Abstract
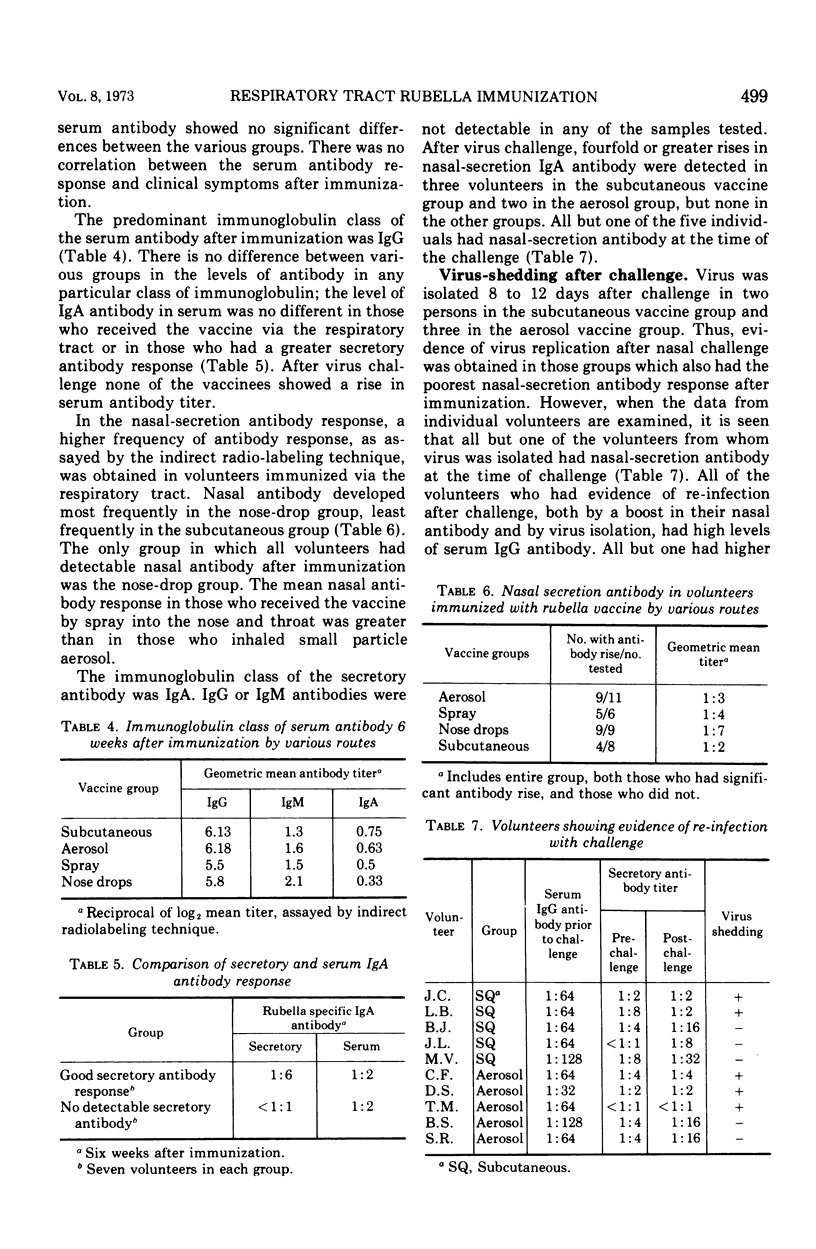
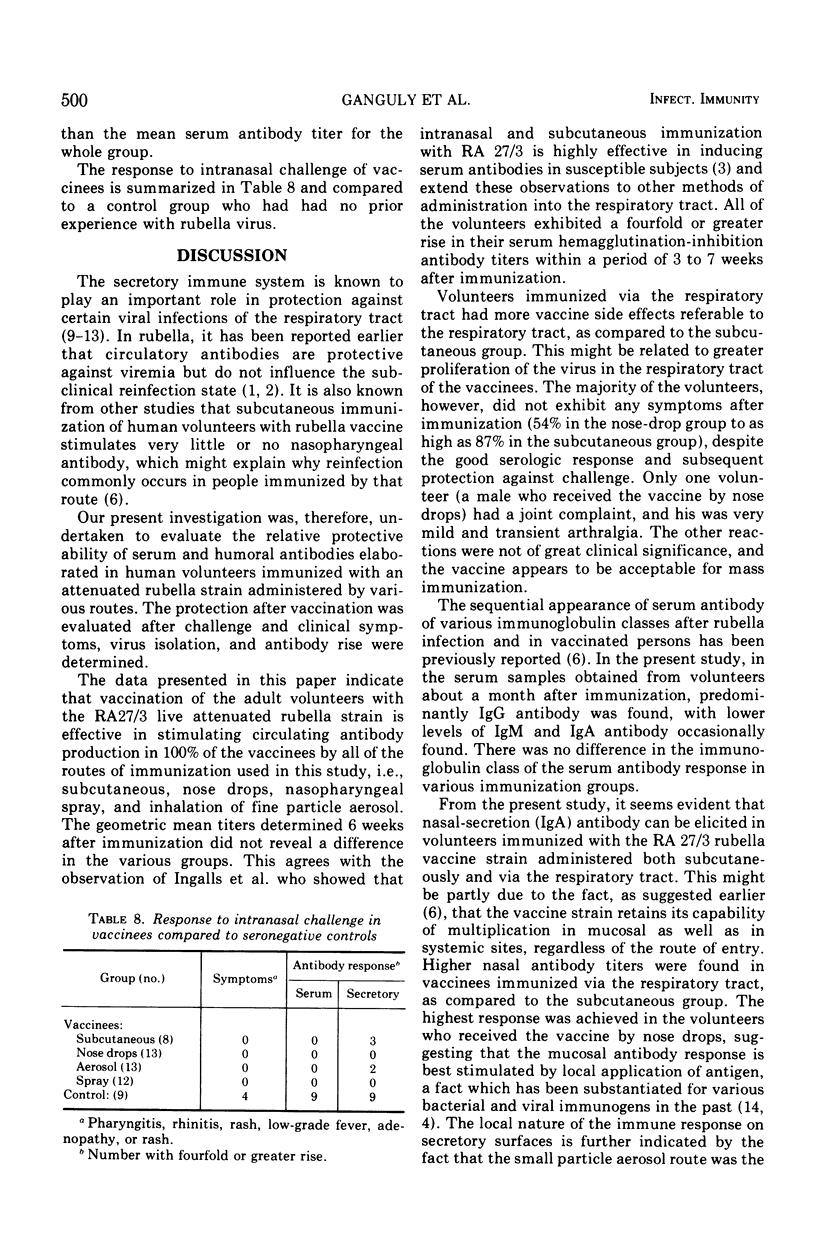
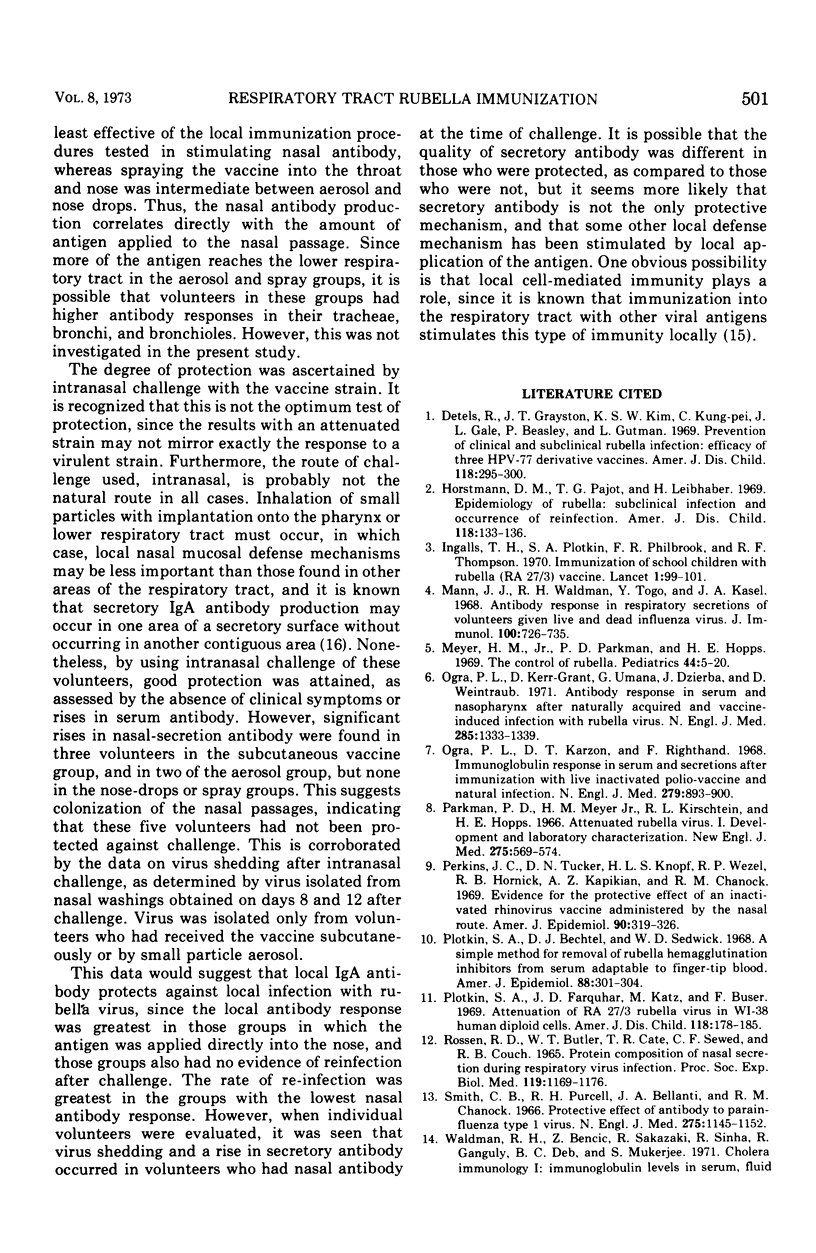
The efficacy of various routes of administration of the live attenuated rubella virus vaccine was evaluated by using 46 seronegative volunteers who were divided into 4 vaccine groups: subcutaneous, nosedrops, spray into posterior oropharynx and nose using large particle aerosol, and inhalation of small particle aerosol through the mouth. Seroconversion was observed in all of the vaccinees regardless of route of immunization. Nasal secretion antibody 6 weeks after immunization was highest in the volunteers who received the vaccine by nose drops (all members of this group had demonstrable nasal secretion antibody after immunization). Only half of the volunteers in the subcutaneous group developed demonstrable nasal secretion antibody. This suggests that nasal secretion antibody was best stimulated when vaccine was given directly into the nose. Volunteers were challenged with the vaccine intranasally at 6 to 8 weeks. None of the volunteers exhibited clinical symptoms or fourfold or greater serum antibody rises after challenge, but fourfold or greater nasal secretion antibody rises were observed in three volunteers in the subcutaneous vaccine group