Abstract
Adalimumab and other tumor necrosis factor-α inhibitors have been shown in the recent years to successfully treat sarcoidosis refractory to systemic corticosteroids and other agents. However, there have been an increasing number of cases of sarcoidosis paradoxically induced by these agents. It is hypothesized that this is due to the disruption of the fine balance of cytokines involved in granuloma formation. We describe the first case of adalimumab-induced subcutaneous nodular sarcoidosis in a patient with pulmonary sarcoidosis.
Keywords: pulmonary sarcoidosis, anti-TNF-α antibody, adalimumab, subcutaneous nodular sarcoidosis
Introduction
Over the past decade, treatment options of sarcoidosis have grown and now include glucocorticoids and cytotoxic agents like methotrexate, azathioprine and leflunomide (1). There have been an increasing number of studies demonstrating efficacy of biological agents such as adalimumab and other tumor necrosis factor (TNF)-α inhibitors in treating refractory sarcoidosis (1,2). Interestingly, a paradoxical phenomenon of sarcoidosis induced by these agents has been described in the recent years (3,4). In these case reports, these agents were used to treat a variety of rheumatologic conditions, after which sarcoidosis developed most frequently in the lungs and surrounding lymph nodes (3) We present the first case of subcutaneous nodular sarcoidosis induced adalimumab.
Case Report
A forty-nine year old African American woman with a history of pulmonary sarcoidosis presented for multiple subcutaneous nodules developing on her extremities after starting adalimumab. She was initially diagnosed with sarcoidosis seventeen years ago when she presented with cough, shortness of breath and weight loss, and transbronchial biopsy performed showed non-necrotizing granulomas without any evidence of infectious causes. She was initially treated with high dose corticosteroids with gradual tapering as her condition improved. After being symptom-free for eleven years, she started developing severe chest pain six years ago. She underwent extensive pulmonary, cardiac and gastroenterology workup, and was diagnosed with costochondritis secondary to sarcoidosis. She responded well to systemic corticosteroids but due to multiple side effects, methotrexate was added as a steroid-sparing agent. She only had a partial response to methotrexate, and ultimately adalimumab 40mg subcutaneously every other week was initiated. Her chest pain resolved completely after two months and she was tapered off prednisone and methotrexate over the next six months.
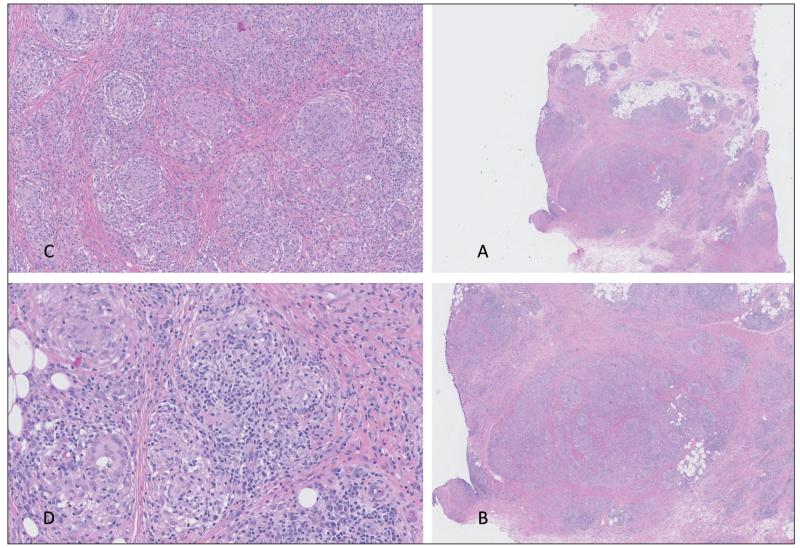
After eight months on adalimumab, she developed multiple subcutaneous nodules on her arms and legs. These were firm, mobile, non-tender nodules without overlying epidermal changes measuring from 1cm to over 5cm in diameter. An incisional biopsy performed on a lesion on her left forearm demonstrated non-necrotizing granulomas in the subcutis (Figure 1).
Fig. 1.
An incisional biopsy shows numerous small, distinct, non-necrotizing granulomas in the subcutis formed by epithelioid histiocytes and multinucleated giant cells, A: hematoxylin and eosin stain (H&E) low power field, B: H&E stain x2, C: H&E stain x4, D: H&E stain x8.
