CT imaging with model-based iterative reconstruction allows for significant patient radiation dose reduction while preserving diagnostic image quality.
Abstract
Purpose
To retrospectively compare image quality and radiation dose between a reduced-dose computed tomographic (CT) protocol that uses model-based iterative reconstruction (MBIR) and a standard-dose CT protocol that uses 30% adaptive statistical iterative reconstruction (ASIR) with filtered back projection.
Materials and Methods
Institutional review board approval was obtained. Clinical CT images of the chest, abdomen, and pelvis obtained with a reduced-dose protocol were identified. Images were reconstructed with two algorithms: MBIR and 100% ASIR. All subjects had undergone standard-dose CT within the prior year, and the images were reconstructed with 30% ASIR. Reduced- and standard-dose images were evaluated objectively and subjectively. Reduced-dose images were evaluated for lesion detectability. Spatial resolution was assessed in a phantom. Radiation dose was estimated by using volumetric CT dose index (CTDIvol) and calculated size-specific dose estimates (SSDE). A combination of descriptive statistics, analysis of variance, and t tests was used for statistical analysis.
Results
In the 25 patients who underwent the reduced-dose protocol, mean decrease in CTDIvol was 46% (range, 19%–65%) and mean decrease in SSDE was 44% (range, 19%–64%). Reduced-dose MBIR images had less noise (P > .004). Spatial resolution was superior for reduced-dose MBIR images. Reduced-dose MBIR images were equivalent to standard-dose images for lungs and soft tissues (P > .05) but were inferior for bones (P = .004). Reduced-dose 100% ASIR images were inferior for soft tissues (P < .002), lungs (P < .001), and bones (P < .001). By using the same reduced-dose acquisition, lesion detectability was better (38% [32 of 84 rated lesions]) or the same (62% [52 of 84 rated lesions]) with MBIR as compared with 100% ASIR.
Conclusion
CT performed with a reduced-dose protocol and MBIR is feasible in the pediatric population, and it maintains diagnostic quality.
© RSNA, 2013
Introduction
Radiation exposure from computed tomography (CT) is of increasing concern to both the medical community and the general public (1–3). This concern is amplified in pediatric populations, as children are more sensitive to the effects of ionizing radiation (4–6). As such, substantial emphasis has been placed on strategies to reduce CT radiation doses while maintaining image quality (7). Most CT dose reduction strategies rely on reducing radiation output from the scanner, with the inherent trade-off being greater image noise and diminished image quality (8,9). Because of this, new iterative CT image reconstruction techniques have been developed in an attempt to decrease image noise when scanning at lower CT radiation doses (10–13).
Model-based iterative reconstruction (MBIR) is a new iterative CT image reconstruction technique. MBIR differs from other iterative reconstruction techniques in that MBIR takes into account the optics of the scanner, including focal spot and detector size. In addition, MBIR can be applied in only one strength, whereas previous iterative techniques could be applied in gradations (eg, 30% adaptive statistical iterative reconstruction [ASIR] combined with filtered back projection [FBP]). To date, only a few studies in which researchers evaluated the effect of MBIR on patient radiation dose and image quality have been published (14–18). Such studies, mostly in adults, have shown that MBIR leads to substantial dose reductions but maintains diagnostic image quality and reduces image noise. The purpose of this study was to objectively and subjectively compare image quality and radiation dose between a reduced-dose CT protocol with MBIR and ASIR and a standard-dose CT protocol with 30% ASIR.
Materials and Methods
Institutional review board approval was obtained for this retrospective, Health Insurance Portability and Accountability Act–compliant study. The requirement for informed consent was waived.
Consecutive patients with cancer (<21 years of age and examined at C.S. Mott Children’s Hospital) who were undergoing routine reduced-dose clinical outpatient CT of the chest, abdomen, and pelvis for follow-up of a known malignancy between May 2012 and July 2012 were identified. All examinations were performed with a 64-section CT scanner (Discovery HD750; GE Healthcare, Waukesha, Wis) with both MBIR (Veo; GE Healthcare) and ASIR (ASiR; GE Healthcare) image reconstruction. All subjects had undergone comparison standard-dose CT of the chest, abdomen, and pelvis performed on the same CT scanner with 30% ASIR reconstruction within the past 12 months. The only exclusion criteria were a lack of prior standard-dose CT within the past 12 months and inpatient status at the time of the examination (because of the time involved in image reconstruction, MBIR reconstructions were not feasible in inpatients and those in the emergency department). None of the consecutive 25 patients had to be excluded for either criterion.
CT Technique
MBIR examinations were performed by using a reduced-dose protocol. Tube current was established by using automatic tube current modulation with a fixed noise index of 47.7. This specific noise index was chosen because it was expected to provide an approximately 50% dose reduction compared with standard-dose routine examinations that use a noise index of 33.6. Tube potential was determined by using a weight-based algorithm (80, 100, or 120 kVp) and was confirmed to be the same between both examinations in all patients. All other CT parameters were identical (Table 1). All examinations were performed by using both oral and intravenous contrast materials that were administered by using routine clinical weight-based algorithms.
Table 1.
Clinical Standard-Dose and Reduced-Dose CT Parameters
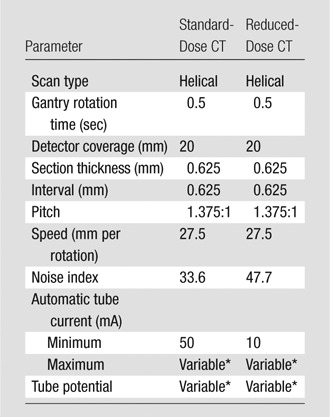
This parameter was based on patient weight.
For the reduced-dose MBIR examinations, CT images were also reconstructed by using FBP and 100% ASIR. In addition to 0.625-mm section thickness source images, MBIR, FBP, and 100% ASIR images were reconstructed in the axial plane by using a 5.0-mm section thickness at a 2.5-mm section interval. ASIR and FBP reconstructions were created by using the standard reconstruction kernel, and these images were used for all of the analyses (ie, soft-tissue, lung, and bone comparisons). MBIR images can be reconstructed only with the equivalent of a standard reconstruction kernel. Comparison standard-dose CT images were reconstructed in the axial plane by using 5.0-mm section thickness at 2.5-mm section intervals and the standard reconstruction kernel. Only the 5.0-mm reconstructed axial images were used for image analysis. Coronal and sagittal images were not reviewed.
Estimating Patient Radiation Dose
Volumetric CT dose index (CTDIvol) was recorded for all examinations and was based on the dose report card created by the CT scanner. The phantom size used for CTDIvol estimation was also documented to ensure that estimates of patient radiation exposure would be valid and to enable size-specific dose estimate (SSDE) calculation. SSDE was calculated for all examinations by using the method described in the American Association of Physicists in Medicine task group report 204, with the scout CT images used to measure the transverse and anteroposterior diameters of each patient (19). Transverse and anteroposterior diameters were summed to determine the conversion factor needed for SSDE determination (20).
