Abstract
The possibility of encountering rare tropical disease presentations is commonly described as a benefit derived by developed world medical trainees participating in clinical service-oriented short-term global health experiences in the developing world. This study describes the health status of a population served by a short-term experience conducted by a North American institute, and the results of a retrospective review are used to identify commonly encountered diseases and discuss their potential educational value. Descriptive analysis was conducted on 1,024 encounter records collected over four unique 1-week-long trips by a North American institution serving Haitian migrant workers in La Romana, Dominican Republic. The top five diagnoses seen in the clinic were gastroesophageal reflux disease (GERD), hypertension (HTN), upper respiratory infections, otitis media, and fungal skin infection. On occasion, diagnoses unique to an indigent tropical population were encountered (e.g., dehydration, malnutrition, parasites, and infections.). These findings suggest a similarity between frequently encountered diagnoses on a short-term clinical service trip in Dominican Republic and primary care presentations in developed world settings, which challenges the assumption that short-term service experiences provide exposure to rare tropical disease presentations. These findings also represent additional data that can be used to better understand the health and healthcare planning among this vulnerable population of Haitian migrant workers.
Introduction
Interest and participation in short-term medical trips continue to grow among trainees and providers. Such efforts represent significant investments of both finances and volunteer time, with a conservative estimate from 2008 identifying nearly US $250 million spent on 6,000 different United States-led volunteer medical trips arising from over 500 different organizations.1 Academic institutions increasingly provide such experiences in the form of medical missions or brigades2 and global health electives abroad, typically lasting from 1 to 4 weeks in duration.3,4 These volunteer experiences often focus on providing clinical services, teaching, or conducting research studies in resource-limited settings abroad.5,6
The Dominican Republic is one of the countries served by these efforts, many of which serve the city of La Romana. A local hospital in La Romana, Good Samaritan Hospital (Hospital el Buen Samaritano), is tasked with providing charity healthcare to sugarcane plantation workers in the community. This population, predominantly made up of Haitian migrant workers, lives in communities called bateyes. These communities often vary on key community health measures, such as population, proximity to an urban center, access to healthcare services, and availability of potable water and food.7–10 This population of undocumented Haitians in the Dominican Republic is largely stable and estimated by the United Nations and other major international organizations at approximately 500,000 to 1 million people.11,12 Notably, despite international recognition, health data on this population are limited and largely unavailable in published literature.
Haitian communities commonly receive healthcare through mobile medical clinics that provide primary care services. These clinics are staffed by visiting short-term teams from the United States and/or Canada and commonly consist of physicians, nurses, pharmacists, other allied health professionals, and public health professionals as well as healthcare trainees.7,10
Existing literature on short-term medical trips suggests that one reason for their popularity is the perception that international medical trips allow people to see unique disease presentations and diseases rarely seen in the developed world. Other reasons for participation include improved clinical judgment and training, increased cultural sensitivity, and fulfillment of altruistic ideals.6,13,14 Using records collected during several short-term medical trips conducted in the Dominican Republic by a United States-based institution, we test these assumptions by identifying the most frequently encountered disease entities and discussing their potential rarity and educational value.
Methods
Clinic context.
Data were collected from patient encounters that took place in 13 separately conducted clinics during a series of medical trips from the same institution in 2011 and 2012. The primary goal of these trips was to expose medical students to primary care work abroad while providing an opportunity to volunteer. Research on disease trends was a secondary goal. Clinical supervision and mentorship were provided by faculty members from the sending institution, whereas local leaders and support staff identified various clinic sites and facilitated clinic operations, including the provision of translation services.
Teams were made up of 16–20 individuals and included medical students in their clinical years, nurses, allied health professionals, and faculty leaders. Each team was equipped with traditional primary care resources and had the ability to conduct standard patient encounters and investigations (including pelvic examinations/pap smears). Most participants had some ability in basic Spanish, but the majority of interviews was conducted through translators. Other than urine dip, urine human chorionic gonadotropin (hCG), and finger-stick blood glucose, laboratory testing and imaging were not available in the field. Patients requiring more advanced investigations and specialist consultation were referred to the local hospital partner.
