A 70-year-old male having a sedentary lifestyle presented with history of a gradually increasing, single plaque over his back [Figure 1] for 20 years. There was no history of pain, ulceration, mucosal lesions, or any other skin lesions. Differential diagnoses of Bowen's Disease (BD), lupus vulgaris, and basal cell carcinoma were considered and the patient was investigated. Investigations revealed a normal hematological work up, a negative Mantoux test and sputum for acid-fast bacilli, a normal chest radiograph and a skin biopsy consistent with BD [Figures 2 and 3]. The patient was started on imiquimod 5% cream for 5 days in a week for 12 weeks which resulted in complete resolution of the lesion clinically [Figure 4] with no adverse effects. Biopsy done six weeks after treatment revealed a normal epidermis [Figure 5]. The patient has been on regular 3-monthly follow up for the past eighteen months, with no recurrence of the lesion.
Figure 1.

Plaque on the back showing erythema in places and hyperpigmentation in others, 6 × 7 cm, irregular, with rough, scaly surface with few fissures and well-demarcated borders in most areas, while at places its ill-defined, breaking down to form another small plaque
Figure 2.
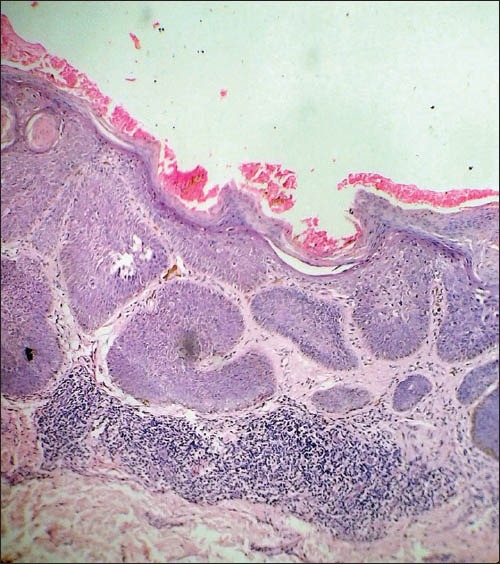
Skin biopsy showing epidermal dysplasia with an intact basement membrane, and atypical keratinocytes having a windblown appearance. Hyperkeratosis, parakeratosis, and acanthosis is present with the dermis showing lymphocytic infiltrate consistent with the findings of BD. (H and E, ×100)
Figure 3.
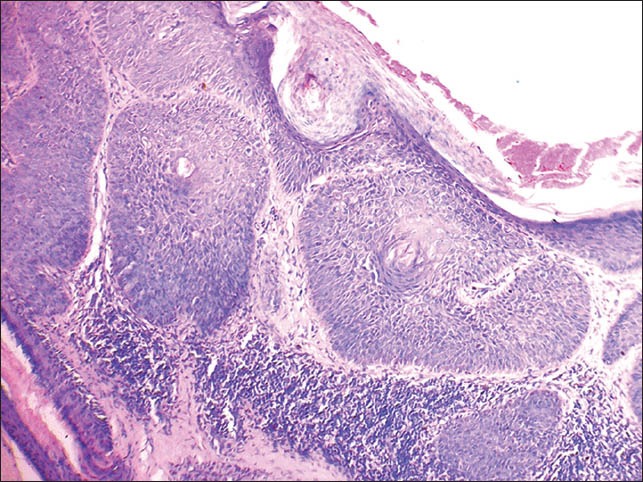
Section of skin showing atypical keratinocytes having a windblown appearance with lymphocytic infiltrate in the dermis suggestive of BD. (H and E, ×400)
Figure 4.

Post treatment plaque shows complete flattening with postinflammatory hyperpigmentation without any induration or scaling. Note, that the lower end shows some amount of fibrosis which represents healed sites of biopsies taken pre- and post treatment
Figure 5.
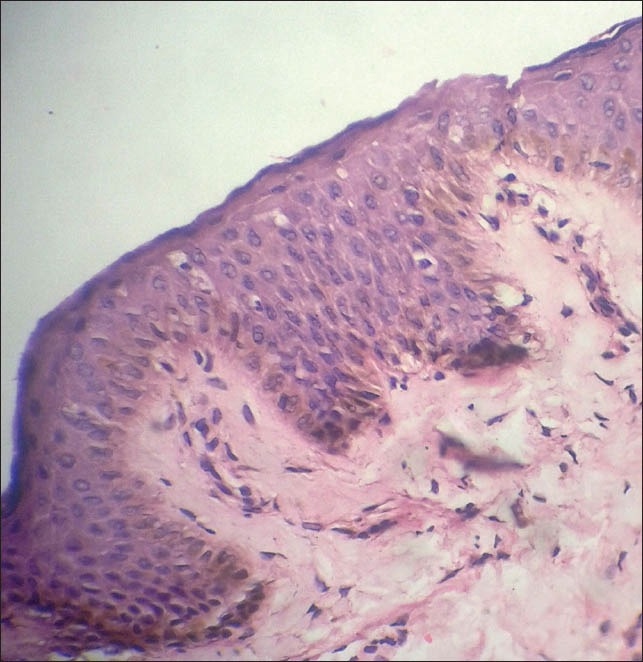
Posttreatment histopathology of skin showing resolution of epidermal changes with marked decrease in infiltrate in the dermis. (H and E, ×400)
BD, a form of squamous cell carcinoma in situ, was described in 1912 by John T. Bowen. The exact incidence in Indian population is not reported. In 1991, a study from Minnesota reported the annual average rate of BD as 14.9 cases per 100,000 whites.[1] In 1994, a study from Hawaii reported a rate 10 times that, 142 per 100,000 persons.[2]
BD typically presents as an asymptomatic, discrete, slowly enlarging erythematous scaly patch or plaque with well-demarcated irregular border. Hyperkeratotic, crusted, fissured, verrucous, or ulcerated surface changes may be seen. Psoriasiform, atrophic, verrucous,[3] hypertrophic, pigmented,[4] and irregular variants have been reported.