Objective Determination of Image Quality
Image noise.—Image noise measurements were obtained with reduced-dose (both MBIR and 100% ASIR reconstructions) and comparison standard-dose 30% ASIR examinations. CT studies were loaded onto a workstation (Advantage, version 4.5; GE Healthcare), and image noise was established by determining the standard deviation (in Hounsfield units) within a region of interest. Noise measurements were performed by a single fellowship-trained and board-certified pediatric radiologist (E.A.S., 2 years of experience in pediatric radiology) at standardized locations.
One noise measurement was obtained in the abdominal aorta at the level of the origin of the superior mesenteric artery by using a region of interest that encompassed approximately two-thirds of the cross-sectional area of the aortic lumen (Fig 1). The same size region of interest was then used for the additional noise measurements in the liver and paraspinal musculature. Three noise measurements were obtained in the liver: they were obtained at the posterior segment of the right lobe, at the anterior segment of the right lobe, and in the middle of the left hepatic lobe. Two noise measurements were obtained in the paraspinal muscles at the level of the superior mesenteric artery; one measurement was obtained on each side of the midline. Average noise measurements in the liver and paraspinal muscles were determined for each structure.
Figure 1a:
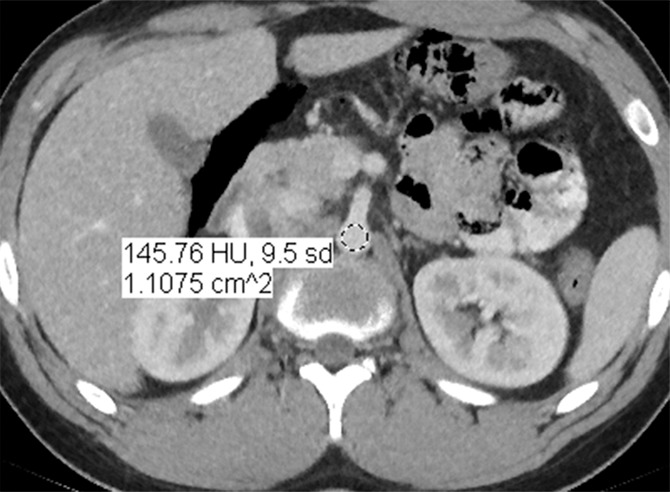
CT images in a 17-year-old boy with a history of Hodgkin disease. (a) Reduced-dose MBIR image, (b) reduced-dose 100% ASIR image, (c) reduced-dose FBP image, and (d) comparison standard-dose 30% ASIR image, all with a region of interest in the abdominal aorta for objective noise measurement. Image noise was recorded as the standard deviation of attenuation (in Hounsfield units) in a given region of interest. The reduced-dose MBIR image has significantly less noise when compared with other reduced-dose and standard-dose reconstructions.
Figure 1b:

CT images in a 17-year-old boy with a history of Hodgkin disease. (a) Reduced-dose MBIR image, (b) reduced-dose 100% ASIR image, (c) reduced-dose FBP image, and (d) comparison standard-dose 30% ASIR image, all with a region of interest in the abdominal aorta for objective noise measurement. Image noise was recorded as the standard deviation of attenuation (in Hounsfield units) in a given region of interest. The reduced-dose MBIR image has significantly less noise when compared with other reduced-dose and standard-dose reconstructions.
Figure 1c:
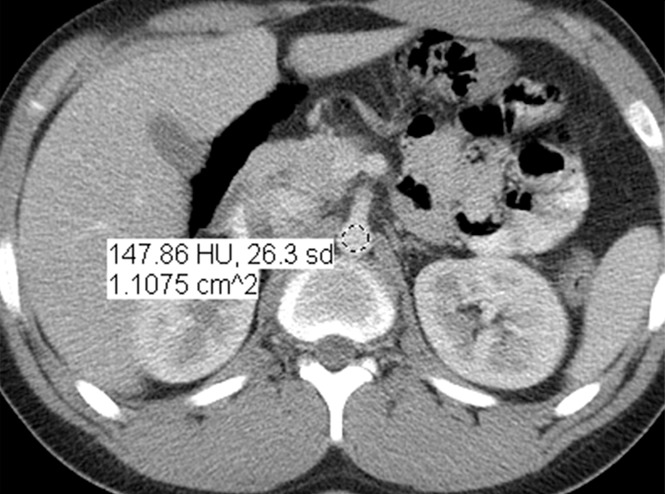
CT images in a 17-year-old boy with a history of Hodgkin disease. (a) Reduced-dose MBIR image, (b) reduced-dose 100% ASIR image, (c) reduced-dose FBP image, and (d) comparison standard-dose 30% ASIR image, all with a region of interest in the abdominal aorta for objective noise measurement. Image noise was recorded as the standard deviation of attenuation (in Hounsfield units) in a given region of interest. The reduced-dose MBIR image has significantly less noise when compared with other reduced-dose and standard-dose reconstructions.
Figure 1d:
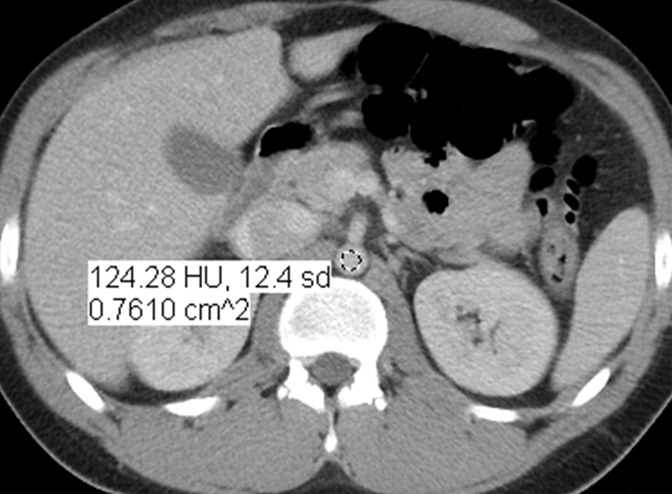
CT images in a 17-year-old boy with a history of Hodgkin disease. (a) Reduced-dose MBIR image, (b) reduced-dose 100% ASIR image, (c) reduced-dose FBP image, and (d) comparison standard-dose 30% ASIR image, all with a region of interest in the abdominal aorta for objective noise measurement. Image noise was recorded as the standard deviation of attenuation (in Hounsfield units) in a given region of interest. The reduced-dose MBIR image has significantly less noise when compared with other reduced-dose and standard-dose reconstructions.
Image spatial resolution.—The modulation transfer function (MTF) was measured to estimate CT image spatial resolution for reduced-dose images (both MBIR and 100% ASIR reconstructions) and comparison standard-dose 30% ASIR images by using a phantom (Catphan 600; Phantom Laboratory, Salem, NY) and imaging software (imageOwl Catphan QA; Phantom Laboratory). The MTF is the spatial frequency representation of the point spread function of the scanner. The CTP528 high-resolution module of the phantom was scanned. This module contains two 0.28-mm-diameter tungsten carbide beads in a soft tissue–like background. The imaging software sums the pixel values of the columns along the x-axis of the point spread function (image matrix of the bead) to obtain the y-axis line spread function, and it sums the pixel values of the columns along the y-axis to obtain the x-axis line spread function. An average line spread function is derived from the x-axis and y-axis line spread functions. The MTF is calculated by taking the fast-Fourier transform of the average line spread function.