Patient encounter cards.
Visiting medical volunteers completed patient encounter cards for single visits; these cards did not serve as a cumulative record of patient care. Cards had fields for demographic information (e.g., name and age of the patient) and the clinic site. Notably, patient sex was not a field on the encounter card; providers were asked to note the sex of the patient in their clinical notes, but this notation did not consistently occur. Additional fields recorded blood pressure and weight, with free text fields recording problems, findings, and treatment. The card also included a family planning consult field with a binary yes or no response. Finally, the card also included a field that identified the provider.
The reverse side of the card included checkboxes for a variety of symptoms and conditions that the patient reported when registering for the clinic. The reverse side was completed before the start of the patient encounter. Only legible encounter cards were included in our final analysis.
Data analysis and review.
Before initiating the data review, a uniform legend of codes was developed to cover patient complaints, diagnoses, and treatments. Chart information selected for review included demographics (age, sex, weight, heart rate, and blood pressure), presenting symptoms and signs, diagnoses, and treatments provided.
The presence of freeform fields resulted in significant variability in the quality and quantity of data captured. To facilitate the accurate collection of data, coders were physicians or medical students who were familiar with the community, the nature of the program, and the material being reviewed. A protocol was developed to reduce interobserver variability between coders. Primary investigators individually reviewed and coded a set of representative cards and compared results. Group discussions resolved coding discrepancies by consensus, which informed the development of standardized definitions and the process to ensure uniformity of coded data.
Coded data were manually reviewed, cleaned, and entered into Stata IC 11 (StataCorp, College Station, TX), from which basic descriptive analyses were conducted identifying population demographics and context. Initial analysis of broad categories then guided additional subanalyses on the interesting initial trends noted. Research ethics approval was obtained from the University of Toronto Institutional Review Board.
Results
Basic batey demographics.
In total, 1,063 encounter cards from 13 days of clinic in 13 bateyes from March of 2011 and 2012 were coded. Exclusion of 39 dental patient encounters provided a final total of 1,024 patient encounters for analysis.
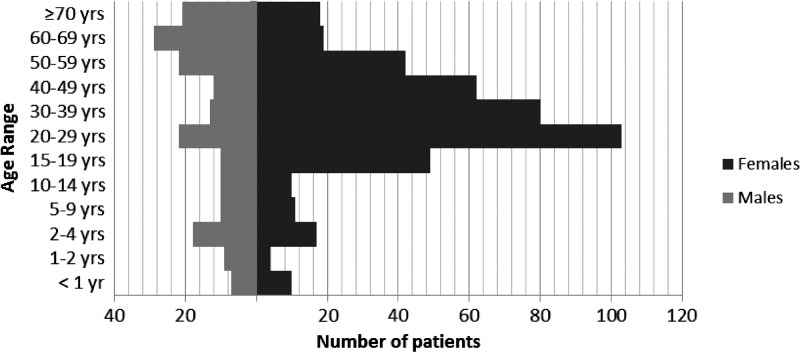
Figure 1 displays the age groups by sex of the patients seen during these clinics.
Figure 1.
Age and sex information of the batey patients in this study.
For 15 encounters, no age information was recorded; similarly, 399 encounters had no sex information. Recorded patient ages ranged from a few days old to greater than 70 years old, with 20- to 29-year-old patients being the largest age group. Of 608 patients for which sex was indicated on the encounter card, 425 (69.9%) patients were female, and 183 (30.1%) patients were male. Notably, patients with sex recorded between the ages of 15 and 39 years old were largely female (65.4% were female and 12.7% were male). This discrepancy was less apparent among older patients; 29% of patients were children, which we defined as being younger than 15 years old, the age at which many individuals leave school and begin to work in this population.