and two in the aerosol group, suggesting that those volunteers had not been protected against challenge. Rubella virus was isolated 8 to 12 days after challenge in two persons in the subcutaneous group and three in the aerosol vaccine group, but none in the nose drops or spray groups. Thus, protection after nasal challenge appeared to be best in those groups which also had the best nasal secretion antibody response after immunization. However, protection did not seem to be correlated with either nasal secretion or serum antibody levels.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Detels R., Grayston J. T., Kim K. S., Chen K. P., Gale J. L., Beasley R. P., Gutman L. Prevention of clinical and subclinical rubella infection. Efficacy of three HPV-77 derivative vaccines. Am J Dis Child. 1969 Aug;118(2):295–300. doi: 10.1001/archpedi.1969.02100040297026. [DOI] [PubMed] [Google Scholar]
- Horstmann D. M., Pajot T. G., Liebhaber H. Epidemiology of rubella. Subclinical infection and occurrence of reinfection. Am J Dis Child. 1969 Jul;118(1):133–136. [PubMed] [Google Scholar]
- Ingalls T. H., Plotkin S. A., Philbrook F. R., Thompson R. F. Immunisation of schoolchildren with rubella (RA27-3) vaccine. Intranasal and subcutaneous administration. Lancet. 1970 Jan 17;1(7638):99–101. doi: 10.1016/s0140-6736(70)90460-5. [DOI] [PubMed] [Google Scholar]