CT scanning parameters were identical to those used for the clinical examinations. As with the clinical examinations, images for the phantom study were reconstructed with the standard reconstruction kernel. The MTF measurements were acquired at 80, 100, and 120 kVp. By plotting MTF versus object spatial frequency (measured in phantom line pairs per centimeter), one can determine the limiting resolution, that is, the spatial frequency at which the MTF is 0.1.
Subjective Determination of Image Quality
Subjective determination of image quality, lesion detection, and normal structure visualization was performed by two board-certified fellowship-trained pediatric radiologists (J.R.D., P.J.S.; 3 and 20 years of experience, respectively). All pertinent images were reviewed by using the same workstation as before after they were displayed by a third radiologist (E.A.S.). Only axial images were reviewed. Image overlays were removed, but readers could not be truly blinded to the type of image reconstruction being reviewed, as the different reconstructions all have different appearances that are inherent and unique.
Overall image quality.—Reduced-dose images (both MBIR and 100% ASIR images) were compared with standard-dose 30% ASIR images to assess subjective overall image quality with respect to the soft tissues, lungs, and bones. Appropriate window-level adjustments were made to optimize visualization of different tissues. Overall image quality was rated for each reduced-dose reconstruction (MBIR and 100% ASIR), as follows: a score of 1 indicated superior image quality compared with the 30% ASIR examination; a score of 2, equivalent image quality compared with the 30% ASIR examination; a score of 3, inferior image quality compared with the 30% ASIR examination but still diagnostic; and a score of 4, nondiagnostic.
Lesion visualization.—Abnormalities described in the finalized reports from reduced-dose examinations were identified. A maximum of four lesions per patient were identified based on order of appearance in the impression section of the imaging report. Patients who did not have focal abnormalities were excluded from this portion of the study (n = 7). The same two readers (J.R.D., P.J.S.) were shown two images from the reduced-dose examination simultaneously; these images were obtained at the same level, and both images contained the lesion. One image was reconstructed by using MBIR, and the other was reconstructed by using 100% ASIR. Reviewers were asked to separately rate visualization of each lesion on the MBIR image compared with visualization of each lesion on the 100% ASIR image by using a four-point scale: a score of 1 indicated better visualization on the MBIR image; a score of 2, equivalent visualization; a score of 3, poorer visualization on the MBIR image but still visible; and a score of 4, the lesion was not visible on the MBIR image. Lesions identified on reduced-dose images were not compared with those on standard-dose images because an increase or decrease in lesion conspicuity could have been due to an interval change in size as opposed to differences in image reconstruction.
Normal structure visualization.—In the final component of the subjective image review, readers assessed visualization of normal anatomic structures. Visualization of normal structures on reduced-dose MBIR and 100% ASIR images was compared with that on standard-dose 30% ASIR images. The two reviewers separately rated visualization of (a) the common bile duct at the level of the pancreatic head, (b) the superior mesenteric artery beyond its origin in the mesenteric root, and (c) the right hepatic vein. Visualization of each structure was again rated with a four-point scale: a score of 1 indicated superior visualization; a score of 2, equivalent visualization; a score of 3, poorer visualization but still visible; and a score of 4, the lesion was not visible.
Statistical Analyses
Patient radiation dose estimates (CTDIvol and SSDE) and the proportion of dose reduction for the reduced-dose MBIR protocol compared with the standard-dose 30% ASIR protocol were described by mean ± standard deviation and range.
Objective noise measurements from all reconstructions were compared pairwise for each anatomic area. The repeated one-way analysis of variance for this comparison was performed where repeated measurements of images in the same patients were not assumed to be independent. The calculated 95% confidence intervals (CIs) were adjusted for multiple comparisons (Scheffe adjustment). Descriptive statistics were used to evaluate the MTF data obtained in the phantom portion of the study.
Subjectively, overall image quality, visualization of focal lesions, and visualization of normal anatomic structures were rated by two readers. The Student t test was used to compare the subjective image quality ratings between different image reconstruction methods. Ratings by each reader initially were analyzed separately. Any differences between readers were then further analyzed with the Stuart-Maxwell test. Once it was established that there was no significant difference between the readers or no change in the inference, the subjective ratings were pooled for further analysis. Mean scores for the subjective image quality ratings were presented for the different image reconstruction methods by comparing reduced-dose 30% ASIR with standard-dose 30% ASIR with 95% CIs. The Student t test was used to compare the subjective quality rating of different image reconstruction methods with that of standard-dose 30% ASIR.
A P value of .05 or less indicated a significant difference for all hypothesis testing. Statistical analysis was performed by using statistical software (SAS, version 9.3; SAS Institute, Cary, NC). We have provided 95% CIs, as the study was somewhat underpowered.
Results
Subjects
Twenty-five patients (11 boys) who met our inclusion criteria were identified. Overall mean age of patients was 10.8 years (range, 1–20 years). Mean age of female patients was 11.3 years (range, 2–20 years). Mean age of male patients was 10.3 years (range, 3–17 years). Patients with a wide range of body types were included in our investigation, with patient weights ranging from 12 to 105 kg and calculated body mass indexes ranging from 14.8 to 39.4. The mean interval between the reduced-dose MBIR examination and the previously performed comparison standard-dose 30% ASIR examination was 121 days (range, 5–336 days).
Patient Radiation Dose
Mean CTDIvol for reduced-dose examinations was 3.1 mGy ± 2.3 (range, 1.0–11.3 mGy). Mean CTDIvol for comparison standard-dose examinations was 5.6 mGy ± 3.3 (range, 2.1–13.9 mGy). On average, CT scanner radiation output (based on CTDIvol) was 46% ± 12 (range, 19%–65%) lower for the reduced-dose protocol than for the standard-dose protocol.
Mean patient SSDE for reduced-dose examinations was 3.2 mGy ± 2.6 (range, 1.0–11.4 mGy). Mean patient SSDE for standard-dose examinations was 5.6 mGy ± 4.0 (range, 2.2–14.5 mGy). On average, mean patient dose based on SSDE was 44% ± 11.5 (range, 19%–64%) lower for the reduced-dose protocol than for the standard-dose protocol.
Objective Determination of Image Quality
Image noise.—Significant differences in objectively measured image noise were identified between the reduced-dose (MBIR and 100% ASIR) and standard-dose (30% ASIR) images for all anatomic areas assessed (abdominal aorta, liver, and paraspinal musculature).
Mean image noise measurements in the abdominal aorta were as follows: reduced-dose MBIR, 12.7 HU (95% CI: 11.6 HU, 13.9 HU); reduced-dose 100% ASIR, 15.3 HU (95% CI: 14.0 HU, 16.4 HU); and standard-dose 30% ASIR, 19.4 HU (95% CI: 18.3, 20.5). There was significantly less image noise in the abdominal aorta on reduced-dose MBIR images than on reduced-dose 100% ASIR images (P < .001) or standard-dose 30% ASIR images (P < .001). Reduced-dose 100% ASIR images also had significantly less image noise than did standard-dose 30% ASIR images (P < .001).
