1523/JNEUROSCI.5290-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Obata K, et al. Roles of extracellular signal-regulated protein kinases 5 in spinal microglia and primary sensory neurons for neuropathic pain. J Neurochem. 2007;102:1569–1584. doi: 10.1111/j.1471-4159.2007.04656.x. [DOI] [PubMed] [Google Scholar]
- 177.Tozaki-Saitoh H, et al. P2Y12 receptors in spinal microglia are required for neuropathic pain after peripheral nerve injury. J Neurosci. 2008;28:4949–4956. doi: 10.1523/JNEUROSCI.0323-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kobayashi K, et al. P2Y12 receptor upregulation in activated microglia is a gateway of p38 signaling and neuropathic pain. J Neurosci. 2008;28:2892–2902. doi: 10.1523/JNEUROSCI.5589-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kobayashi K, Yamanaka H, Yanamoto F, Okubo M, Noguchi K. Multiple P2Y subtypes in spinal microglia are involved in neuropathic pain after peripheral nerve injury. Glia. 2012 doi: 10.1002/glia.22373. [DOI] [PubMed] [Google Scholar]
- 180.Sorge RE, et al. Genetically determined P2X7 receptor pore formation regulates variability in chronic pain sensitivity. Nat Med. 2012;18:595–599. doi: 10.1038/nm.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Cotrina ML, Lin JH, Lopez-Garcia JC, Naus CC, Nedergaard M. ATP-mediated glia signaling. J Neurosci. 2000;20:2835–2844. doi: 10.1523/JNEUROSCI.20-08-02835.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Chen MJ, et al. Astrocytic CX43 hemichannels and gap junctions play a crucial role in development of chronic neuropathic pain following spinal cord injury. Glia. 2012;60:1660–1670. doi: 10.1002/glia.22384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Zhang F, et al. Selective activation of microglia in spinal cord but not higher cortical regions following nerve injury in adult mouse. Mol Pain. 2008;4:15. doi: 10.1186/1744-8069-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Sung B, Lim G, Mao J. Altered expression and uptake activity of spinal glutamate transporters after nerve injury contribute to the pathogenesis of neuropathic pain in rats. J Neurosci. 2003;23:2899–2910. doi: 10.1523/JNEUROSCI.23-07-02899.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Tsuda M, Inoue K, Salter MW. Neuropathic pain and spinal microglia: a big problem from molecules in “small” glia. Trends Neurosci. 2005;28:101–107. doi: 10.1016/j.tins.2004.12.002. [DOI] [PubMed] [Google Scholar]