Abstract
Background:
Misuse of topical corticosteroids is a widespread phenomenon among young people in India, especially women. The practice is associated with significant adverse effects and poor awareness of these effects among the general public.
Aim:
This study was conducted to examine the misuse and adverse effects of topical corticosteroids among the people in Bastar region in Chhattisgarh state of India.
Materials and Methods:
Data collected from patients presenting with at least one of the adverse effects of topical corticosteroids as the chief complaint, from November 2010 to October 2011.
Results:
Out of the 6723 new patients, 379 (5.63%) had presented with misuse and adverse effects of topical corticosteroids, of whom 78.89% were females. More than 65% of the patients were in the age group 10-29 years. The main reason for using the topical corticosteroids was to lighten skin colour and treat melasma and suntan. Acne (37.99%) and telangiectasia (18.99%) were the most common adverse effects noted.
Conclusions:
Misuse of topical corticosteroids has a huge impact on dermatological practice, leading to a significant proportion of visits to the dermatologist. This hydra-headed problem needs multi-dimensional interventions, involving educational, legal and managerial approaches with cooperation from different sectors of society.
Keywords: Cutaneous atrophy, misuse, steroid acne, topical corticosteroid
INTRODUCTION
Topical corticosteroids have made a dramatic contribution to dermatology since the introduction of “compound F” or hydrocortisone in 1952[1] and have become the mainstay of dermatologic treatment of a wide range of inflammatory and non-infectious conditions. Topical corticosteroids are today among the most commonly prescribed medications in dermatology clinics. The clinical effects are mediated by their anti-inflammatory, vasoconstrictive, anti-proliferative and immunosuppressive properties.[2,3]
As potent topical corticosteroids are easily available over-the-counter at a low price, misuse has been noticed among the general population, producing many adverse effects. In spite of being a common problem, only few studies have investigated the misuse of topical corticosteroid products in India.[4,5]
AIM
This study was conducted among the people living in the state of Chhattisgarh, India to assess the frequency of topical corticosteroids misuse, the reasons behind it and the most common adverse effects resulting from it.
METHODS
Patients were recruited for the study from the dermatology out-patient department during the period from November 2010 to October 2011. The patients studied were those who had used topical corticosteroids incorrectly (i.e. for conditions where topical corticosteroids were either not indicated or if indicated, the dose, frequency of application and/or the duration of application was not appropriate) and presented with at least one of the following adverse effects as chief complaint: acne, facial hypertrichosis, plethoric face and telangiectasia, cutaneous atrophy, stretch marks, hyper/hypo pigmentation, tinea incognito, perioral dermatitis, infantile gluteal granuloma and pyoderma.