- Mann J. J., Waldman R. H., Togo Y., Heiner G. G., Dawkins A. T., Kasel J. A. Antibody response in respiratory secretions of volunteers given live and dead influenza virus. J Immunol. 1968 Apr;100(4):726–735. [PubMed] [Google Scholar]
- Meyer H. M., Jr, Parkman P. D., Hopps H. E. The control of rubella. Pediatrics. 1969 Jul;44(1):5–20. [PubMed] [Google Scholar]
- Ogra P. L., Kerr-Grant D., Umana G., Dzierba J., Weintraub D. Antibody response in serum and nasopharynx after naturally acquired and vaccine-induced infection with rubella virus. N Engl J Med. 1971 Dec 9;285(24):1333–1339. doi: 10.1056/NEJM197112092852401. [DOI] [PubMed] [Google Scholar]
- Parkman P. D., Meyer H. M., Jr, Kirschstein R. L., Hopps H. E. Attenuated rubella virus. I. Development and laboratory characterization. N Engl J Med. 1966 Sep 15;275(11):569–574. doi: 10.1056/NEJM196609152751101. [DOI] [PubMed] [Google Scholar]
- Perkins J. C., Tucker D. N., Knope H. L., Wenzel R. P., Hornick R. B., Kapikian A. Z., Chanock R. M. Evidence for protective effect of an inactivated rhinovirus vaccine administered by the nasal route. Am J Epidemiol. 1969 Oct;90(4):319–326. doi: 10.1093/oxfordjournals.aje.a121076. [DOI] [PubMed] [Google Scholar]
