Sir,
A 30-year-old female patient presented with multiple, tiny, honeycomb-type pitted scars over the left cheek [Figure 1], associated with extensive nevus comedonicus involving the left half of the body. Several lesions were seen with multiple, pinhead-sized comedones overlying the hyperpigmented patches, distributed along the lines of Blaschko [Figures 2 and 3] over the left side of the back [Figure 2a and b], chest [Figure 3a], arm, forearm, buttock, thigh, and leg [Figure 3b], since 10 - 15 years. The right half of the body, including the palms and soles were spared. She also had multiple acneiform nodules and tiny sebaceous cysts over the back, associated with the nevus comedonicus, at the time of presentation [Figure 2b]. A linear scar was observed over the back following a surgery on a large sebaceous cyst [Figure 2a]. An examination did not reveal any underlying bony or soft tissue malformation. She had no history of seizures or a history suggestive of ophthalmic abnormalities. A skin biopsy was done on the back, which revealed mild hyperkeratosis, with deep invagination of the epidermis filled with keratin [Figure 4a and b]. Our patient was started on capsule Doxycycline 100 mg, twice a day, for a month, with topical retinoic acid 0.25% gel at night, to which she reported mild improvement.
Figure 1.

Honeycomb-like pitted scars over the face
Figure 2.

(a) Generalized nevus comedonicus along the Blaschko's lines over the back. (b) A close-up view showing acne and Nodular lesions
Figure 3.

Nevus along the Blaschko's lines, (a) over the chest, (b) over left leg
Figure 4.
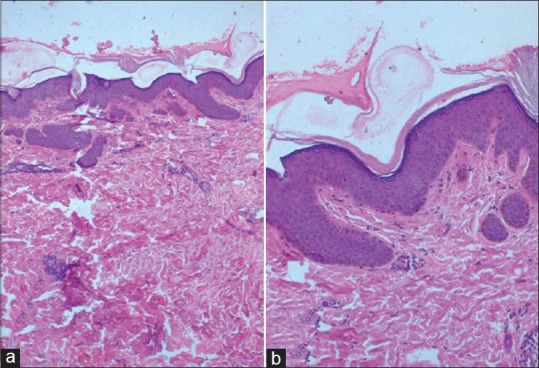
(H and E staining) (a) ×10 multiple keratin-filled pits in the epidermis with mild hyperkeratosis, (b) ×40 scant atrophic sebaceous glands in the dermis
The clinical features, etiopathology, histopathology, and treatment options of nevus comedonicus are briefly reviewed in the light of the literature.
Nevus comedonicus was first described by Kofmann in 1895. It is a rare nevus and may present as a single or multiple lesions. It may be segmental, interrupted, unilateral, bilateral, present in a dermatomal distribution or along the Lines of Blaschko[1] (as in our case). The lesions first appear at birth or during childhood. The hallmark finding in this nevus is the presence of comedo-like dilated pores with keratinous plugs. The nevus follows a non-inflammatory or inflammatory course in the form of recurrent suppuration and pain, in which case it is called nevus acneiformis unilateralis. Histologically the characteristic finding is that of keratin-filled epidermal invaginations associated with atrophic sebaceous glands or follicles. Epidermolytic hyperkeratosis may also be seen.[2] Nevus comedonicus may originate either through mosaicism or through influences on the juxta-epidermal mesenchymal tissue during embryogenesis.[3] Genetic studies have revealed fibroblast growth factor receptor 2 (FGFR2) mutation in comedonal nevus, but not in the adjacent normal skin, which may be responsible for the recurrent acne over this nevus.[4] There is increased expression of the Proliferating Cell Nuclear Antigen (PCNA), Intercellular Adhesion Molecule 1 (ICAM-1), human leucocyte antigen-DR (HLA-DR), and CD 68, representing a focal clonal defect in the growth regulation of the keratinocytes of the infundibula.[5] Nevus comedonicus also forms a part of the epidermal nevus syndrome, as mosaicism may be present in the mesodermal layer derivates. Complex syndromes with extra-cutaneous manifestations may be seen. Central nervous system (CNS) involvement includes epilepsy, electroencephalogram abnormalities, and transverse myelitis. Skeletal system abnormalities include scoliosis, hemivertebrae, spina bifida occulta, absence of fingers, syndactyly, and supernumerary digits. Cutaneous associations include ichthyosis, trichilemmal cysts, leukoderma, white hair, Sturge-Weber syndrome, and hemangiomas. Ocular abnormalities include congenital cataracts, either unilateral or bilateral. Verrucous changes and squamous and basal cell carcinomas have been known to develop over these nevi.[6] Our patient did not have any systemic abnormalities in spite of the extensive involvement of one half of her body.
Nevus comedonicus is usually asymptomatic. Inflammation may be controlled with topical retinoid (tazarotene), tacrolimus ointment, calcipotriene cream, and intralesional steroids. Surgical interventions like extraction, excision, dermabrasion or laser resurfacing may give good cosmetic results.
REFERENCES
- 1.Molho-Pessach V, Schaffer JV. Blaschko lines and other patterns of cutaneous mosaicism. Clin Dermatol. 2011;29:205–25. doi: 10.1016/j.clindermatol.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 2.Schecter AK, Lester B, Pan TD, Robinson-Bostom L. Linear nevus comedonicus with epidermolytic hyperkeratosis. J Cutan Pathol. 2004;31:502–5. doi: 10.1111/j.0303-6987.2004.00206.x. [DOI] [PubMed] [Google Scholar]
- 3.Köse O, Calişkan E, Kurumlu Z. Three different epidermal naevi with no organ involvement: Sebaceous naevus, naevus comedonicus and Becker's naevus. Acta Derm Venereol. 2008;88:67–9. doi: 10.2340/00015555-0321. [DOI] [PubMed] [Google Scholar]
- 4.Callen J, Horn T, Mancini AJ, Salasche SJ, Schaffrr JV, Schwarz T. Benign epidermal tumours and proliferations. Bolognia Dermatology. (2nd ed) 2008;2:109. [Google Scholar]
- 5.Bongiorno MR, Pistone G, Aricò M. Naevus comedonicus: immunohistochemical features in two cases. Acta Derm Venereol. 2003;83:300–1. doi: 10.1080/00015550310016625. [DOI] [PubMed] [Google Scholar]
- 6.Walling HW, Swick BL. Squamous cell carcinoma arising in nevus comedonicus. Dermatol Surg. 2009;35:144–6. doi: 10.1111/j.1524-4725.2008.34396.x. [DOI] [PubMed] [Google Scholar]