Patients were interviewed using a self-prepared questionnaire covering their personal details such as age, gender, employment, marital status, education level, duration and frequency of application of topical corticosteroid and the reasons for using the drug, awareness of proper dosing and adverse effects. Patients were also asked about who had prescribed/recommended the remedy. A full skin examination was performed to detect any condition related to abuse of topical corticosteroids. Most of the diagnoses were exclusively clinical, and were based on the typical, classical features. Potassium hydroxide preparation was made in cases of suspected dermatophyte infection. Potential systemic adverse effects were not investigated in this study.
RESULTS
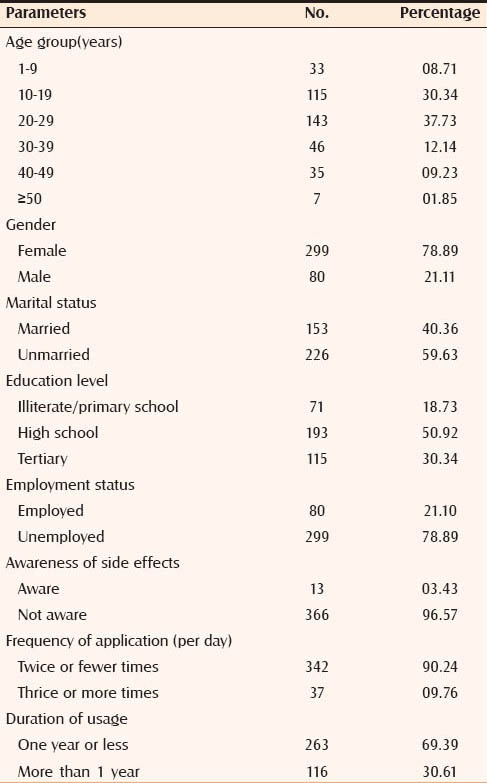
Out of the 6723 new patients seen during the study period, 379 (5.63%) presented with adverse effects of topical corticosteroids resulting from the misuse of these drugs, of whom 78.89% were females. More than 65% of the patients were in the age group of 10-29 years. The mean duration of use was 7.4 months (range: 1-60 months). Only 3.43% patients had some idea of the adverse effects of topical corticosteroids. Most of the patients (96.57%) had not read the leaflet (package insert), either because they were illiterate or because the drug provider had not given any information about the adverse effects, or the drug was supplied without a leaflet. None of the patients knew the dosage, i.e. how much of the drug should be used per body area. The number of applications varied from once daily to 3-4 times a day. Demographic characteristics are listed in Table 1.
Table 1.
Demographic status of patients (n=379)
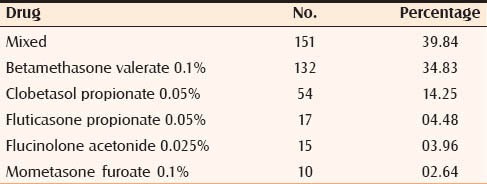
The various topical corticosteroids used are summarized in Table 2. Potent and very potent preparations were used by 88.92% patients, including those who used topical combination preparations of corticosteroid, antibiotic and/or antifungal. Corticosteroids not misused by patients in this study were halobetasol, clobetasol, triamcinolone, desonide and hydrocortisone. This may be because of the limited availability of these products in the area and also because of restricted use, by dermatologists only.
Table 2.
Topical corticosteroid formulation misused
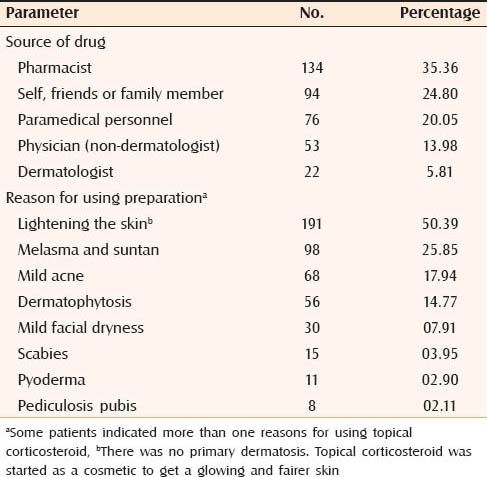
Most of the patients were using topical corticosteroids on advice of pharmacists or paramedical personnel; others were advised by friends and relatives. Only in a few patients were topical corticosteroids prescribed by a physician or a dermatologist. Lightening of skin colour was the main reason for using topical corticosteroids in 50.39% patients in the absence of any primary dermatosis. Another 25.85% of patients used topical corticosteroids for treatment of melasma and suntan. Other reasons for use were acne, dermatophytosis, facial dryness, pyodermas, scabies and pediculosis pubis [Table 3]. Some patients indicated more than one reason for using these medications.
Table 3.
Sources and reasons for using topical corticosteroids (n=379)
The dermatological adverse effects seen after application of topical corticosteroids are listed in Table 4. Acne and plethoric, puffy face with telangiectasia (steroid face) were the most common adverse effects noted. Patients who presented with acneiform eruptions had sudden onset of lesions at the sites of application with predominance of papulopustular lesions. Other adverse effects were facial hypertrichosis, pigmentation disorders, pyodermas, tinea incognito, cutaneous atrophy and perioral dermatitis. Photographs representing some of the adverse effects are shown as Figures 1–8.
Table 4.
Dermatological adverse effects seen (n=379)a
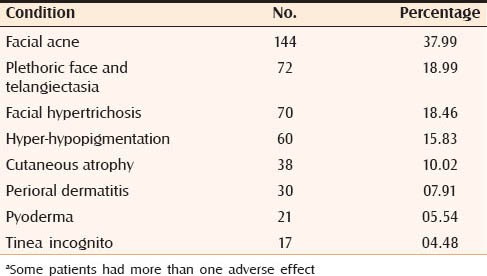
Figure 1.