The classic clinical history is a presentation of a chronic, slowly progressive, scaly plaque that is unresponsive to topical steroids. Ulceration is usually a sign of development of invasive carcinoma and may be delayed for many years after the appearance of intraepidermal changes.
The prognosis of BD is favorable. The majority of studies place the risk of progression to invasive squamous cell carcinoma at 5%.[5] Of those that become invasive, one-third may metastasize.[6]
Multiple therapeutic options are available for treatment of BD, which include medical and surgical.[7] Medical treatment includes topical chemotherapy with 5-fluorouracil and imiquimod 5% cream,[8] radiation therapy with X-rays or Grenz rays, and photodynamic therapy. Surgical options include simple excision with a minimum 4 mm margin around well-defined tumors of less than 2 cm in diameter and wide excision with at least 6 mm margin for larger or less-differentiated tumors or tumors in high-risk locations (e.g. scalp, ears, eyelids, nose, and lips).[9] Other surgical modalities include Mohs micrographic surgery, curettage and electrodessication, cryotherapy and laser ablation.
Because most treatments have a recurrence risk, follow-up at 6 to 12 months is recommended to evaluate for any recurrence. As BD mimics many dermatoses, a high degree of clinical suspicion is required to make a diagnosis in those dermatoses which fail to respond to conventional topical and systemic therapies.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chute CG, Chuang TY, Bergstralh EJ, Su WP. The subsequent risk of internal cancer with Bowen's disease. A population-based study. JAMA. 1991;266:816–9. [PubMed] [Google Scholar]
- 2.Reizner GT, Chuang TY, Elpern DJ, Stone JL, Farmer ER. Bowen's disease (sqamous cell carcinoma in situ) in Kauai, Hawaii: A population-based incidence report. J Am Acad Dermatol. 1994;31:596–600. doi: 10.1016/s0190-9622(94)70222-5. [DOI] [PubMed] [Google Scholar]
- 3.Grekin RC, Swanson NA. Verrucous Bowen's disease of the plantar foot. J Dermatol Surg Oncol. 1984;10:734–6. doi: 10.1111/j.1524-4725.1984.tb01282.x. [DOI] [PubMed] [Google Scholar]
- 4.Ragi G, Turner MS, Klein LE, Stoll HL., Jr Pigmented Bowen's disease and review of 420 Bowen's disease lesions. J Dermatol Surg Oncol. 1988;14:765–9. doi: 10.1111/j.1524-4725.1988.tb01161.x. [DOI] [PubMed] [Google Scholar]
- 5.Kao GF. Carcinoma arising in Bowen's disease. Arch Dermatol. 1986;122:1124–6. [PubMed] [Google Scholar]
- 6.Cox NH, Eedy DJ, Morton CA Therapy Guidelines and Audit Subcommittee, British Association of Dermatologists. Guidelines for management of Bowen's disease: 2006 update. Br J Dermatol. 2007;156:11–21. doi: 10.1111/j.1365-2133.2006.07610.x. [DOI] [PubMed] [Google Scholar]
- 7.van Egmond S, Hoedemaker C, Sinclair R. Successful treatment of perianal Bowen's disease with imiquimod. Int J Dermatol. 2007;46:318–9. doi: 10.1111/j.1365-4632.2007.03200.x. [DOI] [PubMed] [Google Scholar]
- 8.Moreno G, Chia AL, Lim A, Shumack S. Therapeutic options for Bowen's disease. Australas J Dermatol. 2007;48:1–8. doi: 10.1111/j.1440-0960.2007.00317.x. [DOI] [PubMed] [Google Scholar]
- 9.Brodland DG, Zitelli JA. Surgical margins for excision of primary cutaneous squamous cell carcinoma. J Am Acad Dermatol. 1992;27:241–8. doi: 10.1016/0190-9622(92)70178-i. [DOI] [PubMed] [Google Scholar]