The most frequent diagnoses in batey patients.
Two analyses examined general categories of diagnoses by category and subsequently, individual diagnosis. We had 65 coded diagnoses divided into 13 categories.
Table 1 shows the top diagnoses made in the bateyes for all patients.
Table 1.
The most frequent diagnoses made during short-term medical clinic encounters
| Number of patients | |
|---|---|
| Top five systems affected | |
| GI | 267 |
| Derm | 163 |
| CV | 147 |
| OB-GYN | 144 |
| Resp | 130 |
| Top diagnosis | |
| GI: GERD | 190 |
| None | 169 |
| CV: HTN | 144 |
| Resp: cold/upper respiratory tract infection/flu/otitis media | 103 |
| Derm: fungal infection | 74 |
| Diagnoses contained in each system for the top five systems affected | |
| GI: GERD | 190 |
| GI: parasite | 36 |
| GI: malnutrition | 21 |
| GI: constipation | 8 |
| GI: gastroenteritis | 8 |
| CV: HTN | 144 |
| CV: arrhythmia/murmur | 3 |
| Resp: cold/URI/flu/otitis media | 103 |
| Resp: allergic rhinitis | 14 |
| Resp: asthma | 7 |
| Resp: pneumonia | 5 |
| Resp: tuberculosis | 1 |
| Derm: fungal infection | 74 |
| Derm: dermatitis/skin infection, not otherwise specified | 26 |
| Derm: scabies | 22 |
| Derm: eczema | 20 |
| Derm: laceration | 9 |
| Derm: other | 7 |
| Derm: impetigo | 3 |
| Derm: burn | 1 |
| Derm: condyloma | 1 |
| OB-GYN: pregnancy | 58 |
| OB-GYN: candidiasis | 50 |
| OB-GYN: vaginitis, not otherwise specified | 16 |
| OB-GYN: bacterial vaginosis | 12 |
| OB-GYN: pelvic inflammatory disease | 6 |
| OB-GYN: uterine fibroid | 2 |
| OB-GYN: trichomoniasis | 0 |
CV = cardiovascular; Derm = dermatological; flu = flu-like symptom; GI = gastrointestinal; OB-GYN = obstetric and gynecological; Resp = respiratory.
The most common diagnosis was GERD, with the top diagnostic category being gastrointestinal findings. Presentations most frequently fell into the gastrointestinal, cardiovascular, respiratory, obstetric/gynecologic, and dermatological diagnostic categories. The top five individually identified diagnoses paralleled these groupings being GERD, no diagnosis listed/inferred, HTN, upper respiratory infection/otitis media, and fungal skin infection.
HTN in the bateyes.
HTN, the third most common diagnosis, has a particular relevance given the implementation of an anti-HTN program among providers visiting the Good Samaritan Hospital. Coding review noted that 144 patients (22.9% of adults over the age of 20 years) were diagnosed with HTN. Notably, this proportion was noticeably at odds with the number of patients whose measured blood pressures at the encounter were within the HTN range. Applying the The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) criteria for HTN to the recorded systolic and diastolic readings, 321 patients would have met the diagnostic criteria for HTN.
Table 2 lists the 10 most common symptoms described during a patient encounter by those who were diagnosed with HTN by a provider. Although most patients diagnosed with HTN were asymptomatic, there were several complaints, with headache being the top complaint (46 patients reporting some form of headache). Other complaints included visual changes (N = 33), dizziness (N = 20), and chest pain (N = 8).
Table 2.
The 10 most common presenting signs or symptoms of those patients diagnosed with HTN
| Presenting signs/symptoms | Number of patients |
|---|---|
| Headache | 46 |
| Generalized aches/myalgia | 35 |
| Visual changes | 33 |
| Abdominal pain | 32 |
| Dizzy | 20 |
| Backache | 19 |
| Lower limb joint pain | 16 |
| Rash/lesion | 10 |
| Chest pain | 8 |
| Poor appetite | 7 |
Other diagnoses.