- Plotkin S. A., Bechtel D. J., Sedwick W. D. A simple method for removal of rubella hemagglutination inhibitors from serum adaptable to finger-tip blood. Am J Epidemiol. 1968 Nov;88(3):301–304. doi: 10.1093/oxfordjournals.aje.a120888. [DOI] [PubMed] [Google Scholar]
- Plotkin S. A., Farquhar J. D., Katz M., Buser F. Attenuation of RA 27-3 rubella virus in WI-38 human diploid cells. Am J Dis Child. 1969 Aug;118(2):178–185. doi: 10.1001/archpedi.1969.02100040180004. [DOI] [PubMed] [Google Scholar]
- Rossen R. D., Butler W. T., Cate T. R., Szwed C. F., Couch R. B. Protein composition of nasal secretion during respiratory virus infection. Proc Soc Exp Biol Med. 1965 Aug-Sep;119(4):1169–1176. doi: 10.3181/00379727-119-30406. [DOI] [PubMed] [Google Scholar]
- Smith C. B., Purcell R. H., Bellanti J. A., Chanock R. M. Protective effect of antibody to parainfluenza type 1 virus. N Engl J Med. 1966 Nov 24;275(21):1145–1152. doi: 10.1056/NEJM196611242752101. [DOI] [PubMed] [Google Scholar]
- Waldman R. H., Spencer C. S., Johnson J. E., 3rd Respiratory and systemic cellular and humoral immune responses to influenza virus vaccine administered parenterally or by nose drops. Cell Immunol. 1972 Feb;3(2):294–300. doi: 10.1016/0008-8749(72)90168-2. [DOI] [PubMed] [Google Scholar]