Mean image noise measurements in the liver were as follows: reduced-dose MBIR, 8.7 HU (95% CI: 8.3 HU, 9.2 HU); reduced-dose 100% ASIR, 10.4 HU (95% CI: 9.7 HU, 11.1 HU); and standard-dose 30% ASIR, 14.2 HU (95% CI: 13.6 HU, 14.8 HU). There was significantly less image noise in the liver on reduced-dose MBIR images than on reduced-dose 100% ASIR (P < .001) and standard-dose 30% ASIR (P < .001) images. Reduced-dose 100% ASIR images also had significantly less image noise than did standard-dose 30% ASIR images (P < .001).
Mean image noise measurements in the paraspinal musculature were as follows: reduced-dose MBIR images, 8.4 HU (95% CI: 8.0 HU, 8.9 HU); reduced-dose 100% ASIR images, 10.7 HU (95% CI: 9.9 HU, 11.5 HU); and standard-dose 30% ASIR images, 14.0 HU (95% CI: 13.1 HU, 14.8 HU). There was significantly less image noise in the paraspinal muscles on reduced-dose MBIR images than on reduced-dose 100% ASIR images (P < .001) or standard-dose 30% ASIR images (P < .001). Reduced-dose 100% ASIR images also had significantly less image noise than did standard-dose 30% ASIR images (P < .001).
Image spatial resolution.—At 80 kVp, spatial resolution based on MTF limiting resolution (MTF = 0.1) was 9.6 line pairs per centimeter (lp/cm) for reduced-dose MBIR, 7.1 lp/cm for reduced-dose 100% ASIR, and 7.1 lp/cm for standard-dose 30% ASIR. At 100 kVp and 120 kVp, spatial resolution was also better for reduced-dose MBIR compared with reduced-dose 100% ASIR and standard-dose 30% ASIR (Table 2).
Table 2.
MTF Measurements
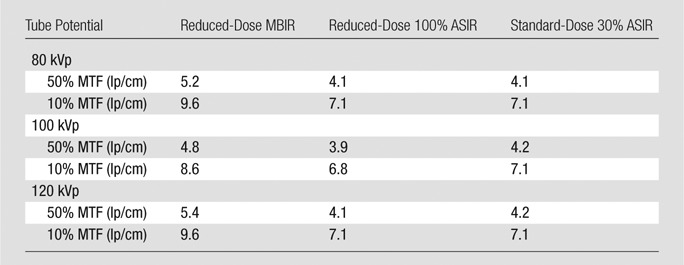
Note.—The MTF was measured by using identical CT parameters for our clinical reduced-dose protocol (reconstructed with MBIR and 100% ASIR) and standard-dose (reconstructed with 30% ASIR) CT protocols at 80, 100, and 120 kVp.
Subjective Determination of Image Quality
In analyzing the ratings between the two readers with the Student t test, there was no difference in the results for each reader’s ratings individually for any comparison, except for the comparison between reduced-dose 100% ASIR and standard-dose CT when evaluating soft tissues. Further analysis of this specific comparison was performed by using the Stuart-Maxwell test, which returned a highly nonsignificant result (P = .816).
Overall image quality.—Ratings were based on the aforementioned four-point scale. There was no significant difference in diagnostic quality ratings between the reduced-dose MBIR images and the standard-dose 30% ASIR images in the soft tissues (mean, 2.08 [95% CI: 1.93, 2.24]; P = .3) or the lungs (mean, 1.98 [95% CI: 1.83, 2.13]; P = .8). Reduced-dose MBIR images were slightly significantly inferior in overall diagnostic quality compared with the standard-dose 30% ASIR images in the evaluation of the bones (mean, 2.17 [95% CI: 2.06, 2.28]; P = .004).
Reduced-dose images reconstructed with 100% ASIR were rated as significantly inferior to standard-dose 30% ASIR images for the soft tissues (mean, 2.23 [95% CI: 2.09, 2.37]; P < .002), lungs (mean, 2.96 [95% CI: 2.84, 3.08]; P < .001), and bones (mean, 2.79 [95% CI: 2.66, 2.93]; P < .001) (Fig 2).
Figure 2a:
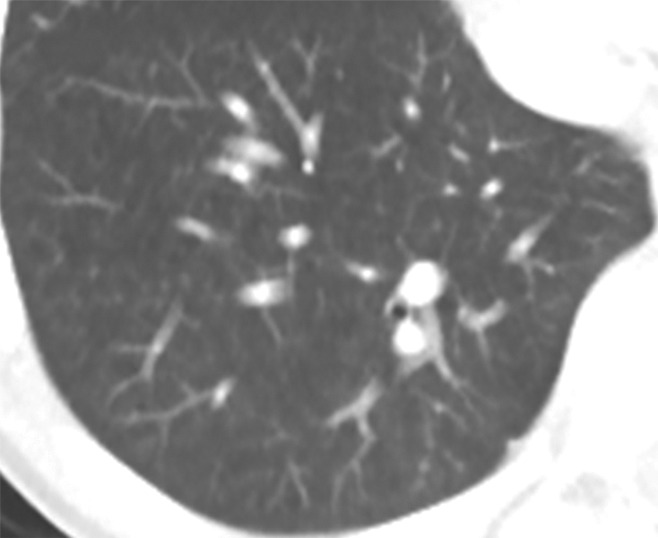
CT images in a 10-year-old boy with diffuse large B-cell lymphoma. Axial reduced-dose CT images reconstructed with (a) MBIR and (b) 100% ASIR show featureless (smoothing effect) appearance of the lungs, with loss of parenchymal detail on b. In particular, distal airways and peripheral vascular structures in the lungs appear indistinct and in some instances are not seen at all on reduced-dose 100% ASIR images.
Figure 2b:
CT images in a 10-year-old boy with diffuse large B-cell lymphoma. Axial reduced-dose CT images reconstructed with (a) MBIR and (b) 100% ASIR show featureless (smoothing effect) appearance of the lungs, with loss of parenchymal detail on b. In particular, distal airways and peripheral vascular structures in the lungs appear indistinct and in some instances are not seen at all on reduced-dose 100% ASIR images.
Lesion visualization.—Eighteen pediatric patients with a total of 42 lesions were included in this portion of our study (Table 3). The mean number of lesions per patient was 2.3. The maximum number of lesions evaluated per patient was four. Each reviewer independently rated lesion visualization with both reduced-dose reconstructions (MBIR and 100% ASIR).
Table 3.
Lesions Included in the Lesion Visualization Portion of the Study
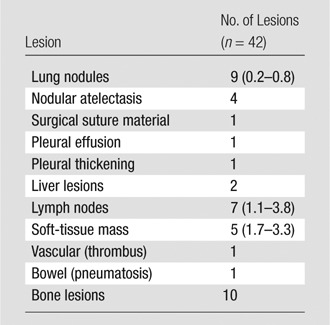
Note.—We compared reduced-dose MBIR images with reduced-dose 100% ASIR images. Data in parentheses are the size range (in centimeters).