Less frequent but important diagnoses included lacerations (N = 9) and fractures (N = 2), which would have required specific material resources and considerable procedural expertise on the part of the medical team. Other less frequent but potentially serious diagnoses recorded included pelvic inflammatory disease (N = 4), cancer (any type; N = 4), cardiac arrhythmia (unspecified; N = 1), osteomyelitis (N = 1), and tuberculosis (N = 1), the management and follow-up for which was unclear. Of note, several diagnoses that were commonly reported would likely be less common in North America; these included fungal infections (N = 73), dehydration (N = 42), parasitic infections (N = 36), and malnutrition (N = 20). Finally, with the exception of HTN, broad trends indicated the diagnosis of more acute and infectious diseases as opposed to non-communicable or mental health conditions. In particular, depression and anxiety, which make up a significant proportion of primary care in developed settings, were rarely noted (N = 2), although this finding may be because specific screening was not being carried out.
Treatments.
We noted that the majority of patients were given common over-the-counter medications that included daily vitamins, acetaminophen, ibuprofen, antacids, ranitidine, and antifungal cream (Table 3). Other than amlodipine, which was given to 127 patients and is the anti-HTN medication typically used in this region of the Dominican Republic, the only other prescription medication that made the top 10 medications was amoxicillin.
Table 3.
The 10 most common medications dispensed to batey patients
| Medication distributed | Number of patients |
|---|---|
| Vitamins | 781 |
| Acetaminophen | 480 |
| Ibuprofen | 236 |
| Tums | 183 |
| Amlodipine | 127 |
| Amoxicillin | 84 |
| Ranitidine | 81 |
| Prenatal vitamins | 61 |
| Antifungal cream | 53 |
| Other | 53 |
Discussion
This study describes observed trends of disease among primary care patients attending a series of mobile visiting clinic in the Dominican Republic. Literature has frequently described the format of mobile clinics in the developing world being provided by medical brigades from North American institutions, suggesting that the clinics studied here are fairly representative of similar efforts elsewhere.2,7,15–17
Although patients of all ages and both sexes were seen, most of the adult patients of working age who came to the clinic were female. The likely reason for this result is that men of working age were working in the sugarcane fields and unable to attend clinic, although data have traditionally also suggested that women are more likely to seek care than men.18 The sex breakdown among the older patients seemed to be more evenly split based on the limited sex information that was available.
The high prevalence of obstetric/gynecologic complaints likely reflects the large proportion of females in this study. However, it could also indicate the need for a focus on women's health in this community. Additional review of the breakdown of the obstetric/gynecologic category shows that pregnancy and presumptive yeast infection were the top concerns. Of note, many patients reported receiving prenatal care elsewhere other than the mobile clinic.
The number of batey patients with HTN was notable given the relationship between HTN and cardiovascular and cerebrovascular diseases. The discrepancy between those formally diagnosed with HTN versus those displaying HTN readings was of particular import. Additional investigation is warranted, particularly given the limited associations derived from the data, the finding of patients with HTN under the age of 30 years of age, and the presentation of potentially symptomatic HTN identified in a number of encounters.
Overall, the vast majority of the diagnoses made by short-term visiting teams to the bateyes of La Romana closely paralleled the diagnoses made in a primary care clinic in developed countries. These diagnoses include common diagnoses, such as upper respiratory tract infections (colds), urinary tract infections, pregnancy, and HTN. However, there are a few notable exceptions, including a high prevalence of fungal skin lesions, parasitic infections, malnutrition, and dehydration, along with a small number of concerning diagnoses that included emergent traumas and chronic deep tissue infections that likely presented to these temporary clinics out of convenience. Additionally, a number of patients did not have a determined diagnosis based on the information available. It is believed that these patients were diagnosed as healthy, but we cannot exclude the possibility that these patients' encounter records were incomplete or unfilled.
