Abstract
Angiokeratomas are a group of vascular ectasias that involve the papillary dermis and may produce papillomatosis, acanthosis and hyperkeratosis of the epidermis. Angiokeratoma circumscriptum is the least common variant among many types. Angiokeratoma circumscriptum neviforme is a still rarer variety of angiokeratoma, which is classically seen at birth. We report here a case of congenital, linear, unilateral, verrucous plaques on the leg of a young girl, diagnosed as angiokeratoma circumscriptum neviforme (ACN).
Keywords: Angiokeratoma circumscriptum neviforme, linear, verrucous plaques
INTRODUCTION
Angiokeratomas are relatively rare vascular lesions, the precise mechanism for their development yet to be known. Variants of angiokeratomas include solitary and multiple angiokeratoma, angiokeratoma circumscriptum, angiokeratoma of Fordyce, angiokeratoma of Mibelli, and angiokeratoma corporis diffusum.[1] Angiokeratoma circumscriptum is the rarest variant. Clinically, it is manifested as dark red to blue-black nodules or plaques presenting unilaterally over the lower extremities. Other sites of presentation include thighs, buttocks, and so on. The lesions often become keratotic and show no tendency for spontaneous remission, posing a concern for cosmesis to the patient.[2]
CASE REPORT
A 16-year-old girl was referred to us for a congenital lesion on her left lower extremity in a linear fashion. To start with, the lesions were stable but these had gradually started to increase in size and number since last 6 years. She gave a history of occasional pain and several episodes of bleeding from the lesions even upon trivial trauma. There were no other systemic symptoms or history of external bleeding from any other site. Family history was noncontributory.
Dermatological examination revealed multiple discrete as well as confluent plaques of various sizes arranged in a linear configuration over the extensor aspect of the lower part of left leg [Figures 1a and b]. The lesions were well-circumscribed, firm to hard, noncompressible, and nontender. The surface of the lesions was verrucous, few of which bled to touch. Lesional palpation did not reveal any pulsation and no bruit was audible on auscultation. Regional lymphadenopathy was absent. There was no discrepancy in the length and circumference of both the legs. Systemic examination was within normal limits. Routine laboratory investigations including complete hemogram and biochemistry panel were noncontributory. An X-ray of the legs did not show any bony abnormalities. Incisional biopsies were taken from multiple sites. Histopathological examination showed features of compact hyperkeratosis, acanthosis, and slight papillomatosis. Papillary dermis showed numerous dilated capillaries containing red blood cells [Figures 2a and b]. No vascular ectasia was appreciable in the reticular dermis or in the subcutaneous tissue.
Figure 1.

Linear, verrucous, well-circumscribed plaques on the left lower leg (a) and close-up view of one of the lesions over the leg showing verrucous and hyperkeratotic surface (b)
Figure 2.
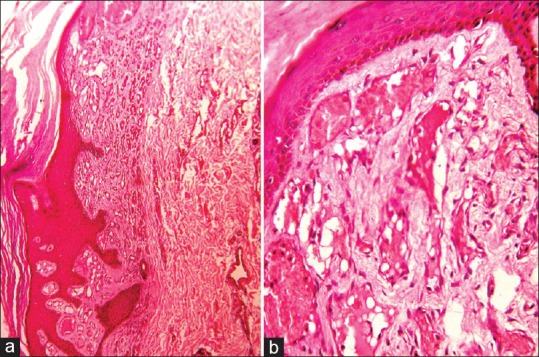
Photomicrograph showing compact hyperkeratosis, acanthosis and slight papillomatosis (H and E, ×40) (a) and dilated vascular spaces containing erythrocytes in the papillary dermis (H and E, ×100) (b)
On the basis of clinical and histopathological features, a diagnosis of angiokeratoma circumscriptum neviforme (ACN) was done. The patient has been referred to the department of plastic surgery for consideration of surgical therapy (diathermy and curettage) and she is also being evaluated for the role of carbon dioxide laser therapy for ablation of the lesions.
DISCUSSION
The lesions of ACN are typically present since birth as unilateral, hyperkeratotic plaques comprising of confluent keratotic papules. Nevoid malformation of the underlying vascular network is thought to be the main cause of ACN.[3] In some cases, the initial presentation may be of multiple red-colored macules, simulating nevus flammeus. Within a few years, they evolve into plaques, the surface being hyperkeratotic and verrucous.[4] Women are affected more commonly than men, in a ratio of approximately 3:1. The sites of predilection on the skin are the gluteal regions and the thighs. Sardana et al.[3] reported an unusual site of occurrence of ACN over the neck. Angiokeratoma circumscriptum has been reported to coexist with angiokeratoma of Fordyce[5] (found on the scrotum) and caviar spots (angiokeratomas of the tongue).[6]
As Imperial and Helwig discussed in 1967,[7] angiokeratomas are not true angiomas but rather telangiectasias of preexisting vessels. The mechanism for development of angiokeratoma circumscriptum is unknown. Several causal factors, such as congenital development, pregnancy, trauma, subcutaneous hematomas, and tissue asphyxia, have all been proposed.