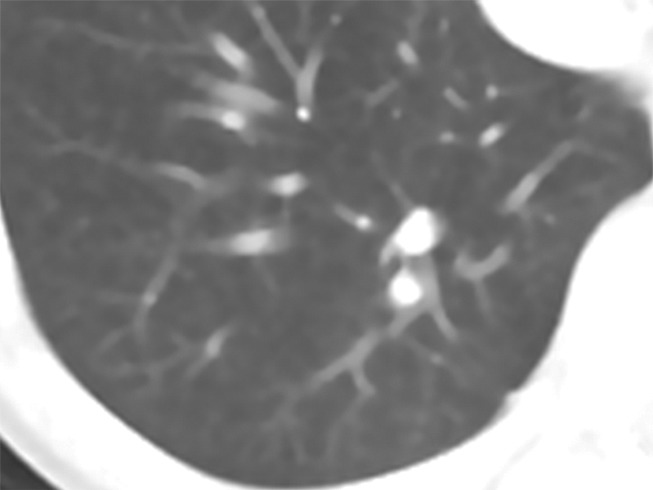
All lesions were visible with both reduced-dose reconstructions (Figs 3, 4; Fig E1 [online]). For 32 (38% [95% CI: 28%, 48%]) of 84 lesion ratings, MBIR images were rated as superior to 100% ASIR images. For the remaining 52 (62%) lesion ratings, MBIR images were rated as equivalent to 100% ASIR images. The MBIR images were not rated inferior to the 100% ASIR images for any lesion.
Figure 3a:
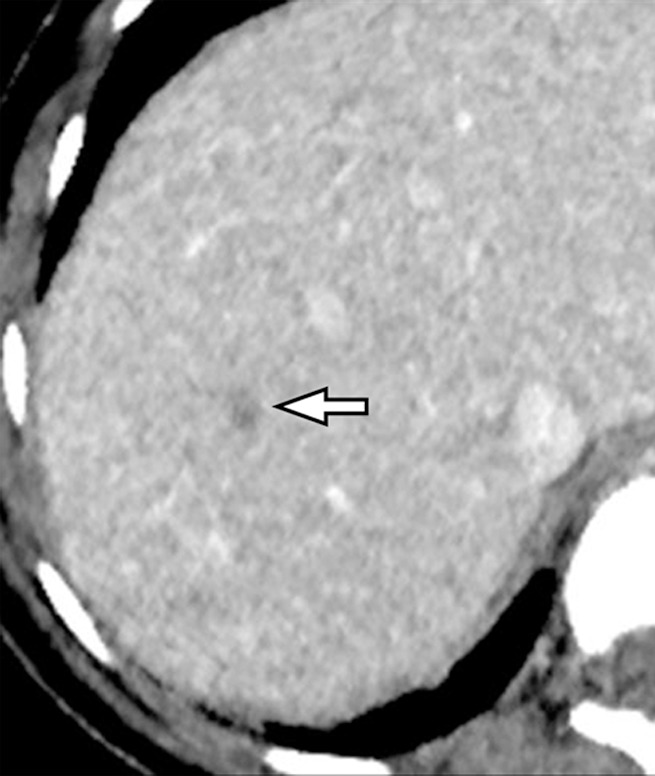
CT images in a 14-year-old girl with treated diffuse large-cell lymphoma secondary to immunosuppression for severe Crohn disease. (a) Reduced-dose MBIR reconstructed image shows a focal hypoattenuating lesion in the right lobe of the liver (arrow). The lesion is more conspicuous on a than on (b) reduced-dose 100% ASIR or (c) reduced-dose FBP images.
Figure 4a:
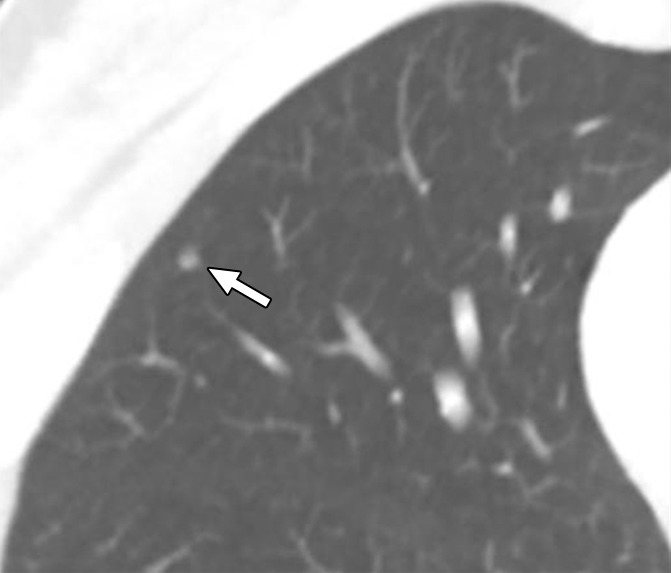
Reduced-dose CT images reconstructed with (a) MBIR and (b) 100% ASIR in a 19-year-old woman with a history of treated Hodgkin disease show a nonspecific 3-mm lung nodule (arrow). The lung appears unusually smooth and featureless on b in comparison with a; however, the nodule is seen equally well on both images.
Figure 3b:
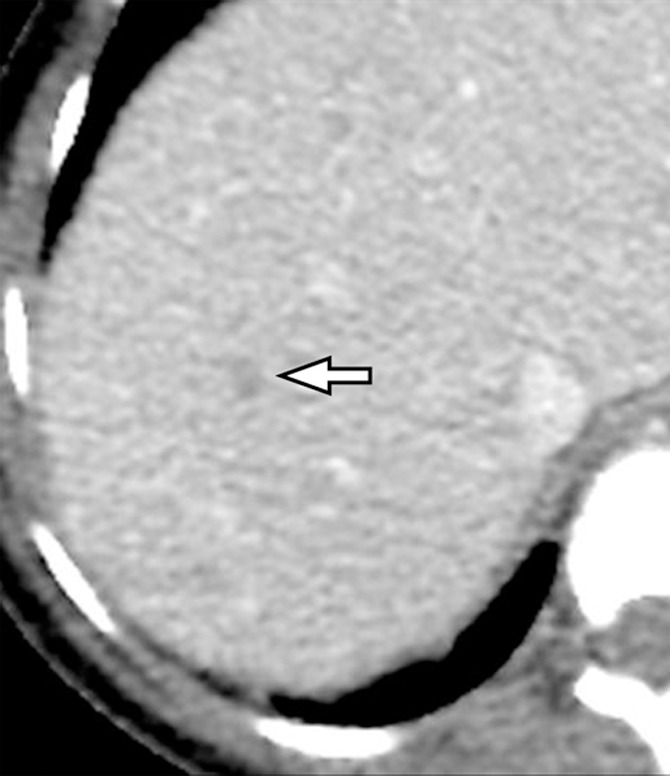
CT images in a 14-year-old girl with treated diffuse large-cell lymphoma secondary to immunosuppression for severe Crohn disease. (a) Reduced-dose MBIR reconstructed image shows a focal hypoattenuating lesion in the right lobe of the liver (arrow). The lesion is more conspicuous on a than on (b) reduced-dose 100% ASIR or (c) reduced-dose FBP images.