Analyses on treatments were limited, because medications on such trips are commonly restricted by what the team has on hand. Our findings, thus, reflect what was available and have limited implications for what physicians would have liked to prescribe. Such limited supplies result in advice for patients to obtain drugs from other sources. Although obtaining medications from local providers can lead to improved compliance and locally appropriate counseling and dispensing, there are also risks related to non-availability at local clinics or unreliable or counterfeit medications. Counterfeit medications have been monitored by the World Health Organization (WHO) over the past decade, with the Dominican Republic Public Health Department reporting that 10% of the medicines arriving in the country are fake and that another 50% of medicines are being produced illegally.19
Interestingly, the most commonly dispensed treatments—approximately one-third of all the treatments rendered—were over-the-counter medications by North American definitions. This finding raises questions about patient access to basic medications and the quantities of these medications that should be dispensed at a given time; furthermore, as with clinics in the United States and Canada, concerns include patient compliance and follow-up. Notably, except for amlodipine, chronic disease medications were not commonly dispensed by these mobile clinics, likely reflecting their acute focus. Collaboration between brigades, development of cumulative recordkeeping, improved patient education, and pursuit of appropriate procurement chains are minimum requirements that would allow such short-term experiences to increase their impact on the burden of chronic disease in this community.
There were several limitations to this study. The nature of translated data and cultural context could have limited findings of more subjective/stigmatizing diagnoses (e.g., depression) as opposed to more objective diagnoses, such as HTN or injury. Similarly, the spectrum of diagnoses seen overall reflects the pattern expected from a primary care clinic; different patterns would be observed from medical work abroad that focuses on specific medical specialties (e.g., surgical care and ophthalmology.) However, if trying to ascertain an overall burden of disease in the population, primary care likely affords the most realistic breadth for doing so.
Data from encounter cards were not initially collected for research purposes but rather, to clinically record a single patient encounter. The incomplete design of the cards (e.g., missing a field to designate whether the patient was male or female and no fields for physical examination findings, laboratory findings, or treatment plans) also limited the data available, whereas collection for clinical purposes without a uniform protocol or form also resulted in interprovider variability with respect to the recorded information and care rendered. The absence of confirmatory testing in this setting further limits our ability to determine which parasites are most prevalent or whether Helicobacter pylori infection is related to the high frequency of GERD seen in this population. In particular, the ratio of supervisor to students may have also contributed to this variability.
A lack of cumulative patient information, caused by absent continuity mechanisms from the local providers, made it difficult to evaluate ongoing care for chronic diseases. This absence of continuity indirectly provided an example to learners of the importance of longitudinal information in the effective provision of primary care. Although implementing an electronic medical record (EMR) system holds some promise to providing continuity of information, the practical challenges of following a highly migratory group of patients who receive care through several providers, including their employer, limit the effectiveness of EMR in this setting. Any solution involving information technology will require local involvement to maintain it, a challenge compounded by monetary limitations and the multiple parties involved. At present, we have implemented a pilot project with patient-held records with the hope of collecting more longitudinal information independent of the patients' current location or where they go to receive care.
Assessing underlying causes of disease patterns was also limited because of a lack of data on the context of the batey communities, such as local access to healthcare facilities, the availability of sanitary drinking water, or the presence of a community school. Future research work will benefit from integrating a more comprehensive overview of health and social structures into pre-departure training curricula. Background knowledge will inform better data collection and support the development of additional research hypotheses.
As a specific example, the conduct of these clinics in the day limits the inclusion of working adult men and thus, limits working adult men being sampled. It is possible, however, that they might seek care elsewhere. Similarly, our results also indicated that pregnant women reported receiving prenatal care from other sources. One possible other source could be sugarcane corporation medical clinics that anecdotally operate independently of visiting medical teams; active research to develop a comprehensive understanding of local health system dynamics is ongoing.