Steroid acne presenting as small, firm, monomorphic, follicular papules over the forehead
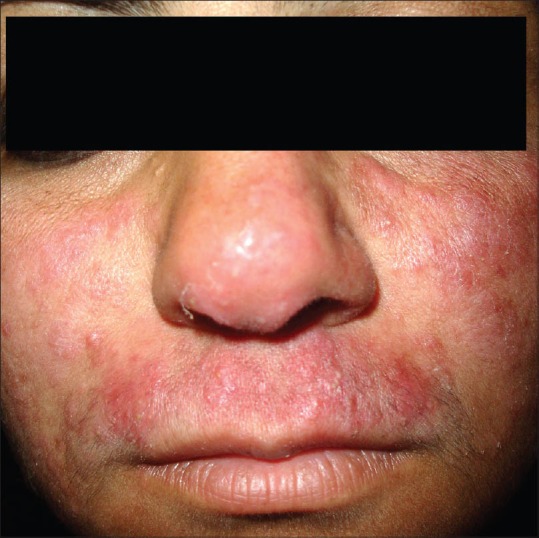
Figure 8.

Perioral dermatitis in 23-year-old girl showing multiple small erythematous papules that are localised to the perioral skin and nasolabial folds
Figure 2.

Steroid acne on the face characterized by pustules and erythema
Figure 3.

Generalized facial erythema due to of telangiectasia, after inappropriate use of high-potency corticosteroids for long term
Figure 4.

Steroid induced hypertrichosis: The patient had continued treatment with topical corticosteroids for 10 months
Figure 5.

Hypopigmentation caused by long term use of topical corticosteroids
Figure 6.
Tinea incognito: The patient had applied topical corticosteroids that masked a diagnosis of tinea
Figure 7.