Figure 3c:
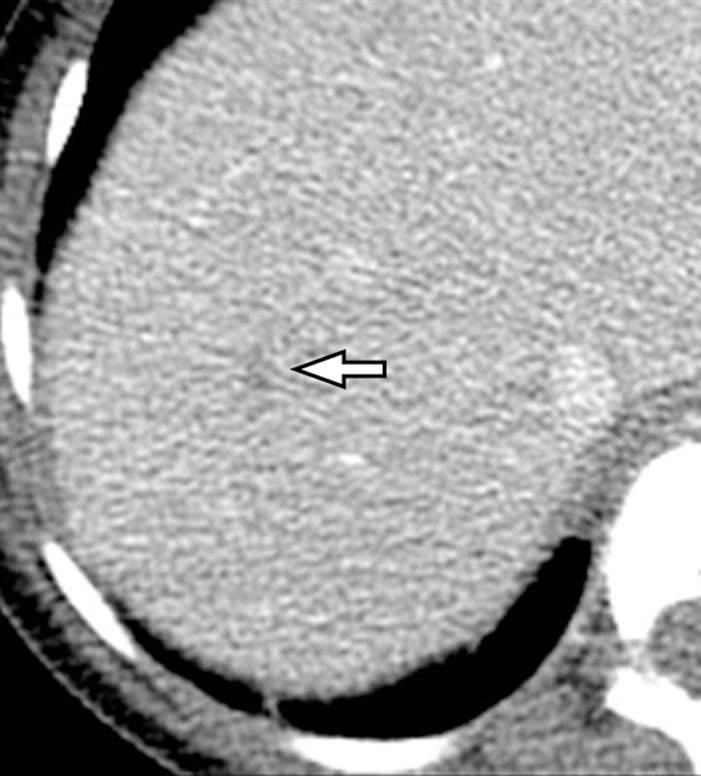
CT images in a 14-year-old girl with treated diffuse large-cell lymphoma secondary to immunosuppression for severe Crohn disease. (a) Reduced-dose MBIR reconstructed image shows a focal hypoattenuating lesion in the right lobe of the liver (arrow). The lesion is more conspicuous on a than on (b) reduced-dose 100% ASIR or (c) reduced-dose FBP images.
Figure 4b:
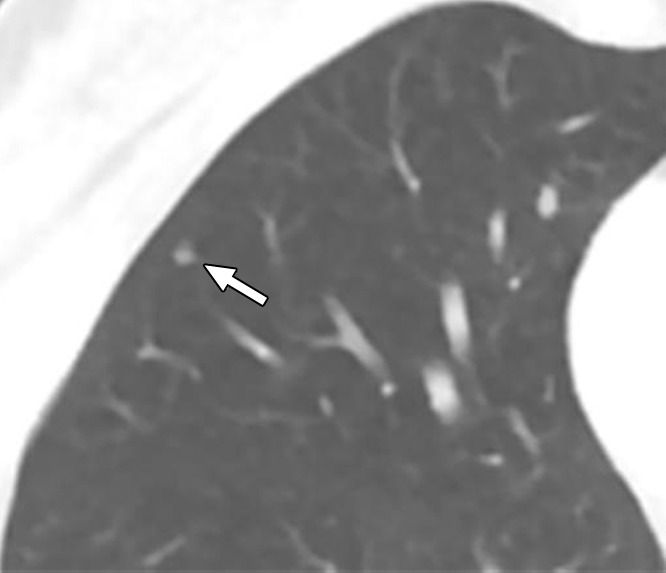
Reduced-dose CT images reconstructed with (a) MBIR and (b) 100% ASIR in a 19-year-old woman with a history of treated Hodgkin disease show a nonspecific 3-mm lung nodule (arrow). The lung appears unusually smooth and featureless on b in comparison with a; however, the nodule is seen equally well on both images.
Normal structure visualization.—There was no significant difference between reduced-dose images (both MBIR and 100% ASIR images) and comparison standard-dose 30% ASIR images regarding visualization of normal anatomic structures (Fig 5). Complete results are shown in Table 4.
Figure 5a:
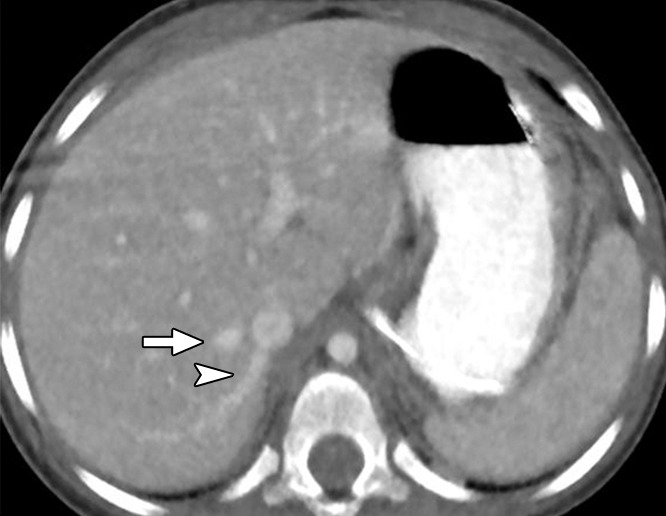
Reduced-dose axial CT images reconstructed with (a) MBIR and (b) 100% ASIR in a 30-month-old girl with a history of malignant germ cell tumor show the right hepatic vein (arrow) and an accessory right hepatic vein (arrowhead). Both venous structures can be seen more clearly in a than in b.
Table 4.
Normal Anatomic Structure Visualization
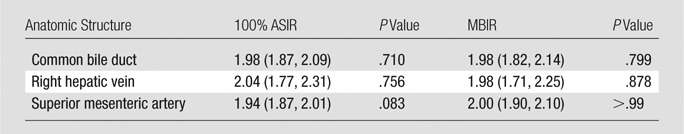
Note.—Unless otherwise indicated, data are mean ratings. Data in parentheses are 95% CIs. Subjective ratings were obtained by comparing reduced-dose MBIR images with 100% ASIR images; standard-dose 30% ASIR images served as the reference standard. Ratings were based on the following scale: 1 = superior to standard-dose 30% ASIR; 2 = equivalent visualization; 3 = inferior visualization, but still visible; 4 = not visible.