There are reports of coexistence of ACN with other vascular malformations, including angiokeratomas of Fordyce, Cobb syndrome, Klippel-Trenaunay syndrome, nevus flammeus, cavernous hemangioma, and traumatic arteriovenous fistula.[4] A thorough systemic evaluation was done and we did not find any such abnormalities in our case.
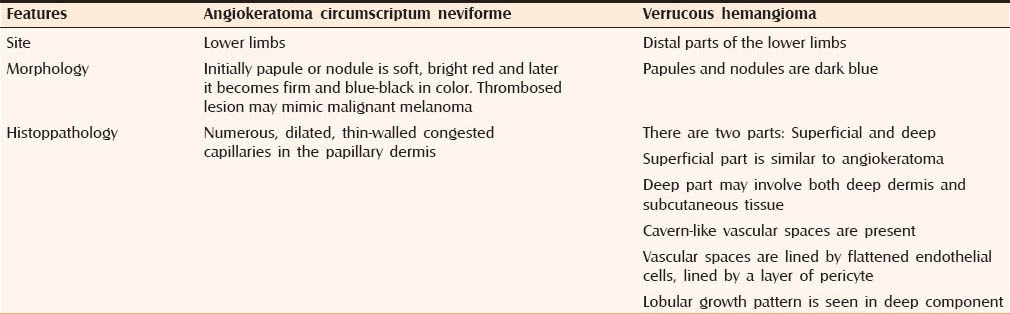
Our main clinical differential diagnosis was verrucous hemangioma which is a congenital, localized, vascular malformation, histopathologically manifesting as dilated capillaries and large endothelial-lined, blood-filled spaces extending well into the reticular dermis and subcutaneous tissue with an overlying hyperkeratosis. The vessels are packed with erythrocytes; this finding is suggestive of vessel thrombosis. A normal-appearing vascular endothelium is found. The dermal connective tissue is usually not involved, but it may contain a few siderophages.[8] But, angiokeratoma, consistent with our case, does not demonstrate the deep angiomatous component of verrucous hemangioma. The salient points of difference between ACN and verrucous hemangioma is shown in Table 1.
Table 1.
Salient points of difference between angiokeratoma circumscriptum neviforme and verrucous hemangioma
Small lesions may be managed by diathermy, curettage and electrocautery, cryosurgery, and surgery. Larger lesions require laser ablation (carbon dioxide or argon laser). One treatment approach is to initiate treatment with an erbium or carbon dioxide laser to remove the hyperkeratotic-acanthotic epidermis, followed by the use of a laser that targets hemoglobin, such as the flash pump dye, Potassium titanyl phosphate, or 880-nm diode laser. In a report by del Pozo and Fonseca,[4] continuous-wave carbon dioxide laser vaporization was found to be a safe and effective treatment for ACN and a successful cosmetic aspect of treated areas was obtained, with minimal pigmentary or textural changes. The Potassium titanyl phosphate laser destroys vascular targets and is relatively specific for cutaneous blood vessels; therefore, it is ideal for the treatment of cutaneous vascular lesions. The rarity of report of this entity in the world literature prompted the present report.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mittal R, Aggarwal A, Srivastava G. Angiokeratoma circumscriptum: A case report and review of the literature. Int J Dermatol. 2005;44:1031–4. doi: 10.1111/j.1365-4632.2005.02252.x. [DOI] [PubMed] [Google Scholar]
- 2.Ghosh SK, Bandyopadhyay D, Ghoshal L, Haldar S. Angiokeratoma circumscriptum naeviforme: A case report of a rare disease. Dermatol Online J. 2011;17:11. [PubMed] [Google Scholar]
- 3.Sardana K, Koranne RV, Sharma RC, Mahajan S. Angiokeratoma circumscriptum naeviforme: Rare presentation on the neck. Australas J Dermatol. 2001;42:294–5. doi: 10.1046/j.1440-0960.2001.00540.x. [DOI] [PubMed] [Google Scholar]
- 4.del Pozo J, Fonseca E. Angiokeratoma circumscriptum naeviforme: Successful treatment with carbon-dioxide laser vaporization. Dermatol Surg. 2005;31:232–6. doi: 10.1111/j.1524-4725.2005.31048. [DOI] [PubMed] [Google Scholar]
- 5.Feramisco JD, Fournier JB, Zedek DC, Venna SS. Eruptive angiokeratomas on the glans penis. Dermatol Online J. 2009;15:14. [PubMed] [Google Scholar]
- 6.Eskiizmir G, Gencoglan G, Temiz P, Ermertcan AT. Angiokeratoma circumscriptum of the tongue. Cutan Ocul Toxicol. 2011;30:231–3. doi: 10.3109/15569527.2010.544278. [DOI] [PubMed] [Google Scholar]
- 7.Imperial R, Helwig EB. Verrucous hemangioma. A clinicopathologic study of 21 cases. Arch Dermatol. 1967;96:247–53. doi: 10.1001/archderm.96.3.247. [DOI] [PubMed] [Google Scholar]
- 8.Calonje E. Vascular Tumors: Tumors and tumor-like conditions of blood vessels and lymphatics. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's Histopathology of Skin. 10th ed. Philadelphia: Lippincott Williams and Wilkins publishers; 2009. p. 1011. [Google Scholar]