Cutaneous atrophy, a sign of topical corticosteroid abuse, over the left axillary region of a 23-year-old male
DISCUSSION
Misuse of topical corticosteroids appears to be a common problem in India, as indicated by the proportion of patients visiting the Department of Dermatology with adverse effects of these drugs. The real problem is probably even greater, as, at the time of the study, many people who had used these drugs may not have presented to the dermatologist or adverse effects had still not appeared. Topical corticosteroids are used as skin lighteners due to their potent bleaching action, and also their anti-inflammatory activity, which can reduce the risk of dermatitis when used along with other irritating skin lightening agents.[6,7] Skin lightening was the main reason for the use of these drugs. This may also explain the female predominance in this study. People of various age groups, socio-economic status, employment and marital status were also found to be using topical corticosteroids as self-medication for conditions where their use is actually not indicated.
The adverse effects are directly related to the potency of topical corticosteroids and have become more prevalent with the introduction of high potency topical corticosteroids. These include effects on the epidermis and the dermis in addition to those resulting from their systemic absorption.[7,8,9,10,11,12]
With the increasing use of topical corticosteroids, a number of adverse effects related to its misuse such as perioral dermatitis, tinea incognito, impetigo incognito and infantile gluteal granuloma have been detected[13,14,15] apart from other complications such as cellulitis, bacterial and fungal infections, acne, skin atrophy and pigmentation disorders. Other less commonly reported problems include delaying the diagnosis of leprosy[16] and erythrodermic psoriasis.[17] Recently a new term “topical steroid-dependent face” has been coined by Saraswat et al.[5] for the condition where, after prolonged use of topical corticosteroid on the face, there is severe rebound erythema, burning and scaling on any attempted cessation of the application.
Unfortunately, we found that most of the topical corticosteroids used were classed as potent or very potent. In spite of the fact that these drugs can cause such serious adverse effects, they are sold without medical prescription or control and there is little awareness about the adverse effects among the general public.
In this study, the main responsibility for the misuse of topical corticosteroids could be attributed to pharmacists, paramedical personnel, the patient, friends or family. Responsibility could also attributed be to general physicians and even some dermatologists to the extent that they did not emphasize the adverse effects and proper dosing of topical corticosteroids to the patients. This may also bring into focus the insufficient knowledge among medical/paramedical personnel about the proper use of topical corticosteroids. It may reflect the shortcomings of the continuing medical education program with regard to this problem.
There were few a shortcomings in this study; first, the diagnoses were mainly clinical and not confirmed by any further investigation. However the features that were observed were typical rather than atypical, making the diagnosis easier. Therefore confirmation by investigations was not felt necessary. Second, it is difficult for patients using topical corticosteroids over a long time to recollect the exact duration of their use. Third, it was difficult for many patients to understand what corticosteroid was until they were shown samples of these drugs. Moreover, flooding of the market with innumerable brands containing corticosteroids makes it more difficult to show a sample of each and every brand for the patient to recognize. This could have led to under-estimation of the frequency of the practice in our evaluation. Despite all these limitations, this study provides data confirming the extensive and uncontrolled use of topical corticosteroids in the study setting.
CONCLUSION
The misuse of topical corticosteroids has a huge impact on dermatological practice as it is responsible for a significant proportion of visits to dermatology clinics. It is a hydra-headed problem that needs multi-dimensional interventions, involving educational, legal and managerial approaches to overcome it. Education of the general public through media programs and introduction of continuing medical education programs for medical, paramedical personnel and pharmacists are probably the most important steps to be taken to create awareness about the hazards of misuse of topical corticosteroids. Secondly, legal approaches should include the enforcement of the existing legislation that potent topical corticosteroids cannot be sold over-the-counter and without the prescription of a qualified doctor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Sulzberger MB, Witten VH. The effect of topically applied compound F in selected dermatoses. J Invest Dermatol. 1952;19:101–2. doi: 10.1038/jid.1952.72. [DOI] [PubMed] [Google Scholar]
- 2.Hughes J, Rustin M. Corticosteroids. Clin Dermatol. 1997;15:715–21. doi: 10.1016/s0738-081x(97)00020-5. [DOI] [PubMed] [Google Scholar]
- 3.Valencia IC, Kerdel FA. Topical glucocorticoids. In: Fitzpatrick T, editor. Dermatology in General Medicine. 5th ed. New York: McGraw-Hill; 1999. pp. 2713–7. [Google Scholar]
- 4.Rathi S. Abuse of topical steroid as cosmetic cream: A social background of steroid dermatitis. Indian J Dermatol. 2006;51:154–5. [Google Scholar]
- 5.Saraswat A, Lahiri K, Chatterjee M, Barua S, Coondoo A, Mittal A, et al. Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol. 2011;77:160–6. doi: 10.4103/0378-6323.77455. [DOI] [PubMed] [Google Scholar]
- 6.Mahé A, Blanc L, Halna JM, Kéita S, Sanogo T, Bobin P. An epidemiologic survey on the cosmetic use of bleaching agents by the women of Bamako (Mali) Ann Dermatol Venereol. 1993;120:870–3. [PubMed] [Google Scholar]
- 7.Arnold J, Anthonioz P, Marchand JP. Depigmenting action of corticosteroids. Experimental study on guinea pigs. Dermatologica. 1975;151:274–80. [PubMed] [Google Scholar]
- 8.Lagos BR, Maibach HI. Frequency of application of topical corticosteroids: An overview. Br J Dermatol. 1998;139:763–6. doi: 10.1046/j.1365-2133.1998.02498.x. [DOI] [PubMed] [Google Scholar]
- 9.Brodkin RH, Janniger CK. The artful use of topical steroids. Cutis. 1998;61:125–6. [PubMed] [Google Scholar]
- 10.Keane FM, Munn SE, Taylor NF, du Vivier AW. Unregulated use of clobetasol propionate. Br J Dermatol. 2001;144:1095–6. doi: 10.1046/j.1365-2133.2001.04213.x. [DOI] [PubMed] [Google Scholar]
- 11.Mahé A, Ly F, Aymard G, Dangou JM. Skin diseases associated with the cosmetic of bleaching products in women from Dakar, Senegal. Br J Dermatol. 2003;148:493–500. doi: 10.1046/j.1365-2133.2003.05161.x. [DOI] [PubMed] [Google Scholar]
- 12.Del Giudice P, Yves P. The widespread use of skin lightening creams in Senegal: A persistent public health problem in West Africa. Int J Dermatol. 2002;41:69–72. doi: 10.1046/j.1365-4362.2002.01335.x. [DOI] [PubMed] [Google Scholar]
- 13.Raynaud E, Cellier C, Perret JL. Depigmentation for cosmetic purposes: Prevalence and side-effects in a female population in Senegal. Ann Dermatol Venereol. 2001;128:720–4. [PubMed] [Google Scholar]
- 14.Ive FA, Marks R. Tinea incognito. Br Med J. 1968;3:149–52. doi: 10.1136/bmj.3.5611.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonifazi E, Garofalo L, Lospalluti M, Scardigno A, Coviello C, Meneghini CL. Granuloma gluteale infantum with atrophic scars: Clinical and histological observations in eleven cases. Clin Exp Dermatol. 1981;6:23–9. doi: 10.1111/j.1365-2230.1981.tb02264.x. [DOI] [PubMed] [Google Scholar]
- 16.Mahé A, Ly F, Badiane C, Baldé Y, Dangou JM. Irrational use of skin-bleaching products can delay the diagnosis of leprosy. Int J Lepr Other Mycobact Dis. 2002;70:119–21. [PubMed] [Google Scholar]
- 17.Ohnishi T, Suzuki T, Watanabe S, Takahashi H. Erythrodermic psoriasis associated with hyperuricemia and Iatrogenic Cushing's syndrome due to topical corticosteroid therapy. Int J Dermatol. 1996;35:379–80. doi: 10.1111/j.1365-4362.1996.tb03647.x. [DOI] [PubMed] [Google Scholar]