Figure 5b:
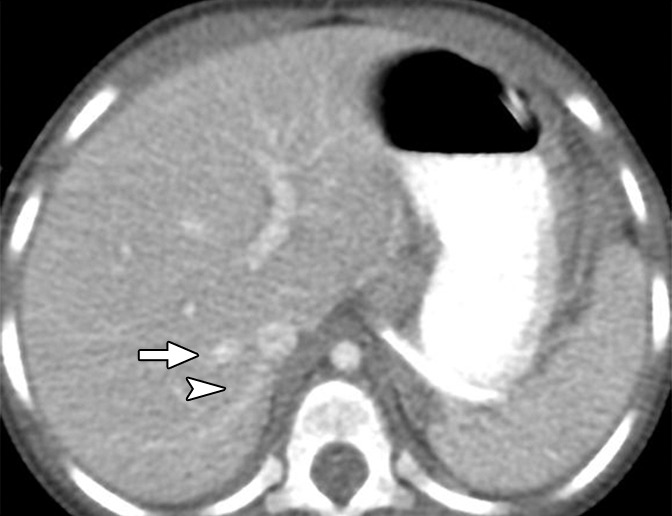
Reduced-dose axial CT images reconstructed with (a) MBIR and (b) 100% ASIR in a 30-month-old girl with a history of malignant germ cell tumor show the right hepatic vein (arrow) and an accessory right hepatic vein (arrowhead). Both venous structures can be seen more clearly in a than in b.
Discussion
Our results show that CT imaging with the MBIR technique enables significant reduction of patient radiation dose while preserving diagnostic image quality. By using the parameters described, both CTDIvol and SSDE measurements showed mean dose reductions of approximately 45% in pediatric patients who underwent body CT. We believe that even greater dose reductions are possible with MBIR, as the images reviewed in this study are still diagnostic and have less noise and better spatial resolution than do standard-dose 30% ASIR images. In theory, such dose reductions should decrease the potential risks of ionizing radiation exposure, including radiation-induced malignancy. Objective measurements of image quality revealed that reduced-dose pediatric CT examinations of the body with the MBIR technique were superior to both reduced-dose images reconstructed with 100% ASIR and standard-dose images reconstructed with 30% ASIR. Reduced-dose MBIR images had significantly less image noise than did images reconstructed with 100% ASIR and comparison standard-dose 30% ASIR images. Reduced image noise in pediatric body CT images should have two potential benefits. First, reduced image noise should, in theory, improve lesion detection and characterization. Second, reduced image noise enables preservation of image quality while using lower tube currents and thus lower radiation dose.
Our objective phantom testing also showed that the reduced-dose images reconstructed with MBIR have superior spatial resolution based on MTF analysis when compared with reduced-dose 100% ASIR and standard-dose 30% ASIR images. While standard-dose 30% ASIR images and reduced-dose 100% ASIR images had very similar spatial resolution, reduced-dose MBIR images were consistently superior with respect to limiting resolution across a range of tube potentials in a soft tissue–like phantom. MTF has been shown to be material dependent (21). The superiority of MBIR compared with ASIR could be even more pronounced in a lunglike attenuation phantom; however, we did not evaluate this in the current study. The better spatial resolution offered by MBIR should be especially beneficial in small children, allowing for detection of smaller lesions and improving lesion delineation.
Subjectively, overall image quality was for the most part maintained on reduced-dose MBIR images. Reduced-dose MBIR image quality was equivalent to standard-dose 30% ASIR image quality for soft-tissue structures and the lungs. However, reduced-dose MBIR image quality was slightly inferior to that of standard-dose 30% ASIR images regarding the appearance of the bones. Reduced-dose images reconstructed with the 100% ASIR technique were rated as inferior to standard-dose 30% ASIR images for soft-tissue, lung, and bone image quality.
It should be noted that reduced-dose images reconstructed with MBIR have a slightly different texture compared with images reconstructed with the FBP or low-percentage ASIR techniques, appearing unusually smooth or mottled. Interestingly, this MBIR appearance is most pronounced on axial images and is less conspicuous on multiplanar reformatted images reconstructed with MBIR. Despite this unique look, our results show that both objective and subjective image quality are nearly always equivalent or superior for reduced-dose MBIR images compared with reduced-dose 100% ASIR images and standard-dose 30% ASIR images. Additionally, the smoothing effect on the lungs was much less noticeable on reduced-dose MBIR images than on 100% ASIR images. The periphery of the lungs appears nearly featureless on reduced-dose 100% ASIR images, whereas detail is restored on reduced-dose MBIR images. Since the primary focus of pediatric body CT is usually assessment of soft-tissue structures and the lungs, reduced-dose imaging with MBIR image reconstruction yields satisfactory image quality.
Subjectively, inferior image quality of reduced-dose MBIR images when evaluating the bones was primarily due to perceived loss of trabecular detail when compared with standard-dose 30% ASIR images. Although the MBIR images have higher spatial resolution and less image noise than do 30% ASIR images, it is possible that the smoothing and mottled appearance of the MBIR images results in a somewhat unnatural or out of focus appearance and leads to the perception of loss of trabecular pattern by the reader. The increased image noise on the FBP and ASIR images may result in the perception of improved visualization at high contrast edges (such as bone), causing the bones to have a more natural appearance and hence being more satisfactory. In our routine clinical practice with reduced-dose body CT, we have found that creating a separate series from the same CT data acquisition (reconstructed with either pure FBP or 30% ASIR) yields suitable image quality and enables diagnostic assessment of osseous structures.
The major limitation of our study was the lack of reviewer blinding. Because of the different inherent imaging appearances of the different reconstruction methods, reviewers could not be truly blinded when they compared different imaging sets. It is conceivable that this could have led to bias, as the readers may have been biased toward demonstrating the acceptability of the MBIR images. A second major limitation of our study was the method with which the lesion detection portion of the study was performed. Because of temporal differences in the two CT acquisitions (standard-dose and reduced-dose protocols), we did not think that we could reliably compare specific lesions between the two protocols, as lesions may have evolved or regressed due to the natural history of the disease process or in patients undergoing antineoplastic therapy. To address this potential confounding factor, we chose to compare two different reconstructions (MBIR and 100% ASIR) of only the reduced-dose protocol acquisition, with the understanding that this comparison was limited, as the 100% ASIR technique is not typically used in clinical practice.
A more minor limitation was the fact that comparison standard-dose 30% ASIR CT examinations were obtained at different time points with respect to the reduced-dose CT examinations, as mentioned previously. It is possible that factors other than image reconstruction technique could affect subjective image quality (eg, intravenous contrast material bolus timing). Ethical concerns prohibit us from performing multiple CT examinations in pediatric patients simply to assess differences in image reconstruction techniques. As a result, variable amounts of time passed between clinically indicated standard- and reduced-dose CT examinations. To minimize this limitation, our study included only pediatric patients who underwent both standard-dose and reduced-dose CT examinations within a 12-month period, with an average interval of approximately 4 months. In theory, this interval could also affect the amount of radiation dose received by a given patient based on CTDIvol, particularly if the patient’s body habitus changed in the interval because of weight gain or weight loss. However, our use of SSDE to calculate patient radiation dose should have limited this effect, as the SSDE calculation accounts for patient size.
In conclusion, our results show that MBIR enables reduced-dose pediatric body CT with preserved image quality. Additional investigations are needed to establish how MBIR affects image quality when imaging other areas of the body, how it affects detection and characterization of specific abnormalities, and if further radiation dose reductions can be achieved. While a goal of reducing radiation doses in pediatric CT is important, all new dose reduction technologies must be critically assessed to ensure that image quality and diagnostic capability are preserved.