Conclusion
Our findings suggest that the patterns of disease noted in the batey populations of La Romana closely mirror those seen in primary care settings in the developed world, with a few notable exceptions related to the community's tropical limited-resource context. The worldwide burden of chronic disease is widely reflected in recent literature and reports, most notably in the 2013 Global Burden of Disease Study published by the WHO. This report identified ischemic heart disease and stroke as being the top two causes of death worldwide, accounting for 25% of global mortality burden.20
Additional research, specifically targeted to the batey population, will help to better understand the effects of observed disease trends on this indigent community. In the context of worldwide growth in rates of stroke and ischemic heart disease, the findings of HTN among this population are concerning, whereas the significant demand for obstetric/gynecologic services and prenatal care has broad implications for maternal/child health efforts.
Similar disease trends will undoubtedly be observed in other settings abroad. The hope is that the patterns described in this study will help medical schools, faculty, and trainees better prepare for and responsibly tailor their global health elective and outreach efforts—be it in the Dominican Republic or elsewhere in the world.
ACKNOWLEDGMENTS
The authors thank Dr. Michele Pugnaire (Senior Associate Dean for Educational Affairs, University of Massachusetts Medical School) for her ongoing support and guidance. The authors further acknowledge the contributions of Dr. Maria Garcia (University of Massachusetts Memorial Medical Center) and thank Moises Sifren Juan, Dr. Franklin Bido, and the staff and healthcare providers of Good Samaritan Hospital, La Romana, Dominican Republic. The authors also thank Caitlin Fogarty, Kristina Prachanronarong, and Vivek Venugopal for their assistance in record review and coding. Ethical approval was obtained from the University of Toronto Research Ethics Board (Protocol ID 28725.)
Footnotes
Authors' addresses: Brian J. Ferrara, Baystate Medical Centre, Springfield, MA, E-mail: brian.ferrara@gmail.com. Elizabeth Townsley and Christopher R. MacKay, University of Massachusetts Medical School, Worcester, MA, E-mails: elizabeth.townsley@umassmed.edu and christopher.mackay@umassmed.edu. Henry C. Lin, Children's Hospital of Philadelphia, Philadelphia, PA, and The 53rd Week, Brooklyn, NY, E-mail: hclin6@gmail.com. Lawrence C. Loh, Dalla Lana School of Public Health, University of Toronto, Toronto, ON, Canada, University of British Columbia, Vancouver, BC, Canada, and The 53rd Week, Brooklyn, NY, E-mail: lloh@jhsph.edu.
References
- 1.Maki J, Qualls M, White B, Kleefield S, Crone R. Health impact assessment and short-term medical missions: a methods study to evaluate quality of care. BMC Health Serv Res. 2008;8:121. doi: 10.1186/1472-6963-8-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rassiwala J, Vaduganathan M, Kupershtok M, Castillo FM, Evert J. Global health educational engagement—a tale of two models. Acad Med. 2013;88:1651–1657. doi: 10.1097/ACM.0b013e3182a6d0b0. [DOI] [PubMed] [Google Scholar]
- 3.Wilson JW, Merry SP, Franz WB. Rules of engagement: the principles of underserved global health volunteerism. Am J Med. 2012;125:612–617. doi: 10.1016/j.amjmed.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Panosian C, Coates TJ. The new medical “missionaries”—grooming the next generation of global health workers. N Engl J Med. 2006;354:1771–1773. doi: 10.1056/NEJMp068035. [DOI] [PubMed] [Google Scholar]