A work-up of other causes of granulomatoses including tuberculosis, fungal infections and foreign material was negative. These results suggested a diagnosis of subcutaneous nodular sarcoidosis. Adalimumab was thought to be the causative agent and was discontinued. Her subcutaneous nodules were resolved in few days after the discontinuation of adalimumab. However, within one month of stopping adalimumab, her severe chest pain returned and adalimumab was resumed in addition to prednisone 10mg daily. Upon rechallenge, her chest pain responded well but the subcutaneous nodules on her extremities recurred. When leflunomide 20 mg daily was added to current regimen, the patient’s subcutaneous nodules started to regress. At the time of manuscript submission, three months after the addition of leflunomide, the patient was free of chest pain and subcutaneous nodules.
Discussion
This is the first case of subcutaneous nodular sarcoidosis induced adalimumab in the English language literature. The recurrence of the lesions upon medication rechallenge supports this diagnosis. Paradoxical induction of inflammatory conditions by TNF-α inhibitors has been extensively described for psoriasis, and there are emerging reports of sarcoidosis induced by these agents (5). In addition to the lungs and lymph nodes, sarcoid lesions associated to TNF-α inhibitors have also been reported in the skin, kidneys, central nervous system, liver and eyes (6-8). The mechanism for this phenomenon remains unknown but is hypothesized to be caused by the disruption of the fine balance of the main cytokines involved in granuloma formation, including TNF-α, interferon-ɣ and interleukin-2 (8). There is increased TNF-α activity in sarcoidosis but it is likely that TNF-α is one of the mediators in the granuloma-formation cascade, increasing or decreasing different cell signaling pathways dependent upon surrounding cells and cytokines, rather than producing a specific immune response (9).
Additional research is needed to elucidate the role of TNF-α in this disease process. Given the increasing frequency of cases, it is important for clinicians to be aware of this side effect and maintain a high index of suspicion for any sarcoidosis-like presentations during treatment with TNF-α inhibitors. Finally, the observation that the addition of leflunomide, which inhibits proliferation of activated and autoimmune lymphocytes, causes the regression of adalimumab-induced subcutaneous nodular sarcoidosis shows an important way of how autoimmune induction can be suppressed.
Acknowledgement
The authors would like to express their thanks to Dr. Amanda Marsch for helping us to prepare pathology images.
References
- 1.Baughman RP, Nunes H, Sweiss NJ, et al. Established and experimental medical therapy of pulmonary sarcoidosis. Eur Respir J. 2013;41:1424–1438. doi: 10.1183/09031936.00060612. [DOI] [PubMed] [Google Scholar]
- 2.Korsten P, Mirsaeidi M, Sweiss NJ. Nonsteroidal therapy of sarcoidosis. Curr Opin Pulm Med. 2013;19:516–523. doi: 10.1097/MCP.0b013e3283642ad0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tong D, Manolios N, Howe G, et al. New onset sarcoid-like granulomatosis developing during anti-TNF therapy: an under-recognised complication. Intern Med J. 2012;42:89–94. doi: 10.1111/j.1445-5994.2011.02612.x. [DOI] [PubMed] [Google Scholar]
- 4.Burns AM, Green PJ, Pasternak S. Etanercept-induced cutaneous and pulmonary sarcoid-like granulomas resolving with adalimumab. J Cutan Pathol. 2012;39:289–293. doi: 10.1111/j.1600-0560.2011.01795.x. [DOI] [PubMed] [Google Scholar]
- 5.Wollina U, Hansel G, Koch A, et al. Tumor necrosis factor-alpha inhibitor-induced psoriasis or psoriasiform exanthemata: first 120 cases from the literature including a series of six new patients. Am J Clin Dermatol. 2008;9:1–14. doi: 10.2165/00128071-200809010-00001. [DOI] [PubMed] [Google Scholar]
- 6.Seve P, Varron L, Broussolle C, et al. Sarcoid-related uveitis occurring during adalimumab therapy. Ocul Immunol Inflamm. 2012;20:59–60. doi: 10.3109/09273948.2011.623213. [DOI] [PubMed] [Google Scholar]
- 7.Korsten P, Sweiss NJ, Nagorsnik U, et al. Drug-induced granulomatous interstitial nephritis in a patient with ankylosing spondylitis during therapy with adalimumab. Am J Kidney Dis. 2010;56:e17–21. doi: 10.1053/j.ajkd.2010.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Massara A, Cavazzini L, La Corte R, et al. Sarcoidosis appearing during anti-tumor necrosis factor alpha therapy: a new “class effect” paradoxical phenomenon. Two case reports and literature review. Semin Arthritis Rheum. 2010;39:313–319. doi: 10.1016/j.semarthrit.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Clementine RR, Lyman J, Zakem J, et al. Tumor necrosis factor-alpha antagonist-induced sarcoidosis. J Clin Rheumatol. 2010;16:274–279. doi: 10.1097/RHU.0b013e3181efa190. [DOI] [PubMed] [Google Scholar]