Advances in Knowledge
■ Both objectively and subjectively, image quality of reduced-dose images reconstructed with model-based iterative reconstruction (MBIR) is superior or equivalent to that of standard-dose CT images and is superior to that of reduced-dose CT images reconstructed with 100% adaptive statistical iterative reconstruction (ASIR) in pediatric patients undergoing body CT.
■ Our reduced-dose protocol yielded substantial reduction in radiation dose (mean reduction, 44%; range, 19%–64%).
■ Objectively, reduced-dose MBIR images had decreased image noise compared with standard-dose 30% ASIR images (aorta, 12.7 HU vs 19.4 HU; liver, 8.7 HU vs 14.2 HU; muscle, 8.4 HU vs 14.0 HU [P < .001]).
■ Subjectively, reduced-dose MBIR images were equivalent to standard-dose 30% ASIR images in the soft tissues (mean score, 2.08 and 1.98, respectively, where 2 indicated equivalent image quality) but were slightly inferior in bones (mean score, 2.17) (P = .004).
■ Reduced-dose images reconstructed with MBIR are superior in terms of spatial resolution in a phantom when compared with reduced-dose images reconstructed with 100% ASIR and standard-dose images reconstructed with 30% ASIR (at 80 kVp, reduced-dose MBIR modulation transfer function [MTF] was 9.6 line pairs per centimeter [lp/cm]; at 100% ASIR, MTF was 7.1 lp/cm; and at standard-dose 30% ASIR, MTF was 7.1 lp/cm).
Implications for Patient Care
■ Clinical pediatric body CT can be performed at reduced patient radiation doses while maintaining diagnostic quality with MBIR.
■ Images reconstructed with MBIR have decreased image noise and superior spatial resolution compared with a combination of ASIR and filtered back projection.
SUPPLEMENTAL FIGURE
Received February 11, 2013; revision requested April 4; revision received July 9; accepted July 24; final version accepted August 1.
Funding: This research was supported by the National Institutes of Health (grant 2UL1TR000433).
Disclosures of Conflicts of Interest: E.A.S. No relevant conflicts of interest to disclose. J.R.D. No relevant conflicts of interest to disclose. M.M.G. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: none to disclose. Other relationships: has a research collaboration with GE Global Research for development of a combined x-ray, optical, and ultrasound system for breast imaging. E.G.C. No relevant conflicts of interest to disclose. N.K. No relevant conflicts of interest to disclose. P.J.S. No relevant conflicts of interest to disclose.
Abbreviations:
- ASIR
- adaptive statistical iterative reconstruction
- CI
- confidence interval
- CTDIvol
- volumetric CT dose index
- FBP
- filtered back projection
- MBIR
- model-based iterative reconstruction
- MTF
- modulation transfer function
- SSDE
- size-specific dose estimate
References
- 1.Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med 2007;357(22):2277–2284. [DOI] [PubMed] [Google Scholar]
- 2.Brody AS, Frush DP, Huda W, Brent RL; American Academy of Pediatrics Section on Radiology. Radiation risk to children from computed tomography. Pediatrics 2007;120(3):677–682. [DOI] [PubMed] [Google Scholar]
- 3.Frush DP. Review of radiation issues for computed tomography. Semin Ultrasound CT MR 2004;25(1):17–24. [DOI] [PubMed] [Google Scholar]
- 4.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation , National Research Council. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII Phase 2. Washington, DC: The National Academies Press, 2006. [PubMed] [Google Scholar]
- 5.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176(2):289–296. [DOI] [PubMed] [Google Scholar]
- 6.Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012;380(9840):499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goske MJ, Applegate KE, Boylan J, et al. The Image Gently campaign: working together to change practice. AJR Am J Roentgenol 2008;190(2):273–274. [DOI] [PubMed] [Google Scholar]
- 8.Verdun FR, Lepori D, Monnin P, Valley JF, Schnyder P, Gudinchet F. Management of patient dose and image noise in routine pediatric CT abdominal examinations. Eur Radiol 2004;14(5):835–841. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MD. Pediatric CT radiation dose: how low can you go? AJR Am J Roentgenol 2009;192(5):1292–1303. [DOI] [PubMed] [Google Scholar]
- 10.Hara AK, Paden RG, Silva AC, Kujak JL, Lawder HJ, Pavlicek W. Iterative reconstruction technique for reducing body radiation dose at CT: feasibility study. AJR Am J Roentgenol 2009;193(3):764–771. [DOI] [PubMed] [Google Scholar]
- 11.Singh S, Kalra MK, Hsieh JA, et al. Abdominal CT: comparison of adaptive statistical iterative and filtered back projection reconstruction techniques. Radiology 2010;257(2):373–383. [DOI] [PubMed] [Google Scholar]
- 12.Singh S, Kalra MK, Shenoy-Bhangle AS, et al. Radiation dose reduction with hybrid iterative reconstruction for pediatric CT. Radiology 2012;263(2):537–546. [DOI] [PubMed] [Google Scholar]
- 13.Beister M, Kolditz D, Kalender WA. Iterative reconstruction methods in X-ray CT. Phys Med 2012;28(2):94–108. [DOI] [PubMed] [Google Scholar]
- 14.Pickhardt PJ, Lubner MG, Kim DH, et al. Abdominal CT with model-based iterative reconstruction (MBIR): initial results of a prospective trial comparing ultralow-dose with standard-dose imaging. AJR Am J Roentgenol 2012;199(6):1266–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katsura M, Matsuda I, Akahane M, et al. Model-based iterative reconstruction technique for radiation dose reduction in chest CT: comparison with the adaptive statistical iterative reconstruction technique. Eur Radiol 2012;22(8):1613–1623. [DOI] [PubMed] [Google Scholar]
- 16.Husarik DB, Marin D, Samei E, et al. Radiation dose reduction in abdominal computed tomography during the late hepatic arterial phase using a model-based iterative reconstruction algorithm: how low can we go? Invest Radiol 2012;47(8):468–474. [DOI] [PubMed] [Google Scholar]
- 17.Singh S, Kalra MK, Do S, et al. Comparison of hybrid and pure iterative reconstruction techniques with conventional filtered back projection: dose reduction potential in the abdomen. J Comput Assist Tomogr 2012;36(3):347–353. [DOI] [PubMed] [Google Scholar]
- 18.Deák Z, Grimm JM, Treitl M, et al. Filtered back projection, adaptive statistical iterative reconstruction, and a model-based iterative reconstruction in abdominal CT: an experimental clinical study. Radiology 2013;266(1):197–206. [DOI] [PubMed] [Google Scholar]
- 19.Boone J, Strauss K, Cody D, et al. Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. Report of AAPM Task Group 204. College Park, Md: American Association of Physicists in Medicine, 2011. [Google Scholar]
- 20.Brady SL, Kaufman RA. Investigation of American Association of Physicists in Medicine Report 204 size-specific dose estimates for pediatric CT implementation. Radiology 2012;265(3):832–840. [DOI] [PubMed] [Google Scholar]
- 21.Richard S, Husarik DB, Yadava G, Murphy SN, Samei E. Towards task-based assessment of CT performance: system and object MTF across different reconstruction algorithms. Med Phys 2012;39(7):4115–4122. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