- 5.Bauer TA, Sanders J. Needs assessment of Wisconsin primary care residents and faculty regarding interest in global health training. BMC Med Educ. 2009;9:36. doi: 10.1186/1472-6920-9-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramsey AH, Haq C, Gjerde CL, Rothenberg D. Career influence of an international health experience during medical school. Fam Med. 2004;36:412–416. [PubMed] [Google Scholar]
- 7.Crouse HL, Macias CG, Cruz AT, Wilson KA, Torrey SB. Utilization of a mobile medical van for delivering pediatric care in the bateys of the Dominican Republic. Int J Emerg Med. 2010;3:227–232. doi: 10.1007/s12245-010-0198-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rojas P, Malow R, Ruffin B, Rothe EM, Rosenberg R. The HIV/AIDS epidemic in the Dominican Republic: key contributing factors. J Int Assoc Physicians AIDS Care (Chic) 2011;10:306–315. doi: 10.1177/1545109710397770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohn KA, Finalle R, O'Hare G, Feris JM, Fernandez J, Shah SS. Risk factors for intrathoracic tuberculosis in children from economic migrant populations of two Dominican Republic bateyes. Pediatr Infect Dis J. 2009;28:782–786. doi: 10.1097/INF.0b013e3181a164a8. [DOI] [PubMed] [Google Scholar]
- 10.Brewer TH, Hasbun J, Ryan CA, Hawes SE, Martinez S, Sanchez J, Butler de Lister M, Constanzo J, Lopez J, Holmes KK. Migration, ethnicity and environment: HIV risk factors for women on the sugar cane plantations of the Dominican Republic. AIDS. 1998;12:1879–1887. doi: 10.1097/00002030-199814000-00020. [DOI] [PubMed] [Google Scholar]
- 11.United Nations Trust Fund for Human Security . Improving Human Security in the Bateyes of the Dominican Republic by Securing Documentation and Ensuring That Vulnerable People's Needs Are Met. 2013. https://docs.unocha.org/sites/dms/HSU/088%20Dominican%20Republic%20-%20FINAL.pdf Available at. Accessed April 5, 2014. [Google Scholar]
- 12.Organization of American States—Inter American Commission on Human Rights Situation of Haitian Migrant Workers and Their Families in the Dominican Republic. 1999. http://www.cidh.org/countryrep/dominicanrep99/Table.htm Available at. Accessed April 5, 2014.
- 13.Houpt ER, Pearson RD, Hall TL. Three domains of competency in global health education: recommendations for all medical students. Acad Med. 2007;82:222–225. doi: 10.1097/ACM.0b013e3180305c10. [DOI] [PubMed] [Google Scholar]
- 14.Miller WC, Corey GR, Lallinger GJ, Durack DT. International health and internal medicine residency training: the Duke University experience. Am J Med. 1995;99:291–297. doi: 10.1016/s0002-9343(99)80162-4. [DOI] [PubMed] [Google Scholar]
- 15.Oken E, Martinez Stoffel E, Stern LJ. Use of volunteer medical brigades to assess growth in Honduras. J Trop Pediatr. 2004;50:203–208. doi: 10.1093/tropej/50.4.203. [DOI] [PubMed] [Google Scholar]
- 16.Martiniuk AL, Adunuri N, Negin J, Tracey P, Fontecha C, Caldwell P. Primary care provision by volunteer medical brigades in Honduras: a health record review of more than 2,500 patients over three years. Int J Health Serv. 2012;42:739–753. doi: 10.2190/HS.42.4.i. [DOI] [PubMed] [Google Scholar]
- 17.Green T, Green H, Scandlyn J, Kestler A. Perceptions of short-term medical volunteer work: a qualitative study in Guatemala. Global Health. 2009;5:4. doi: 10.1186/1744-8603-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bertakis KD, Azari R, Helms LJ, Callahan EJ, Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147–152. [PubMed] [Google Scholar]
- 19.World Health Organization Counterfeit Medicines. 2006. http://www.who.int/medicines/services/counterfeit/impact/ImpactF_S/en/ Available at. Accessed December 13, 2013.
- 20.World Health Organization The Top 10 Causes of Death. Fact Sheet Number 310. 2013. http://www.who.int/mediacentre/factsheets/fs310/en/ Available at. Accessed April 5, 2014.